Abstract
Using telehealth in early intervention has the potential to increase family and child outcomes as well as to increase access to family-centered services. Yet, little is known about families’ perspectives, including concerns, prior to using telehealth in early intervention. The purpose of this study was to explore families’ perceptions and attitudes toward using telehealth in early intervention. Nine focus groups were conducted with 37 families of children with disabilities. Overall, participants preferred in-person visits (versus telehealth) for early intervention services. However, participants recognized some benefits of telehealth in facilitating communication with early intervention professionals and reaching underserved families. In addition to benefits, participants identified barriers to telehealth including limited access to: technology, the internet and materials. Policymakers and professionals should consider the perspectives, priorities and concerns of families before implementing telehealth in early intervention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The purpose of early intervention (EI) is dual-pronged: to address the developmental needs of infants and toddlers (children from birth through 36 months) with developmental delays or disabilities and to provide supports for families to help them understand how to meet their children’s needs (Individuals With Disabilities Education Act [IDEA], 2004). According to IDEA, EI services may include occupational therapy, physical therapy, speech therapy, behavior therapy, and other types of services which can address the developmental needs of children. For example, among children with autism spectrum disorder (ASD), the receipt of applied behavior analysis (ABA) services facilitates improved outcomes (Orinstein et al., 2014).
In the past decade, there is an increasing demand for EI services in the United States (Wise et al., 2010). When children receive EI services, they demonstrate improved developmental outcomes (Fuller & Kaiser, 2019; Noyes-Grosser et al., 2018). However, underserved families (e.g., families: living in rural areas, reflecting minority or low socioeconomic backgrounds; having limited formal education) may face several challenges in accessing sufficient and high-quality EI services. For example, families from low socioeconomic backgrounds may participate in fewer EI services because of scheduling conflicts and transportation costs compared with families from higher socioeconomic backgrounds (Pickard & Ingersoll, 2016). Families from rural areas may encounter provider shortages due to longer travel times for providers (Barr et al., 2019) and higher health care costs (Moffatt & Eley, 2010). Minority families (e.g., Spanish-speaking families) may face barriers in accessing services due to a shortage of Spanish-speaking providers (Williams et al., 2013).
Telehealth could be a potential solution to reduce EI service disparities. According to the American Occupational Therapy Association (Cason et al., 2018), telehealth is an emerging model which allows health-related services to be delivered through information and communication technologies (e.g., videoconferencing, video clips) when patients and providers are in different physical locations. A growing number of studies have reported that the use of telehealth in EI could benefit both families and children (Behl et al., 2017; Blaiser et al., 2013). In a review of the use of telehealth with ABA services, Ferguson et al. (2019) found that telehealth yielded positive outcomes for children. Behl et al. (2017) compared the effectiveness of EI provided via telehealth and in-person among children with hearing impairments. Families who received EI via telehealth (versus in-person) reported greater competence in supporting their children’s developmental needs. In other studies, service providers and families have reported positive experiences with telehealth (Kelso et al., 2009; Wallisch et al., 2019).
Although telehealth could be used to ensure access to EI services for all families, families’ perceptions before the use of telehealth remains unclear. The limited extant research has only examined families’ perceptions of telehealth after it has been used with families (e.g., Ashburner et al., 2016; Behl et al., 2017; Blaiser et al., 2013; Wallisch et al., 2019). In research about the social validity of telehealth, families who have experienced telehealth often report that telehealth was highly acceptable and feasible (Wainer & Ingersoll, 2015; Wallisch et al., 2019). However, only examining the perceptions of families who have experienced telehealth is insufficient. Research has identified some barriers to telehealth, including: technical issues (i.e., low internet speed, lack of troubleshooting resources); less time to develop rapport between therapists, families, and children; few toys and equipment to conduct therapy; and inappropriate environmental arrangements (Ashburner et al., 2016; Cole et al., 2019; Fairweather et al., 2016). These barriers may result in the limited utilization of telehealth by stakeholders (Cason et al., 2012; Cole et al., 2016).
As a first step to widespread use of telehealth, it is important to develop materials and practices to inform families about telehealth. In this way, practitioners can solicit buy-in from families to use telehealth. Thus, exploring the perceptions of diverse families without prior experience with telehealth may help inform the use of telehealth practices and identify the challenges families and practitioners may experience when using telehealth in EI. Such research aligns with the call for more rigorous research about the use of telehealth (Ferguson et al., 2019). To this end, the purpose of this study was to explore families’ perspectives of telehealth in EI. Specifically, three research questions guided this study:
-
1.
What are families’ perceptions regarding the implementation of telehealth in EI?
-
2.
What do families report as advantages and disadvantages to implementing telehealth in EI?
-
3.
What are families’ perceptions of logistical challenges in implementing telehealth in EI?
As our theoretical framework for this study, we used social-cultural capital theory. Social capital entails relationships which afford the exchange of information (Bourdieu, 1986). Many parents of children with disabilities rely on social capital via relationships (e.g., relationships with professionals and/or other parents of children with disabilities, Solomon et al., 2001). Notably, however, social-cultural capital may look different among diverse (e.g., underserved) families with such families having unique strengths (Yosso, 2005) and facing systemic barriers to accessing certain types of capital (Harry, 2008). Social-cultural capital theory helps us navigate and explain how differences among diverse families could lead to differing perceptions of telehalth. For example, underserved families who face systemic barriers to social capital (e.g., limited EI providers) and cultural capital (e.g., limited access to materials and information) could encounter several barriers to using telehealth in EI.
Method
Study Design
To explore the perspectives of families of children with disabilities regarding the use of telehealth in EI, a qualitative design was chosen. Specifically, focus groups were conducted for this study. Focus groups allow individuals with a shared commonality (e.g., families of children who received EI services, Krueger & Casey, 2000) to share their perspectives about a topic.
Participants
To be included in the study, participants needed to be: older than 18 years of age; have a child (aged 0–9 years) who received EI services; and willing to participate in a 60–90 min focus group discussion. A total of nine focus groups (seven in English and two in Spanish) were conducted with 37 participants throughout a Midwestern state. The number of participants per focus group ranged from 1 to 7 participants with an average of four participants in each focus group. The same focus group protocol was used in each focus group, regardless of the size of the focus group. There were no observed differences in group dynamics in relation to the number of participants or demographic composition of each focus group.
Among the 37 participants, the majority of the participants was female (81.1%; n = 30). On average, the participants were 40 years of age (SD = 5.87; range from 33 to 57 years). The majority of the participants identified as White. Notably, 60% of the participants reported annual household incomes of less than $100,000. In addition, 35% of the participants only had a high school education. In four focus groups (two groups in urban areas, one group in a suburban area, and one group in a rural area), there was at least one married couple who participated in the focus group. Although married couples comprised 32% of the total sample, we found that the couples often had different responses to the focus group questions. Since there were six married couples included in the study, we present the demographic information from their 31 children. No parents/couples had more than one child with disabilities. On average, the children were 3.9 years of age (SD = 2.13; range from 1.5 to 9 years). The disabilities of the children varied with most children having developmental delays. See Table 1 for more details.
Recruitment
After the Institutional Review Board approved the study, we distributed the recruitment flyer to EI agencies and providers, disability organizations, and parent support groups to recruit participants. We also used personal contacts and social media (e.g., Facebook, Twitter) to recruit participants. Individuals who were interested in the study contacted the first author to register for a focus group. At the end of each focus group, participants received books and EI materials. If participants completed the member check, they received a $10 gift card.
Setting
Focus groups were conducted throughout a Midwestern state. Specifically, four focus groups were conducted in urban areas, three focus groups were conducted in suburban areas, and two focus groups were conducted in rural areas. Each focus group was held in a location that was convenient to the participants (e.g., an EI office, a provider organization in the community, etc).
Procedures
Focus groups were held from February to May of 2019. Data were collected via a demographic questionnaire and a semi-structured focus group protocol .
Demographic Questionnaire
The first part of the questionnaire included the demographic information of the participant and their child with a disability (e.g., family’s educational background, gender, race, household income, child’s age, disability, and EI services). The second part of the questionnaire was adapted from a previous study examining social validity of telehealth for Spanish-speaking families (Fitton et al., 2017). This part included questions about participant preferences in receiving EI services (e.g., “How would you prefer to receive early intervention services?”), knowledge and attitudes about telehealth, and access and ability to use technology via yes/no, rating scales and open-ended questions.
Focus Group Protocol
To develop the focus group protocol, an extensive literature search was completed (e.g., Ashburner et al., 2016; Iacono et al., 2016). A pilot focus group was conducted with four parents of children who received EI services. Participants requested minor changes to the protocol (e.g., changing the order of questions, allowing more time for the focus group). Changes were made accordingly. Although the pilot participants shaped the protocol, they were not included in this study. A list of the focus group questions can be found in Table 2.
During the focus group, before asking questions about telehealth, we showed a short video about telehealth. Specifically, we showed a YouTube clip of telehealth being used in an occupational therapy session with a family and an occupational therapist. The video was used so participants could visualize a telehealth EI session. Also, a definition of telehealth was shared with the participants before asking about their attitudes toward telehealth in EI. Specifically, the focus group facilitator told the participants: “The definition of telehealth is the use of technology to deliver services, whether medical, educational, etc., remotely. One example of telehealth is a psychologist having a counseling session with a client over the phone. Another example is a speech therapist providing therapy over Skype. Telehealth can involve a variety of technologies, such as phone, Facetime, and videoconferencing” (Fitton et al., 2017).
Among the nine focus groups, two focus groups were conducted in Spanish by a bilingual facilitator who is fluent in Spanish and English and seven focus groups were conducted in English by the first author. Both facilitators have extensive experiences working in EI and the disability field. The focus groups lasted approximately 1–1.5 h, and were attended by two individuals: a facilitator and a note-taker. All of the focus groups were audio-recorded and transcribed verbatim. Spanish focus groups were transcribed and translated using the forward/backward translation method (Brislin, 1970).
Data Analysis
Focus group transcripts were analyzed using constant comparative analysis (Glaser & Strauss, 2017) and emergent coding (Patton, 2002) in alignment with the research questions. Responses were triangulated with other data (e.g., the demographic questionnaire). The first and the second author read three transcripts independently to familiarize themselves with the data (Tesch, 1990). Second, the authors independently coded all transcripts using a line-by-line approach to identify emergent codes (e.g., telehealth as a supplement, child needs physical touch). The Authors recorded comments as they identified key concepts from the text (i.e., ways to use telehealth, advantages of telehealth). Then, the authors met to develop a codebook with the concepts and related codes. Each author independently analyzed the remaining transcripts using the codebook. They met again to compare the codes, resolve disagreements, and determine if new codes were represented in the data. After finalizing the codebook, the authors examined all of the transcripts again to ensure accuracy. They found no additional codes. After comfirming the codes, the authors grouped the codes into categories, and developed the themes anchored to the research questions.
Credibility and Trustworthiness
Several steps were conducted to ensure credibility and trustworthiness and to prevent bias (Brantlinger et al., 2005). First, to ensure that the data were valid and reliable, the authors conducted a member check. Specifically, after the focus group, the authors summarized each focus group discussion and developed a summary. The summary was e-mailed to the relevant participants. Each participant was asked to review and validate the summary (Guba & Lincoln, 1989; Onwuegbuzie & Leech, 2007). Overall, 21 of the 37 participants completed the member check, agreeing with the written summary. No major changes were suggested. Second, the authors debriefed with each other regularly during data collection and analysis to ensure there were no interpretation biases. Thrid, we used negative case analysis to ensure the data were accuately depicted (Brantlinger et al., 2005). Lastly, triangulation was used by gathering and comparing data from different sources (i.e., questionnaire, focus group discussion, notes taken during the focus group).
Reflexivity
All authors have experiences in working within the EI system and the disability field. For example, the first author was an EI provider; thus, she developed rapport with the participants as an EI professional. The second author is the parent of a child who received EI services. Thus, she built rapport with participants by sharing her personal experience within EI. Notably, to address potential biases, the researchers remained neutral while facilitating the focus groups, and discussing their experiences and reflections after each focus group with one another and the rest of the research team.
Findings
Before we present the findings for each research question, two contextual considerations should be noted. First, participants reported viewing the purpose of EI as providing direct services to the child (not the family). For example, Susan, the mother of a child with speech delays, reported: “I like the therapist physically there. It is a nice break for me. I sometimes step away. I can take a shower or do some stuff on the computer in a different room.” This misconception is important context for exploring perceptions of telehealth. Because telehealth would require the parent to be physically present to engage the child in therapy, the parent’s perspective about the purpose of EI may impact perceptions of telehealth. Second, on the questionnaire, most participants had never heard of telehealth (84%; n = 31). Thus, these participants had no experience with telehealth or prior understanding of its use in EI. It is important to consider these contextual findings while reading the themes for each research question.
Family Perceptions of Using Telehealth in EI
Three themes emerged from the participants: (a) a preference for in-person visits (versus telehealth), (b) a perception of telehealth as a supplement--not a replacement--for in-person visits, and (c) a preference for telehealth (versus no EI services).
Preference for in-Person Visits
The majority of participants strongly indicated that they preferred to receive EI services in-person (versus via telehealth). Andres, the Spanish-speaking father of a child with ASD, reported,
Preferiría que viniera la persona [el terapeuta] y le enseñara a mi hijo… no hay nada mejor que interactuar en persona-a-persona. [I would prefer the person [therapist] come and teach my son… there is nothing better than interacting in person-to-person].
Further, participants reported that telehealth would not enable the family and the child to build rapport with therapists. Sofia, the mother of a child with rare genetic syndrome, said: “It is hard to develop a relationship over the phone…it is not the same. And I know my kids especially, she [my daughter] takes a long time to warm up to people.” This theme triangulated with findings from the questionnaire. Specifically, in the questionnaire, all participants ranked “in-person therapy” as their first choice for EI delivery. Participants reported that telehealth was not as effective as in-person therapy; participants also reported that they were not interested in their child receiving EI services via telehealth, when in-person EI services were available.
As a Supplement, Not a Replacement
Despite a preference for in-person EI therapy, some participants reported that they would use telehealth if it was a supplement (versus a replacement) for in-person visits. Ellen, the mother of a child with muscular atrophy, reported: “I would like it [telehealth] as an addition [to EI]. That’s it!” Teressa, the mother of a child with speech delays, wrote in the questionnaire that she would be interested in using telehealth “…if it is just PART of the EI plan.” She further elaborated in the focus group: “I think this [telehealth] is a very interesting complement to it [EI].” Some participants provided additional detail about how telehealth could serve as a supplement. Samantha, the mother of a child with developmental delays and attention-deficit/hyperactivity disorder (ADHD), reported: “I think in between [in-person visits], maybe you wouldn’t have to meet with them [EI therapists], every week or maybe every other week…. But I just don’t think it would be good all the time.” Alice, the mother with a child with ASD, similarly reported: “If you are meeting twice a week, having an in-person meeting the first time and then video conferencing a second time or every or every other week [would be alright].” Participants also reported that telehealth could be used to facilitate communication between parents and therapists. Ellen, the mother a child with muscular atrophy, stated: “…[telehealth] is fine as a follow-up, but not primary [form of EI]. I would happily do, like sort of a monthly, like discussion with my therapists outside of when they are treating my child. I would find that valuable”.
Telehealth Is Better than Nothing
Notably, the majority of the participants reported that they would prefer telehealth over “nothing” or “no EI services”. Daisy, the single mother of a child with speech delays who lived in rural area, reported: “Even though it is not like in-person, face to face, I still feel like it [telehealth] is better than nothing. Anything is better than nothing.” Sofia, the mother of a child with rare genetic syndrome reported, “It [telehealth] is a great tool for people who don’t have an option to have immersive treatments.”
Family Perceptions of Advantages of Telehealth in EI
Despite that none of the participants had used telehealth prior to this study, they identified potential advantages of implementing telehealth in EI. Specifically, advantages included that telehealth could: facilitate family engagement in EI, enable logistical barriers to be overcome, and provide therapists with a more holistic understanding of families.
Family Engagement in EI
Participants reported that telehealth may facilitate family engagement in EI. Specifically, two subthemes emerged: telehealth may facilitate parent training and telehealth may improve communication between therapists and families.
Facilitate Parent Training
Participants reported that telehealth may enable therapists to better engage with families. Specifically, telehealth may enable therapists to: coach parents to implement strategies, provide parents with feedback, and reinforce implementation of strategies outside of therapy sessions. Sofia, the mother of a child with rare genetic syndrome, reported: “I think this [telehealth] can be a really good tool to teach parents… about how you [parents] should coach your kid.” Katie, the mother of a child with ASD, reported: “For me, it [telehealth] is more of the support for the parents. I think it is better that kind of tool than actually helping with the child. It is more of therapy for the parent.”
Participants also reported that telehealth may enable them to record the EI session and implement EI strategies themselves, outside of therapy sessions. In this way, participants could learn how to support their children through recorded telehealth sessions. For example, Vivian, the mother of a child with speech delays, reported: “Live [video] could be great. But even after [i.e., a recorded session] will be awesome. Then, I can watch it, see what they worked on, then can go home and watch it again.” In addition, some participants discussed watching recorded telehealth sessions so they could implement EI strategies outside of the therapy sessions:
Teressa, the mother of a child with speech delays: I would like to be able to occasionally watch it and to see what they are doing so I can do it outside or even pre-record it [session].
Mandy, the mother of a child with ASD: I agree…. if it is a recorded session and it is more like parent training. You can reinforce, like watch this video and this interaction, and your child can be practicing. And you are not missing cues or something like that.
Improve Communication between Therapists and Families
Participants reported that telehealth may facilitate communication between therapists and families, especially if the telehealth session is recorded. Samantha, the mother of a child with developmental delays and ADHD, said: “It doesn’t have to be just in time [in-person]. When we have questions, they [therapists] just videotape themselves answering the questions.” Similarly, participants reported that recorded telehealth sessions may enable parents to share the recording with other family members so they too can implement EI strategies outside of therapy sessions. Daisy, the single mother of a child with speech delays who lived in rural area, reported: “[Videos] can give grandma ideas on how to care for the child.”
Overcome Logistical Barriers
Participants reported that telehealth could benefit underserved families who face systemic barriers in accessing in-person therapy. Such families include individuals: living in rural areas with few EI providers, waiting for EI services, or having disabilities themselves precluding them from leaving the house. Brittney, the mother of a child with a visual impairment, reported: “If there is another option, particularly in the rural area where we had a pretty good waitlist for speech and OT [occupational therapy], they saw therapists once a month, you know. I think there is a place for it [telehealth].” Andres, the father of a child with ASD, explained:
También tengo en cuenta que la discapacitada puede ser la mama o el papa que no puede salir de su casa y no puede caminar, no puede salir o alguna enfermedad que le dificulte salir de su casa. En ese aspecto, yo creo que es perfecto un video. [I also have in mind that for [the] mother or the father who cannot leave the house, cannot walk, or have some illness that makes it difficult to leave the house. In that aspect, I think a video is perfect.]
Family Perceptions of Disadvantages of Telehealth in EI
Participants also reported potential disadvantages of telehealth in EI. Specifically, they reported that telehealth may not be able to meet the child’s needs or the family’s needs.
Ability to Meet the child’s Needs
Child Needs Physical Guidance and in-Person Socialization with Therapists
Participants reported that telehealth may not meet the needs of children who need physical (i.e., hands-on) guidance, and would not enable the child to develop social skills and foster rapport with the therapist. Within a suburban focus group, participants reported:
Samantha, the mother of a child with developmental delays and ADHD: I do think there is a value added in being able to physically direct kids, like my son with ADHD…[he] kind of needs that physical touch or redirect.
Kylie, the mother of a child with ASD: Yeah! Especially like the kids with autism or attachment disorder, they need someone to redirect them.
Alice, the mother with a child with ASD: I think depending on the child. If we are talking about a child with autism….they [the child with ASD] are really going to need to see it [the EI strategy] from somebody other than just mom and dad.
Other participants had similar ideas. Anita, the Spanish-speaking mother of a child with ASD, reported: “Se les dificulta mucho la socialización. Entonces, el ponerles un aparato, un dispositivo [por ejemplo, un iPad para telesalud] enfrente de ellos [niños con autismo], no les va ayudar.” [They [children with ASD] have a hard time socializing. So, putting them on a device [e.g., an iPad for telehealth] will not help them.]. Sofia, the mother of a child with rare genetic syndrome, also reported: “It is hard to develop rapport…a relationship over the phone…it is not the same [compared with in-person therapy].” Alice, the mother with a child with ASD, reported: “…there needs to be the opportunity for them [therapists] to build that relationship [with the child].” On the questionnaire, the majority of participants indicated that they would not be interested in their child receiving EI via telehealth because they believed that their children needed “in person interaction with therapists”.
Children Get Distracted Easily or Lack Attention
Many participants reported that their children would not respond positively to an electronic device used in telehealth. Nancy, the mother of a child with ASD, reported: “He would be trying to find a way to shut that [electronic device] off to go to a Thomas [the train] video.” In contrast, some participants reported that their child was disinterested in technology. For example, Daisy, the single mother of a child with speech delays who lived in rural area reported that she can picture her child “running around” and “chasing after him with a camera, with her phone” within a telehealth session.
Ability to Meet the family’s Needs
Parents Lack Confidence to Implement Strategies
Some participants reported that they do not have the needed expertise and capacity to support their child’s learning via telehealth. They reported feeling uncomfortable implementing EI strategies without the physical presence of therapists. Jessica, the mother of a child with cerebal palsy, reported: “I am not trained to do that…like the Yoga ball, I don’t know how to hold them or do that without their [therapists’] help.” In a suburban focus group, parents of children with physical disabilities reported that they could not learn how to address their children’s physical needs without a therapist physically present:
Ella, the mother of a child with developmental delays: I don’t think they [therapists] could tell me how to do it [therapy] the way that they [therapists] do it.
Ellen, the mother of a child with muscular astrophy: That is my struggle too. I can’t hold her. the way you [the therapist] physically hold her to do stuff…we are not looking at the same thing…I don’t understand all the connection.
Family Perceptions of Needed Logistical Items for Telehealth in EI
Participants voiced concerns about logistical barriers to implementing EI. Specifically, they reported needing access to: high-speed internet and unlimited data, electronic devices, and materials.
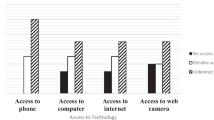
Access to the High-Speed Internet and Unlimited Data Plan
As indicated on the questionnaire, some participants did not have access to the internet (27%, n = 10). Further, some participants (14%, n = 5) reported lacking fast and reliable internet access. In the focus groups, several participants reported that they lacked the internet capability to support telehealth. Nina, the Spanish-speaking mother with low socioeconomic status (SES) staus who has a child of speech delays, reported: “Esperese que tenga internet rápido. Yo tengo el barato. Cuesta un poco tener eso. [Wait until I have fast internet. I have the cheap one. It costs a bit to have that].” Sofia, the mother of a child with rare genetic syndrome questioned: “I think in rural areas…do they have internet access with that kind of bandwidth?” Nancy, the mother of a child with ASD, reported: “You have to have that capability with high-speed internet…We can’t even keep our direct TV hooked up to the wire to the internet because our internet goes down so much.”
Access to Electronic Devices
As reflected on the questionnaire, some participants did not have access to a computer or laptop (32%, n = 12). Several participants reported being unable to afford the equipment needed for telehealth (e.g., computer, webcam). Daisy, the single mother of a child with speech delays who lived in rural area, reported: “I don’t have a computer and I can’t afford it.” Ella, the mother of a child with developmental delays reported: “What if they [parents] have an old laptop [and] it doesn’t have a webcam. Are they going to issue somebody with their own device?”. Also on the questionnaire, several participants indicated that they had no or limited ability to use the computer. For example, Ximena, a Spanish-speaking mother with a child of speech delays, reported that she had limited ability to use computer or laptop wrote: “esta muy bonito el laptop, pero, ¿si yo no lo se prender? [The laptop is very nice, but [what happens] if I do not know how to turn it on]?”
Access to Materials
Many participants reported the importance of the toys and materials which therapists bring for in-person EI sessions. They questioned how telehealth can similarly provide access to toys and materials. Mandy, the mother of a child with ASD, reported:
I am thinking about OT. I have to go get all these stuff for fine motor things to make sure that I have all the resource in my home to do the telehealth. And there is a financial. burden there to get those components.
In a Spanish-speaking focus group, Andres, the father of a child with ASD, said:
Y si yo no tengo el dinero para que la terapeuta me diga, este juguete necesitas, y si yo no tengo dinero para comprar un juguete. ..Como lo voy hacer yo en mi casa se ella los tiene muy aguardados de atrás de la computadora? [And if I do not have the money for the therapist to tell me that you need this toy and if I do not have the money to buy a toy…How will I do it [telehealth] in my house if she [the therapist] has them [the toys] behind the computer?].
Kate, the mother of a child with speech delays, reported:
Like OT, there is so many things they have there that I don’t have at home. If they do something like that (telehealth), they have to tell you to purchase this…. but you don’t have that funding to pay for all the same things they have. It will be a struggle.
Similarly, Nina, the Spanish-speaking mother with low SES staus who has a child of speech delays, reported:
La mayoría de las terapias son—no hablan español. Llevan interprete. ¿Como allí sería el caso? ¿Como se podría entender uno con ellas si esta uno por pantalla? Ósea, no hay servicio de interpretación allí. [Most therapists are-- do not speak Spanish. They carry an interpreter. How would that be in this case [telehealth]? How could one understand them [therapists] if one is on the screen? There is no interpretation service there].
Discussion
In this study, participants were reluctant to use telehealth in EI and preferred in-person visits. Considering the multiple potential benefits of telehealth (Cason et al., 2012; Cole et al., 2019), it is surprising that families had strong reservations about telehealth. Possible explanations for the concerns about telehealth could be misconceptions about the mission and purpose of EI and systemic barriers to accessing telehealth technology and materials. Regarding the former, EI services are designed to promote both child and family outcomes (Division for Early Childhood of the Council for Exceptional Children, 2014). However, many EI providers may feel uncomfortable engaging families in the EI processs; such reluctance may result in parents viewing EI services as child-centered instead of family-centered (McWilliam, 2010; Swafford et al., 2015). Without experiencing family-centered practices and understanding the overarching purpose of EI, it may be hard to attain buy-in from families about using telehealth in EI. With respect to the latter, there are many ways telehealth can be offered ranging from therapists coaching parents to therapists directly interacting with the children (Ashburner et al., 2016; Ekberg et al., 2019). By offering materials explaining the purpose of EI and educating parents about the various methods of telehealth, it may be possible to address this perception.
Participants reported that telehealth could be a great tool to increase timely EI services for underserved families, especially families who were waiting for services. Research has suggested that families who are in need of EI services (e.g., underserved families) may be more responsive to telehealth (Dunkley et al., 2010). However, we found that two barriers could reduce buy-in from families. First, technological difficulties concerned families (Cason et al., 2012; Cole et al., 2019; McCarthy et al., 2019). Rural families are less likely to have access to high-speed internet, and low-income families may not have the needed technology for telehealth (Rideout & Katz, 2016). Regarding the latter, even if families rely on their smartphones to use telehealth, they may not be able to afford the corresponding dataplan. However, ultimately, the cost of such technology and corresponding training may be offset by the availability of high-qualified EI professionals via telehealth (Cason, 2009).
Second, according to parents in the study, the lack of access to therapeutic materials (e.g., toys, sensory integration tools) is another perceived barrier to telehealth (Ashburner et al., 2016; Fairweather et al., 2016; Fitton et al., 2017). Since infants and toddlers spend more time interacting with their parents (than their EI providers), it is critical that providers enhance parents’ capacities to promote their children’s development through natural learning opportunities (e.g., using the toys/materials in the home, McWilliam, 2010). However, EI providers often bring their own toys and learning materials into families’ homes for sessions (Nwokah et al., 2013). Misconceptions about EI services may reflect a larger systemic issue related to professional practice. To dispel this misconception and increase family buy-in for telehealth, it is important to provide materials about the benefits of family-centered, capacity building services and supports within the context of families’ natural environments.
In addition to natural learning opportunities, active parent participation is another critical component of EI. Participants were interested in receiving more support and education from providers. They emphasized that telehealth could be a supplement for parent training. Indeed, research has suggested that technology can facilitate parent training in EI strategies (Vismara et al., 2013). Recently, researchers have proposed the use of hybrid models, wherein families learn to use strategies to support their children’s target skills synchronously and asynchronously (Baharav & Reiser, 2010; Wainer & Ingersoll, 2015). Future research should examine families perceptions about such hybrid telehealth models.
Limitations
There are a few limitations worth consideration. First, the participants were from one Midwestern state, comprised mostly of White parents from urban or suburban areas. Additionally, most of the participants had incomes over $75,000. Families from different ethnic backgrounds, lower SES, or different states may have unique perceptions about using telehealth in EI. Especially given that using telehealth in EI may be most needed for underserved families (Cason, 2009), the findings may have limited transferability. Second, in one rural focus group, only one participant attended the group. Although the group size was not optimal, given the importance of soliciting feedback from underserved (e.g., rural) families, we conducted the focus group protocol with the participant. Third, the participants were limited to families. More diverse perspectives from different stakeholders (i.e., therapists, service coordinators) may provide a more holistic understanding of perspectives toward telehealth in EI.
Finally, individual demographic differences (e.g., socioeconomic background) and child needs (e.g, support needs of the children with disabilities) may impact the findings. As the first study investigating families’ perceptions toward using telehealth in EI, by having heterogenous focus groups with families of different backgrounds, we believe the diverse participants sparked more ideas and conversation about telehealth. However, future research may more closely examine how themes may differ in relaton to family background and child needs.
Directions for Future Research
Future research should develop and test interventions to support families in using telehealth in EI. Such interventions may include parent training or reading materials about telehealth in EI. Such interventions should be developed and tested with respect to: effectiveness (e.g., do families feel more comfortable with telehealth in EI after completing the intervention?), technological literacy (e.g., is the intervention accessible to families with various comfort levels with technology?), and accessibility (e.g., can the intervention be made available to all families regardless of language spoken and geographic location?). Research should especially address whether such interventions help overcome barriers for low-income (Pickard & Ingersoll, 2016), rural (Barr et al., 2019), and minority (Williams et al., 2013) families.
Research is especially needed with respect to underserved families to better explore the use of telehealth in EI. Given the EI service disparities among underserved families (Wise et al., 2010), it is critical to understand their perspectives toward telehealth. Aligned with social-cultural capital theory (Bourdieu, 1986), we found that underserved families faced systemic barriers in accessing capital to use telehealth. To address such disparities, offline apps (Hurwitz et al., 2015) or hotspots for stable internet connections (Cole et al., 2016) may be used to increase capital among these families and ensure their access to EI via telehealth. Notably, it is important to understand how underserved families perceive these potential solutions.
Implications for Practice
Several states have shown an interest in implementing telehealth in EI (Cason et al., 2012). Since telehealth is still an emerging approach for EI, it is critical to consider parents’ concerns about telehealth and dispel myths about telehealth in EI. To this end, we propose that, before implementing telehealth in EI, providers offer training, develop family-friendly materials, and provide technical assistance to families about telehealth in EI. Specfically, practitioners should tailor their practices and resources depending on the family’s experience with telehealth. For example, practitioners may create a website, module or pamphlet explaining how telehealth could be used in EI. Specifically, the materials could emphasize the potential advantages of EI (e.g., meeting underserved families) as well as address potential concerns related to telehealth (e.g., how will technology be provided?). Regarding the latter, for example, practitioners can disscuss with families the importane of a family-centered, strength-based approach (i.e., bagless therapy) to promote parents’ capacities to support their child’s development (Williams & Ostrosky, 2019).
References
Ashburner, J., Vickerstaff, S., Beetge, J., & Copley, J. (2016). Remote versus face-to-face delivery of early intervention programs for children with autism spectrum disorders: Perceptions of rural families and service providers. Research in Autism Spectrum Disorders, 23, 1–14. https://doi.org/10.1016/j.rasd.2015.11.011.
Baharav, E., & Reiser, C. (2010). Using telepractice in parent training in early autism. Telemedicine and E-Health, 16(6), 727–731. https://doi.org/10.1089/tmj.2010.0029.
Barr, M., Dally, K., & Duncan, J. (2019). Service accessibility for children with hearing loss in rural areas of the United States and Canada. International Journal of Pediatric Otorhinolaryngology, 123, 15–21. https://doi.org/10.1016/j.ijporl.2019.04.028.
Brantlinger, E., Jimenez, R., Klingner, J., Pugach, M., & Richardson, V. (2005). Qualitative studies in special education. Exceptional Children, 71(2), 195–207. https://doi.org/10.1177/001440290507100205.
Behl, D. D., Blaiser, K., Cook, G., Barrett, T., Callow-Heusser, C., Brooks, B. M., et al. (2017). A multisite study evaluating the benefits of early. Intervention via telepractice: Infants & Young Children, 30(2), 147–161. https://doi.org/10.1097/IYC.0000000000000090.
Blaiser, K. M., Behl, D., Callow-Heusser, C., & White, K. R. (2013). Measuring costs and outcomes of tele-intervention when serving families of children who are deaf/hard-of-hearing. International Journal of Telerehabilitation, 5(2), 3–10. https://doi.org/10.5195/ijt.2013.6129.
Bourdieu, P. (1986). The forms of capital. In J. G. Richardson (Ed.), Handbook of theory and research for the sociology of education (pp. 241–258). New York, NY: Greenwood.
Brislin, R. W. (1970). Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology, 1(3), 185–216. https://doi.org/10.1177/135910457000100301.
Cason, J. (2009). A pilot telerehabilitation program: Delivering early intervention services to rural families. International Journal of Telerehabilitation, 1, 29–38.
Cason, J., Behl, D., & Ringwalt, S. (2012). Overview of states’ use of telehealth for the delivery of early intervention (IDEA part C) services. International Journal of Telerehabilitation, 4(2), 39–46. https://doi.org/10.5195/IJT.2012.6105.
Cason, J., Hartmann, K., Jacobs, K., & Richmond, T. (2018). Telehealth in occupational therapy. The American Journal of Occupational Therapy, 72, 1–18 Retrieved from http://libproxy.lib.unc.edu/login?url=https://search.proquest.com/docview/2193509193?accountid=14244.
Cole, B., Pickard, K., & Stredler-Brown, A. (2019). Report on the use of telehealth in early intervention in Colorado: Strengths and challenges with telehealth as a service delivery method. International Journal of Telerehabilitation, 11(1), 33–40. https://doi.org/10.5195/ijt.2019.6273.
Cole, B., Stredler-Brown, A., Cohill, B., Baliser, K., Behl, D., & Ringwalt, S. (2016). The development of statewide policies and procedures to implement telehealth for part C service delivery. International Journal of Telerehabilitation, 8(2), 77–82. https://doi.org/10.5195/ijt.2016.6206.
Division for Early Childhood of the Council for Exceptional Children. (2014). Official DEC recommended practices, 2014 Retrieved from https://divisionearlychildhood.egnyte.com/dl/tgv6GUXhVo.
Dunkley, C., Pattie, L., Wilson, L., & McAllister, L. (2010). A comparison of rural speech-language pathologists’ and residents’ access to and attitudes towards the use of technology for speech-language pathology service delivery. International Journal of Speech-Language Pathology, 12(4), 333–343. https://doi.org/10.3109/17549500903456607.
Ekberg, S., Danby, S., Theobald, M., Fisher, B., & Wyeth, P. (2019). Using physical objects with young children in "face-to-face" and telehealth speech and language therapy. Disability and Rehabilitation, 41(14), 1664–1675. https://doi.org/10.1080/09638288.2018.1448464.
Fairweather, G. C., Lincoln, M. A., & Ramsden, R. (2016). Speech-language pathology teletherapy in rural and remote educational settings: Decreasing service inequities. International Journal of Speech-Language Pathology, 18(6), 592–602. https://doi.org/10.3109/17549507.2016.1143973.
Fitton, L., Bustamante, Kristina, N., & Wood, C. (2017). The social validity of telepractice among spanish-speaking caregivers of english learners: An examination of moderators. International Journal of Telerehabilitation, 9(2), 13–24. https://doi.org/10.5195/ijt.2017.6227.
Ferguson, J., Craig, E. A., & Dounavi, K. (2019). Telehealth as a model for providing behaviour analytic interventions to individuals with autism spectrum disorder: A systematic review. Journal of Autism and Developmental Disorders, 49, 582–616. https://doi.org/10.1007/s10803-018-3724-5.
Fuller, E. A., & Kaiser, A. P. (2019). The effects of early intervention on social communication outcomes for children with autism spectrum disorder: A meta-analysis. Journal of Autism and Developmental Disorders., 1–18. https://doi.org/10.1007/s10803-019-03927-z.
Glaser, B. G., & Strauss, A. L. (2017). Discovery of grounded. Theory: Strategies for Qualitative Research. https://doi.org/10.4324/9780203793206.
Guba, E. G., Lincoln, Y. S. (1989). Fourth generation evaluation. Newbury Park, CA: Sage.
Harry, B. (2008). Collaboration with culturally and linguistically diverse families: Ideal versus reality. Exceptional Children, 74, 372–388. https://doi.org/10.1177/001440290807400306.
Hurwitz, L. B., Lauricella, A. R., Hanson, A., Raden, A., & Wartella, E. (2015). Supporting head start parents: Impact of a text message intervention on parent–child activity engagement. Early Child Development and Care, 185(9), 1373–1389. https://doi.org/10.1080/03004430.2014.996217.
Iacono, T., Dissanayake, C., Trembath, D., Hudry, K., Erickson, S., & Spong, J. (2016). Family and practitioner perspectives on telehealth for services to young children with autism. Studies in Health Technology and Informatics, 231, 63–73. Individuals With Disabilities Education Act. , Pub. L. No. 20 U.S.C. § 1400 (2004).
Kelso, G. L., Fiechtl, B. J., Olsen, S. T., & Rule, S. (2009). The feasibility of virtual home visits to provide early intervention: A pilot study. Infants and Young Children, 22(4), 332–340.
Krueger, R. A., & Casey, M. A. (2000). Focus groups: A practical guide for applied researchers (3rd ed.). Thousand Oaks, CA: Sage.
McCarthy, M., Leigh, G., & Arthur-Kelly, M. (2019). Telepractice delivery of family-centred early intervention for children who are deaf or hard of hearing: A scoping review. Journal of Telemedicine and Telecare, 25(4), 249–260. https://doi.org/10.1177/1357633X18755883.
McWilliam, R. A. (2010). Routines-based early intervention: Supporting young children and their families. Baltimore, MD: Brookes.
Moffatt, J. J., & Eley, D. S. (2010). The reported benefits of telehealth for rural Australians. Australian Health Review: A Publication of the Australian Hospital Association, 34(3), 276–281. https://doi.org/10.1071/AH09794.
Noyes-Grosser, D., Elbaum, B., Wu, Y., Siegenthaler, K., Cavalari, R., Gillis, J., & Romanczyk, R. (2018). Early intervention outcomes for toddlers with autism spectrum disorder and their families. Infants & Young Children, 31(3), 177–199. https://doi.org/10.1097/IYC.0000000000000121.
Nwokah, E., Hsu, H. C., & Gulker, H. (2013). The use of play materials in early intervention: The dilemma of poverty. American Journal of Play, 5(2), 187–218.
Onwuegbuzie, A. J., & Leech, N. L. (2007). Sampling designs in qualitative research: Making the sampling process more public. The Qualitative Report, 12, 238–254.
Orinstein, A. J., Helt, M., Troyb, K. E., Barton, M. L., Eigsti, I. M., Naigles, L., & Fein, D. A. (2014). Intervention for optimal outcome in chidlren and adolescents with a history of autism. Journal of Developmental and Behavioral Pediatrics, 35, 247–256.
Patton, M. Q. (2002). Qualitative Research & Evaluation Methods. Retrieved from https://us.sagepub.com/en-us/nam/qualitative-research-evaluation-methods/book232962
Pickard, K. E., & Ingersoll, B. R. (2016). Quality versus quantity: The role of socioeconomic status on parent-reported service knowledge, service use, unmet service needs, and barriers to service use. Autism, 20(1), 106–115. https://doi.org/10.1177/1362361315569745.
Solomon, M., Pistrang, N., & Barker, C. (2001). The benefits of mutual support groups for parents of children with disabilities. American Journal of Community Psychology, 29, 113–132. https://doi.org/10.1023/A:1005253514140.
Swafford, M. D., Wingate, K. O., Zagumny, L., & Richey, D. (2015). Families living in poverty: Perceptions of family-centered practices. Journal of Early Intervention, 37(2), 138–154. https://doi.org/10.1177/1053815115602880.
Tesch, R. (1990). Qualitative. Research: Analysis Types and Software. https://doi.org/10.4324/9781315067339.
Rideout, V., & Katz, V.S. (2016). Opportunity for All? Technology and Learning in Lower-income families. New York: The Joan Ganz Cooney Center at Sesame Workshop.
Vismara, L. A., McCormick, C., Young, G. S., Nadhan, A., & Monlux, K. (2013). Preliminary findings of a telehealth approach to parent training in autism. Journal of Autism and Developmental Disorders, 43, 2953–2969. https://doi.org/10.1007/s10803-013-1841-8.
Wainer, A. L., & Ingersoll, B. R. (2015). Increasing access to an asd imitation intervention via a telehealth parent training program. Journal of Autism and Developmental Disorders, 45(12), 3877–3890. https://doi.org/10.1007/s10803-014-2186-7.
Wallisch, A., Little, L., Pope, E., & Dunn, W. (2019). Parent perspectives of an occupational therapy telehealth intervention. International Journal of Telerehabilitation, 11(1), 15–22. https://doi.org/10.5195/ijt.2019.6274.
Williams, C. S., & Ostrosky, M. M. (2019). What about MY TOYS? Common questions about using a bagless approach in early intervention. Young Exceptional Children, 1096250619829739. https://doi.org/10.1177/1096250619829739.
Williams, M. E., Perrigo, J. L., Banda, T. Y., Matic, T., & Goldfarb, F. D. (2013). Barriers to accessing services for young children. Journal of Early Intervention, 35(1), 61–74. https://doi.org/10.1177/1053815113507111.
Wise, M. D., Little, A. A., Holliman, J. B., Wise, P. H., & Wang, C. J. (2010). Can state early intervention programs meet the increased demand of children suspected of having autism spectrum disorders? Journal of Developmental and Behavioral Pediatrics: JDBP, 31(6), 469–476. https://doi.org/10.1097/DBP.0b013e3181e56db2.
Yosso, T. J. (2005). Whose culture has capital? A critical race theory discussion of community cultural wealth. Race, Ethnicity, and Education, 8, 69–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/ or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, H.W., Burke, M., Isaacs, S. et al. Family Perspectives toward Using Telehealth in Early Intervention. J Dev Phys Disabil 33, 197–216 (2021). https://doi.org/10.1007/s10882-020-09744-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10882-020-09744-y