Abstract
Post-traumatic stress disorder (PTSD) is a condition that can develop after experiencing a traumatic event. Psychoeducation is a treatment approach often used for mental health and PTSD. The aim of this systematic review and meta-analysis was to provide a comprehensive evaluation of randomized controlled trials (RCTs) of psychoeducational interventions for PTSD symptoms in adults. We systematically searched PubMed and Scopus databases for articles published from inception until October 2019. Eight studies that collectively included 719 subjects met the inclusion criteria. Random effects meta-analyses showed a small, neither statistically significant nor clinically important effect of − 0.08 (95% CI − 0.28 to 0.12). In addition, the I2 index was 56.9% indicating the presence of substantial heterogeneity. Findings can be considered preliminary and suggest that psychoeducation does not differ significantly from treatment-as-usual in decreasing PTSD symptoms but holds promise and should be further investigated. Suggestions for future research in the field are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Psychoeducation: Definition and Goals
Psychoeducation is the provision of systematic, relevant, and up-to-date information about an illness or condition (Motlova et al., 2017) offered by counselors and other mental health professionals (Bäuml et al., 2006). Psychoeducation can be defined “as a patient’s empowering training targeted at promoting awareness and proactivity, providing tools to manage, cope and live with a chronic condition and changing behaviours and attitudes related to the condition” (Colom, 2011, p. 339). Psychoeducation stresses empowerment and resilience (Whitworth, 2016) and facilitates a personally responsible handling of the illness (Bäuml et al., 2006). It is considered as a simple therapeutic intervention that can be easily integrated into the clinical environment (Colom, 2011), and its goal is to help people comprehend complex and emotionally loaded information and develop coping strategies (Lukens & McFarlane, 2004).
Psychoeducational interventions provide both disease-specific and general information, as well as skills training (Authier, 1977; Motlova et al., 2017). They may also target anxiety and depression, satisfaction with treatment, knowledge about the condition, resources, self-esteem, quality of life, and well-being (Lukens & McFarlane, 2004). Information might be shared individually or via a group format and can include presentations, assignments, video, online and written material. Some researchers have acknowledged the heterogeneity between psychoeducational interventions in the field of traumatic stress (Krupnick & Green, 2008).
Why Psychoeducation for Trauma
Mental health professionals started using psychoeducation in trauma contexts around the late nineties (Bonsack et al., 2015). Psychoeducation now forms part of different but empirically supported therapies for the treatment of PTS (Gentry et al., 2017; Schnyder et al., 2015; Whitworth, 2016) and is usually delivered in their initial phases.
Research shows that informing people about the consequences of traumatic events on their psychological status offers them a cognitive frame to process their experience and understand their symptoms as normal reactions to trauma (Krupnick & Green, 2008; Phoenix, 2007), thus protecting their self-esteem and giving them a sense of control on their symptoms by teaching them coping strategies (Phoenix, 2007). To that extend, psychoeducation is crucial in the first stage of trauma recovery, that of safety and stabilization (Herman, 2015), when problems related to the trauma history are identified, expectations for treatment are defined, and coping skills to deal with painful memories are taught (Phoenix, 2007). Psychoeducation can serve as a useful tool for battling against the natural tendency to avoid recognizing and confronting fear-conditioned memories (Southwick et al., 2008), which is very common among traumatized people. Psychoeducation also has the potential to prevent or ameliorate chronic post-traumatic stress disorder (PTSD), by helping patients or their family to recognize the signs and seek help (Southwick et al., 2008).
Psychoeducation can be delivered at different time points, before a potentially traumatic event, right after the event for those affected, or later for those who manifest post-traumatic symptoms (Creamer & O'Donnell, 2008). Moreover, patients provide positive appraisals for psychoeducation (Mills et al., 2014; Pratt et al., 2005) and evaluate it as useful and easy to understand (Pratt et al., 2005). Thus, psychoeducation seems an appropriate therapeutic option for mental health professionals to use in trauma contexts.
Psychoeducation for Trauma: Content and Communication
The psychoeducational content for trauma usually consists of information about the nature and the progress of post-traumatic reactions, ways to deal with the trauma-reminding stimuli and strategies to cope with the symptoms (Schnyder et al., 2015) and feelings of depression, anger, guilt, and shame (Krupnick & Green, 2008). In addition, information is included regarding when someone should reach for help and the type of specialist that can help (Krupnick & Green, 2008). When psychoeducation is offered as part of a more complex treatment regimen, its role also consists of informing patients about the therapeutic procedures, so they can form realistic expectations (Phoenix, 2007).
Some psychoeducational interventions include the use of leaflets that contain easily understood information depending on the target group. However, the mere offer of a leaflet or the provision of general guidelines only is not the most recommendable way to provide psychoeducation (Colom, 2011). A therapeutic discussion can ensure that the patient will not reach wrong conclusions and believe that they are dysfunctional. For this reason, communication of the content is best done in an interactive way, with ample time for questions (Motlova et al., 2017) and the creation of a supportive relationship between the client and the specialist is paramount (Whitworth, 2016).
Part of a psychoeducational intervention is also teaching participants general or specific skills (Authier, 1977). This skills training element is considered as one of the most important features of psychoeducation, which accounts for its effectiveness (Authier, 1977). Hobfol et al., (2008) indicated that training tools that illustrate complex behavior, encourage practice, and use successive approximation to enhance skills should be part of psychoeducation. However, the goals should be realistic; therefore, trying to educate people on too many skills during a short psychoeducational program might be an exaggeration (Bäuml et al., 2006).
Psychoeducation for Trauma: Preliminary Evidence
Various psychoeducational interventions have been implemented in different populations exposed to trauma with positive preliminary results, such as decreased PTS and depression symptoms (e.g., Ball et al., 2013; Im et al., 2018; Roe-Sepowitz et al., 2014; Rowe et al., 2014). Adding psychoeducation to a medication intervention for earthquake survivors resulted in greater decrease in anxiety and PTS symptoms, as well as decreased avoidance and increased problem-solving scores (Oflaz et al., 2008).
Trauma-informed psychoeducational interventions have produced increases in knowledge about trauma and PTSD and high levels of satisfaction (Pratt et al., 2005), increased alcohol retention (Odenwald & Semrau, 2012), decreases in PTSD symptom severity (Mills et al., 2014), and positive results on psychosocial factors, such as sense of community, social support, and mental health awareness (Im et al., 2018).
A series of psychoeducational interventions for veterans also produced some positive results, such as increases in PTSD knowledge and skills, improved family functioning and symptom status (Fischer et al., 2013), decreases in reactivity to criticism (Interian et al., 2016), and improvements in attitudes about PTSD, stress, and help-seeking (Gould et al., 2007). Also a short video-based psychoeducational intervention was deemed feasible and cost-effective for female sexual assault survivors (Miller et al., 2015). These preliminary findings, despite their limitations, suggest that psychoeducation has beneficial effects on traumatized people.
Purpose of the Study
Southwick et al. (2008) recognized that psychoeducation has become a widely used but poorly studied intervention in the field of traumatic stress. Other researchers also agreed that the evidence was insufficient to determine its effectiveness and called for more rigorous assessments (Ruzek, 2008; Wessely et al., 2008). In this direction, the purpose of this study was (1) to identify psychoeducational interventions for PTS and record their content and (2) to assess scientific evidence regarding the effectiveness of psychoeducation in alleviating PTS symptoms in adults under the format of a systematic review and meta-analysis.
Method
Types of Interventions
We defined as psychoeducational any intervention applied to adults that (1) provided information about and ways to cope with PTS in a structured way, (2) was described as psychoeducational per se, and (3) the psychoeducational component was the dominant component of the intervention. We applied these criteria based on Creamer and O’Donnell’s (2008) suggestion to evaluate psychoeducation in isolation rather than in conjunction with active elements of other interventions, to better understand its impact. As a first step to systematically assess psychoeducation we thought that merging too different concepts would seriously challenge the results’ interpretation.
Types of Studies and Participants
We considered randomized RCT that included adult populations and compared a psychoeducational intervention to a control group (TAU, waitlist, or placebo).
Types of Outcomes
The primary outcome was reduction in PTSD symptoms in standardized tests.
Review Inclusion/Exclusion Criteria
We considered the following eligibility criteria: (1) type of study was RCT, (2) age of participants > 18 years old, (3) participants had experienced a potentially traumatic event, (4) described a psychoeducational intervention as defined earlier, (5) outcomes reported included PTSD total scores, and (6) sufficient statistical information was provided to calculate effect sizes. Diagnosis of PTSD was not a requirement.
Literature Search
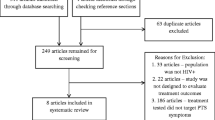
We searched the following online databases, PubMed and Scopus, from inception until 30 of October 2019, without restrictions in language, to identify articles describing psychoeducational interventions for PTS symptoms in adults. Combinations of the following keywords were used: psychoeducation*, posttraumatic stress*, PTSD*, posttraumatic stress disorder*, intervention*. We reviewed abstracts of 526 identified articles, 8 of these satisfied the eligibility criteria, resulting in a final sample of 719 participants. A flow diagram of the procedure followed in this study for the identification and inclusion of articles is presented in Fig. 1.
Assessment of Risk of Bias in Included Studies
We assessed Risk of Bias (RoB) for each of the studies included in the meta-analysis based on the Cochrane risk of bias criteria described in the Cochrane Handbook for Systematic Reviews of Interventions, with ratings of “low risk”, “high risk” and “unclear risk” for the six domains of the tool; (1) sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding of participants and personnel (performance bias), (4) incomplete outcome data (attrition bias), (5) selective outcome reporting (reporting bias), and (6) blinding of outcome assessment (detection bias) (Higgins et al., 2011).
Studies with low risk of selection bias adequately described the sequence generation and the concealment of treatment group allocation. Due to the psychological nature of the interventions, blinding of either participants or personnel delivering the treatments was unclear in most of the studies. Detection bias was not assessed in this meta-analysis as outcome assessments in almost all studies were conducted through self-reports of participants. The assessment of attrition bias was based on whether the involved studies thoroughly described withdrawals and drop-outs (Table 1).
Analyses
We calculated the standardized mean difference between intervention and control groups using Cohen’s d estimate. An effect size smaller than 0.20 is considered small, 0.20–0.50 represents a medium effect, and larger than 0.80 a large effect (Cohen, 1992).
We used a random-effects model, which is preferable and more realistic to fixed-effects model when heterogeneity is expected (Nikolakopoulou et al., 2014). Based on other reviews about psychoeducation (e.g., Lukens & McFarlane, 2004) which highlight the differences between the interventions regarding content, duration, and intensity, we expected considerable heterogeneity. We used the I2 index to express the proportion of variability that is due to heterogeneity rather than sampling error, with values larger than 50% indicating the presence of heterogeneity (Deeks et al., 2011). In all our analyses we used Stata 13 (StataCorp, 2013) and more specifically the metan command (Chaimani et al., 2014; Harris et al., 2008).
Results
Systematic Review
Characteristics of the Studies
Data from 8 studies comparing psychoeducation to TAU or waitlist were included in this meta-analysis. The characteristics of the studies are summarized in Table 2. The interventions had different target groups, affirming the fact that psychoeducation can be tailored to the needs of people with different conditions (Bäuml et al., 2006).
Apart from evaluating PTS symptoms, all studies in this meta-analysis also evaluated anxiety and depression (e.g., Als et al., 2015) or emotional/psychological distress (e.g., Ghafoori et al., 2016). Psychoeducational interventions commonly address anxiety and depression regardless of the problem. Five studies had the intervention delivered individually (e.g., Scholes et al., 2007), while three used a group format (e.g., Kaslow et al., 2010).
Two studies involved a single session intervention of 20–30 (Shipherd et al., 2016) or 90 min (Ghafoori et al., 2016). Two others provided psychoeducation via self-help booklets (Scholes et al., 2007; Turpin et al., 2005). In contrast, two studies ensured therapist contact by supporting the intervention with a telephone call (Als et al., 2015) or assigning homework to participants and providing feedback (Sveen et al., 2017). In two studies the intervention consisted of more sessions; 6 weekly modules accessed via a secure website (Sveen et al., 2017), and 10 meetings, including check-ins, structured discussions, and activities (Kaslow et al., 2010).
Information was given on: (1) common reactions to trauma or to the specific condition (e.g. Sveen et al., 2017; Turpin et al., 2005), (2) PTSD, i.e. development, symptoms, treatment, (Als et al., 2015), (3) coping strategies- ranging from advice to skills-training- (e.g. Turpin et al., 2005; Yeomans et al., 2010), (4) sources of further support (Als et al., 2015; Turpin et al., 2005) or referral (Ghafoori et al., 2016). Other topics addressed were learning difficulties (Als et al., 2015), intrusive cognitions (Shipherd et al., 2016), burns, stress and sleep, and family communication (Sveen et al., 2017), spouse abuse, suicide, safety planning, risk, and protective factors (Kaslow et al., 2010), rationale of exposure therapy and barriers to treatment (Ghafoori et al., 2016), themes of trauma, loss, anger, trust, and the roots of violence (Yeomans et al., 2010). Two studies explicitly mentioned normalization as a goal (Shipherd et al., 2016; Turpin et al., 2005) and another two studies tried to foster the links to community (Kaslow et al., 2010; Yeomans et al., 2010).
Participants’ Appraisals of Psychoeducation
Five studies included information on participants’ perceptions of psychoeducation. According to these, psychoeducation was deemed by most participants as useful (e.g., Als et al., 2015), informative, comprehensible, meaningful, and supportive (Sveen et al., 2017). Participants stated that the information made them feel more prepared for life after the traumatic event (82%) and less anxious or concerned (77%) (Als et al., 2015). They evaluated as particularly helpful the provision of information and advice (47%), the normalization of reactions (32%) (Turpin et al., 2005), and the coping techniques learned (Sveen et al., 2017). The majority found the psychological sequelae and the coping strategies section of the booklet useful (Scholes et al., 2007). Ghafoori et al. (2016) also detected a 19.1% increase in reported mental health service engagement.
Participants made positive statements, i.e. that the program had made the situation better (Sveen et al., 2017). Half of them reported that the program had helped them with their problems, emphasizing the chance to process and talk about the incident again and to learn skills for doing so with others. Few participants found the program upsetting or boring, time-consuming and some felt they had insufficient time.
Effect of Psychoeducation on PTS Symptoms
Data analysis from the included studies revealed a small effect size (SMD = − 0.08, 95% CI − 0.28 to 0.12, τ2 = 0.0408, z = 0.77, p = 0.441). However, the inspection of the 95% predictive interval (95% CI − 0.28 to 0.12) suggests that a future study may be in either direction. Therefore, the effect of psychoeducation in reducing PTS symptoms remains unclear. The level of heterogeneity was substantial (I2 = 56.9%, p = 0.023), as also seen from the forest plot in Fig. 2 and the heterogeneity variance estimate (τ2 = 0.0408).
Publication Bias and Small Study Effects
Small study effects (smaller studies showing systematically larger effects compared to large studies) were investigated in the study through a funnel plot, which revealed that the studies were symmetrically distributed; therefore, there is no indication of small study effects (Fig. 3). The Egger’s test held similar results (Coef. = − 0.927, Sd. Error = 1.06, p = 0.414). Small-study effects are typically used as a proxy for publication bias (Mavridis & Salanti, 2014). With only eight studies we lack power to detect the phenomenon of small-study effects.
Discussion
The results of the present study are in line with previous reviews regarding psychoeducation for post-traumatic stress (Wessely et al., 2008; Whitworth, 2016), which highlight the ambiguity between the findings of different studies. Our review suggests that psychoeducation is a flexible and well-received treatment option that can be adjusted to different environments and populations. However, the overall effect for psychoeducation for decreasing PTSD symptoms was small and the meta-analysis failed to detect a clear difference between psychoeducation and TAU in PTS symptom reduction. The reasons for this are further discussed below.
Limitations
First, some methodological limitations must be acknowledged, such as the small number of included studies. It is possible that a wider search would result in more studies. Even though we did not set any restrictions regarding language, all studies were in English. Another limitation is the considerable heterogeneity between the interventions. They varied in terms of their characteristics (e.g., duration and dosage, delivery mode, settings, content, sample, and type of trauma). Heterogeneity was addressed by applying the random-effects model in the analysis, but it was not explored due to the small sample of the studies. Third, psychoeducation was tested against TAU and waitlist in total. The examination of each category separately might have held different results.
Suggestions to Improve Psychoeducation
When the content of the interventions was examined, a debate emerged as to whether psychoeducation includes skills-training (and to what extent) or consists of information only. Based on the literature review, it should include both, but in practice it equals mostly to information. This occurs especially when psychoeducation serves as the control group for another intervention to be tested (e.g., Morland et al., 2019), even though skills-training is considered an important feature of psychoeducation (Authier, 1977; Motlova et al., 2017; Hobfol et al., 2008).
In the studies included in the meta-analysis, one study explicitly taught relaxation techniques (Yeomans et al., 2010), another included instructions for selected techniques (Sveen et al., 2017), one provided structured proactive advice based on cognitive-behavioral strategies (Scholes et al., 2007), and three studies contained advice on managing the situation (e.g., Als et al., 2015). The authors conclude that more emphasis should be placed on teaching skills, as part of psychoeducation. This suggestion is particularly useful for counselors, as it will help them attend to their clients’ needs more efficaciously. Along with skills-training, a trustful relationship with the specialist and the consideration of cultural factors (Ruzek, 2008) are considered prerequisites for a psychoeducational intervention.
Implications for Research and Practice
A set of factors is crucial in determining the level of effectiveness of psychoeducation in alleviating PTS symptoms. By examining the included studies, a possible assumption could be that when participants’ traumatization cannot be attributed solely to one specific event or trauma type, then psychoeducation does not seem to be effective (e.g., Ghafoori et al., 2016; Yeomans et al., 2010). When participants vary a lot between them, a positive effect cannot be easily detected. Another possibility might be that solely one psychoeducational session is inefficient to reduce PTS symptoms. One session could make participants more conscious of their symptoms, but without providing them enough time for normalization to be achieved (e.g., Ghafoori et al., 2016; Yeomans et al., 2010).
In contrast, when participants exhibit the same type of trauma and the intervention is simple but supported by therapist contact (e.g., Als et al., 2015; Sveen et al., 2017) there is a tendency to report less PTS symptoms. In a population difficult to reach, such as parents of hospitalized children, passive psychoeducation supported by therapist contact seems to be beneficial. However, the provision of psychoeducation booklets does not seem effective in reducing PTS symptoms in hospitalized adults (Scholes et al., 2007; Turpin et al., 2005).
It is possible that certain groups of participants might benefit more from other well-established treatment options, such as exposure therapy. Even in that case, it would be of great interest to examine the role of psychoeducation as adjunctive part of such a treatment. Another important issue that needs to be highlighted is the positive appraisals that psychoeducation receives from participants (e.g., Mills et al., 2014). This should not be disregarded, given the difficulties that arise in trauma contexts. Psychoeducation certainly seems to address some of people’s needs in a pleasant way.
Moreover, participants in the included studies did not have a diagnosis of PTSD but were at risk of manifesting PTS symptoms because they had experienced potentially traumatic events. Although they reported symptoms, in lack of a PTSD diagnosis, the role of psychoeducation in these interventions can be considered preventive. Results might have been different if participants had PTSD. This could be another area of future investigation.
Finally, the overall result is confounded by several factors, such as methodological, process factors, as well as sample characteristics. Future research should address this issue by taking these factors into account (Creamer & O’Donnell, 2008; Krupnick & Green, 2008; Southwick et al., 2008). Their effect could explain why some forms of psychoeducation are effective while others are not or why it is effective for some people and for who (Kilpatrick et al., 2008; Lukens & McFarlane, 2004). This information would be very valuable for counselors, as it would allow them to tailor their intervention accordingly.
Conclusions
The promising preliminary results of psychoeducation for trauma in areas of interest, apart from PTS symptom alleviation, and the inconclusive results of the present study should prompt researchers to keep investigating until they figure out the correct formulas that work for different people. The authors agree with Ruzek (2008) that psychoeducation can be improved by revising its goals and by creating clear and realistic expectations grounded in a theory about providing information in the context of trauma. In fact, this will allow professionals to use psychoeducation more efficaciously as a tool to meet the unique set of client needs. The authors call for more RCTs testing the effectiveness of different forms of psychoeducation in different populations that will surpass the limitations of previous research.
Data Availability
The data that support the findings of this study are available from the corresponding author [VCB], upon reasonable request.
Code availability
Not applicable.
References
Studies with an asterisk are included in the meta-analysis
Acevedo-Ibarra, J. N., Juárez-García, D. M., Espinoza-Velazco, A., & Buenaventura-Cisneros, S. (2019). Cognitive behavioral stress management intervention in Mexican colorectal cancer patients: Pilot study. Psycho-Oncology, 28(7), 1445–1452. https://doi.org/10.1002/pon.5094
*Als, L. C., Nadel, S., Cooper, M., Vickers, B., & Garralda, M. E. (2015). A supported psychoeducational intervention to family mental health following discharge from pediatric intensive care: Feasibility and pilot randomized control trial. British Medical Journal Open. https://doi.org/10.1136/bmjopen-2015-009581
Authier, J. (1977). The psychoeducation model: Definition, contemporary roots, and content. Canadian Counselor, 12(1), 15–22.
Ball, S., Karatzias, T., Mahoney, A., Ferguson, S., & Pate, K. (2013). Interpersonal trauma in female offenders: A new, brief, group intervention delivered in a community-based setting. The Journal of Forensic Psychiatry & Psychology, 24(6), 795–802. https://doi.org/10.1080/14789949.2013.852233
Bäuml, J., Froböse, T., Kraemer, S., Rentrop, M., & Pitschel-Walz, G. (2006). Psychoeducation: A basic psychotherapeutic intervention for patients with schizophrenia and their families. Schizophrenia Bulletin, 32(1), S1–S9. https://doi.org/10.1093/schbul/sbl017
Bonsack, C., Rexhaj, S., & Favrod, J. (2015). Psychoeducation: Definition, historique, interet et limites. Annales Medico-Psychologiques, 173(1), 79–84. https://doi.org/10.1016/j.amp.2014.12.001
Chaimani, A., Mavridis, D., & Salanti, G. (2014). A hands-on practical tutorial on performing meta-analysis with Stata. Evidence Based Mental Health, 17(4), 111–116. https://doi.org/10.1136/eb-2014-101967
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. https://doi.org/10.1037/0033-2909.112.1.155
Colom, F. (2011). Keeping therapies simple: Psychoeducation in the prevention of relapse in affective disorders. The British Journal of Psychiatry, 198(5), 338–340. https://doi.org/10.1192/bjp.bp.110.090209
Creamer, M., & O’Donnell, M. (2008). The pros and cons of psychoeducation following-trauma: Too early to judge? Psychiatry Interpersonal and Biological Processes, 71(4), 319–321. https://doi.org/10.1521/psyc.2008.71.4.319
Deeks, J. J., Higgins, J. P. T., & Altman, D. G. (2011). Analyzing data and undertaking meta-analyses. In J. P. T. Higgins, & S. Green (Eds.), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. www.handbook.cochrane.org.
Eichfeld, C., Farrell, D., Mattheβ, M., Bumke, P., Sodemann, U., Ean, N., & Mattheß, H. (2019). Trauma stabilization as a sole treatment intervention for post-traumatic stress disorder in Southeast Asia. Psychiatric Quarterly, 90(1), 63–88. https://doi.org/10.1007/s11126-018-9598-z
Fischer, E. P., Sherman, M. D., Han, X., & Owen, R. R. (2013). Outcomes of participation in the REACH multifamily group program for veterans with PTSD and their families. Professional Psychology: Research and Practice, 44(3), 127–134. https://doi.org/10.1037/a0032024
Gentry, J. E., Baranowsky, A. B., & Rhoton, R. (2017). Trauma competency: An active ingredients approach to treating posttraumatic stress disorder. Journal of Counseling & Development, 95(3), 279–287. https://doi.org/10.1002/jcad.12142
*Ghafoori, B., Fisher, D., Korosteleva, O., & Hong, M. (2016). A randomized, controlled pilot study of a single-session psychoeducation treatment for urban, culturally diverse, trauma-exposed adults. The Journal of Nervous and Mental Disease, 204(6), 421–430. https://doi.org/10.1097/NMD.0000000000000512
Goldman, C. R. (1988). Toward a definition of psychoeducation. Hospital and Community Psychiatry, 39(6), 666–668. https://doi.org/10.1176/ps.39.6.666
Gould, M., Greenberg, N., & Hetherton, J. (2007). Stigma and the military: Evaluation of a PTSD psychoeducational program. Journal of Traumatic Stress, 20(4), 505–515. https://doi.org/10.1002/jts.20233
Harris, R. J., Deeks, J. J., Altman, D. G., Bradburn, M. J., Harbord, R. M., & Sterne, J. A. C. (2008). Metan: Fixed- and random-effects meta-analysis. The Stata Journal, 8(1), 3–28. https://doi.org/10.1177/1536867X0800800102
Herman, J. L. (2015). Trauma and recovery: The aftermath of violence – from domestic abuse to political terror. Basic Books.
Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., & Sterne, J. A. C. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. https://doi.org/10.1136/bmj.d5928
Hobfol, E. E., Walter, K. H., & Horsey, J. K. (2008). Dose and fit are vital to intervention success. Psychiatry, 71(4), 308–318. https://doi.org/10.1521/psyc.2008.71.4.308
Im, H., Jettner, J. F., Warsame, A. H., Isse, M. M., Khoury, D., & Ross, A. I. (2018). Trauma-informed psychoeducation for Somali refugee youth in urban Kenya: Effects on PTSD and psychosocial outcomes. Journal of Child and Adolescent Trauma, 11(4), 431–441. https://doi.org/10.1007/s40653-017-0200-x
Interian, A., Kline, A., Perlick, D., Dixon, L., Feder, A., Weiner, M. D., Goldstein, M. F., Hennessy, K., Hill, L. S., & Losonczy, M. (2016). Randomized controlled trial of a brief Internet-based intervention for families of veterans with posttraumatic stress disorder. Journal of Rehabilitation Research & Development, 53(5), 629–640. https://doi.org/10.1682/JRRD.2014.10.0257
*Kaslow, N. J., Leiner, A. S., Reviere, S., Jackson, E., Bethea, K., Bhaju, J., Rhodes, M., Gantt, M. J., Senter, H., & Thompson, M. P. (2010). Suicidal, abused African American women’s response to a culturally informed intervention. Journal of Consulting and Clinical Psychology, 78(4), 449–458. https://doi.org/10.1037/a0019692
Kilpatrick, D. G., Cougle, J. R., & Resnick, H. S. (2008). Reports of the death of psychoeducation as a preventative treatment for posttraumatic psychological distress are exaggerated. Psychiatric, 71(4), 322–328. https://doi.org/10.1521/psyc.2008.71.4.322
Krupnick, J. L., & Green, B. L. (2008). Psychoeducation to prevent PTSD: A paucity of evidence. Psychiatric, 71(4), 329–331. https://doi.org/10.1521/psyc.2008.71.4.329
Lukens, E. P., & McFarlane, W. R. (2004). Psychoeducation as evidenced-based practice: Considerations for practice, research, and policy. Brief Treatment and Crisis Intervention, 4(3), 205–225. https://doi.org/10.1093/brief-treatment/mhh019
Miller, K. E., Cranston, C. C., Davis, J. L., Newman, E., & Resnick, H. (2015). Psychological outcomes after a sexual assault video intervention: A randomized trial. Journal of Forensic Nursing, 11(3), 129–136. https://doi.org/10.1097/JFN.0000000000000080
Mills, K. L., Ewer, P., Dore, G., Teesson, M., Baker, A., Kay-Lambkin, F., & Sannibale, C. (2014). The feasibility and acceptability of a brief intervention for clients of substance use services experiencing symptoms of post traumatic stress disorder. Addictive Behaviors, 39(6), 1094–1099. https://doi.org/10.1016/j.addbeh.2014.03.013
Morland, L., Macdonald, A., Grubbs, K. M., Mackintosh, M. A., Monson, C., Glassman, L., & Glynn, S. (2019). Design of a randomized superiority trial of a brief couple treatment for PTSD. Contemporary Clinical Trials Communications. https://doi.org/10.1016/j.conctc.2019.100369
Motlova, L. B., Balon, R., Beresin, E. V., Brenner, A. M., Coverdale, J., & H., Guerrero, A. P. S., Louie, A. K., & Roberts, L. W. (2017). Psychoeducation as an opportunity for patients, psychiatrists, and psychiatric educators: Why do we ignore it?. Academic Psychiatry, 41, 447–451. https://doi.org/10.1007/s40596-017-0728-y
Nikolakopoulou, A., Mavridis, D., & Salanti, G. (2014). Demystifying fixed and random effects meta-analysis. Evidence Based Mental Health, 17(2), 53–57. https://doi.org/10.1136/eb-2014-101795
Odenwald, M., & Semrau, P. (2012). Reducing dropout among traumatized alcohol patients in detoxification treatment: A pilot intervention study. European Addiction Research, 18(2), 54–63. https://doi.org/10.1159/000333336
Oflaz, F., Hatipoğlu, S., & Aydin, H. (2008). Effectiveness of psychoeducation intervention on post-traumatic stress disorder and coping styles of earthquake survivors. Journal of Clinical Nursing, 17(5), 677–687. https://doi.org/10.1111/j.1365-2702.2007.02047.x
Phoenix, B. J. (2007). Psychoeducation for survivors of trauma. Perspectives in Psychiatric Care, 43(3), 123–131. https://doi.org/10.1111/j.1744-6163.2007.00121.x
Pratt, S. I., Rosenberg, S., Mueser, K. T., Brancato, J., Salyers, M., Jankowski, M. K., & Descamps, M. (2005). Evaluation of a PTSD psychoeducational program for psychiatric inpatients. Journal of Mental Health, 14(2), 121–127. https://doi.org/10.1080/09638230500066356
Roe-Sepowitz, D. E., Bedard, L. E., Pate, K. N., & Hedberg, E. C. (2014). Esuba: A psychoeducation group for incarcerated survivors of abuse. International Journal of Offender Therapy and Comparative Criminology, 58(2), 190–208. https://doi.org/10.1177/0306624X12465410
Rowe, H., Sperlich, M., Cameron, H., & Seng, J. (2014). A quasi-experimental outcomes analysis of a psychoeducation intervention for pregnant women with abuse-related posttraumatic stress. Journal of Obstetric Gynecologic & Neonatal Nursing, 43(3), 282–293. https://doi.org/10.1111/1552-6909.12312
Ruzek, J. I. (2008). Wanted: A theory of post-trauma information delivery. Psychiatric, 71(4), 332–338. https://doi.org/10.1521/psyc.2008.71.4.332
Schnyder, U., Ehlers, A., Elbert, T., Foa, E. B., Gersons, B. P. R., Resich, P. A., & Cloitre, M. (2015). Psychotherapies for PTSD: What do they have in common? European Journal of Psychotraumatology. https://doi.org/10.3402/ejpt.v6.28186
*Scholes, C., Turpin, G., & Mason, S. (2007). A randomized controlled trial to assess the effectiveness of providing self-help information to people with symptoms of acute stress disorder following a traumatic injury. Behaviour Research and Therapy, 45(11), 2527–2536. https://doi.org/10.1016/j.brat.2007.06.009
*Shipherd, J. C., Salters-Pedneault, K., & Fordiani, J. (2016). Evaluating postdeployment training for coping with intrusive cognition: A comparison of training approaches. Journal of Consulting and Clinical Psychology, 84(11), 960–971. https://doi.org/10.1037/ccp0000136
Southwick, S., Friedman, M., & Krystal, J. (2008). Does psychoeducation helps prevent posttraumatic psychological distress? In reply. Psychiatry, 71(4), 303–307. https://doi.org/10.1521/psyc.2008.71.4.303
StataCorp. (2013). Stata Statistical Software (Release 13) [Computer software]. StataCorp. https://www.stata.com/.
*Sveen, J., Andersson, G., Buhrman, B., Sjöberg, F., & Wllebrand, M. (2017). Internet-based information and support program for parents of children with burns: A randomized controlled trial. Burns, 43(3), 583–591. https://doi.org/10.1016/j.burns.2016.08.039
*Turpin, G., Downs, M., & Mason, S. (2005). Effectiveness of providing self-help information following acute traumatic injury: Randomized controlled trial. British Journal of Psychiatry, 187(1), 76–82. https://doi.org/10.1192/bjp.187.1.76
Wessely, S., Bryant, R. A., Greenberg, N., Earnshaw, M., Sharpley, J., & Hacker Hughes, J. (2008). Does psychoeducation helps prevent posttraumatic psychological distress? Psychiatry, 71(4), 287–302. https://doi.org/10.1521/psyc.2008.71.4.287
Whitworth, J. D. (2016). The role of psychoeducation in trauma recovery: Recommendations for content and delivery. Journal of Evidence-Informed Social Work, 13(5), 442–451. https://doi.org/10.1080/23761407.2016.1166852
*Yeomans, P. D., Forman, E. M., Herbert, J. D., & Yuen, E. (2010). A randomized trial of a reconciliation workshop with and without PTSD psychoeducation in Burundian sample. Journal of Traumatic Stress, 23(3), 305–312. https://doi.org/10.1002/jts.20531
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethics approval was not required for this type of study.
Consent to participate
Formal consent was not required for this type of study.
Consent for publication
Formal consent was not required for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brouzos, A., Vatkali, E., Mavridis, D. et al. Psychoeducation for Adults with Post-Traumatic Stress Symptomatology: A Systematic Review and Meta-Analysis. J Contemp Psychother 52, 155–164 (2022). https://doi.org/10.1007/s10879-021-09526-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10879-021-09526-3