Abstract
This article discusses demoralization in patients with chronic pain and the role of psychotherapy at combating chronic demoralization associated with chronic pain. The advantages of the biopsychosocial conceptual framework for the understanding of chronic pain are highlighted. Demoralization may be viewed as a combination of distress and subjective incompetence. While the distress experienced by the patient may be understandable and commensurate to the predicament, the co-occurrence of subjective incompetence (the polar opposite of resilience) and its escalation to helplessness, and hopelessness may result in suicidal attempts, demands for euthanasia, or death by suicide. The complexity of chronic pain and its relationship to demoralization may be examined from multiple perspectives. Biological, psychological, social and cultural variables play varying roles depending on the observer’s perspective and the context of the observation. The role of psychotherapy in chronic pain may be viewed in terms of multiple pathways through which language, cognitive style, behavior, relationships, attitude towards pain, and awareness of the body modify the relative influences of top-down and bottom-up processing of information within the pain neuromatrix. Various psychotherapeutic interventions developed for patients with chronic pain are reviewed and recommendations are made for future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pain has been defined as “pain that persists 6 months after an injury, and beyond the usual course of an acute disease, or a reasonable time for a comparable injury to heal; that is associated with chronic pathologic processes causing continuous or intermittent pain for months or years; and that may continue in the presence or absence of demonstrable pathologies, may not be amenable to routine pain control methods, and healing may never occur”. (Machikanti et al. 2009). In the United States, prevalence estimates for chronic pain in adults range from 2 to 40 % with a median point prevalence of 15 %. (Hardt et al. 2008).
Historically, pain has been characterized as “peripheral nociceptive”, “peripheral neuropathic”, and a disturbance in pain processing in the central nervous system, called “central neuropathic or centralized pain”, found in fibromyalgia, irritable bowel syndrome, tension headache, and temporomandibular joint disease. Recent research, however, points to multiple potential mechanisms, peripheral and central, for chronic pain, leading to the designation of “mixed pain states”, typically found in low back pain but also documented in other pain conditions (Clauw 2014).
For centuries, clinicians and researchers in the Western world interpreted symptoms such as pain as a result of a specific disease state derived from observable pathology, and directed treatment at correcting the underlying physical disturbance. This biomedical conceptual framework (incorrectly called biomedical “model”) predicted that once the physical disturbance was corrected, the psychological and social difficulties associated with symptoms would disappear.
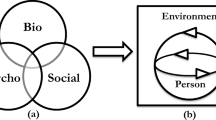
The biomedical framework failed to explain several clinical observations on chronic pain. First, disparities may exist between the observable pathology and the severity of pain and its associated psychological distress and disability. The fear of the patient may be disproportionate to the severity of the observed pathology. The results of the laboratory investigations and imaging studies may be unremarkable or inconsistent with the symptoms. Symptoms may persist after the pathology is treated and patients with identical observable pathologies may report different pain experiences. Among patients with chronic pain, these disparities, persistence, and individual differences are commonly found in conditions such as back pain, fibromyalgia, headache, and temporomandibular disorders. Limitations such as these led to a shift away from the biomedical framework to a more inclusive biopsychosocial framework (Turk and Monarch 2002).
A critical task in clinical psychiatry is the recognition of the link between the data collected on a patient and the facts about that patient upon which a treatment plan is built. Known as “formulation”, this step in the diagnostic process allows the psychiatrist to organize the data, make sense of the clinical presentation, and prescribe the appropriate interventions. Being only a proposal for a “paradigm shift”, the biopsychosocial framework did not offer any specific guidance on how to arrive at a formulation. This important gap was filled by McHugh and Slavney (1998) who proposed a comprehensive and integrative approach to the understanding of mental disorders in terms of four perspectives, each the legacy of an intellectual tradition: the perspectives of diseases, behaviors, dimensions (intelligence and personality), and life stories. Research elucidates which perspective or combination of perspectives best accounts for a clinical presentation. By interpreting the clinical presentation from each perspective, recognizing the limitations of each, and separating the relevant information from the irrelevant, an integrated and comprehensive model is built. This model is a set of scientific (i.e., falsifiable) hypotheses logically leading to an individualized treatment plan.
Understanding Demoralization
It is well known that the experience of chronic pain can be demoralizing. But what is demoralization and what role does it play in aggravating, perpetuating, or predisposing to the pain experience?
The term “demoralization” was introduced in 1961 by Frank. He demonstrated that demoralization is “the chief problem of all patients who come to psychotherapy” and that “the effectiveness of all psychotherapeutic schools lies in their ability to restore patient morale”. According to Frank, demoralization is “the state of mind of a person deprived of spirit or courage, disheartened, bewildered, and thrown into disorder or confusion” (Frank and Frank 1991).
How can we distinguish demoralization from depression? According to Klein, while demoralization involves a loss of anticipatory pleasure but not of consummatory pleasure, both anticipatory and consummatory pleasures are lost in major depressive disorder (Klein et al. 1980 p. 230–231). Research has shown, however, that depression and demoralization may or may not co-exist (See, for example, Clarke et al. 2005; Mangelli et al. 2005; and Guidi et al. 2011). The ability to experience and exhibit a full range of affect, or to experience pleasure in meaningful activities, or to function well when demands are not placed cannot help us recognize the presence or absence of demoralization in patients with major depressive disorder in whom anhedonia is part of their disorder.
Depression may be distinguished from demoralization by conceptualizing motivation as involving a magnitude and a direction. A patient who is depressed but not demoralized has the sense of direction, i.e., knows what needs to be done to reduce or get out of the predicament, but lacks the magnitude of motivation, the “will power” as it is called in common parlance, that leads him or her to initiate the appropriate behaviors. The converse is true of a patient who is demoralized but not depressed. A demoralized person is more than willing to get out of the predicament but has lost the cognitive map to overcome the stressful situation. Contrasting with the persistence of the depressed mood of a patient with major depressive disorder, the mood of a demoralized patient is context sensitive and may brighten up rather rapidly if circumstances improve, encouragement is received, or self-control is regained (de Figueiredo 1993). Demoralization is not the same as “adjustment disorder”. This diagnosis was introduced in DSM-III and maintained in subsequent editions of the DSM but the latest edition (DSM-5) changed the definition of this diagnosis to “development of emotional or behavioral symptoms in response to an identifiable stressor” and re-classified by placing it among stress-related disorders. The pre-DSM-5 diagnosis of “adjustment disorder” had low reliability and questionable validity (Grassi et al. 2007; Semprini et al. 2010; de Figueiredo 2013) and the reliability and validity of the new definition proposed in DSM-5 is unknown.
Further characterization of demoralization presented it as involving two components, distress and subjective incompetence (SI) (de Figueiredo 2011). By generalizing and modifying slightly a definition proposed for cancer patients, distress may be defined as follows: “An unpleasant emotional experience of a psychological, social, and/or spiritual nature that may interfere with the ability to cope effectively with a stressful situation” (National Comprehensive Cancer Network 2003). Distress is broader in scope than fear or catastrophizing, including a wide range of feelings that characterize the clinical presentations of demoralization. SI is a self-perceived incapacity to perform tasks and express feelings deemed appropriate in a stressful situation, resulting in pervasive uncertainty and doubts about the future. The stressful situation disconfirms assumptions about self and others and about the continuity of the past and present with the future. Individuals with subjective incompetence are puzzled, indecisive, uncertain, facing a dilemma, unclear as to ways out of the situation, placed in a deadlock, impasse, quandary, or plight. SI is not the same as lack of self-efficacy. The two constructs may be inter-correlated, but SI refers strictly to the loss of the directional component of motivation, and not to loss of its magnitude, whereas lack of self-efficacy refers to both.
The importance of demoralization as a separate clinical entity and its deconstruction into distress and SI are supported by research (Tecuta et al. 2015; Robinson et al. 2016). As the intensity or duration of the stressful situation increases, a person experiencing SI eventually may become helpless and hopeless. This cascade may culminate in existential despair, meaninglessness, and suicide (de Figueiredo 2013 and the references cited therein).
Diagnostic criteria and operational definitions of demoralization have been proposed and tested. The Diagnostic Criteria for Psychosomatic Research (DCPR) for demoralization have been applied to medically ill patients and the Kissane and Clarke criteria have identified demoralization in patients with cancer and other chronic and debilitating illnesses. Several scales to assess demoralization as well as a scale for SI have been developed and shown to be reliable and valid. Research diagnostic criteria for demoralization aimed at more general use (i.e., for both psychiatric and non-psychiatric patients and the general population) have also been proposed (de Figueiredo 2013 and the references cited therein).
The Complexity of Chronic Pain
Tissue damage or dysfunction causes neural patterns or maps that produce pain (Damasio 1999, 2010). This process has several components: sensory, perceptual, affective, cognitive, and conative or volitional. Perception is the processing of the information delivered from sensory inputs and can be shaped by learning, memory, and expectation. Initially, this process occurs outside conscious awareness. The perception of pain can be dissociated from knowing that pain exists (cognitive component), suffering as a result of pain (affective component), and making a choice or decision to do something about the pain (volitional component). Neural patterns or maps are converted by the brain into mental images, a process that begins at the level of the brain stem and diencephalon and eventually reaches the cortex (Damasio 1999, 2010). The signs delivered from the periphery are interpreted as symbols representing images or ideas which, in turn, may be unconscious but may rise to consciousness. The connotative meaning of the information is probably critical at building the affective component of pain. The pain experience becomes a quale by a mechanism still poorly understood and hotly debated. As Ramachandran and Blakeslee assert, “pain is an opinion on the organism’s state of health, rather than a mere reflective response to an injury” (Ramachandran and Blakeslee 1999). Indeed, the interplay between “bottom-up” and “top-down” processes produces the brain’s summary “opinion” as to the state of bodily safety.
The gate control theory and its subsequent development, the neuromatrix theory, both proposed by Melzack, are attempts to integrate biological, psychological, and social variables to explain the individual differences in pain experience within the biopsychosocial framework (Melzack 1999, 2001). As Melzack noted, a “pain neuromatrix” has evolved in human beings that enables interplay between “bottom-up” processing of tissue pain sensations as danger signals and “top-down” regulation of the nociceptive information by the allocation of attention and by the encephalin and endorphin systems for analgesia. The pain neuromatrix has two separate divisions for perceiving different dimensions of pain. One gauges the intensity of suffering, while the other merely maps the location of the pain and registers its sensory characteristics. These divisions are established at the periphery, where “slow transmission” unmyelinated C fibers carry suffering information within peripheral nerves, while “fast transmission” lightly myelinated A-delta fibers carry sensory characteristics within the same peripheral nerve. From the periphery, these divisions are maintained all the way to the cerebral cortex. C fibers terminate in the amygdala, insula, and ventral anterior cingulate gyrus whose neural circuits regulate the perception of pain-related suffering while A-delta fibers end in the parietal sensory cortex whose neural circuits detect the location and the quality of pain.
Homeostasis is maintained by an assessment of the stressors, both external and internal, and activation of physiological and behavioral processes (stress responses) designed to meet the challenges interpreted as threatening survival. In chronic pain, the hypothalamic-pituitary-adrenal axis orchestrates the stress response in conjunction with the information exchanged with the dorsal horn of the spinal cord, the affect generating limbic system, and the immune system. In addition, prolonged (chronic) stress is associated with central sensitization of nociception. This central sensitization involves hypersensitivity to mechanical stimuli, a major increase in membrane excitability and synaptic efficiency in spinal neurons involved in nociception, and a corresponding reduction in inhibitory neurons (Latremoliere and Woolf 2009; Woolf 2011). A key role is played in this process by Substance P and its preferred receptor, neurokinin 1 (NK1R) (Mantyh 2002).
What is detected and reported to the brain is a danger signal that could be accepted, ignored, or amplified by the brain. This modulation takes into consideration not just the danger signal from the periphery but also cognitions, including assumptions and expectations, emotions, and behaviors associated with chronic pain, in short, the entire meaningful ecosystem.
The pre-frontal cortex and the dorsal cingulate gyrus have been associated with the executive function and what has been appropriately called “memory of the future” (Ingvar 1985). In this type of memory, behavioral algorithms are stored as templates for linking sensory and perceptual information to anticipated events on the basis of past experiences and the present situation. Perhaps in situations perceived as very stressful, a cortico-limbic imbalance or dysregulation involving the pre-frontal cortex and the dorsal cingulate gyrus creates the loss of a cognitive map clinically detected as SI, the hallmark of demoralization.
Demoralization in Chronic Pain
Not every patient with chronic pain is demoralized. A recent study of 242 patients with medically unexplained somatic symptoms, mostly headache, pain in the extremities, and weakness of the body, only two patients had demoralization as measured by DCPR (Desai and Chaturvedi 2016). Given the complexity of chronic pain, an integrative and comprehensive diagnostic formulation derived from the four perspectives mentioned above (diseases, behaviors, dimensions, and life stories) and an understanding that pain is contextualized are likely to capture the relevant information and point to a meaningful treatment plan.
-
a.
The “disease perspective”: From the “disease perspective”, it is important to determine if the pain reported by the patient meets the criteria for “chronic pain” in terms of its duration, its course, and its relationship to the underlying pathology if present. Also, is a comorbid mental disorder or physical illness complicating the pain or being exacerbated by the pain?
-
b.
The “behavior perspective”: Here the activity of the whole organism in its situational and historical context is the focus of attention. Should the clinical presentation be attributed to “illness behavior”? This type of behavior is a function of multiple illness, patient, and treatment system-related variables and their complex interactions (Mechanic 1995). Is the pain complicated by unhealthy behaviors such as substance dependence?
-
c.
The “dimensional perspective”: Sub-groups of chronic pain patients (dysfunctional, interpersonally distressed, and adaptive copers) report differing levels of pain and have different personality profiles. The dysfunctional sub-group reports the highest level of pain, with lower openness to new experience, followed by the interpersonally distressed, who perceive their significant others as unsupportive and even punitive, being more likely to be introverted and scoring higher in neuroticism. The lowest level of pain is reported by the adaptive copers, who are likely to be extroverted and open to new experience (Turk and Rudy 1988, 1990; Nitch and Boone 2004).
-
d.
The “perspective of life story”: Finally, should the clinical presentation be attributed to a disruption of the patient’s life story? Such disruption makes demoralization more likely to occur and the expression of both chronic pain and demoralization may be contextualized by the culture.
Each interpretation may be revealing to a greater or lesser extent and perspectives may be combined to obtain a clearer picture. Biological, psychological, social and cultural variables play varying roles depending on the observer’s perspective and the context of the observation. For example, it has been proposed that abnormalities in the development of the shared physical and social pain neural system during the developmental years may lead to increased sensitivity to physical and social pain in adulthood (Landa et al. 2012). A re-analysis of the data in the original article reporting the shared neural system indicated, however, that the neural representations for physical pain and social rejection may not be the same after all, implying that the “sharing”, in this instance, refers to cooperation among networks that need not be anatomically or even functionally identical (Woo et al. 2014).
Despite a wealth of evidence that demoralization is a reliable and valid clinical construct, relatively few studies have examined the interrelations of demoralization and pain. In chronic pain, repeated activation of neural, endocrine, and immune responses designed to react to acute stress creates an allostatic load and accelerates the disease process. This phenomenon was recognized by Gruenberg in patients with prolonged and persistent psychotic disorders who remained in mental hospitals for many years, and he called it “social breakdown syndrome” (Gruenberg 1974). This syndrome has since been recognized in other institutions, such as prisons, and it has been noted in the community at large with the elderly population stigmatized by social isolation and role loss (Radebaugh et al. 1987). It was a diagnosis in DSM-II but it was eliminated from DSM-III and subsequent editions of the DSM due to what appears to be an excessive adherence to the so-called “biomedical model” and a bias against the biopsychosocial framework.
In patients with chronic pain, the “pain trap” represents a maladaptive coping response that appears to account for progressively increasing disability from the pain condition (Levine and Phillips 2012). The pain trap is a cycle in which pain sensations activate amygdala and insula aversion responses that then entrain the patient’s attentional focus, which further activates aversion responses. This readying of mind and body for anticipated suffering is termed “bracing”. If the pain sensations are perceived as a threat to survival, a bracing response is evoked that mobilizes motor, autonomic and endocrine systems in a readiness to respond. The pain trap thus becomes a vicious cycle, with pain leading to a behavioral sequence of bracing, constricting, worsening of pain, helplessness, and freeze response. This vicious cycle has the potential for progression from helplessness to hopelessness and suicide. Patients with traumatic past life experiences are particularly at high risk for progressive worsening of pain-related suffering and demoralization from the pain trap.
Demoralization as measured by PERI-D was found to be associated with phantom tooth pain and myofascial face pain, and, in the latter case, both the intensity of pain and demoralization were significantly greater in the peak dark months than in the peak light months (Gallagher et al. 1995). This finding is important because it shows that demoralization and pain can be intimately associated with each other, perhaps reinforcing each other and propelled by the same etiological factors. Demoralization assessed by DCPR was found to be associated with greater pain intensity (Porcelli et al. 2009). In patients with myofascial pain syndromes, pain events (as distinguished from other negative events) were associated with greater negative change which, in turn, was associated with higher demoralization as measured by PERI-D (Lennon et al. 1990). In a study of patients with chronic temporomandibular pain and dysfunction syndrome (TMPDS), an independent and significant association was found between PERI-D demoralization and lower immune function (decreased lymphocytic proliferative activity), as measured by concanavallin A (Con A) and pokeweed mitogen (PWM)(Marbach et al. 1990).
Other well-designed studies have examined patients with both chronic pain and depression but demoralization was not assessed (Dohrenwend et al. 1999; Merikangas et al. 1990). Similar designs, combined with clinimetric methods to assess the allostatic load and with biological measures of the stress and immune responses, could be used for the study of demoralization in chronic pain patients and the efficacy of psychotherapy at promoting recovery and health. Induction of positive mood after stress reduced pain in depressed patients with chronic pain associated with fibromyalgia and/or osteoarthritis, thus suggesting that in some cases at least, depression does not alter pain or mood stress reactivity but delays the recovery from pain (Davis et al. 2014). Again, since screening scales for depression also include items on SI, it is possible that the subjects in these studies were demoralized, not just depressed.
The Role of Psychotherapy
Psychotherapy attempts to reduce demoralization and suffering from chronic pain despite ongoing nociceptive stimuli. Psychotherapy was defined by Frank as the relief of demoralization in one or more persons by a trained professional using an approach based on a particular theory or paradigm. After comparing various modalities of psychotherapy, Frank concluded that the specific theoretical orientation of the therapist is irrelevant for the success of psychotherapy. The active ingredients of successful psychotherapy, according to Frank, are the personal qualities of the therapist, the trust of the patient on the therapist, the expectations of the patient, and the nature of the therapist-patient relationship in a healing setting (Frank and Frank 1991). It should be noted however, that while all psychotherapies may be equally efficacious at relieving distress, their efficacy may differ at combating SI (i.e., increasing resilience), reducing the allostatic load, and promoting emotional regulation and functional improvement.
Psychotherapy for chronic pain can be best understood in terms of multiple pathways through which language, cognitive style, behavior, relationships, attitude towards pain, and awareness of the body modify the relative influences of top-down and bottom-up processing of information within the pain neuromatrix (McRae et al 2012). Regardless of the type of psychotherapy - whether psychodynamic, behavioral, cognitive-behavioral, interpersonal, family, mindfulness, or embodiment - what matters most is how specific pathways are activated and influence information processing in the pain neuromatrix and its summary “opinion” as to the state of bodily safety. Psychotherapy may help reduce the suffering and demoralizing component of pain (pain affect) by modulating the regulation of the amygdala, insula, and ventral anterior cingulate gyrus by the prefrontal cortex and the dorsal cingulate gyrus (Melzack 1999, 2001; Griffith 2010, pp. 38–47). This re-regulation would be “top-down” for the verbal interventions (psychodynamic psychotherapy, cognitive-behavioral psychotherapy, and interpersonal psychotherapy) and the mind-body therapies and “bottom-up” for physical therapy, and medications that reduce tissue inflammation.
Demoralization has a nocebo effect upon chronic pain that exacerbates the severity of suffering (Tacey 2010). It is both an effect and a cause of chronic pain. Chronic pain commonly engenders a sense of isolation, subjective incompetence, helplessness, and hopelessness. Such demoralization in turn has an adverse effect upon top-down regulation by the prefrontal cortex. This regulation is mediated by perspective-taking circuits, placebo circuits, and attention allocation, all of which are components of the brain’s internal system for analgesia (Ochsner and Gross 2005; Tacey 2010): Suppression and much perspective taking is conscious and volitional. Perspective-taking circuits normally dampen pain suffering by suppressing arousal of amygdala, insula, and ventral anterior cingulate cortex (vACC); demoralization releases these processing centers from inhibition (Ochsner and Gross 2005). The placebo response normally attenuates pain suffering by the prefrontal cortex activating the encephalin endogenous opiate system in the midbrain, whose descending fibers inhibit pain transmission within the spinal cord (Beneditti et al. 2005; Finniss et al. 2010; Tacey 2010). Expectations for relief of pain activate the placebo response. Demoralization brings expectations for distress and SI, which convert the placebo response into a nocebo response.
Within the brain, attention allocation can disrupt emotional processes, and suffering from pain can be moderated by shifting focus of attention, which limits the activation of amygdala, insula, and vACC by nociceptive stimuli (Rainville et al. 2002; Raz 2005). Demoralization, however, re-focuses attention so that the activation of these systems is heightened instead. Attention allocation to moderate fear or suffering from pain sensations has both implicit (unconscious) and explicit (conscious) elements. Emotion regulation protects the functional integrity of the prefrontal cortex and its capacities for perspective-taking, placebo response, and attention allocation. The distress and SI of demoralization most likely activate amygdala arousal. Emotion regulation is bolstered by reducing the cognitive load upon the prefrontal cortex and, in particular, amygdala arousal (Arsten 2009).
Management of suffering by the analgesia systems mentioned above occurs primarily at a “bracing” phase of coping with pain in which expectations for manageability of distress are brought to bear upon the sensory processing of nociceptive stimuli (Levine and Phillips 2012). Stages of nociception begin with perception of pain sensations. If these pain sensations are perceived as a threat to survival, a bracing response is evoked that mobilizes motor, autonomic, endocrine systems in a readiness to respond. This bracing response constricts focus of attention solely upon the threat, shuts down placebo circuits, and utilizes prefrontal perspective-taking to release from inhibition the subcortical amygdala-insula-vACC systems. Bracing thus exaggerates the suffering component of pain. Bracing provides an opportunity for distant emotional memories of traumatic experiences to interpret incoming nociceptive signals as catastrophic, rather than bothersome. Patients caught up in this “pain trap” experience progressive worsening of pain-related suffering and they probably become demoralized.
Most psychotherapies target the disruption of the “pain trap” in which a patient becomes increasingly avoidant of anticipated suffering (“bracing”) rather than the actual physical sensations of pain. Psychological management of chronic pain emphasizes strategies to prevent the behavioral sequence of the pain trap from becoming a habitual coping response. Each of the major psychotherapies has methods for accomplishing this aim.
As stated above, a useful way to conceptualize how psychotherapy can relieve both demoralization and suffering of chronic pain is to examine how psychotherapy activates different components of the brain’s internal systems for analgesia, which, as a consequence, diminishes distress and SI and disrupts the “pain trap”.
The efficacy of psychotherapy is largely due to certain factors shared by all psychotherapeutic modalities. These include attunement to a patient’s tolerance for emotional arousal, cognitive style, and discernment of strengths and competencies; building a robust therapeutic alliance; and mobilizing hope and an expectancy that change is possible. These common factors activate each of the above four components of the brain’s internal analgesia systems. A clinician’s skills for mobilizing these common factors of change are more important for the success of psychotherapy than the specific type of intervention being used or the theoretical orientation of the therapist (Duncan et al 2010). The complexity of the pain neuromatrix is such that there are multiple points of entry where an intervention can reduce overall suffering from pain by either attenuating the bottom-up transmission of nociceptive information or by amplifying the efficacy of the top-down regulation of the information.
Several psychotherapeutic interventions and strategies have been developed for patients with chronic pain. Demoralization was not assessed in the studies reporting these interventions but a case could be made that they reduce distress or SI or both. While differing in the techniques employed, they share several goals: to reduce the allostatic load; reduce distress; enhance resilience, the polar opposite of SI; improve emotional regulation; and promote functional improvement. These include psychodynamic, behavioral, cognitive-behavioral, interpersonal and family psychotherapies, and a number of mind-body interventions, such as mindfulness and embodiment.
Psychodynamic psychotherapy attempts to optimize the common factors of psychotherapy by prioritizing listening, understanding, and validating experience. As a result, both distress and SI are reduced (Duncan et al 2010). Developing a secure attachment relationship within the psychotherapist can confer a sense of safety, a powerful force in emotion regulation (Eisenberger 2013). Clarifications and interpretations foster salutatory perspective-taking and placebo responses.
Examples of behavioral approaches are relaxation training, diaphragmatic breathing, progressive muscle relaxation, autogenic training, visualization and guided imagery, operant behavior therapy, graded activation, time-contingent medication schedules, and fear avoidance. These approaches are aimed at improving emotional regulation.
Having the patient as an active participant in the treatment plan, cognitive-behavioral psychotherapy fosters salutatory perspective-taking and placebo responses, as well as improved emotion regulation. Psycho-education on pain physiology, realistic treatment expectations, and recommendations for avoiding the pain trap reduce distress and SI and activate common factors of change, promoting cognitive re-structuring and improvement in problem solving skills. Cognitive re-appraisal is focused upon meaning, purpose, and identity, rather than ruminations about suffering. SI is reduced because a cognitive map is being built. Behavioral approaches such as the ones mentioned above are also employed. Behavioral activation emphasizing absorption in pleasurable and gratifying experiences reduces distress and improves emotion regulation.
Interpersonal and family psychotherapy is focused on improvement of social skills. This type of therapy mobilizes common factors of change, resolves relational conflicts that generate distress, and facilitates relational coping that lessens both distress and subjective incompetence (Sprenkle et al. 2009; Eisenberger 2013).
Mindfulness has been defined as “the awareness that arises through intentionally attending in an open, accepting, and discerning way to whatever is arising in the current moment” and involves self-regulation of attention and orientation to experience (Shapiro and Carlson 2009 p. 556; Bishop et al. 2004). While cognitive behavioral psychotherapy concentrates on restructuring of negative thoughts, and interpersonal psychotherapy targets improvement in social skills, mindfulness-based psychotherapy enhances acceptance, positive affect, pain coping, cognitive flexibility, and resilience. Mindfulness-based interventions include mindfulness-based stress reduction, mindfulness-based cognitive therapy, acceptance and commitment therapy, and variants or combinations of these.
Embodied psychotherapy is based on the belief that recognition and mastery of pain require an increase in the awareness of the body. Embodied psychotherapies include yoga, relaxation, and meditation; imagery, hypnosis, and biofeedback; and a number of embodied experiential psychotherapies, such as art psychotherapy, analytical music therapy, dance-movement psychotherapy, and breath-activated interoception (Astin 2004). These psychotherapies practice self-regulation of attention and orientation to experience (Shapiro and Carlson 2009 p. 556; Bishop et al. 2004); enhance acceptance and cognitive flexibility, which improve emotion regulation and foster salutatory perspective-taking and activation of placebo responses; and practice experiencing pain sensations with non-fear responses, such as curiosity or interest in patterns of sensations, which improves emotion regulation.
Combinations of these various approaches have also been used (Roditi and Robinson 2011). For example, a combination of interpersonal psychotherapy and brief psychodynamic interpersonal psychotherapy tailored to co-morbid pain and depression has been described and shown to be effective (Poleshuck et al. 2010; Sattel et al. 2012). A promising intervention is the classification-based cognitive functional psychotherapy (CB-CFP). In this therapy, patients are rigorously classified by the sub-types of their chronic pain and the therapy uses multimodal interventions by targeting perceptions, beliefs, fears, and associated behaviors (Fersum et al. 2013). Demoralization may be countered even at bedside (Griffith and Gaby 2005).
Excellent reviews and meta-analyses have been published on the efficacy of these interventions in chronic pain patients (See, for example, van Tulder et al. 2000; Astin et al. 2003; Eccleston et al. 2009; McCracken and Thompson 2011; Dunford and Thompson 2010; Chiesa and Serreti, 2011; Veehof et al., 2011; Carlson 2012; Crow et al. 2015). In general, studies aimed at examining the efficacy of these therapies have led to mixed results or small effects, with the level of evidence being rated as weak, largely due to methodological problems such as small sample sizes, lack of randomization, or lack of usual care or no-intervention groups, thus making the interpretation of the results difficult. This lack of strong scientific support applies to multimodal, integrative therapies for the self-management of chronic pain symptoms as well (Lee et al. 2014).
An important element of effective psychotherapy with chronic pain patients is the clinician’s management of his or her own emotional reactivity to a patient’s pain (Otti et al. 2010). Empathic pain motivates emotional distancing from a visibly hurting patient. A clinician’s mirror neuron system enables the clinician’s pain neuromatrix to be activated by the patient’s facial expressions, vocalizations, and posture indicative of pain. This system operates automatically, largely outside conscious awareness (Jensen et al. 2014). Managing empathic pain is essential for clinicians treating chronic pain patients. Strategies that aid management of empathic pain include: collaborating with the patient as a partner by promoting the patient’s self-management of pain; sustaining respect for the patient by avoiding judgment about the patient’s struggles with pain; managing empathic fatigue by pacing intensity of care for chronic pain patients; attending to emotional self-care through recreation and supportive relationships; and seeking consultation from colleagues for challenging patients.
Last, but not the least, is the need to study and ameliorate the meaningful ecosystem in which the patient with chronic pain is embedded. This includes the patient’s beliefs about his or her relationships with family members, friends, other significant others, and society at large. Demoralization has not been sufficiently studied in non-Western or non-Westernized cultures and it is unclear how chronic pain and demoralization are expressed in various cultures. The cross-cultural efficacy of psychotherapy for chronic pain remains poorly understood.
Clinical Implications and Future Directions
In the United States, progress in the study of demoralization in patients with chronic pain has been slow. Funding for research having been largely dictated by the diagnostic categories specified in the DSM, an important obstacle has been the absence of demoralization in successive editions of the DSM. Other obstacles have been the misconceptions that demoralization is “normal” or that it does not occur by itself, independently of a mental disorder or a physical illness.
Despite these obstacles, progress in the study of pain and demoralization is gaining steam. As stated above, criteria and operational definitions for demoralization are now available. It is important to find out if demoralized individuals are more likely to experience chronic pain. Is demoralization a risk factor for chronic pain, more likely to occur in patients with chronic pain, a consequence of the chronic pain experience, and likely to lead to poor adherence to treatment, or demand for “pain killers”? To what extent does demoralization contribute to the amplification of the chronic pain experience? How is demoralization of chronic pain patients expressed, and how should it be treated, in non-Western cultures?
Data currently available suggests that no single treatment for demoralized patients with chronic pain will be efficacious by itself. Rather, a combination of treatment modalities may be successful. It is unclear which treatment modalities are most efficacious to which patients with the least side-effects and adverse events. A study of efficacy of psychotherapy for demoralized patients with chronic pain should classify patients rigorously, be assessor blinded, have an adequate sample size; adequate design, with randomization and inclusion of usual care and no intervention control groups; and prolonged longitudinal follow-up equivalent for all groups. Such study should determine the extent to which a given therapy or combination of therapies comes close to, or surpasses, the efficacy goals envisioned for the “perfect” chronic pain drug: “provide early and prolonged pain relief; have peripheral and central effects; have neuroprotective effects; protect against neurodegenerative effects; enhance endogenous analgesic systems through receptor mediated or other mechanisms; and modulate cytokine/immune responses” (Borsook et al. 2007). In addition, the study should determine to what extent each therapy or combination of therapies can reduce distress, reduce subjective incompetence (i.e., enhance resilience), reduce the allostatic load, reduce disability, promote emotional regulation, and improve function and quality of life. The assessments used in these studies should have acceptable reliability and empirical validity, not just face or construct validity, both of which may be deceiving. Empirical validity can be established in psychiatry not only with laboratory investigations but also with cross-cultural comparisons. Ideally, standardized imaging protocols should be used across studies integrated with molecular imaging and brain biomarkers of outcomes (Borsook et al. 2011a, b). Until then, such therapies should be viewed as helpful in many cases, definitely worth trying, and adjuvant to the overall care of the patient.
Conclusion
The distress experienced by patients in chronic pain may be understandable but the occurrence of SI may be viewed as a red flag for a cascade of events that, in the absence of an appropriate intervention, may result in suicidal attempts, demands for euthanasia, or death by suicide. All forms of psychotherapy attempt to help the patient re-script his or her life story by relieving distress, countering SI (i.e., promoting resilience), and restoring function. For the chronically demoralized patient in chronic pain, the reduction of the allostatic load promoted by psychotherapy brings the patient closer to a restoration of health.
While distress may be normal, the co-occurrence of SI (i.e., the appearance of demoralization) requires that some counteraction be taken by the patient, with or without professional help. The deconstruction of demoralization into distress and SI in the face of adversity allows us to bypass the “normal” vs “abnormal” dichotomy. Psychotherapists might explain to the demoralized patient that while distress is normal and understandable, the sense of incompetence, the perceived inability to overcome the stressful situation, and the feelings of helplessness and hopelessness could be countered and mastered, and then provide the patient with methods and tools to achieve that mastery.
References
Arsten, A. F. T. (2009). Stress signaling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience, 10, 410–422.
Astin, J. A. (2004). Mind-body therapies for the management of pain. Clinical Journal of Pain, 20(1), 27–32.
Astin, J. A., Shapiro, S. L., Eisenberg, D. M., & Forys, K. L. (2003). Mind-body medicine: State of the science, implications for practice. Journal of the American Board of Family Practice, 16, 131–147.
Beneditti, F., Mayberg, H. S., Wager, T. D., Stohler, C. S., & Zubieta, J.-K. (2005). Neurobiological mechanisms of the placebo effect. Journal of Neuroscience, 25, 10390–10402.
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., et al. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241.
Borsook, D., Becerra, L., & Hargreaves, R. (2011a). Biomarkers for chronic pain and analgesia, part 1: The need, reality, challenges, and solutions. Discovery Medicine, 11(58), 197–207.
Borsook, D., Becerra, L., & Hargreaves, R. (2011b). Biomarkers for chronic pain and analgesia, part 2: How, where, and what to look for using functional imaging. Discovery Medicine, 11(58), 209–219.
Borsook, D., Moulton, E. A., Schmidt, K. F., & Becerra, L. R. (2007). Neuroimaging revolutionizes therapeutic approaches to chronic pain. Molecular Pain, 3, 3–25.
Carlson, L. (2012). Review Article: Mindfulness-Based Interventions for Physical Conditions: A Narrative Review Evaluating Levels of Evidence. International Scholarly Research Notices (ISRN), 2012.
Chiesa, A., & Serreti, A. (2011). Mindfulness-based interventions for chronic pain: a systematic review of the evidence. Journal of Alternative and Complementary Medicine, 17(1), 83–93.
Clarke, D. M., Kissane, D. W., Trauer, T., & Smith, G. C. (2005). Demoralization, anhedonia and grief in patients with severe physical illness. World Psychiatry, 4(2), 95–105.
Clauw, D. J. (2014). Fibromyalgia: A clinical review. Journal of the American Medical Association, 311(15), 1547–1555.
Crow, E. M., Jeannot, E., & Trewhela, A. (2015). Effectiveness of Iyengar yoga in treating spinal (back and neck) pain: A systematic review. International Journal of Yoga, 8(1), 3–14.
Damasio, A. (1999). The feeling of what happens. Body and emotion in the making of consciousness. New York: Harcourt Brace & Company.
Damasio, A. (2010). Self comes to mind. Constructing the conscious brain. New York: Pantheon Books.
Davis, M. C., Thummala, K., & Zautra, A. J. (2014). Stress-related clinical pain and mood in women with chronic pain: moderating effects of depression and positive mood induction. Annals of Behavioral Medicine, 48(1), 61–70.
de Figueiredo, J. M. (1993). Depression and demoralization: Phenomenologic differences and research perspectives. Comprehensive Psychiatry, 34(5), 308–311.
de Figueiredo, J. M. (2011). Deconstructing demoralization: Distress and subjective incompetence in the face of adversity. In R. D. Alarcon & J. B. Frank (Eds.), The psychotherapy of hope: The legacy of persuasion and healing (pp. 107–124). Baltimore, MD: The Johns Hopkins University Press.
de Figueiredo, J. M. (2013). Distress, demoralization, and psychopathology. Diagnostic boundaries. The European Journal of Psychiatry, 27(1), 61–73.
Desai, G., & Chaturvedi, S. K. (2016). Do Diagnostic Criteria for Psychosomatic Research explain diagnosis of medically unexplained somatic symptoms? Psychotherapy and Psychosomatics, 85, 121–122.
Dohrenwend, B. P., Raphael, K. G., Marbach, J. J., & Gallagher, R. M. (1999). Why is depression comorbid with chronic myofascial face pain? A family study test of alternative hypotheses. Pain, 83, 183–192.
Duncan, B. L., Miller, S. D., Wampold, B. E., & Hubble, M. A. (2010). The heart and soul of change: Delivering what works in therapy. Washington, DC: American Psychological Association.
Dunford, E., & Thompson, M. (2010). Relaxation and mindfulness in pain: a review. Reviews in Pain British Journal of Pain, 4(1), 18–22.
Eccleston, C., Williams, A.C. & Morley, S. (2009) Psychological therapies for the management of chronic pain (excluding headache) in chronic pain. Cochrane Database of Systematic Reviews 2009 (2) Article No. CD0047072.
Eisenberger, N. I. (2013). An empirical review of the neural underpinnings of receiving and giving social support: implications for health. Psychosomatic Medicine, 75, 545–556.
Fersum, K. V., O’Sullivan, P., Skouen, J. S., Smith, A., & Kvale, A. (2013). Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: A randomized controlled trial. European Journal of Pain, 17(6), 916–928.
Finniss, D. G., Kaptchuk, T. J., & Benedetti, F. (2010). Biological, clinical, and ethical advances of placebo effects. Lancet, 375, 686–695.
Frank, J. D., & Frank, J. B. (1991). Persuasion and healing. A comparative study of psychotherapy. Baltimore: The Johns Hopkins University Press.
Gallagher, R. M., Marbach, J. J., Raphael, K. G., Handte, J., & Dohrenwend, B. P. (1995). Myofascial face pain: seasonal variability in pain intensity and demoralization. Pain, 61, 113–120.
Grassi, L., Mangelli, L., Fava, G. A., Grandi, S., Ottolini, F., Porcelli, P., et al. (2007). Psychosomatic characterization of adjustment disorders in the medical setting: some suggestions for DSM-V. Journal of Affective Disorders, 101, 251–254.
Griffith, J. L. (2010). Religion that heals, religion that harms. New York: Guilford Press.
Griffith, J. L., & Gaby, L. (2005). Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics, 46(2), 109–116.
Gruenberg, E. M. (1974). The social breakdown syndrome and its prevention. In G. Caplan (Ed.), American handbook of psychiatry (pp. 697–711). New York, NY: Basic Books.
Guidi, J., Fava, G. A., Picardi, A., Porcelli, P., Bellomo, A., Grandi, S., et al. (2011). Subtyping depression in the medically ill by cluster analysis. Journal of Affective Disorders, 132, 383–388.
Hardt, J., Jacobsen, C., Goldberg, J., Nickel, R., & Buchwald, D. (2008). Prevalence of chronic pain in a representative sample in the United States. Pain Medicine, 9(7), 803–812.
Ingvar, D. H. (1985). “Memory of the future”: an essay on the temporal organization of conscious awareness. Human Neurobiology, 4(3), 127–133.
Jensen, K. B., Petrovic, P., Kerr, C. E., Kirsch, I., Raicek, J., Cheetham, A., et al. (2014). Sharing pain and relief neural correlates of physicians during treatment of patients. Molecular Psychiatry, 19(3), 392–398.
Klein, D. F., Gittelman, R., Quitkin, F., & Rifkin, A. (1980). Diagnosis and drug treatment of psychiatric disorders: adults and children. Baltimore: Williams & Wilkins.
Landa, A., Peterson, B. S., & Fallon, B. A. (2012). Somatoform pain: A developmental theory and translational research review. Psychosomatic Medicine, 74(7), 717–727.
Latremoliere, A., & Woolf, C. J. (2009). Central sensitization: A generator of pain hypersensitivity by central neural plasticity. Journal of Pain, 10, 895–926.
Lee, C., Crawford, C., Swann, S., & Active Self-Care Therapies for Pain (PACT) Working Group (2014) Multimodal, integrative therapoies for the self-management of chronic pain symptoms. Pain Medicine 15: S76–S85.
Lennon, M. C., Dohrenwend, B. P., Zautra, A. J., & Marbach, J. J. (1990). Coping and adaptation to facial pain in contrast to other stressful life events. Journal of Personality and Social Psychology, 59, 1040–1050.
Levine, P., & Phillips, M. (2012). Freedom from Pain. Boulder, CO: Sounds True.
Machikanti, L., Singh, V., Datta, S., Cohen, S. P., & Hirsch, J. A. (2009). American Society of Interventional Pain Physicians. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician, 12(4), E35–E70.
Mangelli, L., Fava, G. A., Grandi, S., Grassi, L., Ottolini, F., Porcelli, P., et al. (2005). Assessing demoralization and depression in the setting of medical disease. Journal of Clinical Psychiatry, 66(3), 391–394.
Mantyh, P. W. (2002). Neurobiology of substance P and the NK1 receptor. Journal of Clinical Psychiatry, 63(Suppl. 11), 6–10.
Marbach, J. J., Schleifer, S. J., & Keller, S. E. (1990). Facial pain, distress, and immune function. Brain, Behavior, and Immunity, 4, 243–254.
McCracken, L. M., & Thompson, M. (2011). Psychological advances in chronic pain: a concise selective review of research from 2010. Current Opinion in Supportive and Palloiative Care, 5(2), 122–126.
McHugh, P. R., & Slavney, P. R. (1998). The perspectives of psychiatry. Baltimore, MD: Johns Hopkins University Press.
McRae, K., Misra, S., Prasad, A. K., Pereira, S. C., & Gross, J. J. (2012). Bottom-up and top-down emotion generation: implications for emotion regulation. SCAN, 7, 253–262.
Mechanic, D. (1995). Sociological dimensions of illness behavior. Social Science & Medicine, 41(9), 1207–1216.
Melzack, R. (1999). From the gate to the neuromatrix. Pain Supplement, 6, 121–126.
Melzack, R. (2001). Pain and the neuromatrix in the brain. Journal of Dental Education, 65(12), 1378–1382.
Merikangas, K. R., Angst, J., & Isler, H. (1990). Migraine and psychopathology. Archives of General Psychiatry, 47, 849–853.
National Comprehensive Cancer Network. (2003). Distress management clinical practice guidelines in oncology. Journal of the National Comprehensive Cancer Network, 1, 344–374.
Nitch, S. R., & Boone, K. B. (2004). Normal personality correlates of chronic pain subgroups. Journal of Clinical Psychology in Medical Settings, 11(3), 203–209.
Ochsner, K. N., & Gross, J. J. (2005). The cognitive control of emotion. Trends in Cognitive Sciences, 9, 242–249.
Otti, A., Guendel, H., Laer, L., Wohlschlaeger, A. M., Lane, R. D., Decety, J., et al. (2010). I know the pain you feel: How the human brain’s default mode predicts our resonance to another’s suffering. Neuroscience, 169(1), 143–148.
Poleshuck, E. L., Gamble, S. A., Corta, N., Hoffman-King, D., Cerrito, B., Rosario-McCabe, L. A., et al. (2010). Interpersonal psychotherapy for co-occurring depression and chronic pain. Professional Practice: Research and Practice, 41(4), 312–318.
Porcelli, P., Bellomo, A., Quartesan, R., Altamura, M., Iuso, S., Ciannameo, S., et al. (2009). Psychosocial functioning in consultation-liaison psychiatry patients: influence of psychosomatic syndromes, psychopathology, and somatization. Psychotherapy and Psychosomatics, 78(6), 352–358.
Radebaugh, T. S., Hooper, F. J., & Gruenberg, E. M. (1987). The Social Breakdown Syndrome in the elderly population living in the community: The Helping Study. British Journal of Psychiatry, 151, 341–346.
Rainville, P., Hofbauer, R. K., Bushnell, M. C., Duncan, G. H., & Price, D. D. (2002). Hypnosis modulates the activity in cerebral structures involved in the regulation of consciousness. Journal of Cognitive Neuroscience, 14(Supplement), 887–901.
Ramachandran, V. S., & Blakeslee, S. (1999). Phantoms in the Brain. New York: William Morrow.
Raz, A. (2005). Attention and hypnosis neural substrates and genetic associations of two converging processes. International Journal of Clinical and Experimental Hypnosis, 52, 237–258.
Robinson, S., Kissane, D. W., Brooker, J., & Burney, S. (2016). A review of the construct of demoralization: history, definitions, and future directions for palliative care. American Journal of Hospice and Palliative Care, 33(1), 93–101.
Roditi, D., & Robinson, M. E. (2011). The role of psychological interventions in the management of patients with chronic pain. Psychology Research and Behavior Management, 4, 41–49.
Sattel, H., Lahmann, C., Gundel, H., Guthrie, E., Kruse, J., Noll-Hussong, M., et al. (2012). Brief psychodynamic interpersonal psychotherapy for patients with multi-somatoform disorder: randomized controlled trial. The British Journal of Psychiatry, 200(1), 60–67.
Semprini, F., Fava, G. A., & Sonino, N. (2010). The spectrum of adjustment of disorders: Too broad to be clinically helpful. CNS Spectrum, 15(6), 382–388.
Shapiro, S. L., & Carlson, S. E. (2009). The art and science of mindfulness: Integrating mindfulness into psychology and the helping professions. Washington, DC: American Psychological Association Publications.
Sprenkle, D. H., Davis, S. D., & Lebow, J. (2009). Common factors in couple and family therapy: The overlooked foundation for effective practice. New York: Guilford Press.
Tacey, I. (2010). Getting the pain you expect: mechanisms of placebo, nocebo and reappraisal effects in humans. Nature Medicine, 16, 1277–1283.
Tecuta, L., Tomba, E., Grandi, S., & Fava, G. A. (2015). Demoralization: a systematic review on its clinical characterization. Psychological Medicine, 45, 673–691.
Turk, D. C., & Monarch, E. S. (2002). Biopsychosocial perspective on chronic pain. In D. C. Turk & R. J. Gatchel (Eds.), Psychological approaches to pain management: A practitioner’s handbook (pp. 3–29). New York: Guilford.
Turk, D. C., & Rudy, T. E. (1988). Toward an empirically derived taxonomy of chronic pain patients: Integration of psychological assessment data. Journal of Consulting and Clinical Psychology, 56(2), 233–238.
Turk, D. C., & Rudy, T. E. (1990). The robustness of an empirically derived taxonomy of chronic pain patients. Pain, 44, 5–28.
Van Tulder, M. W., Ostelo, R., Vlaeyen, J. W., Linton, S. J., Morley, S. J., & Assendelft, W. J. (2000). Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane Back Review Group. Spine, 25, 2688–2699.
Veehof, M. M., Oskam, M. J., Schreurs, K. M., & Bohlmeijer, E. T. (2011). Acceptance-based interventions for the treatment of chronic pain: a systematic review and meta-analysis. Pain, 152(3), 533–542.
Woo, C.-W., Koban, L., Krose, E., Llindquist, M. A., Banich, M. T., Ruzic, L., et al. (2014). Separate neural representations for physical pain and social rejection. Nature Communications, 5, 5380.
Woolf, C. J. (2011). Central sensitization: Implications for the diagnosis and treatment of pain. Pain, 152((Suppl.)), S2–S15.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Figueiredo, J.M., Griffith, J.L. Chronic Pain, Chronic Demoralization, and the Role of Psychotherapy. J Contemp Psychother 46, 167–177 (2016). https://doi.org/10.1007/s10879-016-9331-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10879-016-9331-x