Abstract
The ability to monitor the physiological effect of the analgesic agent is of interest in clinical practice. Nonstationary changes would appear in photoplethysmography (PPG) during the analgesics-driven transition to analgesia. The present work studied the properties of nonlinear methods including approximate entropy (ApEn) and sample entropy (SampEn) derived from PPG responding to a nociceptive stimulus under various opioid concentrations. Forty patients with ASA I or II were randomized to receive one of the four possible remifentanil effect-compartment target concentrations (Ceremi) of 0, 1, 3, and 5 ng·ml−1 and a propofol effect-compartment target-controlled infusion to maintain the state entropy (SE) at 50 ± 10. Laryngeal mask airway (LMA) insertion was applied as a standard noxious stimulation. To optimize the performance of ApEn and SampEn, different coefficients were carefully evaluated. The monotonicity of ApEn and SampEn changing from low Ceremi to high Ceremi was assessed with prediction probabilities (PK). The result showed that low Ceremi (0 and 1 ng·ml−1) could be differentiated from high Ceremi (3 and 5 ng·ml−1) by ApEn and SampEn. Depending on the coefficient employed in algorithm: ApEn with k = 0.15 yielded the largest PK value (0.875) whereas SampEn gained its largest PK of 0.867 with k = 0.2. Thus, PPG-based ApEn and SampEn with appropriate k values have the potential to offer good quantification of analgesia depth under general anesthesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Analgesia, hypnosis and immobility are three important components of anesthesia [1, 2]. Clinically, the response resulting from neural processing of painful stimulus is defined as ‘nociception’, and the potential of analgesic agent to attenuate the response is defined as ‘anti-nociception’. An ideal analgesia depth means obtaining an adequate balance between nociception and anti-nociception. The accurate measurement of analgesia depth could reduce drug consumption and adverse impacts including postoperative hyperalgesia [3, 4]. Nevertheless, there is no standard indicator available for monitoring analgesia depth. Previous studies have suggested that the nociception-anti-nociception (NAN) balance is related to analgesics dose, the stimulus intensity, and sedation state [5], i.e. if there is an indicator dependent on analgesic concentration or stimulus intensity during muscle paralysis when sedation state is kept at a steady state, analgesia could be administrated by merely adjusting the dosage of analgesics.
The ability to monitor the physiological effect of the analgesic agent is of interest in clinical practice. Photoplethysmography (PPG) is mediated by sympathetic nervous system and its detection is readily accessible [6]. PPG has advantages of simplicity and rapidity in signal processing with simple morphology and without mixed signals. It has been proven that several parameters such as PPG amplitude (PPGA), pulse beat interval (PBI) and surgical pleth index (SPI) are correlated with the stimulus intensity or analgesia depth [7, 8], however, without desirable accuracy [9, 10].
In the field of anesthesia, nonlinear variables are mainly applied in evaluating unconsciousness and focused on EEG signal [5, 11]. Few studies have considered their relationship with analgesia depth or applied them to other physiological signals. Considering the disturbances caused by noxious stimulus are nonstationary, the nonlinear indices could quantify better the irregularity of dynamical signals [12]. Based on the prominent results in estimating levels of anesthetic-induced unconsciousness [13,14,15], approximate entropy (ApEn) and sample entropy (SampEn) are considered to have the potential in monitoring NAN balance under the constant hypnotic states.
The purpose of this paper was to examine the methodology of ApEn and SampEn calculations, focusing on the variations of recorded signal under various analgesics concentrations and the influence of different coefficients employed in ApEn and SampEn. The key question addressed was whether ApEn and SampEn had a monotonic response to analgesic depth. In this study, sedative properties were reflected using state entropy (SE) and anti-nociception was administrated using remifentanil [16].
2 Methods
2.1 Anesthesia and data collection
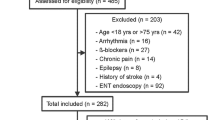
The study was approved by the Ethics Committee of Women’s Hospital School of Medicine Zhejiang University. Forty patients with American Society of Anesthesiologists (ASA) physical status I or II, scheduled for gynecologic laparoscopy surgery or breast surgery under general anesthesia were enrolled. We excluded patients with cardiovascular disease or autonomic nervous dysfunction, difficult airway (Mallampattis test III or IV), body mass index over 30 kg·m−2, and chronic use of alcohol or psychoactive medication. Patients were allocated randomly to receive one of four possible remifentanil effect-compartment target concentrations (Ceremi): 0 (n = 10, group R0), 1 (n = 10, group R1), 3 (n = 10, group R3), 5 (n = 10, group R5) ng·ml−1. In this study, the concentration of remifentanil at 0 and 1 ng·ml−1 represented underdosage of analgesics, whereas the concentration at 5 ng·ml−1 represented overdosage.
With no premedication administration, patients were anesthetized with propofol and remifentanil, and muscle relaxant was achieved with 0.15 mg·kg−1 cisatracurium. Propofol and remifentanil were administrated using target-controlled infusion (TCI) pump (Orchestra Primea, Fresenius, France) programmed with propofol pharmacokinetic dataset [17] and remifentanil pharmacokinetic dataset [18]. The target was adapted such that before laryngeal mask airway (LMA) insertion SE was maintained at 50 ± 10 and steady-state target Ceremi was obtained. LMA insertion was applied as a standard noxious stimulus.
Photoplethysmographic signal was monitored and collected using anesthesia monitoring (CARESCAPE B650, GE Healthcare, Finland) with sample rate at 100 Hz. Recordings were exported as comma-separated value formatted files in arbitrary unit. A 1-min window before and after LMA insertion (N = 12,000) was designated for off-line analysis.
2.2 ApEn
ApEn introduced by Pincus [19], is a measure quantifying the unpredictability of a finite length signal. For a time series X(i) = x(1), x(2),…, x(L) with L data points, ApEn could be calculated as follows.
-
(i)
Reconstitute the time series X(i) as m-dimensional sequence vectors Xm(1) to Xm(L − m + 1):
$$ X_{m} (i) = \{ x(i),x(i + 1), \ldots ,x(i + m - 1)\} ,\quad i = 1,2, \ldots ,L - m + 1. $$(1) -
(ii)
Compute the distance d between the vectors Xm(i) and Xm(j):
$$ d\left[ {X_{m} \left( i \right),X_{m} \left( j \right)} \right] = \max \left( {\left| {x\left( {i + l} \right) - x\left( {j + l} \right)} \right|} \right),\quad l = 0,1, \ldots ,m. $$(2) -
(iii)
Calculate the probability:
$$ C_{i}^{m} (r) = \frac{{B_{i} }}{L - m + 1}, $$(3)where Bi is the number of Xm(j) satisfying d[Xm(i), Xm(j)] ≤ r. The tolerance r is defined as:
$$ r = k\sigma , $$(4)where σ is the standard deviation of L data points, and k is a constant.
-
(iv)
We further define:
$$ \phi^{m} (r) = \frac{1}{L - m + 1}\sum\nolimits_{i = 1}^{L - m + 1} {\ln C_{i}^{m} (r)} . $$(5)Set m = m + 1, and repeat steps (i)–(iv):
$$ \phi^{{m{ + }1}} (r) = \frac{1}{L - m}\sum\nolimits_{i = 1}^{L - m} {\ln C_{i}^{{m{ + }1}} (r)} , $$(6)and calculate ApEn:
$$ {\text{ApEn}}(m,r,L) = \phi^{m} (r) - \phi^{m + 1} (r). $$(7)
Previous researches [15, 20,21,22] have shown that the selection of parameters L, m, and r has a great influence on outcomes. The parameter L should be 10m–20m to gain a valid statistics. Also, the choice of r value requires care as detailed system information would be lost if r is too large, whereas the extracted information would mainly be signal noise if r is too small. ApEn in this study was calculated using 10-s time windows (L = 1000) to track consistent changes in PPG recording with m = 2. The choice of L = 1000, rather than prolonged time period (L = 2000 or 3000) [23, 24], ensured less time delay when 1000 was sufficient to estimate ApEn and SampEn validly [22, 25]. The coefficient k was recommended to be 0.05 to 0.25. Given that its optimal value was different for various applications [15, 23], five different k values were tested: 0.05, 0.1, 0.15, 0.2, and 0.25.
2.3 SampEn
SampEn proposed by Richman and Moorman [25] is an improved algorithm from ApEn. SampEn differs from ApEn in two ways to reduce bias. Firstly, SampEn does not count self-matches. Bi is defined as the number of Xm(j) satisfying d[Xm(i), Xm(j)] ≤ r, i ≠ j. Secondly, the number of reconstituted vectors is L − m instead of L − m + 1 in embedding dimension m, so that the number of vector comparison would be equal for both embedding dimension m and m + 1. Accordingly, the probability is adjusted.
SampEn is calculated as follows:
where
The selection of parameters L, m, and r for SampEn was same to ApEn [26, 27].
2.4 Data processing and optimal timestamp selection
The off-line PPG signal with N data points (N = 12,000) was analyzed using Matlab software (version R2017b, Mathwork Inc., MA, USA). Generally, band-pass filter was applied to remove noise in PPG signal. Considering the good quality of the PPG signal acquired from monitoring, this step was simplified with moving average filter for its good performance in eliminating sharp noises. yn represented the raw off-line PPG while yyn represented the preprocessed PPG displayed in Fig. 1. The span of moving average filter was set as 5, as described in:
To observe the continuous response of variables to stimulus, ApEn and SampEn time series were constructed using PPG data. A 10-s time window (L = 1000) obtained one ApEn and SampEn value as their definitions. The window slid in L/10 steps with 900 data points overlapped [23]. Thus the length of ApEn and SampEn time series was (N − L)/(L/10) + 1 = 111, where the ‘1’ represented the last 10-s time window. Each measure contained four time series, describing the average variation under four levels of opioid dosage.
Based on the time series, two values were extracted for each variable to characterize the states before and after the stimulus. The baseline of all observation indices (bef) was defined as the ApEn and SampEn values calculated using the data of last 10 s before stimulus, and the values of ApEn and SampEn at optimal timestamp occurring after the stimulus were defined as aft. Rules were made for determining the optimal timestamp.
In consideration of the fact that Ceremi of 3 ng·ml−1 is adequate for the supposed impact of LMA insertion defined as a moderate noxious stimulus [7, 28], the time series of 5 ng·ml−1 Ceremi was not taken into account for the localization of the optimal timestamp. At one timestamp, the distance of variables’ time series between 0 and 1 ng·ml−1 was defined as d1 and the distance between 1 and 3 ng·ml−1 was defined as d2. The timestamp where satisfying max(d1 + d2) and \(\min\!\left( {d_{1}^{2} + d_{2}^{2} } \right)\) was considered as the optimal timestamp. Max(d1 + d2) was calculated for yielding the greatest possible distinction between 0 and 3 ng·ml−1, and then \(\min\!\left( {d_{1}^{2} + d_{2}^{2} } \right)\) rendered the difference of each comparison largest. If there was more than one eligible point, the median would be extracted.
2.5 Statistical analysis
Values were presented as mean ± standard deviation unless otherwise indicated. All tests were 2-tailed. The bef and aft values were both analyzed from four levels using Kruskal–Wallis H test (IBM SPSS Statistics 25.0, SPSS Inc., Chicago, IL, USA) for investigating the influence of Ceremi on indices during nonnoxious and noxious events. Wilcoxon signed-rank test (Graphpad Prism 7, Graphpad Software Inc., San Diege, CA, USA) was employed to test the response to LMA insertion by comparing bef and aft values. The detailed effect of remifentanil was examined using Mann–Whitney test by comparing any two aft values. A p value less than 0.05 (p < 0.05) was considered statistically significant.
Prediction probabilities (PK) were calculated as a criterion to assess the applicability of indicators in predicting analgesic depth by PKMACRO spreadsheets [29]. If the indicator composes a concordance, no matter in the same or opposite direction, with remifentanil concentration, the PK would be great. A PK value of 1.0 means a perfect prediction whereas a PK of 0.5 means no better prediction than a random guess. In case PK ∈ [0, 0.5], PK could be normalized by calculating 1-PK [15].
3 Results
Characteristic data of the 40 patients were illustrated in Table 1. The four groups showed no statistically significant differences in terms of age, weight, height, or the body mass index (BMI).
3.1 ApEn and SampEn time series
Shapes of the ApEn and SampEn time series with different k choices were presented in Fig. 2. The variation trends of ApEn and SampEn were generally similar when the k value was same. In the curves with positive slope, the sharp increase in low Ceremi groups (R0 and R1) and slight increase in high Ceremi groups (R3 and R5) were clearly suppressed in a dose-dependent manner. Switching the k value from 0.05 to 0.25, the curves had less overlaps among groups after stimulus.
The points conforming to max(d1 + d2) and min(d12 + d22) were summarized (Table 2). The location of optimal timestamp, ranging from 65 to 70, was comparatively farther away from the stimulus point with the increase of k value. The value of each measure at its optimal timestamp was selected as aft for later analysis.
3.2 The relationship between variables and Ceremi before and after LMA insertion
During the nonnoxious period, variables were not correlated with tested Ceremi. The bef values of measures were displayed in Table 3. The p values of Kruskal–Wallis H test for ApEn (0.567, 0.615, 0.748, 0.419, and 0.172 respectively) and SampEn (0.750, 0.131, 0.116, 0.121, and 0.082 respectively) with k = 0.05, 0.1, 0.15, 0.2, and 0.25 were apparently larger than 0.05.
Table 3 also displayed the reactions (aft values) of ApEn and SampEn after LMA insertion. The stimulus increased all variables dramatically during underdosage of analgesics (Ceremi = 0 and 1 ng·ml−1) except ApEn with k = 0.25. No significant increase was observed under the dosage of 3 and 5 ng·ml−1.
Examined variables at optimal timestamp of four groups were demonstrated in Fig. 3. The behaviors of ApEn and SampEn depended considerably on k values: Measures with all k values except k = 0.25 showed excellent capability in distinguishment between low Ceremi (0 and 1 ng·ml−1) and high Ceremi (3 and 5 ng·ml−1). The differences between 0 ng·ml−1 and high Ceremi were more and more significant with the increasing k value. However, the decreases of ApEn and SampEn responding to increasing Ceremi were not continuous when k = 0.05 and 0.1. ApEn with k = 0.15, 0.2, and 0.25 and SampEn with k = 0.2 and 0.25 could significantly differentiate group R0 from R1. The discrimination between R1 and R3 was not detected using indices with k = 0.25. No variables could reveal substantial differences between R3 and R5.
Figure 4 presented the predictive powers of variables in indicating analgesic depth. PK became larger first and then reduced with the increase of k value. The best value of k was determined based on the type of entropy parameter. For SampEn, k value of 0.2 provided the best monotonic response to Ceremi with PK = 0.867. ApEn with k = 0.15 yielded the largest PK value, 0.875.
4 Discussion
In this paper, the application of entropy methods to PPG signal was studied to assess the depth of analgesia during propofol–remifentanil anesthesia. We compared the effects of ApEn and SampEn with various coefficients to make a distinction among Ceremi, expecting the monotonicity of measures would be in accord with opioid concentrations.
4.1 Time series of entropies with no analgesics administration
The time series of entropies varied with the continuous transition from unconsciousness to pain, as illustrated in Fig. 2. The curves of variables were maintained at a specific state when num ≤ 51. After LMA insertion applied, entropies started to increase and then subsequently decreased to its original state after saturating to the maximum. It was obvious that entropy variables could be affected by nociceptive input and its diversification was consistent with that of the degree of nociception. Nevertheless, it was inevitable to observe that the values of entropies were relatively small less than 0.5. This could be ascribed to the choice of L (L = 1000) that the variation contained in PPG data within 10 s was limited. Despite that, the discrimination detected using entropies with L = 1000 was enough for studying the influence of drug concentrations.
4.2 Dependency of ApEn and SampEn on Ceremi
All measures remained roughly unaffected by remifentanil concentrations before LMA insertion. The results were in accordance with the previous studies [30, 31]. This demonstrated that parameters were reliable to provide relevant evaluation of patients’ response to stimulus as they were independent on Ceremi during nonnoxious events.
Remifentanil had dose-dependent influence on ApEn and SampEn after LMA insertion. The main observations from this study were that (1) stimulation-induced changes of entropies during ‘adequate’ analgesia (Ceremi = 3 and 5 ng·ml−1) markedly diminished in comparison with ‘inadequate’ analgesia (Ceremi = 1 and 0 ng·ml−1); and (2) ApEn and SampEn were significantly correlated to remifentanil concentration with appropriate k values. This follows that physiological signal tends to be more resistant to stimulus and more regular as the anesthesia deepens. However, the variables could not discern 3 from 5 ng·ml−1. This implied the incapacities of measures for evaluating over-dose opioid drugs.
Entropy measures were heavily relied on the choice of k values. When k = 0.05 and 0.1, the changes of ApEn and SampEn were not monotonous. We speculated that the variations caused by LMA insertion under Ceremi = 3 and 5 ng·ml−1 and the noise in the signal are both small, the extracted information decided by k = 0.05 mixed too much noise. ApEn and SampEn with 0.25 outperformed others in discerning 0 from 1 ng·ml−1 whereas other k values could perform better in differing 1 from 3 ng·ml−1. This might be attributed to the fact that the changes of PPG with no remifentanil or Ceremi of 1 ng·ml−1 were so intense that the distances defined for ApEn and SampEn with small k values were not long enough to observe the discrepancy. The PK values of indices with k ≥ 0.15 were all greater than 0.8. A choice of k = 0.15 for ApEn was superior to other measures with PK = 0.875. With the objective of obtaining large PK value, ApEn and SampEn were both good methods for indicating the analgesia depth.
On the other hand, compared with the good performances of EEG-derived ApEn and SampEn (PK values ranged from 0.86 to 0.89) in the previous studies of awareness monitoring, the efficiencies of PPG-derived ApEn and SampEn in qualification of analgesia depth during propofol–remifentanil anesthesia were similar. This indicated that both hypnotic and analgesic effects could be detected by ApEn and SampEn, though no one has ever studied how to distinguish the two effects contained in ApEn and SampEn so far.
4.3 Comparisons between entropies and other nociception-related physiologic variables
To examine the efficiencies of entropies, the contrast of variables and other nociception-related physiologic indices including PPGA and PBI was conducted. Given that each pulse could compute one PPGA and PBI value whereas the calculation of entropies requires a period of PPG data, we extracted the bef and aft values of PPGA and PBI using different method mentioned in the previous research [31].
PPGA and PBI were averaged the minute before (bef) and after (aft) LMA insertion, as presented in Fig. 5. PPGA could only distinguished the stimulus-induced differences at Ceremi of 0 and 1 ng·ml−1. PBI had a better capacity compared with PPGA. Diverse drug concentrations could be discriminated using PBI with PK value of 0.830. However, PBI was significantly affected by remifentanil concentrations during nonnoxious period. This would reduce the accuracy in the evaluation of patients’ responses during the presence of the stimulation.
PPGA and PBI before (white boxes) and after (gray boxes) stimulation at 0, 1, 3, and 5 ng·ml−1 remifentanil effect-compartment concentrations (R0, R1, R3, and R5 respectively). Data were median, interquartile range, and range. *p < 0.05 and **p < 0.01 vs. pre-stimulus value. #p < 0.05, ##p < 0.01, ###p < 0.001, and ####p < 0.0001 vs. lower remifentanil concentration
4.4 Related research
A few studies considering the nonlinear measures during propofol–remifentanil anesthesia have been published. In [23], EEG-derived ApEn, SampEn and permutation entropy were examined in three groups with various dosages of remifentanil. The results showed remifentanil had a consistent dose-dependent effect on ApEn and SampEn throughout the transition from awake to burst suppression state. No stimulation had been applied and analgesia depth was not assessed. In [32], spectral entropy was chosen to predict a motor response to noxious stimulation. In contrast to this paper, the hypnotic state was merely controlled by observing whether the patient lost consciousness, rather than an objective indicator such as SE. The predictive value of entropy was weak with PK < 0.8. Besides, researchers used to designate ‘movement’ as an end point and explored the relationship between measures and ‘movement’ [32,33,34]. The usefulness of these researches was limited in paralyzed patients on the one hand, on the other hand, muscle relaxants which were usually applied to make the operation easy would seriously affect the observation of movement. In general, nonlinear features have not been thoroughly studied in the field of analgesia and standard research procedure is needed to establish.
In our previous research, some outstanding linear measures including diastolic interval (DI) were extracted in the time domain. In future work, linear and nonlinear features would be combined, and more kinds of physiological signals would be added to monitor the underlying changes caused by the autonomic system during anesthesia.
4.5 Limitations
First, larger subjects would be needed to strengthen the present findings. The hoc-post power calculation was performed for Wilcoxon signed-rank test and Mann–Whitney test using G*power software. As to Wilcoxon signed-rank test, the associations between bef and after values of entropies with various k values were firstly assessed using Spearman’s rank correlation coefficient test. According to α = 0.05, sample size = 10 and the effect size reckoned using means, standard deviations and correlations, it was found that only the paired groups with statistical significance achieved the power of 0.8. This indicated that the differences before and after stimulus at Ceremi of 3 and 5 ng·ml−1 might be detected as the amount of data increased. As to Mann–Whitney test, the power values were all less than 0.8 when two groups with closer concentrations were compared. Hence larger sample size was needed to further verify the relationships of these groups.
Secondly, the study protocol could be further optimized. During the data collection in this study, sedation state (SE value) and stimulation type (LMA insertion) of all patients were held relatively constant, and different patients received different remifentanil doses. Based on this study protocol, the purpose of revealing the correlation between remifentanil doses and variables’ response to noxious stimulus could be achieved. Similar research has been conducted before [29]. In actual clinical practices, however, the nociception resulted from LMA insertion was not exactly the same. Though we had designated the same anesthesiologist to complete the LMA insertion in this pilot study, standard painful stimulation such as tetanic stimulation (STIM) was still required in further research [34,35,36].
5 Conclusion
The importance of our results was that PPG-derived nonlinear variables could correctly grade part of the relations of remifentanil concentrations and monitor the trend of analgesia depth. ApEn and SampEn with judicious choice of k value were both practical approaches in reflecting the underlying changes when different remifentanil concentrations were administrated.
References
Eger EI, Sonner JM. Anaesthesia defined (gentlemen, this is no humbug). Best Pract Res Clin Anaesthesiol. 2006;20:23–9.
Guignard B. Monitoring analgesia. Best Pract Res Clin Anaesthesiol. 2006;20:161–80.
Fechner J, Ihmsen H, Schuttler J, et al. The impact of intra-operative sufentanil dosing on post-operative pain, hyperalgesia and morphine consumption after cardiac surgery. Eur J Pain. 2013;17:562–70.
Steyaert A, De Kock M. Chronic postsurgical pain. Curr Opin Anesthesiol. 2012;25:584–8.
Gruenewald M, Ilies C. Monitoring the nociception-anti-nociception balance. Best Pract Res Clin Anaesthesiol. 2013;27:235–47.
Korhonen I, Yli-Hankala A. Photoplethysmography and nociception. Acta Anaesthesiol Scand. 2009;53:975–85.
Huiku M, Uutela K, van Gils M, et al. Assessment of surgical stress during general anaesthesia. Br J Anaesth. 2007;98:447–55.
Bonhomme V, Uutela K, Hans G, et al. Comparison of the Surgical Pleth Index (TM) with haemodynamic variables to assess nociception-anti-nociception balance during general anaesthesia. Br J Anaesth. 2011;106:101–11.
Edry R, Recea V, Dikust Y, et al. Preliminary intraoperative validation of the nociception level index a noninvasive nociception monitor. Anesthesiology. 2016;125:193–203.
Choi BM, Park C, Lee YH, et al. Development of a new analgesic index using nasal photoplethysmography. Anaesthesia. 2018;73:1123–30.
Ni ZQ, Wang L, Meng J, et al. EEG signal processing in anesthesia feature extraction of time and frequency parameters. Procedia Environ Sci. 2011;8:215–20.
Jordan D, Stockmanns G, Kochs EF, et al. Electroencephalographic order pattern analysis for the separation of consciousness and unconsciousness an analysis of approximate entropy, permutation entropy, recurrence rate, and phase coupling of order recurrence plots. Anesthesiology. 2008;109:1014–22.
Wei Q, Liu Q, Fan SZ, et al. Analysis of EEG via multivariate empirical mode decomposition for depth of anesthesia based on sample entropy. Entropy. 2013;15:3458–70.
Kreuzer M. EEG based monitoring of general anesthesia: taking the next steps. Front Comput Neurosci. 2017;11:Art 56.
Koskinen M, Seppanen T, Tong SB, et al. Monotonicity of approximate entropy during transition from awareness to unresponsiveness due to propofol anesthetic induction. IEEE Trans Biomed Eng. 2006;53:669–75.
Vakkuri A, Yli-Hankala A, Talja P, et al. Time-frequency balanced spectral entropy as a measure of anesthetic drug effect in central nervous system during sevoflurane, propofol, and thiopental anesthesia. Acta Anaesthesiol Scand. 2004;48:145–53.
Schnider TW, Minto CF, Gambus PL, et al. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology. 1998;88:1170–82.
Minto CF, Schnider TW, Egan TD, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997;86:10–23.
Pincus SM. Approximate entropy as a measure of system complexity. Proc Natl Acad Sci USA. 1991;88:2297–301.
Bruhn J, Ropcke H, Hoeft A. Approximate entropy as an electroencephalographic measure of anesthetic drug effect during desflurane anesthesia. Anesthesiology. 2000;92:715–26.
Liu Q, Chen YF, Fan SZ, et al. A comparison of five different algorithms for EEG signal analysis in artifacts rejection for monitoring depth of anesthesia. Biomed Signal Process Control. 2016;25:24–34.
Pincus SM, Goldberger AL. Physiological time-series analysis: what does regularity quantify. Am J Physiol. 1994;266:H1643–H16561656.
Kortelainen J, Koskinen M, Mustola S, et al. Effect of remifentanil on the nonlinear electroencephalographic entropy parameters in propofol anesthesia. In: Conf Proc IEEE Eng Med Biol Soc, 2009. p. 4994–7.
Shalbaf R, Behnam H, Sleigh J, et al. Measuring the effects of sevoflurane on electroencephalogram using sample entropy. Acta Anaesthesiol Scand. 2012;56:880–9.
Richman JS, Moorman JR. Physiological time-series analysis using approximate entropy and sample entropy. Am J Physiol Heart Circ Physiol. 2000;278:H2039–H20492049.
Liang ZH, Wang YH, Sun X, et al. EEG entropy measures in anesthesia. Front Comput Neurosci. 2015;9:Art 16.
Shalbaf R, Behnam H, Sleigh JW, et al. Monitoring the depth of anesthesia using entropy features and an artificial neural network. J Neurosci Methods. 2013;218:17–24.
Rantanen M, Yli-Hankala A, van Gils M, et al. Novel multiparameter approach for measurement of nociception at skin incision during general anaesthesia. Br J Anaesth. 2006;96:367–76.
Smith WD, Dutton RC, Smith NT. Measuring the performance of anesthetic depth indicators. Anesthesiology. 1996;84:38–51.
Shoushtarian M, Sahinovic MM, Absalom AR, et al. Comparisons of electroencephalographically derived measures of hypnosis and antinociception in response to standardized stimuli during target-controlled propofol–remifentanil anesthesia. Anesth Analg. 2016;122:382–92.
Martini CH, Boon M, Broens SJL, et al. Ability of the Nociception Level, a multiparameter composite of autonomic signals, to detect noxious stimuli during propofol–remifentanil anesthesia. Anesthesiology. 2015;123:524–34.
Weil G, Passot S, Servin F, et al. Does spectral entropy reflect the response to intubation or incision during propofol–remifentanil anesthesia. Anesth Analg. 2008;106:152–9.
von Dincklage F, Correll C, Schneider MHN, et al. Utility of nociceptive flexion reflex threshold, bispectral index, composite variability index and noxious stimulation response index as measures for nociception during general anaesthesia. Anaesthesia. 2012;67:899–905.
Gruenewald M, Ilies C, Herz J, et al. Influence of nociceptive stimulation on analgesia nociception index (ANI) during propofol–remifentanil anaesthesia. Br J Anaesth. 2013;110:1024–30.
Renaud-Roy E, Stöckle P-A, Maximos S, et al. Correlation between incremental remifentanil doses and the Nociception Level (NOL) index response after intraoperative noxious stimuli. Can J Anesth. 2019;66:1049–61.
Funcke S, Sauerlaender S, Pinnschmidt HO, et al. Validation of innovative techniques for monitoring nociception during general anesthesia a clinical study using tetanic and intracutaneous electrical stimulation. Anesthesiology. 2017;127:272–83.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No: 81870868), Major Scientific Project of Zhejiang Lab (Grant No: 2018DG0ZX01) and China’s Natural Science Foundation #31627802.
Author information
Authors and Affiliations
Contributions
WC was responsible for study design, data analysis, manuscript preparation and revision. FJ contributed to the study design, data analysis and revised the manuscript for important intellectual content. XC and HC were involved in the study design, data collection, manuscript revision and project supervision. YF and CJ were responsible for data collection and interpretation of data. JM and SC contributed to data analysis and critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed on human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Research Ethics Committee (No. 20170131) and informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, W., Jiang, F., Chen, X. et al. Photoplethysmography-derived approximate entropy and sample entropy as measures of analgesia depth during propofol–remifentanil anesthesia. J Clin Monit Comput 35, 297–305 (2021). https://doi.org/10.1007/s10877-020-00470-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00470-6