Abstract
Many children with cancer are diagnosed during infancy and toddlerhood (< 3 years of age), potentially resulting in disrupted and/or missed developmental opportunities. Our objective was to describe the functioning of infants and toddlers with cancer who were clinically referred for evaluation at a hospital-based psychology clinic. Data from 29 very young children with cancer (Mage = 23.62 ± 6.6 months; 55.2% male) who completed clinically referred assessments from 2010 to 2015 were abstracted. Children were 11.3 months post-diagnosis (SD = 7.77, range 1–29 months) with just over half off-therapy at the time of assessment (55.2%). Overall, developmental functioning was significantly below expectations [t(22) = − 8.99, p < .001]. Adaptive functioning [t(25) = − 6.41, p < .001] was also significantly below expectations. Infants and toddlers with cancer appear to be at significant risk for weaknesses in early cognitive and adaptive functioning. The margin of deficits found in this study warrant the need for further investigation and consideration of this young population to ensure optimal functional development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Infancy and toddlerhood mark the most dramatic developmental changes during the human lifespan, concurrent with a time of significant brain development (Casey, Giedd, & Thomas, 2000; Jernigan, Baaré, Stiles, & Madsen, 2011; Stiles, 2008). Specifically, very young children rapidly acquire skills across cognitive, adaptive, and psychosocial domains. To achieve optimal development, infants and toddlers require predictability, consistency, reciprocal interactions, warmth, perceived security, and opportunities to explore and experiment within their environment (National Research Council and Institute of Medicine, 2000). Recent advances in neuroscience have increased understanding of the pivotal role of early social interactions in brain development (Meltzoff & Kuhl, 2016). Interruption and insult during this critical period, such as a cancer diagnosis and required treatments, have the potential to result in significant and long-lasting effects (Anderson & Kunin-Batson, 2009; Olsson, Perrin, Lundgren, Hjorth, & Johanson, 2014).
Almost half of children with cancer are diagnosed and treated during infancy and toddlerhood (Siegel, Miller, & Jemal, 2015; Ward, DeSantis, Robbins, Kohler, & Jemal, 2014). As such, the ongoing development of these very young children may be disrupted due to a number of factors, including prolonged stays in the hospital, medical procedures, and removal from typical routines. This disruption may have the consequence of diminishing those essential needs for social interaction, exploration, and predictability which may negatively impact later development (see Harman, Wise, & Willard, 2018 for a review). Fortunately, advances in treatment have dramatically increased the survival rates of children with cancer over the past few decades (Abdullah, Qaddoumi, & Bouffet, 2008). Subsequently, there has been an increased awareness of the need to understand the impact of treatment and diagnosis on the social, emotional, behavioral, and overall developmental functioning of children with cancer.
Very young age at diagnosis is typically considered a significant risk factor for development of later adverse problems (Mulhern et al., 2001). This is particularly true for neurocognitive late effects in children with diseases and treatments that affect the central nervous system (CNS; e.g., brain tumors, acute leukemias) (Moleski, 2000; Mulhern, Merchant, Gajjar, Reddick, & Kun, 2004). Despite these risks, there is a paucity of literature on the cognitive and psychosocial functioning of infants and toddlers treated for cancer. Existing research has focused mainly on the potential for preserving neurocognitive functioning of young children under the age of three through the avoidance of cranial radiation therapy (Dhall et al., 2008; Lafay-Cousin et al., 2009). Limited work has also focused on the functional outcome of young children treated for brain tumors. Specifically, Stargatt et al. (2006) investigated the cognitive and adaptive development of children diagnosed with brain tumors during infancy and found delays in multiple domains of adaptive function at diagnosis along with cognitive deficits during follow-up. Similarly, Bornstein et al. (2012) prospectively studied the neurodevelopment of very young children with non-CNS-affecting cancers (i.e., retinoblastoma, neuroblastoma, acute leukemia) and found deficits within motor, mental, and language skills compared to healthy controls. Several recent papers (Fay-McClymont et al., 2017; Willard, Leung, Huang, Zhang, & Phipps, 2014; Willard, Qaddoumi, et al., 2014) have also highlighted the potential vulnerabilities of this age range for deficits or declines in cognitive and adaptive functioning across diverse cancer types (CNS and non-CNS impacting). Despite the salient findings of these few studies providing evidence that very young children are at risk, there is still very limited research regarding the developmental outcomes of this population. Subsequently, there is a critical need for a more explicit focus across domains.
Given the critical nature of infancy and toddlerhood on later development and the limited cancer-specific research on patients in this age range, the objective of this paper was to characterize the cognitive and adaptive functioning of very young children (under the age of 3 years) treated for cancer. Using a clinical sample of children evaluated within a hospital-based psychology clinic, we hypothesized that those patients with CNS-affecting diagnoses (e.g., brain tumors) would demonstrate greater deficits in functioning across domains, though we also expected that most children assessed would demonstrate weaknesses in at least some domains of developmental functioning.
Methods
Procedures
Psychological assessment data of infants and toddlers with cancer were retrospectively abstracted from the medical records of a pediatric-focused cancer institution. All participants completed a clinically referred assessment in the hospital-based psychology clinic between 2010 and 2015. Participants were eligible for this study if they were under the age of 3 years at the time of assessment and diagnosed with a malignancy. Institutional Review Board approval was obtained prior to data abstraction. Thirty-two children under 3 years of age were assessed in the clinic during this timeframe; three had a diagnosis of non-malignancy and were excluded. As such, a final sample of 29 infants and toddlers met inclusion criteria for this study.
Data abstracted from the medical charts included demographic (e.g., age, race, gender) and medical (e.g., diagnosis, treatment) information. The psychological assessment data included measures of early cognitive and adaptive functioning. As all data were clinically collected, the present study was limited to the measures chosen by individual clinicians, rather than a standard battery. Nineteen children (65.5%) were administered measures in both domains. Assessment data were collapsed and combined across similar measures and domains when possible (see “Measures” below).
The sample for this study included 29 very young children under the age of 36 months (M = 23.62 ± 6.6 months, 8–34 months). The majority of patients were male (n = 16, 55.2%) and white (n = 20, 69.0%). All primary diagnostic categories were represented, including solid tumors (n = 15, 51.7%), brain tumors (n = 9, 31.0%), and leukemias (n = 5, 17.2%). Just over half of patients were off-therapy at the time of assessment (n = 16, 55.2%), and a mean of 11.34 months since diagnosis (median = 9.0 months, SD = 7.77, 1–29 months). Treatment plans varied with a majority of patients receiving chemotherapy (n = 21, 72.4%). Notable was one patient with a premorbid diagnosis of Down syndrome and another with 13q deletion syndrome, both of which are associated with developmental and learning difficulties (Baud et al., 1999; Grieco, Pulsifer, Seligsohn, Skotko, & Schwartz, 2015). About a third of patients (n = 9, 31.0%) received a psychological diagnosis (e.g., Expressive Language Disorder, Cognitive Disorder Not Otherwise Specified, Mixed Development Disorder) as a result of their assessment. See Table 1 for more detailed demographic and treatment information.
Measures
Early Cognitive Functioning
Two measures were utilized by clinicians to assess early cognitive functioning, with 23 (79.3%) patients administered such a measure during their evaluation. Most patients were administered the Mullen Scales of Early Learning (n = 15; Mullen, 1995) with the remaining administered the Bayley Scales of Infant and Toddler Development, Second Edition (n = 8; Bayley, 1993). For analytical purposes, the primary indices of interest that were collapsed across measures included Cognitive Composite, Gross Motor, Fine Motor, Expressive Language, and Receptive Language. The Cognitive Composite for both measures is presented as a Standard Score (M = 100, SD = 15). Scores for the other subscales—initially presented as T scores or scaled scores—were converted to T scores (M = 50, SD = 10) (if necessary) for ease of interpretation and comparison purposes.
Adaptive Functioning
Adaptive functioning was assessed via the parent-reported versions of the Vineland Adaptive Behavior Scales, Second Edition (VABS-2; Sparrow, Cicchetti, & Balla, 2005) and the Adaptive Behavior Assessment System, Second Edition (ABAS-2; Harrison & Oakland, 2003). Most patients (n = 21, 72.4%) completed an adaptive measure as part of their battery (48.3% ABAS-2). Similar scores across these two measures included an overall Adaptive Functioning Composite as well as indicators of Socialization, Communication, Daily Living, and Motor Skills. Given differences in standardized scores available for these two measures (v-scale scores vs. scaled/standard scores), all scores were converted to standard scores (M = 100, SD = 15) for ease of interpretation and in order to collapse and compare across domains/measures.
Analytical Plan
Descriptive statistics were used to characterize the sample for each domain including mean, standard deviation, and percentage in the at-risk or clinically significant range, which were operationalized as one and two standard deviations below the normative mean. The mean scores for participant functioning in each domain were compared to the published normative mean for each measure using one-sample t tests. Analysis of variance (ANOVA) was used to examine differences in functioning based on clinically relevant risk factors: diagnostic category (brain tumor versus solid tumor) and treatment status (on-therapy versus off-therapy), gender, and whether a psychological diagnosis was assigned, deferred, or not given.
Results
Descriptive Analyses
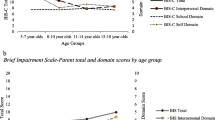
One-sample t tests and mean scores for all domains are available in Table 2 (cognitive functioning) and Table 3 (parent-reported adaptive functioning). All developmental domains were significantly below the normative mean. For the cognitive composite, a majority of patients achieved scores that fell one or two standard deviations below the mean (47.9% and 30.4%, respectively) with average scores significantly below normative expectations [M = 77.30, SD = 12.11, t(22) = − 8.99, p < .001]. A majority of patients (82.6%) achieved scores in the extremely low to low average range with no patients in the high average to superior ranges (Fig. 1). For all domains of cognitive functioning, more patients than would be expected fell one and/or two standard deviations below the normative mean (20.8–47.9% and 25–50%, respectively).
Overall, parent-reported adaptive functioning scores were also lower than would be expected (Table 3, Fig. 1). For all domains of adaptive functioning, more patients than would be expected fell one and/or two standard deviations below the normative mean (9.5–44.5% and 19.0–30.8%, respectively). The average overall adaptive functioning composite score was significantly below normative expectations [M = 79.46, SD = 16.34, t(25) = − 6.41, p < .001]. Scores were also significantly below normative expectations for the social, daily living, communication, and motor skills composites (Table 3).
Predictors of Functioning
Analyses were completed to compare patients based on diagnostic category and treatment status on the cognitive and adaptive composites. Results revealed a statistically significant difference in the cognitive composite based on diagnostic category [F(1, 18) = 7.07, p = .016]. Patients with brain tumors demonstrated mean scores 12.65 points lower than those with solid tumors (brain tumor M = 70.44, SD = 10.19, solid tumor M = 83.09, SD = 10.88). There was not a statistically significant difference in parent-reported adaptive functioning based on diagnostic category [F(1, 19) = 1.85, p = .19; brain tumor M = 73.0, SD = 15.91, solid tumor M = 83.08, SD = 17.47]. Further, there were no significant differences for cognitive [F(1, 21) = 0.01; on-therapy M = 79.56, SD = 14.86; off-therapy M = 75.86, SD = 10.32] or adaptive functioning [F(1, 24)) = 0.50; on-therapy M = 79.08, SD = 15.03; off-therapy M = 79.79, SD = 17.94] based on treatment status (on versus off) at the time of assessment.
Results revealed no differences in functioning based on gender [Cognitive: F(1, 21) = 1.12; adaptive: F(1, 24) = 0.55]. In contrast, there was a significant difference between groups based on if a diagnosis was assigned, deferred, or not given following the evaluation for overall adaptive functioning [F(2, 23) = 4.92, p < .02]. Specifically, those patients who did not receive a psychological diagnosis following assessment had adaptive scores within the Average range (M = 90.30), which were higher than those who did receive a diagnosis (M = 70.0, Borderline range) and those where a diagnosis was deferred (M = 74.78, Borderline/delayed range). In contrast, there was not a significant difference between groups based on psychological diagnosis for early cognitive functioning [F(2, 20) = 1.50].
Discussion
The objective of the current study was to characterize the early cognitive and adaptive functioning of clinically referred infants and toddlers diagnosed with cancer. The vast majority of our sample demonstrated clinically significant impairments in cognitive functioning. Indeed, almost all patients in our sample exhibited below average cognitive functioning, with none exceeding the average range. Consistent with this finding, a majority of our sample demonstrated significant impairments in adaptive functioning as well. Functioning within overall cognitive and adaptive domains exhibited little variance irrespective of diagnostic category, treatment status or gender, though patients with brain tumors demonstrated significantly lower cognitive functioning as compared to patients with solid tumors. While our sample was potentially biased by clinical referral, ultimately, results suggest that infants and toddlers treated for cancer—irrespective of known risk factors—potentially represent a population that is at risk for cognitive and adaptive delays.
In contrast with expectations based on extant literature (Mulhern & Butler, 2004; Stargatt et al., 2006), infants and toddlers with brain tumors did not consistently demonstrate more adaptive difficulties than infants and toddlers with non-CNS diagnoses (i.e., solid tumor). However, these findings are in keeping with more recent research that has demonstrated cognitive and adaptive deficits in young children and toddlers treated for non-CNS diagnoses (Bornstein et al., 2012; Willard, Leung et al., 2014; Willard, Qaddoumi et al., 2014). In combination, these findings assert the need for additional systematic longitudinal assessment of functioning of young children with cancer, regardless of diagnosis. Certainly these findings are in contrast with studies of older children, and suggest that very young children with cancer may need to be viewed differently than older children. Indeed, given the potential influence of insecure attachment, diminished predictability, and missed developmental opportunities for infants and toddlers who spend their early years undergoing treatment, an increased recognition and focus on infants and toddlers with cancer is critical.
Congruent with a need for further study is a need for early detection of deficits, which is critical for early intervention and prevention efforts. Given the malleability of early development, infants and toddlers may benefit from remediation or prevention of deficit through increased referrals to early intervention services (Guarlnick, 2011; Harman et al., 2018; Hebbeler et al., 2007). Harman et al. (2018) recently highlighted the existing evidence concerning the various developmental risk factors for children with cancer under 3 years of age and the associated long-term sequelae. Given the provided evidence and as experts in their respective fields, it is their recommendation that all infants and toddlers with cancer be systematically referred for Early Intervention services as soon as possible after initial diagnosis. Fortunately, state funding is provided for Early Intervention services for infants and toddlers with developmental delays or those at risk for delays through Part C of the Individuals with Disabilities Education Act (Individuals with Disabilities Education Act, 2004). These services—which often includes rehabilitation services as well as psychological therapies for the child and family—can be implemented within the hospital, community center, or home, depending on the child and family’s need. Further, these early intervention services do not focus solely on the infant/toddler, but rather engage in an efficacious family-centered approach to ensure optimal developmental outcomes (Harman et al., 2018; Hebbeler et al., 2007). Observed weaknesses in gross- and fine-motor skills and receptive and expressive language documented in our sample support the need for rehabilitation services for young children with cancer.
This study has a number of limitations that should be noted. The biggest limitation is the small sample size. Given the methodology of a retrospective chart review, we were constrained by the sample that was assessed during our timeframe. The small sample limited us from examining functioning by history of radiation therapy, or a diagnosis of leukemia. Thus, analyses may be interpreted as pilot data and had a larger sample size been available, the effects may have been more pronounced. Further, our sample was clinically referred. As such, there may be potential bias in regard to the severity of the findings. Referrals to our psychology clinic are frequently made for routine surveillance given the cognitive and adaptive risks for these patients (Bornstein et al., 2012; Fouladi et al., 2005; Stargatt et al., 2006), though a portion of our sample was likely referred due to clinician concern for developmental delays. Regardless, the significance of deficits within our sample—most notably within cognitive functioning—was concerning and warranted report irrespective of this potential bias given how little is known about very young children treated for cancer in the literature. Moreover, our findings are generally consistent with other studies of infants and toddlers with brain tumors and retinoblastoma that were prospectively followed (Fay-McClymont et al., 2017; Fouladi et al., 2005; Sands et al., 2010; Willard, Qaddoumi, et al., 2014). Relatedly, as all data were clinically collected, the present study was limited to those measures that were utilized which required collapsing and combining of scores across measures, thus limiting sample size in some domains. Finally, it is well known that socioeconomic status, environment, and parent factors influence cognitive functioning and developmental outcomes in young children (Kingston, McDonald, Austin, & Tough, 2015; Nagayoshi et al., 2017; Caspi et al., 2016). However, this information was not accessible for our sample as it is not systematically collected during clinical assessments at our institution. Prospective studies should ensure collection of this information to determine if these factors play a moderating role in the cognitive and adaptive functioning of infants and toddlers treated for cancer.
Results of this study demonstrate the potential vulnerability of infants and toddlers’ cognitive and adaptive development when treated for cancer. Children less than 3 years of age who have been treated for cancer are largely understudied, with the results of this study highlighting early indication of cognitive and adaptive function delays. Further, functional weaknesses appear to be present irrespective of the traditional risk factors of diagnosis and treatment status. Consequently, there is a strong need to better understand the developmental trajectory of infants and toddlers treated for cancer—especially those with non-CNS-affecting diagnoses. Future research must prospectively assess these young patients and also seek to intervene in order to promote the best possible developmental outcomes. As such, future studies must have an increased focus on adapting and applying intervention and prevention efforts. Ultimately, further investigation of very young children treated for cancer is critical in order to identify and address these core deficits as early as possible, thereby promoting normalized and positive developmental trajectories of this population.
References
Abdullah, S., Qaddoumi, I., & Bouffet, E. (2008). Advances in the management of pediatric central nervous system tumors. Annals of the New York Academy of Sciences,38, 22–31. https://doi.org/10.1196/annals.1414.005.
Anderson, F. S., & Kunin-Batson, A. S. (2009). Neurocognitive late effects of chemotherapy in children: The past 10 years of research on brain structure and function. Pediatric Blood & Cancer,52, 159–164. https://doi.org/10.1002/pbc.21700.
Baud, O., Cormier-Daire, V., Lyonnet, S., Desjardins, L., Turleau, C., & Doz, F. (1999). Dysmorphic phenotype and neurological impairment in 22 retinoblastoma patients with constitutional cytogenetic 13q deletion. Clinical Genetics,55, 478–482. https://doi.org/10.1034/j.1399-0004.1999.550614.x.
Bayley, N. (1993). Bayley scales of infant development (2nd ed.). San Antonio, TX: The Psychological Corporation.
Bornstein, M. H., Scrimin, S., Putnick, D. L., Capello, F., Haynes, O., Falco, S., … Pillon, M. (2012). Neurodevelopmental functioning in very young children undergoing treatment for non-CNS cancer. Journal of Pediatric Psychology, 37, 660–673. https://doi.org/10.1093/jpepsy/jss003.
Casey, B. J., Geidd, J. N., & Thomas, K. M. (2000). Structural and functional brain development and its relation to cognitive development. Biological Psychology,54, 241–257. https://doi.org/10.1016/S0301-0511(00)00058-2.
Caspi, A., Houts, R. M., Belsky, D. W., Harrington, H., Hogan, S., Ramrakha, S., …, Moffit, T. E. (2016). Childhood forecasting of a small segment of the population with large economic burden. Nature Human Behaviour, 1, 0005. https://doi.org/10.1038/s41562-016-0005.
Dhall, G., Grodman, H., Ji, L., Sands, S., Gardner, S., Dunkel, I. J., …, Finlay, J. L. (2008). Outcome of children less than three years old at diagnosis with non-metastatic medulloblastoma treated with chemotherapy on the “Head Start” I and II protocols. Pediatric Blood & Cancer, 50, 1169–1175. https://doi.org/10.1002/pbc.21525.
Fay-McClymont, T. B., Ploetz, D. M., Mabbott, D., Walsh, K., Smith, A., Chi, S. N., & Lafay-Cousin, L. (2017). Long-term neuropsychological follow-up of young children with medulloblastoma treated with sequential high-dose chemotherapy and irradiation sparing approach. Journal of Neurooncology,133, 119–128. https://doi.org/10.1007/s11060-017-2409-9.
Fouladi, M., Gilger, E., Kocak, M., Wallace, D., Buchanan, G., Reeves, C., & Mulhern, R. (2005). Intellectual and functional outcome of children 3 years old or younger who have CNS malignancies. Journal of Clinical Oncology,23, 7152–7160. https://doi.org/10.1200/JCO.2005.01.214.
Grieco, J., Pulsifer, M., Seligsohn, K., Skotko, B., & Schwartz, A. (2015). Down syndrome: Cognitive and behavioral functioning across the lifespan. American Journal of Medical Genetics Part C (Seminars in Medical Genetics),169, 135–149. https://doi.org/10.1002/ajmg.c.31439.
Guarlnick, M. J. (2011). Why early intervention works: A systems perspective. Infants Young Child,24, 6–28. https://doi.org/10.1097/IYC.0b013e3182002cfe.
Harman, J. L., Wise, J., & Willard, V. W. (2018). Early intervention for infants and toddlers: Applications for pediatric oncology. Pediatric Blood & Cancer,65, e26921. https://doi.org/10.1002/pbc.26921.
Harrison, P., & Oakland, T. (2003). Adaptive behavior assessment system (2nd ed.). San Antonio, TX: The Psychological Corporation.
Hebbeler, K., Spiker, D., Bailey, D., Scarborough, A., Mallik, S., Simeonsson, R., …, Nelson, L. (2007). Early intervention for infants and toddlers with disabilities and their families: Participants, services, and outcomes: Final report of the National Early Intervention Longitudinal Study (NEILS). Menlo Park, CA: SRI International.
Individuals with Disabilities Education Act, 20 S.S.C. § 1400 (2004).
Jernigan, T. L., Baare, W. F. C., Stiles, J., & Madsen, K. S. (2011). Postnatal brain development: Structural imaging of dynamic neurodevelopmental processes. Progress in Brain Research,189, 77–92. https://doi.org/10.1016/B978-0-444-53884-0.00019-1.
Kingston, D., McDonald, S., Austin, M. P., & Tough, S. (2015). Association between prenatal and postnatal psychological distress and toddler cognitive development: A systematic review. PLoS ONE,10(1–16), e0126929. https://doi.org/10.1371/journal.pone.0126929.
Lafay-Cousin, L., Bouffet, E., Hawkins, C., Amid, A., Huang, A., & Mabbott, D. J. (2009). Impact of radiation avoidance on survival and neurocognitive outcome in infant medulloblastoma. Current Oncology,16, 21–28. https://doi.org/10.3747/co.v16i6.435.
Meltzoff, A. N., & Kuhl, P. K. (2016). Exploring the infant social brain: What’s going on in there? Zero to Three,36, 2–9.
Moleski, M. (2000). Neuropsychological, neuroanatomical, and neurophysiological consequences of CNS chemotherapy for acute lymphoblastic leukemia. Archives of Clinical Neuropsychology,15, 603–630. https://doi.org/10.1016/S0887-6177(99)00050-5.
Mulhern, R. K., & Butler, R. W. (2004). Neurocognitive sequelae of childhood cancers and their treatment. Pediatric Rehabilitation,7(1), 1–14. https://doi.org/10.1080/13638490310001655528.
Mulhern, R. K., Merchant, T. E., Gajjar, A., Reddick, W. E., & Kun, L. E. (2004). Late neurocognitive sequelae in survivors of brain tumors in childhood. Lancet Oncology,5, 399–408. https://doi.org/10.1016/S1470-2045(04)01507-4.
Mulhern, R. K., Palmer, S. L., Reddick, W. E., Glass, J. O., Kun, L. E., Taylor, J., …, Gajjar, A. (2001). Risks of young age for selected neurocognitive deficits in medulloblastoma are associated with white matter loss. Journal of Clinical Oncology, 19, 472–479. https://doi.org/10.1200/JCO.2001.19.2.472.
Mullen, E. M. (1995). Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service.
Nagayoshi, M., Hirose, T., Toju, K., Suzuki, S., Okamitsu, M., Teramoto, T., & Takeo, N. (2017). Related visual impairment to mother-infant interaction and development in infants with bilateral retinoblastoma. European Journal of Oncology Nursing,28, 28–34. https://doi.org/10.1016/j.ejon.2017.02.002.
National Research Council, Institute of Medicine. (2000). From neurons to neighborhoods: The science of early childhood development. Washington, DC: National Academy Press.
Olsson, I. T., Perrin, S., Lundgren, J., Hjorth, L., & Johanson, A. (2014). Long-term cognitive sequelae after pediatric brain tumor related to medical risk factors, age, and sex. Pediatric Neurology,51, 515–521. https://doi.org/10.1016/j.pediatrneurol.2014.06.011.
Sands, S. A., Oberg, J. A., Gardner, S. L., Whiteley, J. A., Glade-Bender, J. L., & Finlay, J. L. (2010). Neuropsychological functioning of children treated with intensive chemotherapy followed by myeloablative consolidation chemotherapy and autologous hematopoietic cell rescue for newly diagnosed CNS tumors: An analysis of the head start II survivors. Pediatric Blood & Cancer,54, 429–436. https://doi.org/10.1002/pbc.22318.
Siegel, R. L., Miller, H. D., & Jemal, A. (2015). Cancer statistics, 2015. CA Cancer Journal for Clinicians,65, 5–29. https://doi.org/10.3322/caac.21254.
Sparrow, S. S., Cicchetti, D. V., & Balla, D. A. (2005). Vineland adaptive behavior scales (2nd ed.). San Antonio, TX: Pearson.
Stargatt, R., Rosenfeld, J. V., Anderson, V., Hassall, T., Maixner, W., & Ashley, D. (2006). Intelligence and adaptive function in children diagnosed with brain tumour during infancy. Journal of Neurooncology,80, 295–303. https://doi.org/10.1007/s11060-006-9187-0.
Stiles, J. (2008). The fundamentals of human brain development. Integrating nature and nurture. Cambridge, MA: Harvard University Press.
Ward, E., DeSantis, C., Robbins, A., Kohler, B., & Jemal, A. (2014). Childhood and adolescent cancer statistics. CA Cancer Journal for Clinicians,64, 83–103. https://doi.org/10.3322/caac.21219.
Willard, V. W., Leung, W., Huang, Q., Zhang, H., & Phipps, S. (2014a). Cognitive outcome after pediatric stem-cell transplantation: Impact of age and total-body irradiation. Journal of Clinical Oncology,32, 3982–3988. https://doi.org/10.1200/JCO.2014.56.2223.
Willard, V. W., Qaddoumi, I., Chen, S., Zhang, H., Brennan, R., Rodriguez-Galindo, C., …, Phipps, S. (2014). Developmental and adaptive functioning in children with retinoblastoma: A longitudinal investigation. Journal of Clinical Oncology, 32, 2788–2793. https://doi.org/10.1200/JCO.2013.53.1996.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Ansley E. Kenney, Jennifer L. Harman, Andrew E. Molnar, Jr., Niki Jurbergs, and Victoria W. Willard declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (St Jude Children’s Research Hospital) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kenney, A.E., Harman, J.L., Molnar, A.E. et al. Early Cognitive and Adaptive Functioning of Clinically Referred Infants and Toddlers with Cancer. J Clin Psychol Med Settings 27, 41–47 (2020). https://doi.org/10.1007/s10880-019-09619-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-019-09619-1