Abstract
Residency is a stressful period in a physician’s development, characterized by long work hours, time pressure, and excessive work load, that can exert negative effects on residents’ mental health. Job burnout and negative work–home interference may play a major role in residents’ mental health problems. The present study used the job demands-resources model as a theoretical framework to examine the way in which job demands (e.g., workload, emotional demands) and job resources (e.g., supervisor support, job autonomy) were associated with residents’ mental health. From a pool of 290 medical residents, 264 (91 %) completed the questionnaires. Applying structural equation modeling techniques, the results showed that greater emotional exhaustion (β = −.65, SE = .09, p < .001) and more work–home interference (β = −.26, SE = .10, p < .05) were related to poor mental health. Specific job demands (i.e., high workload) and particular job resources (i.e., low opportunities for professional development and low supervisor support) were related to poor mental health not directly but only indirectly, via emotional exhaustion or work–home interference. Thus, through work-related emotional exhaustion, the impact of work conditions might be transmitted to and interfere with non-work related domains such as family life, as well as with domain-unspecific aspects of well-being, such as mental health and psychological distress. Implications of the results and suggestions for future research and practice are outlined.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Residency is a period in a physician’s development, during which skills in a specialty need to be gained while, simultaneously, high-quality patient care is expected to be provided. In daily practice, the resident is both a trainee and “learner”, and a “professional” and provider of care to patients (Gillespie, Paik, Ark, Zabar, & Kalet, 2009). Medical residency has been characterized as a period of “temporary imbalance,” where residents’ investment in professional growth and development can lead to reprioritization among multiple domains of their life and sacrifices in personal domains, including family, social, physical, mental, spiritual, and financial (Ratanawongsa, Wright, & Carrese, 2007). Universally, residency is associated with high levels of physical and emotional stress (Prins et al., 2007; Thomas, 2004). Factors that may contribute to residents’ job stress include: time demands, time pressure, long work hours, excessive workload, increased responsibility, sleep deprivation, lack of autonomy, lack of control over time, work planning, work organization, interpersonal relationships, as well as intimidation and harassment from members of the healthcare team, and difficulties with work–home balance (Aminazadeh et al., 2012; Cohen & Patten, 2005; IsHak et al., 2009; Lockley et al., 2004; McCray, Cronholm, Bogner, Gallo, & Neill, 2008).
Resident physicians’ high job stress has been associated with reduced patient safety and more self-reported errors, such as later patient discharge due to heavy workload, provision of poor quality of care, and inadequate attention paid to and insufficient time spent for patients (Prins et al., 2009). Moreover, job stressors often exert negative effects on residents’ psychological well-being, making them more susceptible to mental health problems, such as depression (Wang, Sun, Chi, Wu, & Wang, 2010). Thus, medical residents’ job stress and mental health issues might be a matter of concern and motivated the present study, which aims to delineate the factors related to the mental health status of medical residents, especially since very few reports on Greek resident mental health have thus far been published.
Regarding residents’ mental health problems, previous studies have shown that the prevalence of depressive symptoms in residents is around 20 %, depending on the tool used to screen for depression, year of residency, field of residency, and residency program characteristics (Collier, McCue, Markus, & Smith, 2002; Fahrenkopf et al., 2008; Goebert et al., 2009; Lebensohn et al., 2013). Cohen and Patten (2005) recorded that 17 % of Canadian resident physicians rated their mental health as fair or poor, which was more than double the amount reported in the general population. Depressed residents have been found to make significantly more medication errors than their non-depressed peers (Fahrenkopf et al., 2008), while more than 60 % of residents reporting a major medical error in the last three months have been found positive for depression (West et al., 2006). Thus, identifying the factors associated with residents’ mental health problems is a crucially important public health issue.
Contextual and Theoretical Background
Medical education and practical training of Greek medical residents is often unstructured, heterogeneous and informal, and is largely offered by the most experienced senior colleagues. The selection process for entering a residency program is presently exclusively decided by the Greek Ministry of Health in the frame of the National Healthcare System, solely based on waiting lists without any criteria of merit and excellence. The waiting time for a medical school graduate to start specialty training is very long (e.g., up to five years for surgical specialties; Hellenic Quality Assurance and Accreditation Agency, 2010; Kostakis & Mantas, 2008). The organizational difficulties particular to the Greek National Healthcare System (Economou & Giorno, 2009) may result in excessive continuous working hours, increased work stress and time pressures, demanding job conditions in terms of mental effort, role ambiguity and high uncertainty about the future prospects of residents (Msaouel et al., 2010; Panagopoulou, Montgomery, & Benos, 2006). Demanding work conditions may lead medical residents to experience burnout and subsequent mental health problems (Hakanen, Schaufeli, & Ahola, 2008). Burnout has been defined as a psychological syndrome of overwhelming emotional exhaustion, feelings of disinterest, cynicism or depersonalization, and a sense of low personal accomplishment or effectiveness, in response to chronic interpersonal stressors on the job (Maslach, Schaufeli, & Leiter, 2001). Medical residents are especially vulnerable to burnout (Prins et al., 2007, 2010). Burnout prevalence rates among first-year U.S. internal medicine residents have been found to range between 47 and 61 % near the end of internship (Ripp et al., 2011), while 58 % of residents are burned out during their third year (Campbell, Prochazka, Yamashita, & Gopal, 2010). High emotional exhaustion or high depersonalization scores range from 47 to 70 % among surgery residents, even after restriction on and reduction in work hours (Gelfand et al., 2004). Among medical residents in Greece, approximately 57 % have been found to experience high emotional exhaustion, 66.2 % have been found to experience high depersonalization, while 58.5 % reported a sense of reduced personal accomplishment (Msaouel et al., 2010). There has been convincing evidence supporting the positive association between burnout and mental health problems (Hakanen et al., 2008; Hakanen & Schaufeli, 2012).
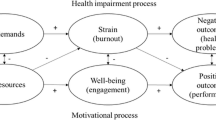
A limitation of previous studies that focused on residents’ job stress is that researchers have not based their hypotheses about mental health problems on strong conceptual frameworks. The current study used the job demands-resources (JD-R) model as a theoretical framework that could take into account possible job demands and job resources in an integral way (Fig. 1; Demerouti & Bakker, 2011). The JD-R model, proposed by Demerouti, Bakker, Nachreiner, and Schaufeli (2001), assumes that health impairments (e.g., burnout) and decreased well-being can develop when job demands are high and job resources are limited, as such negative working conditions can lead to energy depletion and undermine employees’ motivational potential, respectively. Job demands refer to those physical, social, psychological, or organizational aspects of the job that require sustained physical, cognitive, or emotional effort. Examples include work overload, time pressure, and emotional demands. Job resources refer to those aspects of the job that are instrumental to achieve work goals, may reduce job demands and the associated psychological burden, or promote personal growth, learning, and development. Examples include job autonomy, supportive colleagues and supervisor, performance feedback, and opportunities to learn (Demerouti & Bakker, 2011). The JD-R model focuses on subjective perceptions and cognitive appraisals rather than on objective job characteristics that may operate outside the individual’s awareness, because such perceptions may mediate the effects of more objective characteristics on outcomes. The JD-R model does in some aspects resemble the ABCX model of stress and crisis (Hill, 1949; McCubbin & Patterson, 1983), given that the ABCX model places emphasis on stressors (or demands), available resources, appraisal and attribution of meaning to stressors, as well as the interaction among them, in order for disruption and a crisis to be produced.
One important concept that has attracted researchers’ interest and has been studied within the JD-R theoretical framework is negative work–home interference (WHI). Negative work-home interference is defined as a challenge faced by an employee when role pressures and obligations from the work and family domains are mutually incompatible in some respect, where work responsibilities negatively influence family obligations (Greenhaus & Beutell, 1985). Negative WHI has been suggested to be an outcome variable within the JD-R model (Schaufeli & Taris, 2014). Work-family studies have identified work overload as a key antecedent of work–home interference (e.g., van der Heijden, Dillingh, Bakker, & Prins, 2008), while burnout may, over time, negatively spill over to home, leading to an increased sense of being overwhelmed by home demands (Bakker & Demerouti, 2013; ten Brummelhuis & Bakker, 2012). Moreover, negative WHI has been related to serious consequences including depression (Allen, Herst, Bruck, & Sutton, 2000). Bakker, ten Brummelhuis, Prins, and van der Heijden (2011) applied the JD-R model to the work–home interface, using a sample of Dutch medical residents. They found that the combination of high job demands (e.g., work overload, emotional and cognitive demands) and low job resources (e.g., supervisory coaching, opportunities for development) was positively associated with partner ratings of the employee’s negative work–home interference and conflict.
Previous studies have supported the mediating role of both burnout and WHI in the relationship between job demands/resources and mental health. Rantanen, Kinnunen, Feldt, and Pulkkinen (2008) have found spillover relations between domain-specific (e.g., job exhaustion) and general well-being (e.g., psychological distress), while Hakanen et al. (2008) have confirmed the mediated health impairment process leading from job demands through burnout to depression. Additionally, negative work-to-family spillover has been found to mediate the relationship between high work stress and depressive symptomatology (Franche et al., 2006). Similarly, Geurts, Kompier, Roxburgh, and Houtman (2003) found that WHI played a mediating role in the relationship of workload and work conditions to context-free indicators of well-being (e.g., depressive mood and symptoms). The indirect path linking a combination of high job demands and low control to mental health through work-to-family interference has also been verified by Magee, Stefanic, Caputi, and Iverson (2012). According to the conservation of resources theory (COR; Hobfoll, 1989), as a response to chronic stresses, employees may experience burnout, when they suffer an ongoing drain of resources (e.g., social support) and perceive a net loss, which cannot be replenished, of emotional, physical, or cognitive energy that they possess. As more strain is experienced in one domain (e.g., work), fewer resources are available to fulfill one’s role in another domain (e.g., family). Those employees with fewer resources (e.g., less supervisor support) may be more vulnerable to resource loss and less capable of resource gain (Gorgievski & Hobfoll, 2008). This process may lead to an escalating spiral of losses, wherein symptoms of depression may become the predominant emotions (Hobfoll & Shirom, 2001).
In the present cross-sectional study we focused particularly on burnout symptoms of emotional exhaustion, as related to residents’ mental health problems. Emotional exhaustion reflects the stress dimension of burnout and may be considered the main component and the most obvious manifestation of this complex syndrome (Maslach et al., 2001). This dimension has been used to represent the main aspects of professional burnout in previous studies (e.g., Bakker, Demerouti, & Verbeke, 2004; Van den Broeck, de Cuyper, de Witte, & Vansteenkiste, 2010). Through emotional exhaustion, which reflects work-related and domain-specific well-being, the impact of work conditions can be transmitted to other life domains (e.g., family), and can contribute to domain-unspecific (or context-free) outcomes (e.g., residents’ mental health; Frone, 2003). Thus, the main hypothesis was that burnout (emotional exhaustion) would mediate the relation between job demands/resources on the one hand, and WHI and mental health problems on the other hand (hypothesis 1). Supplementary to that, it was hypothesized that: a) job demands would be directly and positively associated with burnout (emotional exhaustion) and work–home interference (hypotheses 2a and 2b, respectively); b) job resources would be directly and negatively associated with burnout, i.e., emotional exhaustion (hypothesis 3); and c) burnout (emotional exhaustion) and work–home interference would be directly and positively related to mental health problems (hypotheses 4a and 4b, respectively). A secondary purpose of the study was to assess the internal consistency and construct reliability, as well as convergent and discriminant validity of the constructs included in our study, because the whole instrument had not previously been validated in the Greek version.
Methods
Participants and Procedures
All full-time residents, who were employed by Evangelismos General Hospital, which is the largest Greek hospital in the National Healthcare Service, located in the capital city of Athens, with a capacity of 960 beds, covering 25 different specialties, were invited to participate in the study. To be enrolled, the residents had to meet the following inclusion criteria: (1) being appointed at least three months prior to the survey period and (2) participating in the on-call rotation. An anonymous questionnaire was distributed to all residents who were eligible to participate; they were asked to return the completed questionnaires in a sealed envelope that was placed in a non-transparent empty box by the participant, in order to ensure the anonymity of the questionnaire. One week after the initial distribution of the questionnaire the principal investigator contacted those residents who were eligible to participate in order to remind them about it, while he made a second reminder visit one month later. Participation in the study was voluntary. There was no interference in the study by anyone outside the team of researchers, which means that no pressure was applied by clinical or educational supervisors, managers or others to either take part in or ignore the study. Of the 290 eligible residents, 264 (91 %) responded. Table 1 summarizes sociodemographic and job-related characteristics of the sample. The study participants had a mean age of 33.5 years (SD = 3.3, range = 25–47), 141 (53.4 %) were male and 170 (64.4 %) were single. The majority of residents (44.3 %) were being trained in internal medicine. The number of residents exceeding the limit of 56 h per week, set up by the European Working Time Directive, was calculated to be 142 (61.2 %).
Measures
Sociodemographic details included age, gender and marital status. Regarding job demands and resources, all measures were based on scales from the Questionnaire on the Experience and Evaluation of Work (Schaufeli & Bakker, 2004; Van Veldhoven & Meijman, 1994). Job demands were assessed via a questionnaire that included 13 items, which were rated on a 5-point Likert scale ranging from 1 (never) to 5 (always), according to the frequency with which the respondent felt a particular way in relation to his or her work. These 13 items were grouped into four scales: emotional demands due to working conditions (EDW; 3 items, e.g., “Does your job put you in emotionally upsetting situations?”), patients’ emotional demands (EDP; 3 items, e.g., “Do you have contact with difficult or demanding patients or relatives in your job?”), cognitive demands (CD; 3 items, e.g., “Does your job requires a lot of precision or carefulness?”), and workload (WL; 4 items, e.g., “Do you work under time pressure?”). The items of the four factors had been used by Bakker et al. (2004, 2010).
Job resources were assessed via a questionnaire that included 14 items, which were rated according to the frequency with which the respondent felt a particular way in relation to his or her work. These 14 items were grouped into four scales: autonomy in the job (AUT; 3 items, e.g., “Can you decide on your own, how your work is executed?”); opportunities for professional development (PD; 3 items, e.g., “Does your job offer you opportunities to learn new things?”); support from colleagues (SC; 3 items, e.g., “Can you count on your colleagues when you encounter difficulties in your job?”); and supervisor’s support (SS; 5 items, e.g., “In your work, do you feel appreciated by your supervisor?”). Two scales (i.e., AUT and PD) were rated on a 4-point Likert scale, ranging from 1 (rarely) to 4 (almost always). The remaining two scales (i.e., SC and SS) were rated on a 5-point Likert scale, ranging from 1 (never) to 5 (always). All items had previously been used by Bakker, Demerouti, Taris, Schaufeli, and Schreurs (2003). The scales were translated from English into Greek, following forward–backward translation procedures (Wild et al., 2005). Initially, two professional translators, native Greek speakers with a high level of fluency in English, independently translated the questionnaire into Greek. Subsequently, two professional translators, native English speakers and fluent in Greek, translated the Greek language version back into English. A reconciliation process and further revisions ensured that the back translation was sufficiently similar to the original questionnaire. The semi-final Greek version of the instrument was then pilot-tested and given to a small group of medical residents, and interviews were conducted with them, in order to ensure the clarity and comprehensibility of the items. When no further adaptations were required, the translated questionnaire was finally approved for use among the target population.
Emotional exhaustion, considered as the main aspect of burnout and denoting a sense of being depleted of one’s emotional and physical resources, was measured with the 9-item emotional exhaustion scale from the Maslach Burnout Inventory (MBI; Maslach & Jackson, 1986). Sample items included: “I feel emotionally drained from my work,” “I feel used up at the end of the workday,” and “I feel like I’m at the end of my rope.” Scale items were scored on a 7-point frequency rating scale ranging from 0 (never) to 6 (every day). Higher scores on this scale indicated greater emotional exhaustion. The MBI has already been translated and validated in Greek (Anagnostopoulos & Papadatou, 1992; Papadatou, Anagnostopoulos, & Monos, 1994).
Work–home interference was measured by 4 items based on those of Geurts et al. (2005; e.g., “Do you find it difficult to fulfill your family obligations because of your work schedule?”). Items were rated on a 4-point Likert scale ranging from 1 (rarely) to 4 (almost always). Higher scores indicated more WHI.
The Mental Health Index (MHI-5) was used to measure participants’ general mental health status. MHI-5 is a five-item tool, part of the Short Form Health Survey (SF-36; Ware, Kosinski, & Gandek, 2003) and has been translated and validated in Greek (Anagnostopoulos, Niakas, & Pappa, 2005; Pappa, Kontodimopoulos, & Niakas, 2005). Each item of MHI-5 was rated on a 6-point Likert scale ranging from 1 (all of the time) to 6 (none of the time) according to the frequency with which the respondent felt a particular way, during the past 4 weeks (e.g., “Have you felt so down in the dumps that nothing could cheer you up?”, “Have you felt downhearted and blue?”, “Have you been a very nervous person?”). Two items (e.g., “Have you been a happy person?”) were reverse scored to ensure that a higher item value indicated better mental health. Therefore, the summed scores ranged from 5 to 30, which could be linearly transformed to a 0 to 100 scale, with higher scores corresponding to better mental health, according to the standard procedures for calculation of the mental health scale scores (Ware et al., 2003). The instrument is considered to be a non-specific measure of mental health and includes items that measure the occurrence and extent of psychological distress (mainly related to symptoms of anxiety, depression, and loss of emotional/behavioral control; Trainor, Mallett, & Rushe, 2013), while the two positively worded, reverse-scored, items are intended to measure psychological well-being (Ware et al., 2003). The MHI-5 has been found to have satisfactory predictive validity in screening for depressive disorders (Friedman, Heisel, & Delavan, 2005; Means-Christensen, Arnau, Tonidandel, Bramson, & Meagher, 2005; Silveira et al., 2005; Yamazaki, Fukuhara, & Green, 2005), mood disorders (Rumpf, Meyer, Hapke, & John, 2001), and some anxiety disorders such as generalized anxiety disorder and obsessive–compulsive disorder in community settings (Cuijpers, Smits, Donker, ten Have, & de Graaf, 2009). Performance of the MHI-5 scale in terms of predicting mental health problems (such as depression) has been found to be similar to that of the General Health Questionnaire (GHQ-12; Hoeymans, Garssen, Westert, & Verhaak, 2004).
Other work-related characteristics that were recorded included type of specialty, years between graduation and beginning of specialty training, true working hours per day, number of on-calls per month, number of residents in department, number of specialists in department and number of patients in department. From the above mentioned information, the mean working hours per week could be calculated, allowing us to determine whether the European Working Time Directive (EWTD) was violated or not (Editorial, 2010). The Directive lays down provisions for a maximum 48-hour working week (including overtime), a rest break after six consecutive hours’ work, rest periods of at least 11 consecutive hours per 24-hour period, a minimum weekly rest period of 24 uninterrupted hours for each 7-day period, and a minimum of four weeks’ paid leave per year, to protect workers from adverse health and safety risks (Morrow, Burford, Carter, & Illing, 2012). Before August 2009, the working week limit was 56 h. Moreover, we could easily calculate the number of residents per specialist ratio and the number of patients per resident ratio. Finally, we grouped the 25 different specialties into three large groups: internal medicine (e.g., cardiology, nephrology, oncology, gastroenterology, pulmonary disease), surgical (e.g., general surgery, cardiothoracic), and other (e.g., diagnostic and laboratory such as radiology, microbiology) specialty groups.
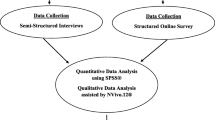
Statistical Analyses
Regarding the number of cases included in the various statistical analyses, some respondents had missing values on some analysis variables. But the missing value rate was small (<5 %). One contemporary, highly recommended, method for dealing with missing data and statistical power loss is multiple imputation (MI; Enders, 2010; Graham, 2009; Janssen et al., 2010). We used LISREL 8.80 (Du Toit & du Toit, 2001; Jöreskog & Sörbom, 2008) to implement the MI procedure. The MI procedure produces estimates for the missing values that take the place of the values that are missing. This procedure is described in detail in Schafer (1997) and uses the Expectation-Maximization (EM) algorithm. The imputed dataset is a complete dataset.
Subsequently, all scale items were subjected to a confirmatory factor analysis (CFA) using LISREL 8.80 (Jöreskog & Sörbom, 2008), followed by structural equation modeling (SEM). CFA is hypothesis-driven and is used when the goal is to identify latent variables when there is sufficient theoretical and empirical basis for a researcher to specify, in advance, the appropriate number of factors to retain and the pattern of zero and nonzero loadings of the measured variables on the common factors (Jöreskog, Sörbom, du Toit, & du Toit, 2000). One of the advantages of CFA is that it enables the researcher to account for measurement error and unreliability in measures of variables. Correlation matrices of continuous non-normal variables and the corresponding asymptotic covariances were used as input, and estimates were derived applying the maximum likelihood method. Apart from the loadings of each indicator on the underlying factors, the models included measurement error terms, representing variance that was not accounted for by the factors. SEM specified the relationships between the latent independent (exogenous) and the latent dependent (endogenous) variables and assigned the explained and unexplained variance. Four indices were used to assess goodness of fit of the model: the root-mean-square error of approximation (RMSEA) accompanied by its associated 90 % confidence interval, the comparative fit index (CFI), the non-normed fit index (NNFI) that included a correction for model complexity, and the standardized root mean square residual (SRMR). Model fit was considered adequate when CFI was greater than .95, NNFI was greater than .95, RMSEA was lower than .06, and SRMR was lower than .08 (Hu & Bentler, 1999).
In order to assess convergent validity of the constructs, the average variance extracted (AVE) was calculated. The AVE of a construct equals the sum of all squared standardized factor loadings (obtained from CFA) divided by the number of items loading on it. Fornell and Larcker (1981) suggested adequately convergent valid measures of each latent construct should contain less than 50 % error variance (i.e., AVE should be .50 or above, signifying that, on average, the variance due to measurement error is less than the variance captured by an underlying factor). Construct reliability (CR) was also used as an indicator of convergent validity. CR was computed from the squared sum of factor loadings for each construct and the sum of the error variance terms for a construct. CR estimates equal to .70 or higher suggested good reliability. Moreover, AVE was also used to evaluate discriminant validity of the constructs (Hair, Black, Babin, Anderson, & Tatham, 2010). Discriminant validity of a target factor was established if the squared inter-construct correlation estimates associated with that factor were less than its AVE estimate, suggesting that the target factor had more internal (extracted) variance than variance shared between the factors. Discriminant validity of a target factor was further established when correlations with other constructs were (in absolute value) equal to or below .707, providing evidence of measure distinctness, since the constructs would have less than half of their variance in common.
To assess whether mediation was present in the theoretical model, the significance of the indirect effects of independent variables (i.e., job demands/resources) on the dependent variable (i.e., mental health) transmitted through multiple mediators (i.e., emotional exhaustion and WHI), operating in a serial fashion, was tested using SEM and the bias-corrected bootstrap confidence intervals (CI). Bootstrapping is a non-parametric resampling method that can be extended to designs involving indirect effects. In the case of simple mediation, indirect effects equal the product of two unstandardized regression coefficients, one representing the effect of the independent variable on the proposed mediator, and the other representing the effect of the mediator on the dependent variable, controlling for the independent variable (Frazier, Tix, & Barron, 2004). However, using the product of regression coefficients for making inferences about indirect effects, involves implicit assumption that the sampling distribution of the indirect effect is normal. There are reasons to suspect that this assumption does not hold when mediation is present (Shrout & Bolger, 2002). Thus, bootstrapping has been recommended (MacKinnon, Lockwood, & Williams, 2004). To bootstrap the sampling distribution of the indirect effects, the regression coefficients are repeatedly estimated k times with bootstrap samples, each of which contains n cases randomly sampled with replacement from the original sample (that is a given case can be selected multiple times), where n is the size of the original sample. This process yields k estimates of the indirect effects of the independent variable on the dependent variable. These k values of the indirect effects are then sorted from low to high, thus enabling the specification of the lower and upper bounds of the desired CI. Bootstrapping was conducted using Analysis of Moment Structures (AMOS) v.21 (Arbuckle, 2012), generating 2,000 bootstrap samples and 95 % bias-corrected CIs for indirect effects. Given that an indirect effect might be detected even when the direct or total effect was not statistically significant (Rucker, Preacher, Tormala, & Petty, 2011), the direct and total effects were tested separately.
Results
Regarding the job-related characteristics of participants, the mean working hours per day, not including on-call duties, were 8.0 (SD = 1.5), the mean number of days-off was 1.6 (SD = 1.7) per month, the mean number of on-calls was 6.9 (SD = 1.6) per month and the mean working hours per week, including on-call duties, were 60.9 (SD = 14.7). The mean residents/specialist ratio was 1.9 (SD = 1.0) and the mean patients/resident ratio was 3.0 (SD = 2.0). The latter referred only to specialties with immediate contact with patients. The mean remaining time to complete training was 26.0 (SD = 15.2) months, while the mean time between medical graduation and beginning of specialty training was 3.0 (SD = 1.8) years.
Convergent and Discriminant Validity, and Construct Reliability
Results obtained from CFA regarding convergent validity of the constructs (Table 2) showed that all constructs exhibited AVE values above the .50 criterion, ranging from .506 to .688. Moreover, CR values were all above the conventional threshold of .70, ranging from .752 to .900. Regarding discriminant validity of the constructs, we compared the shared variances between paired factors with the average variance extracted of the individual factors. For example, it can be seen that the AVE of .528 for workload is greater than the shared variance of .411 (i.e., correlation .6412) between workload and cognitive demands, as well as than the shared variance between workload and each one of the rest of the constructs. All constructs included in Table 2 had more internal (extracted) variance than variance shared between the factors, supporting their discriminant validity.
Correlation Analysis
Regarding correlations among the factors, as seen in Table 2, better residents’ mental health was significantly and strongly correlated with more professional development (r = .293, p ≤ .001), supervisor support (r = .355, p ≤ .001), and support from colleagues (r = .282, p ≤ .001), while medical residents who experienced poor mental health were characterized by greater emotional exhaustion (r = −.706, p < .001), more WHI (r = −.625, p < .001), workload (r = −.265, p < .01), emotional demands due to working conditions (r = −.167, p < .05), and patients’ emotional demand (r = −.231, p < .01).
Confirmatory Factor Analysis and Structural Equation Modeling
An 11-factor model was tested, where the factors were allowed to be oblique (i.e., each factor was allowed to correlate with the others). In Fig. 2, the items that served as indicators of the latent constructs are shown. In this diagram, observed variables are represented by rectangles and latent variables are enclosed in ellipses.
Completely standardized solution for the variables included in the model (n = 262). Observed variables are represented by rectangles and latent variables are enclosed in ellipses. Numbers enclosed in rectangles indicate unique variances (e.g., measurement errors) and those in the middle of arrows pointing from latent variables to observed ones indicate factor loadings. Significant direct paths among latent variables are represented by bold straight lines with one-way arrows pointing to them, while corresponding standardized regression coefficients are placed in the middle of these arrows. All factor loading values displayed are statistically significant at the .01 level. Non-bold straight lines with one-way arrows pointing to latent variables represent non-significant direct paths.*p < .05, ***p < .001
The unstandardized loadings of the items on the factors were all statistically significant at 5 % level. Completely standardized factor loadings ranged from .43 to .98, while 73 % of them were large (≥.71) meaning that the majority of the squared standardized loadings were larger than .50 (i.e., the majority of the variance in the indicators was due to the latent constructs, which suggests an adequate level of validity among individual indicators). Accordingly, the majority of the observed variables were reliable and good measures of their latent variables. Most of the standard errors of the unstandardized parameter estimates were small (< .07), indicating that the values of the model free parameters had been estimated accurately. All measurement errors in the observed variables were statistically significant at 5 % level, except the measurement error of one item that loaded on the “support from colleagues” factor. Analysis of modification indices and standardized residuals suggested that there was evidence of measurement error correlations. Thus, covariation between measurement errors of the items “working is a strain” and “feel too much stress” (both being indicators of the emotional exhaustion factor), and between errors of the items “down in dumps” and “blue/downhearted” (both being indicators of the mental health factor) was taken into account. Measurement error covariances (equal to .29 and .16, respectively) were not large enough to signify multidimensionality (MacKenzie, Podsakoff, & Podsakoff, 2011). The measurement model had a good fit to the data, with χ 2/df = 1.79 (<3), SRMR = .07, RMSEA = .055 (90 % CI [.051, .059]), NNFI = .96, CFI = .96. Regarding the structural equation model, the fit of this model to the data was also satisfactory, with χ 2/df = 1.71, SRMR = .07, RMSEA = .052 (90 % CI [.048, .057]), NNFI = .96, CFI = .96. All variables included in the structural equations (e.g., job demands and job resources latent variables) accounted for a large proportion of variance in emotional exhaustion (31.6 %) and WHI (47.3 %), and an even larger proportion in mental health (73.4 %).
Direct Effects in SEM Analysis
The standardized regression coefficients of the latent dependent variables in the structural relationships to mental health were statistically significant. As shown in Fig. 2, the downward pointing vertical arrows that connect the latent variables of emotional exhaustion and work–home interference to mental health indicate that these structural relationships are statistically significant. More specifically, emotional exhaustion (β = −.65, SE = .09, p < .001) and WHI (β = −.26, SE = .10, p < .05) were significantly related to mental health. The direction of the sign of the former path coefficient indicated that higher scores on emotional exhaustion were associated with lower levels of mental health. The negative coefficient for the latter variable indicated that medical residents who more frequently experienced work-to-home conflict, had lower levels of mental health. Moreover, emotional exhaustion was positively and significantly related to WHI (β = .50, SE = .08, p < .001).
As shown in the first panel of Table 3 pertaining to direct effects, other significant direct paths were also found, e.g., from workload to emotional exhaustion (β = .31, SE = .11, p < .05) and WHI (β = .32, SE = .12, p < .05), and from professional development (β = −.31, SE = .10, p < .001) and supervisor support (β = −.18, SE = .09, p < .05) to emotional exhaustion. More specifically concerning supervisor support and professional development, the direction of the signs of the path coefficients was consistent with the interpretation that higher scores in supervisor support and professional development were associated with lower emotional exhaustion. All the above mentioned direct effects were significant in the model that included both direct and indirect effects. Additionally, as shown in the second panel of Table 3, the total (direct and indirect) effects of workload, supervisor support and support from colleagues on mental health were statistically significant at the 5 % level.
Indirect Effects in Mediation Analysis
To assess whether mediation was present in the model, the significance of the indirect effects of job demands and job resources on mental health through emotional exhaustion and WHI (mediators) was tested using the bias-corrected bootstrap confidence intervals (CIs). As can be seen from the first panel of Table 4 pertaining to the standardized specific indirect effects, professional development (β = .20, 95 % CI [.07, .35]) and supervisor support (β = .12, 95 % CI [.03, .21]) were significantly related to mental health through emotional exhaustion, while workload was significantly associated with mental health through emotional exhaustion, β = −.20, 95 % CI [− .36, −.06]. To elaborate on this point, greater perceived opportunity for professional development was associated with increased mental health, in part because a greater opportunity reduced feelings of emotional exhaustion, which in turn could improve mental health. Similarly, greater supervisor support helped improve mental health in part because more support reduced emotional exhaustion, which in turn bolstered mental health. Increased workload was negatively associated with mental health, at least in part because higher workload increased emotional exhaustion, which in turn negatively affected mental health. Workload was also significantly associated with mental health through WHI, β = −.08, 95 % CI [− .19, −.01]. Analogous effects, but with an opposite sign, held true with emotional exhaustion as the mediator of the job demands/resources-WHI relationship. For example, greater supervisor support was related to lower WHI, in part because more supervisor support reduced emotional exhaustion, which in turn decreased WHI. All three-path indirect effects of the exogenous variables on mental health (e.g., the specific indirect effect of workload on mental health passing through both mediators) were statistically non-significant at the .05 level. As shown in the second panel of Table 4, the total indirect effects of professional development, workload, and supervisor support on mental health, passing through either mediator (i.e., emotional exhaustion or WHI) were statistically significant. Furthermore, emotional exhaustion was indirectly related to mental health via WHI, β = −.13, 95 % CI [−.25, −.03]. This led to the rejection of the null hypothesis that the indirect effect was zero, given that the corresponding 95 % CI did not contain zero. Thus, greater emotional exhaustion was found to be related to higher WHI, which in turn was associated with poor mental health.
Regarding our study results on the role of some objective measures of job stress, such as compliance with EWTD, we added the binary variable “compliance with EWTD” (0 = yes, 1 = no) as an independent variable in our model, and re-ran our analyses. Certain standardized regression coefficients of “compliance with EWTD” in the structural relationships to burnout and job demands, were statistically significant. In particular, compliance with EWTD was significantly related to workload (β = .350, SE = .060, p < .01), cognitive demands (β = .195, SE = .069, p < .01) and patients’ emotional demands (β = .137, SE = .068, p < .05). The direction of the sign of the path coefficients indicated that more working hours than that allowed under the EWTD were associated with higher scores on workload, cognitive demands, and patients’ emotional demands. No statistically significant coefficients were found for the paths from “compliance with EWTD” to job resources or burnout (emotional exhaustion). This confirms our assumption that it is not the objective stressors (i.e., compliance with EWTD) that count, but the subjectively experienced strains (i.e., perceived workload). We also added “level/year of training” (indexed as number of months remaining to complete residency) as an independent variable in our model, and re-ran our analyses. Only a few of the standardized regression coefficients of “level of training” in the structural relationships to burnout and job resources were statistically significant. In particular, job autonomy (β = −.160, SE = .064, p < .05) and support from colleagues (β = .205, SE = .054, p < .01) were significantly related to level of training. The direction of the sign of the path coefficients indicated that a more advanced year of residency (i.e., less remaining months) was associated with higher scores on autonomy and lower scores on support from colleagues. No statistically significant coefficients were found for the paths from “level of training” to job demands or burnout (emotional exhaustion).
Regarding specialty area (measured as a nominal variable, and applying ANOVA) we found that there were no statistically significant differences between residents of different specialties (i.e., surgical, internal medicine, diagnostic/laboratory) regarding burnout (emotional exhaustion), F(2, 260) = 2.18, p > .05, and job resources, e.g., support from colleagues, F(2, 261) = 1.16, p > .05, although for supervisor support, it was found that residents of internal medicine had significantly higher scores on supervisor support than those of laboratory specialties, F(2, 261) = 3.93, p < .05. This again confirms our assumption that, generally speaking, it is not the objective stressors (i.e., level of training, specialty area) that count, but the subjectively experienced strains (i.e., perceived lack of support related to different levels of training or different specialties).
Discussion
The aim of the current study was to test a research model that specified possible factors associated with mental health of Greek medical residents, based on the JD-R model. CFA provided support for the reliability and convergent and discriminant validity of the constructs (e.g., job demands and resources, emotional exhaustion, work–home interference, mental health). Results obtained from SEM confirmed our research hypotheses. First, job demands (workload) and job resources (supervisor support, professional development) were indirectly associated with WHI and mental health, and transmitted their effects on mental health through emotional exhaustion. In this way, we confirmed the mediating role of burnout (emotional exhaustion) in the relationship between job demands/resources, WHI and mental health, as hypothesized. These findings are consistent with that of previous research and meta-analyses (Amstad, Meier, Fasel, Elfering, & Semmer, 2011; Kelloway & Barling, 1991). Warr (2007) has suggested that work stress may be directly associated with work-related, domain specific, well-being/strain (e.g., burnout) and indirectly related to more general, domain-unspecific, indicators of well-being/strain (e.g., context-free mental health), which are mediated by work-related strain. In this way, domain-specific well-being (seen as a proximal variable) may be related to general well-being (seen as a distal variable).
Second, our results brought out job demands (i.e., workload associated with working fast, working extra hard, working under time pressure, and experiencing job overload) as the main factor directly and significantly related to the health impairment process, leading to burnout (emotional exhaustion), confirming our hypotheses. This result is in line with that of numerous previous studies that have identified positive associations between work overload and burnout (e.g., Demerouti et al., 2001; Xanthopoulou et al., 2007). Although workload has been regarded as a “job challenge” (rather than a job hindrance), it seems that this may not be true for medical residents. For example, Greek medical residents were found to be dissatisfied with the quality and challenges of their residency training, as well as with their work responsibilities and continuous medical education activities, and felt that their daily schedule involved too much routine and trivial medical paperwork (Msaouel et al., 2010). The Greek healthcare system has relied heavily on the service of junior doctors and medical residents, while cover at night has been provided by medical residents who remain in the hospital for long hours, whilst the consultant is on call from home (Panagopoulou et al., 2006). Workload, fast work, and time pressure may, therefore, be experienced as overwhelming, instead of challenging, by medical residents. Furthermore, in line with previous studies (e.g., Byron, 2005), job demands were also positively associated with WHI, as expected in hypothesis 2b.
Third, two types of job resources (i.e., professional development and supervisor support) were directly and negatively associated with burnout (emotional exhaustion), confirming our hypotheses. Previous studies (e.g., Hakanen et al., 2008; Schaufeli & Bakker, 2004; van Daalen, Willemsen, Sanders, & van Veldhoven, 2009) have reported similar findings regarding the job resources-burnout relationship. Ratanawongsa et al. (2007) have argued that residents’ professional development and growth may promote their professional satisfaction and may be closely connected to their well-being. Supervision in the setting of residents’ medical education has the goal of helping to assure each resident’s development of the skills, knowledge, and attitudes required to enter the unsupervised practice of medicine (Accreditation Council for Graduate Medical Education [ACGME], 2011). Inadequate supervision has been found to be positively correlated with reports of negative features of residents’ training, including medical errors, sleep deprivation, stress, and conflict with other medical personnel, and inversely related to residents’ positive ratings of their learning, time spent with attending physicians, and overall satisfaction with the residency experience (Baldwin, Daugherty, & Ryan, 2010). Cohen and Patten (2005) found that the majority of residents identified their program director as a possible resource, while Farnan et al. (2012) suggested that enhanced clinical supervision of care provided by resident physicians might improve both patient- and education-related outcomes. Low interpersonal conflicts and enhanced interpersonal relationships with one’s supervisor are related to job satisfaction, organizational commitment and low turnover intentions (Frone, 2000a). It seems that obtaining “reward from work” is very important in reducing the risk of poor psychological well-being (Haoka et al., 2010).
Fourth, in accordance with previous research (Allen et al., 2000; Hakanen & Schaufeli, 2012; Mikkelsen & Burke, 2004; van Daalen et al., 2009), hypotheses 4a and 4b assuming that burnout (emotional exhaustion) and WHI would be positively related to poor mental health, were also supported. Amstad et al. (2011) suggested that work-family conflict could affect well-being not only with respect to family and working life, but also in general psychological status. In this regard, Frone (2000b), Hakanen et al. (2008), and Warr (2007) have also reported significant interrelations between work-family conflict, job burnout (as a work-related outcome), and subjective well-being (e.g., depression, anxiety).
Contrary to assumptions of the JD-R model, some job demands, i.e., emotional demands from patients or the work environment, were not significantly related to emotional exhaustion or mental health problems. Several factors might account for this result. Demanding or noncompliant patients and complaining family members may be a major source of stress for residents who have to function in an emotionally loaded working environment. However, such strains may provide good preparation for being an efficient physician, who can survive residency and justify a sense of superiority and separateness from other people. Additionally, residents may tend to underestimate patients’ distress and suffering through various cognitive mechanisms, e.g., trivializing patients’ distress, blaming the victim, or considering that persons may somehow deserve their misfortunes (Lazarus, 1985). Another factor that may play a role is that many residents expect to have fulfilling, personally rewarding interactions with patients, and these relationships may be important sources of emotional satisfaction for residents. For these reasons, emotional demands from patients, or the work environment, might be less troublesome than we anticipated, and so might not contribute significantly to residents’ emotional exhaustion or mental health problems. Regarding cognitive demands, these may not be related to residents’ emotional exhaustion or mental health problems, given that such demanding work environment (e.g., requiring lot of concentration, lot of precision, great deal of carefulness) may be most beneficial to their professional development and growth.
Regarding the finding that some job resources (i.e., job autonomy, support from colleagues) did not appear to be significantly related to emotional exhaustion or mental health problems, the following interpretations could be offered. In the healthcare system, work processes are often guided by protocols. Moreover, residents sometimes describe the attending physician as a “micromanager” who dictates the plan of care for patients to the housestaff and allows few autonomous decisions (Farnan, Johnson, Meltzer, Humphrey, & Arora, 2009). To be sure, attending supervisors who micromanage may prevent residents from fully developing their own clinical skills. Yet, supervisors with this style also may provide direct, close onsite supervision (at the bedside), and so create a safer learning environment in which residents may feel more comfortable about being accountable for the decisions they make. As a result, it seems that having a say in how the work is done (i.e., job autonomy) may be less desirable, important or relevant to medical residents. This might explain why residents’ autonomy was not found to be a factor significantly related to emotional exhaustion or mental health problems. Supervisor support and professional development may be more effective in reducing emotional exhaustion due to work overload and the subsequent negative effects on WHI and mental health. These findings may justify our choice to treat the various types of job demands and job resources as separate constructs rather than as equivalent, predetermined (a priori) indicators of latent factors, i.e., either job demands or resources. The impact of any specific job demand or job resource on emotional exhaustion, work–home interference, and mental health depends on how persons in that specific work environment perceive those demands and resources, and the roles and interpersonal relationships those persons have in that work setting.
As far as support from colleagues is concerned, we found there was a significant positive total effect of this factor on residents’ mental health. This is consistent with the findings of Frone (2000a) indicating that interpersonal conflicts and poor interpersonal relationships with coworkers are related to poor personal psychological outcomes (e.g., depression). Relationships among coworkers are based on a communal sharing model of interpersonal relations (Fiske, 1992), where interpersonal conflicts are likely to affect adversely one’s self-evaluation and psychological health, because they undermine one’s sense of self, similarity with others, being liked by socially equivalent others, and being united with others by a common identity.
Study Strengths, Limitations, and Suggestions for Future Research
Among the strengths of our study we should mention the use of a well-developed theoretical framework that could take into account a broad range of specific job characteristics, and the application of CFA and SEM techniques to the analysis of our data. Still, the results of this study must be viewed in light of some limitations, which also suggest possible directions for further research. In the first place, because this study was limited to residents of one large urban public general hospital, our findings may not be generalizable and may not apply to residents in other programs at other hospitals (e.g., private specialized hospitals in rural areas), or in other healthcare systems. However, our study design was strengthened by the inclusion of residents from a variety of specialties and residency years. Secondly, given that our study was cross-sectional, it was not possible to make causal inferences about the relationships between job demands/resources and outcome variables. Longitudinal studies are needed to make assumptions about path directionality. Thirdly, although we focused on unidirectional paths among job demands, resources, and outcomes, dynamic relations, reciprocal causation, and loss/gain spirals might exist, in which job demands, WHI, burnout and mental health might mutually influence each other over time. Thus, although it is likely that job demands and work–home conflict influence mental health problems, it may be the other way round as well. That is, mental health problems may influence the perception of stress-related factors at work and at home. Furthermore, the effects of work-to-family conflict may be reduced by family-to-work facilitation (where family life can enhance work life). In this regard, future research should place more reliance on pre-existing models that combine family stress theory and family resilience theory, such as the family adjustment and adaptation response (FAAR) model (Patterson, 1988), or Hill’s model of work-family facilitation and conflict (Hill, 2005). Additionally, “causal” paths may exist between job demands and job resources. That is, instead of operating in parallel, job demands and resources may operate in a serial fashion, where one type of job demands (e.g., workload) may affect another type of job demands (e.g., cognitive demands) which, in turn, may transmit its effects to one type of job resources (e.g., decreased professional development opportunities), eventually leading to burnout and mental health problems. Thus, sequential causal relations should be examined between job demands and resources. Fourthly, the variables included in the JD-R model were measured at an individual/employee level. Given burnout contagion (Bakker, LeBlanc, & Schaufeli, 2005; Hakanen, Perhoniemi, & Bakker, 2013) and shared perceptions and experiences in teams or in entire organizations (e.g., hospitals), it might be worthwhile for future research on the JD-R model to consider and explore collective perceptions and experiences regarding job demands and resources, and mental health, using multilevel modeling. Fifthly, the role of personal resources (e.g., self-efficacy, optimism) was not examined in the present study. Future research should integrate personal resources into the JD-R model. Finally, although the present study focused on negative outcomes and the health impairment process leading to burnout and mental health problems, future research should consider positive outcomes and the motivational process as well, modeled in a joint fashion, leading to work engagement and job crafting.
Practical Implications
Regarding implications of our findings, the results of our study suggest a number of practical implications. First, given that our results confirm the significant association between WHI and indicators of mental health and psychological well-being, organizations, program directors, and supervisors who are interested in healthy residents should make attempts to minimize conflicts between work and family life. Organizations should be motivated to create a family-friendly work environment and implement family-friendly policies to minimize the adverse effects of certain occupational factors. Organizational work-family initiatives, that may be promoted, may include flexible work arrangements, supportive social interactions, dependent-care assistance (e.g., child care referral services) and general resource services (e.g., work-family seminars to assist residents in managing their multiple work and family role demands, conflict resolution training). The role of supervisors is especially important in this respect, so they should be encouraged and supported in their attempts to convey a family-friendly climate and diminish work-to-family conflict.
Second, given that our results confirm the key role of burnout (emotional exhaustion) in the relationship between job demands/resources and residents’ mental health, intervention studies should be conducted to reduce burnout. Awa, Plaumann, and Walter (2010) found that 80 % of all burnout intervention programs led to a reduction in burnout. However, the majority of these studies were person-directed, including cognitive behavioral training, relaxation, psychotherapy, counseling, clinical supervision, psychosocial skill and communication training. Only 8 % of them were organization-directed. The organization-directed interventions included social support, cognitive behavioral, and management skill training, or personal care giving. Recently, West et al. (2014) implemented a novel institutional-based intervention conducting a randomized clinical trial and involving physicians who attended small-group sessions. Topics addressed during the sessions included meaning in work, personal and professional balance, as well as caring for patients. Practicing physicians with specific expertise in communication and teaching courses in small groups acted as group facilitators. The intervention incorporated elements of mindfulness, self-awareness, reflection, shared experience, and small-group learning for nine months. Participants were found to experience improved meaning and engagement in work and reduced burnout (depersonalization). Regarding work-directed interventions to prevent occupational stress, particularly among healthcare workers, there is limited evidence that such studies can effectively reduce stress symptoms or the levels of burnout (Marine, Ruotsalainen, Serra, & Verbeek, 2006). There may be that interventions concerning burnout have tended to focus on the micro level (the individual physician) or on job redesign/task restructuring rather than healthcare system and medical education redesign. In the latter case, burnout may be considered as a systems problem, towards which interventions should be directed.
Additionally, there are some programs available that aim at assisting medical education programs, their residents, and faculty to identify, prevent, and manage resident fatigue, burnout, and impairment. One such program is the Learning to Address Impairment and Fatigue to Enhance Patient Safety (LIFE) curriculum (Andolsek & Cefalo, 2005). The learning modules of this program were designed to identify common challenges present in residency programs, provide an early warning system for impairments in residents, and implement strategies that may manage symptoms of impairment and poor performance. The curriculum uses CD-ROM and web material for self-directed learning, and consists of workshops on several topics including fatigue and sleep deprivation, stress and depression, substance abuse, resident burnout, boundary violations, disruptive behavior and workplace bullying and harassment, problem residents, and the value of instructive feedback to residents. The burnout module, in particular, presents signs, symptoms, and consequences of burnout, describes characteristics in the individual, the work environment, and the family that increase the risk of burnout, and provides management techniques to help prevent, identify, or alleviate burnout. The curriculum also encourages policies that: make residents feel part of the decision-making process; involve residents in ongoing evaluations of the curricula, rotations, and faculty; strengthen resident input in design and implementation of the evaluation system; use resident input to develop policies on harassment; survey residents regarding their perception of personal well-being; and survey residents on their beliefs about how they are viewed by the faculty and by co-workers. In these ways, a bottom-up participatory approach is encouraged rather than a top-down, more authoritarian approach. Residents can also learn coping skills, negotiation techniques, and conflict resolution methods, which may be used to reduce feelings of burnout.
Third, as far as the association between burnout and medical school education is concerned, burnout in medical students has been found to be associated with reports of unprofessional behavior by students (e.g., cheating, dishonest clinical behavior) and with students holding less altruistic views regarding physicians’ responsibility to society (Dyrbye et al., 2010). Given that medical students’ professional identity and medical ethics are shaped early on in the medical school, restructuring of the learning environment and medical school education is warranted. Attention should be paid not only to the formal aspects that influence the attributes of a medical professional, but also to the hidden curriculum, the informal and tacit aspects of professionalism, transmitted through peer-to-peer and faculty-to-resident contact. Significant aspects of that hidden curriculum constitute formidable challenges to the growth of healthy professionalism, including factors such as: abuse of power in the hierarchy of medical training; disrespect for and dehumanization of patients; failure to achieve authentic human connection between peers, or between students and teachers; and a culture that expects residents to make personal sacrifices for their career (Gaufberg, Batalden, Sands, & Bell, 2010).
Fourth, regarding interventions to enhance residents’ mental health status, obstacles to seeking help and care must be overcome. Residents are usually reluctant to seek or obtain mental health treatment, and so they delay or avoid seeking appropriate care due to multiple barriers that include: ambivalence or denial about the reality of mental health problems; preference to manage problems on their own; lack of time; lack of convenient access to care; financial constraints; and concerns about potential academic jeopardy because of stigma, and the fear of possible violations of privacy and confidentiality (Dunn, Green Hammond, & Roberts, 2009; Guille, Speller, Laff, Epperson, & Sen, 2010; Pitt, Rosenthal, Gay, & Lewton, 2004; Wallace, Lemaire, & Ghali, 2009). Residents’ mental health problems may not be recognized or addressed until impairment is obvious and severe. Consequently, young doctors are especially vulnerable to experiencing depressive symptoms (Wang et al., 2010) as well as to developing other mental health problems including anxiety (Peterlini, Tibério, Saadeh, Pereira, & Martins, 2002). Thus, residents, faculty, and program directors should shift their attitudes toward mental illness and mental health treatment, try to destigmatize mental illness, and change the “hidden curriculum” that perpetuates the notion that psychiatric disorders and psychological problems are shameful. Utilization of confidential evidence-based mental health services by medical residents should be encouraged and given high priority.
Better access to and use of individually-focused interventions has an important role to play in promoting and protecting medical residents’ mental health. Prospective individually-based programs that promote residents’ self-awareness and reflection, and which instill interest in self-care, can help prevent emotional exhaustion and improve physician wellness (e.g., Bakker, Oerlemans, & Ten Brummelhuis, 2013; Dunn, Arnetz, Christensen, & Homer, 2007; Gardiner, Lovell, & Williamson, 2004). Clearly, individually-focused interventions should be a component of a larger and broader set of organization-driven, system-level interventions that might modify the structure of the medical training system and change that system’s culture in directions that could provide better support to residents and protect residents from emotional exhaustion that would otherwise foster mental health problems.
References
Accreditation Council for Graduate Medical Education. (2011). Common program requirements. Retrieved from http://www.acgme.org/acgmeweb/Portals/0/dh_dutyhoursCommonPR07012007.pdf.
Allen, T. D., Herst, D. E. L., Bruck, C. S., & Sutton, M. (2000). Consequences associated with work-to-family conflict: A review and agenda for future research. Journal of Occupational Health Psychology, 5, 278–308.
Aminazadeh, N., Farrokhyar, F., Naeeni, A., Naeeni, M., Reid, S., Kashfi, A., et al. (2012). Is Canadian surgical residency training stressful? Canadian Journal of Surgery, 55, S145–S151.
Amstad, F. T., Meier, L. L., Fasel, U., Elfering, A., & Semmer, N. K. (2011). A meta-analysis of work-family conflict and various outcomes with a special emphasis on cross-domain versus matching-domain relations. Journal of Occupational Health Psychology, 16, 151–169.
Anagnostopoulos, F., Niakas, D., & Pappa, E. (2005). Construct validation of the Greek SF-36 health survey. Quality of Life Research, 14, 1959–1965.
Anagnostopoulos, F., & Papadatou, D. (1992). Factorial composition and internal consistency of the Greek version of the Maslach burnout inventory administered to a sample of nurses. Psychological Themata, 5, 183–202.
Andolsek, K., & Cefalo, R. C. (Eds.). (2005). Learning to address impairment and fatigue to enhance patient safety (LIFE): Teachers guide. Office of Continuing Medical Education: Duke University School of Medicine.
Arbuckle, J. L. (2012). IBM SPSS Amos (Version 21.0): User’s guide. Chicago, IL: IBM Corporation.
Awa, W. L., Plaumann, M., & Walter, U. (2010). Burnout prevention: A review of intervention programs. Patient Education and Counseling, 78, 184–190.
Bakker, A. B., & Demerouti, E. (2013). The spillover-crossover model. In J. G. Grzywacz & E. Demerouti (Eds.), New frontiers in work and family research (pp. 54–70). New York: Psychology Press.
Bakker, A. B., Demerouti, E., Taris, T. W., Schaufeli, W. B., & Schreurs, P. J. G. (2003). A multi-group analysis of the job demands-resources model in four home care organizations. International Journal of Stress Management, 10, 16–38.
Bakker, A. B., Demerouti, E., & Verbeke, W. (2004). Using the job demands-resources model to predict burnout and performance. Human Resource Management, 43, 83–104.
Bakker, A. B., LeBlanc, P. M., & Schaufeli, W. B. (2005). Burnout contagion among intensive care nurses. Journal of Advanced Nursing, 51, 276–287.
Bakker, A. B., Oerlemans, W., & Ten Brummelhuis, L. L. (2013). Becoming fully engaged in the workplace: What individuals and organizations can do to foster work engagement. In R. J. Burke & C. L. Cooper (Eds.), The fulfilling workplace: The organization’s role in achieving individual and organizational health. Burlington, VT: Gower.
Bakker, A. B., ten Brummelhuis, L. L., Prins, J. T., & van der Heijden, F. M. (2011). Applying the job demands-resources model to the work-home interface: A study among medical residents and their partners. Journal of Vocational Behavior, 79, 170–180.
Bakker, A. B., van Veldhoven, M., & Xanthopoulou, D. (2010). Beyond the demand-control model: Thriving on high job demands and resources. Journal of Personnel Psychology, 9, 3–16.
Baldwin, D. C., Daugherty, S. R., & Ryan, P. M. (2010). How residents view their clinical supervision: A reanalysis of classic national survey data. Journal of Graduate Medical Education, 2, 37–45.
Byron, K. (2005). A meta-analytic review of work-family conflict and its antecedents. Journal of Vocational Behavior, 67, 169–198.
Campbell, J., Prochazka, A. V., Yamashita, T., & Gopal, R. (2010). Predictors of persistent burnout in internal medicine residents: A prospective cohort study. Academic Medicine, 85, 1630–1634.
Cohen, J. S., & Patten, S. (2005). Well-being in residency training: A survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Medical Education, 5, 21.
Collier, V. U., McCue, J. D., Markus, A., & Smith, L. (2002). Stress in medical residency: Status quo after a decade of reform? Annals of Internal Medicine, 136, 384–390.
Cuijpers, P., Smits, N., Donker, T., ten Have, M., & de Graaf, R. (2009). Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Research, 168, 250–255.
Demerouti, E., & Bakker, A. B. (2011). The job demands-resources model: Challenges for future research. South African Journal of Industrial Psychology, 37, 1–9.
Demerouti, E., Bakker, A. B., Nachreiner, F., & Schaufeli, W. B. (2001). The job demands-resources model of burnout. Journal of Applied Psychology, 86, 499–512.
Du Toit, M., & du Toit, S. (2001). Interactive LISREL: User’s guide. Lincolnwood, IL: Scientific Software International.
Dunn, P. M., Arnetz, B. B., Christensen, J. F., & Homer, L. (2007). Meeting the imperative to improve physician well-being: Assessment of an innovative program. Journal of General Internal Medicine, 22, 1544–1552.
Dunn, L. B., Green Hammond, K. A., & Roberts, L. W. (2009). Delaying care, avoiding stigma: Residents’ attitudes toward obtaining personal health care. Academic Medicine, 84, 242–250.
Dyrbye, L. N., Stanford Massie, F., Eacker, A., Harper, W., Power, D., Durning, S. J., et al. (2010). Relationship between burnout and professional conduct and attitudes among US medical students. Journal of the American Medical Association, 304, 1173–1180.
Economou, C., & Giorno, C. (2009). Improving the performance of the public health care system in Greece (Organization for Economic Co-operation and Development-Economics Department Working Paper No. 722). Paris: OECD Publishing.
Editorial. (2010). Doctors’ training and the European Working Time Directive. Lancet 375, 2121.
Enders, C. K. (2010). Applied missing data analysis. New York: The Guilford Press.
Fahrenkopf, A. M., Sectish, T. C., Barger, L. K., Sharek, P. J., Lewin, D., Chiang, V. W., et al. (2008). Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ, 336, 488–491.
Farnan, J. M., Johnson, J. K., Meltzer, D. O., Humphrey, H. J., & Arora, V. M. (2009). On-call supervision and resident autonomy: From micromanager to absentee attending. American Journal of Medicine, 122, 784–788.
Farnan, J. M., Petty, L. A., Georgitis, E., Martin, S., Chiu, E., Prochaska, M., et al. (2012). A systematic review: The effect of clinical supervision on patient and residency education outcomes. Academic Medicine, 87, 428–442.
Fiske, A. P. (1992). The four elementary forms of sociality: Framework for a unified theory of social relations. Psychological Review, 99, 689–723.
Fornell, C., & Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research, 18, 39–50.
Franche, R., Williams, A., Ibrahim, S., Grace, S. L., Mustard, C., Minore, B., et al. (2006). Path analysis of work conditions and work-family spillover as modifiable workplace factors associated with depressive symptomatology. Stress and Health, 22, 91–103.
Frazier, P. A., Tix, A. P., & Barron, K. E. (2004). Testing moderator and mediator effects in counseling psychology research. Journal of Counseling Psychology, 51, 115–134.
Friedman, B., Heisel, M., & Delavan, R. (2005). Validity of the SF-36 five-item mental health index for major depression in functionally impaired, community-dwelling elderly patients. Journal of the American Geriatrics Society, 53, 1978–1985.
Frone, M. R. (2000a). Interpersonal conflict at work and psychological outcomes: Testing a model among young workers. Journal of Occupational Health Psychology, 5, 246–255.
Frone, M. R. (2000b). Work-family conflict and employee psychiatric disorders: The National Comorbidity Survey. Journal of Applied Psychology, 85, 888–895.
Frone, M. R. (2003). Work-family balance. In J. C. Quick & L. E. Tetrick (Eds.), Handbook of occupational health psychology (pp. 143–162). Washington, D.C.: American Psychological Association.
Gardiner, M., Lovell, G., & Williamson, P. (2004). Physician you can heal yourself! Cognitive behavioural training reduces stress in GPs. Family Practice, 21, 545–551.
Gaufberg, E. H., Batalden, M., Sands, R., & Bell, S. K. (2010). The hidden curriculum: What can we learn from third-year medical student narrative reflections? Academic Medicine, 85, 1709–1716.
Gelfand, D. V., Podnos, Y. D., Carmichael, J. C., Saltzman, D. J., Wilson, S. E., & Williams, R. A. (2004). Effect of the 80-hour workweek on resident burnout. Archives of Surgery, 139, 933–940.
Geurts, S. A. E., Kompier, M. A. J., Roxburgh, S., & Houtman, I. L. D. (2003). Does work-home interference mediate the relationship between workload and well-being? Journal of Vocational Behavior, 63, 532–559.
Geurts, S. A. E., Taris, T. W., Kompier, M. A. J., Dikkers, J. S. E., Van Hooff, M. L. M., & Kinnunen, U. M. (2005). Work-home interaction from a work psychological perspective: Development and validation of a new questionnaire, the SWING. Work & Stress, 19, 319–339.
Gillespie, C., Paik, S., Ark, T., Zabar, S., & Kalet, A. (2009). Residents’ perceptions of their own professionalism and the professionalism of their environment. Journal of Graduate Medical Education, 1, 208–215.
Goebert, D., Thompson, D., Takeshita, J., Beach, C., Bryson, P., Ephgrave, K., et al. (2009). Depressive symptoms in medical students and residents: A multischool study. Academic Medicine, 84, 236–241.
Gorgievski, M. J., & Hobfoll, S. E. (2008). Work can burn us out or fire us up: Conservation of resources in burnout and engagement. In J. R. B. Halbesleben (Ed.), Handbook of stress and burnout in health care (pp. 7–22). New York: Nova Science Publishers.
Graham, J. W. (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576.
Greenhaus, J. H., & Beutell, N. J. (1985). Sources of conflict between work and family roles. Academy of Management Review, 10, 76–88.
Guille, C., Speller, H., Laff, R., Epperson, C. N., & Sen, S. (2010). Utilization and barriers to mental health services among depressed medical interns: A prospective multisite study. Journal of Graduate Medical Education, 2, 210–214.
Hair, J. F., Black, B., Babin, B., Anderson, R. E., & Tatham, R. L. (2010). Multivariate data analysis: A global perspective. NJ: Pearson Education.
Hakanen, J. J., Perhoniemi, R., & Bakker, A. B. (2013). Crossover of exhaustion between dentists and dental nurses. Stress and Health,. doi:10.1002/smi.2498.
Hakanen, J. J., & Schaufeli, W. B. (2012). Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. Journal of Affective Disorders, 141, 415–424.
Hakanen, J. J., Schaufeli, W. B., & Ahola, K. (2008). The job demands-resources model: A three-year cross-lagged study of burnout, depression, commitment, and work engagement. Work & Stress, 22, 224–241.
Haoka, T., Sasahara, S., Tomotsune, Y., Yoshino, S., Maeno, T., & Matsuzaki, I. (2010). The effect of stress-related factors on mental health status among resident doctors in Japan. Medical Education, 44, 826–834.
Hellenic Quality Assurance and Accreditation Agency. (2010). External evaluation report for the University of Ioannina Medical School. Athens: HQA.
Hill, R. (1949). Families under stress: Adjustment to the crises of war separation and reunion. New York: Harper and Brothers.
Hill, E. J. (2005). Work-family facilitation and conflict, working fathers and mothers, work-family stressors and support. Journal of Family Issues, 26, 793–819.
Hobfoll, S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44, 513–524.
Hobfoll, S. E., & Shirom, A. (2001). Conservation of resources theory. In R. T. Golembiewski (Ed.), Handbook of organizational behavior (2nd ed., pp. 57–80). New York, NY: Dekker.
Hoeymans, N., Garssen, A. A., Westert, G. P., & Verhaak, P. F. M. (2004). Measuring mental health of the Dutch population: A comparison of the GHQ-12 and the MHI-5. Health and Quality of Life Outcomes, 2, 23.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55.
IsHak, W. W., Lederer, S., Mandili, C., Nikravesh, R., Seligman, L., Vasa, M., et al. (2009). Burnout during residency training: A literature review. Journal of Graduate Medical Education, 1, 236–242.
Janssen, K. J. M., Donders, A. R. T., Harrell, F. E., Vergouwe, Y., Chen, Q., Grobbee, D. E., et al. (2010). Missing covariate data in medical research: To impute is better than to ignore. Journal of Clinical Epidemiology, 63, 721–727.
Jöreskog, K. G., & Sörbom, D. (2008). LISREL 8.80 for windows [Computer Software]. Lincolnwood, IL: Scientific Software International Inc.
Jöreskog, K., Sörbom, D., du Toit, S., & du Toit, M. (2000). LISREL 8: New statistical features. Lincolnwood, IL: Scientific Software International Inc.
Kelloway, E. K., & Barling, J. (1991). Job characteristics, role stress and mental health. Journal of Occupational Psychology, 64, 291–304.
Kostakis, A., & Mantas, D. (2008). Surgical education in Greece. World Journal of Surgery, 32, 2167–2171.
Lazarus, R. S. (1985). The trivialization of distress. In J. C. Rosen & L. J. Solomon (Eds.), Prevention in health psychology (pp. 279–298). Hanover, NH: University Press of New England.
Lebensohn, P., Dodds, S., Benn, R., Brooks, A. J., Birch, M., Cook, P., et al. (2013). Resident wellness behaviors: Relationship to stress, depression, and burnout. Family Medicine, 45, 541–549.
Lockley, S. W., Cronin, J. W., Evans, E. E., Cade, B. E., Lee, C. J., Landrigan, C. P., et al. (2004). Effect of reducing interns’ weekly work hours on sleep and attentional failures. New England Journal of Medicine, 351, 1829–1837.
MacKenzie, S. B., Podsakoff, P. M., & Podsakoff, N. P. (2011). Construct measurement and validation procedures in MIS and behavioral research: Integrating new and existing techniques. MIS Quarterly, 35, 293–334.
MacKinnon, D. P., Lockwood, C. M., & Williams, J. (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128.
Magee, C. A., Stefanic, N., Caputi, P., & Iverson, D. C. (2012). The association between job demands/control and health in employed parents: The mediating role of work-to-family interference and enhancement. Journal of Occupational Health Psychology, 17, 196–205.
Marine, A., Ruotsalainen, J. H., Serra, C., & Verbeek, J. H. (2006). Preventing occupational stress in healthcare workers (review). Cochrane Database of Systematic Reviews, 4, Art. No.: CD002892.
Maslach, C., & Jackson, S. E. (1986). Maslach burnout inventory (Manual) (2nd ed.). Palo Alto, CA: Consulting Psychologists Press.
Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52, 397–422.
McCray, L. W., Cronholm, P. F., Bogner, H. R., Gallo, J. J., & Neill, R. A. (2008). Resident physician burnout: Is there hope? Family Medicine, 40, 626–632.
McCubbin, H. I., & Patterson, J. M. (1983). The family stress process: The double ABCX model of family adjustment and adaptation. Marriage and Family Review, 6, 7–37.
Means-Christensen, A. J., Arnau, R. C., Tonidandel, A. M., Bramson, R., & Meagher, M. W. (2005). An efficient method of identifying major depression and panic disorder in primary care. Journal of Behavioral Medicine, 28, 565–572.
Mikkelsen, A., & Burke, R. J. (2004). Work-family concerns of Norwegian police officers: Antecedents and consequences. International Journal of Stress Management, 11, 429–444.
Morrow, G., Burford, B., Carter, M., & Illing, J. (2012). The impact of the working time regulations on medical education and training: Literature review. Durham: Durham University, Centre for Medical Education Research.
Msaouel, P., Keramaris, N. C., Tasoulis, A., Kolokythas, D., Syrmos, N., Pararas, N., et al. (2010). Burnout and training satisfaction of medical residents in Greece: Will the European work time directive make a difference? Human Resources for Health, 8, 16.
Panagopoulou, E., Montgomery, A., & Benos, A. (2006). Burnout in internal medicine physicians: Differences between residents and specialists. European Journal of Internal Medicine, 17, 195–200.
Papadatou, D., Anagnostopoulos, F., & Monos, D. (1994). Factors contributing to the development of burnout in oncology nursing. British Journal of Medical Psychology, 67, 187–199.
Pappa, E., Kontodimopoulos, N., & Niakas, D. (2005). Validating and norming of the Greek SF-36 health survey. Quality of Life Research, 14, 1433–1438.
Patterson, J. M. (1988). Families experiencing stress: I. The family adjustment and adaptation response model—Applying the FAAR model to health-related issues for intervention and research. Family Systems Medicine, 6, 202–237.
Peterlini, M., Tibério, I. F., Saadeh, A., Pereira, J. C., & Martins, M. A. (2002). Anxiety and depression in the first year of medical residency training. Medical Education, 36, 66–72.
Pitt, E., Rosenthal, M. M., Gay, T. L., & Lewton, E. (2004). Mental health services for residents: More important than ever. Academic Medicine, 79, 840–844.
Prins, J. T., Gazendam-Donofrio, S. M., Tubben, B. J., Van Der Heijden, F. M., Van De Wiel, H., & Hoekstra-Weebers, J. E. (2007). Burnout in medical residents: A review. Medical Education, 41, 788–800.
Prins, J. T., Hoekstra-Weebers, J. E. H. M., Gazendam-Donofrio, S. M., Dillingh, G. S., Bakker, A. B., Huisman, M., et al. (2010). Burnout and engagement among resident doctors in the Netherlands: A national study. Medical Education, 44, 236–247.
Prins, J. T., van der Heijden, F. M., Hoekstra-Weebers, J. E. H. M., Bakker, A. B., van de Wiel, H. B. M., Jacobs, B., et al. (2009). Burnout, engagement and resident physicians’ self-reported errors. Psychology, Health & Medicine, 14, 654–666.
Rantanen, J., Kinnunen, U., Feldt, T., & Pulkkinen, L. (2008). Work-family conflict and psychological well-being: Stability and cross-lagged relations within one- and six-year follow-ups. Journal of Vocational Behavior, 73, 37–51.
Ratanawongsa, N., Wright, S. M., & Carrese, J. A. (2007). Well-being in residency: A time for temporary imbalance? Medical Education, 41, 273–280.
Ripp, J., Babyatsky, M., Fallar, R., Bazari, H., Bellini, L., Kapadia, C., et al. (2011). The incidence and predictors of job burnout in first-year internal medicine residents: A five-institution study. Academic Medicine, 86, 1304–1310.
Rucker, D. D., Preacher, K. J., Tormala, Z. L., & Petty, R. E. (2011). Mediation analysis in social psychology: Current practices and new recommendations. Social and Personality Psychology Compass, 5, 359–371.
Rumpf, H.-J., Meyer, C., Hapke, U., & John, U. (2001). Screening for mental health: Validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Research, 195, 243–253.
Schafer, J. L. (1997). Analysis of incomplete multivariate data. New York: Chapman & Hall/CRC.
Schaufeli, W. B., & Bakker, A. B. (2004). Job demands, job resources, and their relationship with burnout and engagement: A multi-sample study. Journal of Organizational Behavior, 25, 293–315.
Schaufeli, W. B., & Taris, T. W. (2014). A critical review of the job demands-resources model: Implications for improving work and health. In G. F. Bauer & O. Hammig (Eds.), Bridging occupational, organizational and public health: A transdisciplinary approach (pp. 43–68). Dordrecht: Springer.
Shrout, P. E., & Bolger, N. (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7, 422–445.
Silveira, E., Taft, C., Sundh, V., Waern, M., Palsson, S., & Steen, B. (2005). Performance of the SF-36 Health survey in screening for depressive and anxiety disorders in an elderly female Swedish population. Quality of Life Research, 14, 1263–1274.
Ten Brummelhuis, L. L., & Bakker, A. B. (2012). A resource perspective on the work-home interface: The work-home resources model. American Psychologist, 67, 545–556.
Thomas, N. K. (2004). Resident burnout. Journal of the American Medical Association, 292, 2880–2889.
Trainor, K., Mallett, J., & Rushe, T. (2013). Age related differences in mental health scale scores and depression diagnosis: Adult responses to the CIDI-SF and MHI-5. Journal of Affective Disorders, 151, 639–645.
Van Daalen, G., Willemsen, T. M., Sanders, K., & van Veldhoven, M. J. P. M. (2009). Emotional exhaustion and mental health problems among employees doing “people work”: The impact of job demands, job resources and family-to-work conflict. International Archives of Occupational and Environmental Health, 82, 291–303.
Van den Broeck, A., de Cuyper, N., de Witte, H., & Vansteenkiste, M. (2010). Not all job demands are equal: Differentiating job hindrances and job challenges in the job demands-resources model. European Journal of Work and Organizational Psychology, 19, 735–759.
Van der Heijden, F., Dillingh, G., Bakker, A., & Prins, J. (2008). Suicidal thoughts among medical residents with burnout. Archives of Suicide Research, 12, 344–346.
Van Veldhoven, M., & Meijman, T. F. (1994). Het meten van psychosociale arbeidsbelasting met een vragenlijst: De Vragenlijst Beleving en Beoordeling van de Arbeid (VBBA) [The measurement of psychosocial strain at work: The questionnaire experience and evaluation of work]. Amsterdam: Nederlands Instituut voor Arbeidsomstandigheden.
Wallace, J. E., Lemaire, J. B., & Ghali, W. A. (2009). Physician wellness: A missing quality indicator. Lancet, 374, 1714–1721.
Wang, J.-N., Sun, W., Chi, T.-S., Wu, H., & Wang, L. (2010). Prevalence and associated factors of depressive symptoms among Chinese doctors: A cross-sectional survey. International Archives of Occupational and Environmental Health, 83, 905–911.
Ware, J. E., Kosinski, M., & Gandek, B. (2003). SF-36 Health Survey: Manual and interpretation guide. Lincoln, RI: QualityMetric Inc.
Warr, P. (2007). Work, happiness, and unhappiness. New York: Lawrence Erlbaum.
West, C. P., Dyrbye, L. N., Rabatin, J. T., Call, T. G., Davidson, J. H., Multari, A., et al. (2014). Intervention to promote physician well-being, job satisfaction, and professionalism: A randomized clinical trial. Journal of the American Medical Association-Internal Medicine, 174, 527–533.
West, C. P., Huschka, M. M., Novotny, P. J., Sloan, J. A., Kolars, J. C., Habermann, T. M., et al. (2006). Association of perceived medical errors with resident distress and empathy. Journal of the American Medical Association, 296, 1071–1078.
Wild, D., Grove, A., Martin, M., Eremenco, S., McElroy, S., Verjee-Lorenz, A., et al. (2005). Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR Task Force for translation and cultural adaptation. Value in Health, 8, 94–104.
Xanthopoulou, D., Bakker, A. B., Dollard, M. F., Demerouti, E., Schaufeli, W. B., Taris, T. W., et al. (2007). When do job demands particularly predict burnout? The moderating role of job resources. Journal of Managerial Psychology, 22, 766–786.
Yamazaki, S., Fukuhara, S., & Green, J. (2005). Usefulness of five-item and three-item mental health inventories to screen for depressive symptoms in the general population of Japan. Health and Quality of Life Outcomes, 3, 48.
Acknowledgements
The authors would like to thank the Editor-in-Chief and three anonymous reviewers for their constructive suggestions and helpful comments on an earlier version of this paper.
Conflict of Interest
Dr. Anagnostopoulos, Dr. Demerouti, Dr. Niakas, Dr. Sykioti, and Dr. Zis declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anagnostopoulos, F., Demerouti, E., Sykioti, P. et al. Factors Associated with Mental Health Status of Medical Residents: A Model-Guided Study. J Clin Psychol Med Settings 22, 90–109 (2015). https://doi.org/10.1007/s10880-014-9415-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-014-9415-2