Abstract
Thermal imbalances are very common during surgery. Hypothermia exposes the patient to post-operative shivering, cardiac dysfunction, coagulopathy, bleeding, wound infection, delayed anesthesia recovery, prolonged hospital stay and increased hospitalization cost. There are many factors contributing to intraoperative hypothermia. This is a prospective cohort study conducted through observation and measurement of pediatric surgical patients’ temperature. Convenience sampling methods were used in this study. Initial skin temperature and core temperature at 10 min, 30 min,1 h, 2 h, 3 h, 4 h, 5 h, 6 h and at the end of surgery were recorded. Body temperature was monitored from time of transfer to the operating table until recovery and discharge to the respective pediatric ward. The overall incidence of intraoperative hypothermia was still very high at about 46.6% even though active and passive temperature management were carried out during surgery. Patient’s age, body weight, duration of surgery, type of surgery, intraoperative blood loss, type of anesthesia and operating room temperature were factors that contributed to intraoperative hypothermia. Hypothermia is common in surgery, especially in major and long duration surgery. Intraoperative hypothermia can be life threatening if it is not handled carefully. Various methods are used before, during and after surgery to maintain a patient’s body temperature within the normothermia range. The use of an active warming device like the Bair Hugger® air-forced warming system seems to be a good method for reducing the risk of intraoperative hypothermia and effectively maintaining body temperature for all major and minor surgeries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
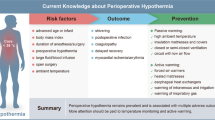
Thermal imbalances during surgery are common [1]. The body core temperature drops by 1 to 2 degrees Celcius (°C) following induction of anesthesia [1]. Hypothermia is defined as a fall in body core temperature to below 35 °C. Children lose their body core temperature faster than adults due to their body mass to body surface ratio. Hypothermia, even for a short duration, increases the risk of adverse outcomes for patients undergoing minor or major surgery regardless of age.
Heat loss takes place by the mechanism of radiation, conduction, convection and evaporation at the body surface or through the airway [2]. Inadvertent hypothermia also exposes patients to the risk of post-operative shivering, postoperative myocardial ischemia, coagulopathy, surgical bleeding, wound infection and delayed recovery from anesthesia [3,4,5,6,7]. Even a short duration of 30 min is known to cause adverse outcomes. Hypothermia also prolongs the stay in hospital, which incurs a higher cost [8]. Therefore, intraoperative temperature monitoring is important to detect, prevent and treat hypothermia in the early stages of a patient’s surgery. Moreover, low environmental temperatures during surgery and anesthesia cause intraoperative hypothermia.
The aim of this research is to study the effect of type of surgery, age, ambient operating temperature and initial temperature on core temperature of patients during surgery. This study also aims to explore the factors affecting intraoperative hypothermia and the best methods to maintain body temperature at normothermia. We concentrated on 8 factors that had been implicated in pediatric anesthesia regarding temperature management.
Several studies using prospective and randomized trial methodology were carried out to identify the risk factors for an imbalance in temperature during perioperative and peri-anesthetic hypothermia. The phenomenon of heat loss during the perioperative and peri-anesthetic stages of surgery has been well known since the 1960s. However, it is important to identify the best method of reducing the risk of hypothermia to a minimum during and immediately after surgery.
2 Materials and methods
This is a prospective cohort study conducted through observation and collection of temperature data in pediatric surgical patients. The primary goal of the study is to determine any association between age, body weight, type of surgery, total blood loss and type of anesthesia in the occurrence of hypothermia. In particular data are collected on the following parameters and analyzed statistically: (1) Operating room temperature, (2) Age, (3) Body weight, (4) Type of operation, (5) Type of anesthesia, (6) Duration of surgery, (7) Type of warming devices, (8) Blood loss.
Convenience sampling methods were used in this study. Anesthesia was induced in the operation theatre in all pediatric patients. No premedication was given to the child pre-operatively. Hold-mask anesthesia was used for minor and short duration surgeries, which is above 30 min and less than 1 h. A total of 854 surgical cases were selected from the elective surgery list over a period of 18 months but only 502 cases fulfilled the criteria for this study.
The study was carried out after obtaining permission from the director of the University of Malaya Medical Centre (UMM), as well as from the Medical Centre Research Committee (MCRC). Before obtaining verbal consent, the purpose of the study was explained to the parents or guardians of the patients. They were then assured that all of the data collected would remain strictly anonymous and confidential, and would be used for academic purposes only. The purpose of the study was also explained to the Master of Anesthesiology students who were participating in the data collection.
There were three different ambient operating room (OR) temperature settings, ≥ 23 °C, 23 °C (22.5–23.5 °C) and ≤ 23 °C. In the “low” OR group, the OR temperature ranged between 20.5–22.5 °C and in the “high” OR group, the range was 23.5–27.0 °C. The recording of operating room temperature, core temperature and skin temperature began at “patient on table”. The initial skin temperature and core temperature at 10 min, 30 min, and 1 h, 2 h, 3 h, 4 h, 5 h, 6 h and at the end of the surgery were recorded. The core temperature was recorded by insertion of a nasopharyngeal probe. The skin temperature was recorded by placing the probe at the patient’s armpit or axilla with the arm kept adducted at all times. Patients with fever, sepsis and surgical procedures shorter than 30 min were excluded from the study. All babies were placed on a constant electric warming blanket with a temperature of 38.5 °C (101.3 °F). The babies were covered when the core temperature measurements were taken. The head was covered by a stocking cap, while the legs and arms were covered by orthoban to keep the baby warm during surgery. Infusion fluids were warmed to 37 °C (98.6 °F) before intravenous transfusion was given. If a blood transfusion was needed during surgery, the blood was warmed to 37° (98.6 °F). The breathing system was not heated, but a “humid-vent” was connected to the tracheal tube connector in all pediatric patients. Warmed peritoneal irrigation fluids of 37 °C (98.6 °F) were used during surgery and, if necessary, a warm abdominal pack was also used to cover the abdominal organs. The babies were covered with one layer of linen surgical drape during surgery.
The study data were analyzed focusing on age, body weight, types of surgery (major surgery: Any elective or emergent surgical procedure that usually involves general anesthesia and/or respiratory assistance, in which a major body cavity is penetrated and exposed, or for which a substantial impairment of physical or physiological functions is produced; Minor surgery: Any elective or emergent surgical procedure that does not involve general anesthesia and/or respiratory assistance), duration of the surgery core and skin temperature and ambient operating room temperature.
Data were analyzed using the Statistical Package for Social Science (SPSS version 11.5) The tested variables were age, gender, body weight, race, duration of the procedure, type of surgery, type of anesthesia and anesthetic drugs, duration of recovery stay, total blood transfusion and estimated blood loss during surgery. Descriptive statistics were used to describe the study sample and the measures. A repeated measure of variance (ANOVA) was performed in this study to examine the correlation between age, body weight, duration of surgery, type of surgery, type of anesthesia and anesthetic drugs in relation to intraoperative hypothermia. The level of significance for all inferential statistical tests was set at 0.05 to indicate a significant difference in perioperative temperature (to compensate for multiple comparisons).
3 Results
A total of 854 surgical cases were selected from the elective surgery list over a period of 18 months and divided into four groups (neonate, infant, toddler and older child). Only 502 surgical cases fulfilled the eligibility criteria. In terms of percentage, there were 63 percent male patients and 33 percent female patients enrolled in this study. The majority of the patients were Malay (48%), followed by Chinese (33%), Indian (17%), local ethnic minorities (Punjabi, Iban and Bajau) and foreigners (Indonesian, Burmese and Sudanese). The highest percentage of pediatric surgical patients were in the older children group (6 to 12 years) at 37%, followed by infants (1 month to 1 year) at 31%, toddlers (2 to 5 years) at 30% and neonates (1 day to 28 days) at 2%.In terms of body weight, the majority of patients were in the underweight range 1 kg to 15 kg (57%) followed by 16 kg to 30 kg (32%), 31 kg to 45 kg (7%) and above 46 kg (4%). The mean (± SD) body weight of patients was 16.23 ± 11.88 kg, the median was 13 kg and the mode was 13 kg. The minimum body weight was about 1 kg and the maximum body weight was about 66 kg. In terms of duration of surgery, 73.1% of patients underwent surgery for 30 min to 2 h, 14.7% for 2 to 4 h, 6.8% for 4 to 6 h and 5.4% for more than 6 h. Of the different patient groups, infants (43.1%) comprised the largest group undergoing major surgery, followed by older children (27.5%), toddlers (24.2%) and neonates (5.2%) (Table 1). Major surgery involves the opening of a body cavity such as laparotomy and thoracotomy. In terms of minor surgery, the majority of patients were from the older child group (39.6%), followed by toddlers (33.2%), infants (26.1%) and neonates (1.1%) (Table 2).
In terms of types of anesthesia, 55.4% of the patients underwent anesthesia with “Intermittent Positive-Pressure Ventilation” (IPPV) or “Laryngeal Mask Airway” (LMA). Another 29.3% underwent combined anesthesia IPPV or LMA with regional anesthesia (caudal, spinal or epidural anesthesia), while 12.7% of patients were sedated using the hold-mask technique. An extremely small percentage of patients underwent minor and short surgeries such as excision biopsy, circumcision and herniotomy via tracheostomy (Fig. 1). Figure 2 shows the trends in core temperature for different categories of pediatric patient. During the first 10 to 30 min of anesthesia, a slight drop in core temperature was observed in all categories of patient. A decrease of 1 °C (33.8 °F) in core temperature was found in neonates, and the p value was > 0.05 due to the small number of patients (12/502). The decrease in core temperature was 0.1 °C (32.18 °F) in infants, 1 °C (33.8 °F) in toddlers and 0.3 °C (32.54 °F) in older children. However, after 30 min of anesthesia, core temperatures increased in infants while the core temperatures of toddlers and older children were still decreasing and remained lower than those of the infant group. Mean core temperature showed a slight increase in the first 10 min after anesthesia irrespective of different initial core temperatures. The core temperatures in all categories of patient increased drastically after 1 h due to the use of the various warming devices available.
There were three different ambient operating room (OR) temperature settings, ≥ 23 °C, 23 °C (22.5–23.5 °C) and ≤ 23 °C. In the “low” OR group, the OR temperature ranged between 20.5–22.5 °C and in the “high” OR group, the range was 23.5–27.0 °C. Mean core and skin temperatures significantly decreased 10 min after the induction of anesthesia and continually decreased afterwards in neonates, infants, toddlers and older children. One hundred and thirty-four (26.7%) pediatric patients underwent surgery in theatres where the operating room temperature settings were above 23 °C while 83 (16.5%) patients experienced 23 °C ambient temperatures and 285 (56.8%) patients experienced below 23 °C temperatures. Core temperature showed an increase in all patients (neonates, infants, toddlers and middle child group) for whom warming devices were used during surgery. There was a mild drop of 0.2 °C to 0.3 °C (32.36 °F to 32.54 °F) in core temperature where operating room temperature settings were above 23 °C after 180 min. This was due to the core-peripheral re-distribution of internal heat, which was dependent on the type and dose of anesthesia, the amount of surgical exposure, ambient temperatures and use of warming devices (Fig. 3).
Comparison between major and minor surgery among the four groups of children shows that core temperatures changed for major and minor surgery within 30 min, regardless of age, after anesthesia induction. The mean core temperature of all patients decreased after 10 min of anesthesia induction (Fig. 4). The core temperature increased after 120 min of surgery due to the use of warming devices.
There were 153 major operations and 349 minor operations in this study. The majority of patients had a surgical blood loss of less than 50 mls (84.3%). Only 8.2% had a surgical blood loss of 50 mls to 100 mls, while the percentages of those with a surgical blood loss of 100 mls to 150 mls (2%) and 150 mls to 200 mls (1.2%) were even smaller. About 4.3% of patients had a blood loss of more than 200 mls during major and long duration surgery. The majority of patients did not need a blood product transfusion (89.6%), and only 10.4% of the patients received a blood transfusion during surgery.
There were no other statistically significant differences when controlling for (1) Operating room temperature, (2) Age, (3) Body weight, (4) Type of operation, (5) Type of anesthesia, (6) Duration of surgery. This may be due to small samples and a future study will be warranted to look in more detail at all these.
4 Discussion
The overall incidence of intraoperative hypothermia in this study was noted to be high (53.2%) despite active and passive temperature management during surgery. The percentage of hypothermia was 83.3% for neonate, is 56.1% for infants, 46.4% for toddlers and 54.4% for older children. About 1.2% of the children developed moderate hypothermia (core temperature between 28 °C and 32 °C) at the end of surgery. There were many factors contributing to the intraoperative hypothermia noted in this study. The incidence of inadvertent intraoperative hypothermia was higher in neonates, infants and toddlers compared with older children. The older children had a slower body heat loss during the intraoperative period due to their large body surface ratio compared with the younger children; therefore, their temperature loss was slower compared to the younger children. This study also shows that the ambient operating room temperature can significantly affect the core temperature of neonates, infants, toddlers and older children during surgery. However, neonates and infants cannot maintain their core temperature during surgery even with a warmer ambient operating room temperature. Major surgery, longer duration of surgery, type of anesthesia, and age of child are risk factors for inadvertent hypothermia. This study also reveals current intraoperative core temperature practice and management in a teaching hospital. It is important to identify the clinical risk factors contributing to intraoperative hypothermia. With this, optimal thermal management can be carried out to maintain patient core temperature during surgery. There are many methods which can be used to maintain a patient’s body core temperature and to prevent excessive heat loss due to the effect of anesthesia and environmental factors, for example theatre ambient temperature control, the use of an intravenous infusion warmer, an orthoban (cotton wool) wrap followed by a plastic wrap on the extremities and an overhead heater. Plastic covering on the torso and extremities is an inexpensive and effective method for reducing the incidence of intraoperative hypothermia by 21 to 46% among preterm neonates. However, it should be used with caution to prevent the risk of hyperthermia [9]. In this study, we found that a combination of a Bair Hugger®, Thermamed® warming blanket and a fluid warmer is best for maintaining intraoperative core temperature. Blood loss was minimal therefore discarded as factor in the analysis.
This study also shows that neonates, infants, toddlers and older children are unable to maintain their core temperature regardless of operating room temperature and type of surgery, even though various types of maintaining measure are taken during surgery. Their core temperature will fall 10 min after administration of anesthesia drugs and gases. Neonates, infants and toddlers do worse compared with older children. In contrast, neonates, infants and toddlers are more stable with high operating room temperature settings and during short duration surgery. However, we have to bear in mind that we only have 12 neonates in this study and it may not be representative in general. Controlling for the various possible factors influencing core temperature lead to smaller groups being compared and thus a larger study may be warranted to remove more possible confounders.
The major causes of a decrease in core temperature are anesthetic induced inhibition of tonic thermoregulatory vasoconstriction and core-to-peripheral redistribution of body heat. A large amount of body heat will flow rapidly to the periphery, and even effective active heating systems often fail to prevent core hypothermia during the first hour of surgery. However, the main key to maintaining normothermia is minimizing the re-distribution process during relatively short operations. Thus, various types of warming device are used to maintain normothermia and prevent excessive heat loss during surgery. From observations made during this study, the use of the Bair Hugger® warming system, Thermamed® active warming blanket and infusion warmer (Anemex® and Hotline®) are sufficient to maintain core temperature and prevent the risk of moderate hypothermia, which is caused by anesthetic drugs and physiological changes in a cool environment (Fig. 5). A few studies have shown that the active warming blanket is very effective in maintaining the intraoperative body core temperature [10]. In contrast, two infants (aged 4 months and 6 weeks) sustained first and secondary degree thermal burns due to the incorrect use of the Bair Hugger® cub blanket [11]. Burn injuries were reported in a case report on children who had undergone short duration and minor surgery (circumcision) [12], and another severe burn injury was associated with the improper use of a forced-air warming device [13,14,15]. According to Azzam & Krock (1995), common types of misuse are the following five types of operator error, (1) warming non-perfused or poorly perfused skin, (2) contact of heated plastic with skin, (3) use of the delivery host without a warming cover, (4) use of other manufacturer’s warming cover and (5) use of the Bair Hugger® model 200/250 with anesthetized patients, whereas this model is recommended for use on conscious patients because it has a higher heat output and a higher set thermostat. Improper use of an active warming blanket will expose the patient to the risk of thermal burn injury. Therefore, active warming blankets need to be used cautiously and according to the manufacturer’s recommendations. In our study, there were no thermal burns reported in any of the surgery cases.
Although many studies of inadvertent intraoperative hypothermia have been carried out in western countries, this is the first study of inadvertent hypothermia incidence to be carried out in a middle income developing ASEAN country such as Malaysia. The study reveals a high incidence of inadvertent hypothermia and identifies the risk factors that affect intra-operative core temperature maintenance.
Hypothermia prevention measures should be taken to prevent inadvertent hypothermia during surgery in all children regardless of their age, type of surgery and type of anesthesia. Several professional societies, such as the Association of Perioperative Registered Nurses (AORN) and the National Institute for Health and Care Excellence (NICE) [16,17,18], have recommended various strategies for improving intra-operative core temperature management. With these measures, the incidence of inadvertent intraoperative hypothermia can be reduced to a minimum.
References
Sessler D. Perioperative thermoregulation and heat balance. The Lancet. 2016;387(10038):2655–64. https://doi.org/10.1016/S0140(15)00981-2.
Diaz JH. Perinatal anesthersia and critical care. Philadelphia: W.B. Saunder Company; 1991.
Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209–15. https://doi.org/10.1056/NEJM199605093341901.
Tander B, Bari S, Karakaya D, Ariturk E, Rizalar R, Bernay F. Risk factors influencing inadvertent hypothermia in infants and neonates during anesthesia. Pediatr Anesth. 2005;15:574–9.
Stoddart PA, Lauder GR. Problems in anesthesia: pediatric anesthesia. London: Martin Dunitz; 2004.
Agrawal N, Sewell DA, Griswold ME, Frank SM, Hessel TW, Eisele DW. Hypothermia during head and neck surgery. Am Laryngol Rhinol Otol Soc Inc. 2003;113(8):1278–1282.
Frank SM, Nguyen JM, Garcia CM, Barnes A. Temperature monitoring practices during regional anesthesia. Anesth Analg. 1999;88(2):373–7.
Sessler DI. (2002). Temperature disturbances Gregory G.A’s pediatric anesthesia. (4th ed.). New York: Churchill Livingstone. pp. 53–84.
Uzun G, Mutluoglu M, Evinc R, Ozdemir O, Sen H. Severe burn injury associated with misuse of forced-air warming device. J Anesth. 2010; 24:980–981. https://doi.org/10.1007/s00540-010-1031-1.
Yi J, Xiang ZY, Deng XM, Fan T, Fu RG, Geng WM, Guo RH, He N, Li CH, Li L, Li M, Li TZ, Tian M, Wang G, Wang L, Wang TL, Wu AS, Wu D, Xue XD, Xu MG, Yang XM, Yang ZM, Yuan JH, Zhao QH, Zhou GQ, Zuo MZ, Pan S, Zhan LJ, Yao M, Huang YG. Incidence of inadvertent intraoperative hypothermia and its risk factors in patients undergoing general anesthesia in Beijing: a prospective regional survey. PLoS ONE. 2015. https://doi.org/10.1371/journal.pone.0136136.
Azzam FK, Krock JL. Thermal burn in two infants associated with a forced air warming system (letter). Anesth Analg. 1995;81(3):661.
Kafrouni H. & Fadel Z.Thermal injury due to use of a forced air warming blanket during paediatric surgery. Anaesth Crit Care Pain Med. 2016;35(2):175. https://doi.org/10.1016/j.accpm.2015.11.003.
Metha SP. Burn injuries from warming devices in the operating room. Am Soc Anaesthesiol. 2013;77(2):16–7.
Chung K, Lee SM, Oh SC, Choi J, Cho HS. Thermal burn injury associated with a forced-air warming device. Korean J Anesthesiol. 2012 Apr;62(4):391–2. https://doi.org/10.4097/kjae.2012.62.4.391.
Oatley HK, Blencowe H, Lawn JE. (2016). The effect of coverings, including plastic bags and wraps, on mortality and morbidity in preterm and full-term neonates. J Perinatol. 2016;36:S82–S88. https://doi.org/10.1038/jp.2016.35.
Guideline for the prevention of unplanned patient hypothermia. In: Guidelines for perioperative practice. Denver, CO: AORN, Inc. https://www.aorn.org/guidelines/clinical-resources/clinical-faqs/hypothermia. Accessed 17 Nov 2015
Guideline for a safe environment of care, part 2. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc. https://www.aorn.org/guidelines/clinical-resources/clinical-faqs/hypothermia. Accessed 17 Nov 2015.
NICE. Inadvertent hypothermia overview. National Institute for Health and Clinical Excellent. http://pathways.nice.org.uk/pathways/inadvertent-perioperative-hypothermia. Accessed 2016.
Author information
Authors and Affiliations
Contributions
LLL designed the current study protocol, data collection tool and database with substantial intellectual input from Professor LC and Professor SR. Data collection was performed by LLL. Data cleaning, validation and queries were performed by LLL. All statistical analysis was performed by LLL with advice from Professor SR. Contributions to interpretation of data were received from all authors. First draft of manuscript was written by LLL with intellectual input from Professor LC. In addition, critical review of and contributions to subsequent drafts were received from Dr. KSN Associate Professor MHS, Professor LC and Professor SR. All authors reviewed and approved the final draft of the manuscript prior to submission. All authors agree to be accountable for the accuracy and integrity of the piece of work.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the director of University of Malaya Medical Centre (UMMC), as well as from the Medical Centre Research Committee (MCRC).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lai, LL., See, MH., Rampal, S. et al. Significant factors influencing inadvertent hypothermia in pediatric anesthesia. J Clin Monit Comput 33, 1105–1112 (2019). https://doi.org/10.1007/s10877-019-00259-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00259-2