Abstract
The aim of this study was to investigate the effect of controlled hypotension on cerebral oxygen saturation (rSO2) using near infrared spectroscopy (NIRS) and evaluation of postoperative cognitive function in patients undergoing rhinoplasty. Fifty adult patients who were scheduled for elective rhinoplasty surgery and required controlled hypotension were enrolled in this prospective study. Controlled hypotension was provided using a combination of propofol and remifentanil infusion supplemented with nitroglycerin infusion as necessary. rSO2 was evaluated during controlled hypotension by NIRS. Cerebral desaturation was observed in 5 out of 50 patients (10 %) during hypotensive anesthesia. The greatest decrease from baseline was 28 % when MAP was 57 mmHg. In both non-desaturated and desaturated patients, postoperative MMSE scores were significantly lower than preoperative scores. There was a 4 % decrease in the non-desaturated patients and a 7 % decrease in the desaturated patients when preoperative and postoperative MMSE scores were compared. A decline in cognitive function 1 day after surgery was observed in 23 patients (46 %) and in all patients with intraoperative cerebral desaturation. The current study showed that even if SpO2 is in the normal range, there might be a decrease of more than 20 % in cerebral oxygen saturation during controlled hypotension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Controlled hypotension decreases arterial pressure to reduce blood loss and the need for transfusion during surgery, as well as to improve the quality of the surgical field [1]. Controlled hypotension is defined as a reduction of the systolic blood pressure to 80–90 mmHg, a reduction of mean arterial pressure (MAP) to 50–65 mmHg or a 30 % reduction of baseline MAP [2]. The reduction of bleeding is essential in surgery of the middle ear, endoscopic sinus surgery, plastic and reconstructive microsurgery, ophthalmologic surgery and neurosurgery, which all have low hemorrhagic potential, to ensure a clear surgical field [1, 2].
Rhinoplasty is considered to be one of the most challenging procedures in both the field of aesthetic surgery and otolaryngology. The anatomical features of the nose along with the unique properties, which make the reshaping of the tissue uncomplicated, compounded by the complication of intraoperative bleeding, all make the surgeon’s postoperative goal more difficult to achieve. Many rhinoplasty surgeons prefer to work with a controlled hypotensive anesthesia. Decreased intraoperative bleeding allows the surgeon to visualize the operative field better in turn allowing for a better analysis of the tissue and a more comfortable utilization of preferred techniques [3–5].
Controlled hypotension could result in tissue ischemia of the vital organs and the inhibition of the autonomic nervous system. None of the current data indicate that controlled hypotension with a MAP between 50 and 65 mmHg is a risk in young and healthy patients. However, most candidates for controlled hypotension have organ dysfunctions that are not detectable by a clinical examination [1].
Near infrared spectroscopy (NIRS) provides a continuous means of noninvasively monitoring the oxygenation of cerebral venous (75 %) and arterial (25 %) blood. NIRS measures the ratio of oxyhemoglobin to total hemoglobin in a field beneath the sensor, and this ratio is expressed as a percentage of regional cerebral oxygen saturation (rSO2) [6]. NIRS is widely used to provide real-time information on cerebral oxygenation in patients undergoing various procedures, including cardiac [7], orthopedic [8], laparoscopic [9] and abdominal surgery [10]. However, the relationship between rSO2 and controlled hypotension has not been established in patients undergoing rhinoplasty.
It was hypothesized that controlled hypotension would reduce rSO2 during rhinoplasty. Therefore, the aim of this study was to investigate the effects of controlled hypotension in rSO2 using NIRS and evaluation of postoperative cognitive function.
2 Methods
2.1 Study protocol
After receiving approval from the local institutional research ethics committee and written informed consent from each patient, 50 American Society of Anesthesiology (ASA) I patients who were scheduled for elective rhinoplasty and required controlled hypotension were enrolled in this prospective study. Exclusion criteria were as follows: patients who did not give consent, ASA II and above, age under 18 years, body mass index over 30 kg/m2, anticoagulation therapy, previous hypersensitivity to any of the study drugs and/or a preoperative Mini Mental State Examination (MMSE) score of 23 or less.
The study patients were kept fasting following the standard guidelines and premedicated with 0.02 mg/kg of intravenous (IV) midazolam 15 min prior to the induction of anesthesia. In the operating room, all patients were in supine position. Standard monitoring (electrocardiogram, non-invasive blood pressure, pulse oximetry, temperature) was applied. Further, rSO2 was bilateral monitored using NIRS. Sensors for cerebral oximetry were placed bilaterally on the right and left sides of forehead before the induction of anesthesia.
The patients’ age, weight and height were noted. Measurements of MAP, heart rate (HR), peripheral oxygen saturation (SpO2), right and left rSO2, end-tidal carbon dioxide (Et-CO2) and body temperature were recorded before induction of anesthesia (baseline), after induction of anesthesia (0 min) and every 5 min thereafter.
After preoxygenation, anesthesia was induced with propofol (2 mg/kg), lidocaine (1 mg/kg), rocuronium (0.6 mg/kg) and remifentanil (0.25 mcg/kg/min). After endotracheal intubation, ventilation was started using a 60 % air-in-oxygen mixture (tidal volume, 8 mL/kg; respiratory rate, 12 bpm). Anesthesia was maintained with propofol (8–12 mg/kg/h) and remifentanil (0.1–0.3 mcg/kg/min) infusion during anesthesia. All patients received IV saline at 5 mL/kg/h. After induction of anesthesia, hypotension was induced and maintained at a target MAP of 50–60 mmHg with continuous infusion of propofol and remifentanil. If the target MAP could not be induced, nitroglycerin infusion was started. When incidental hypotension below the target MAP occurred, a bolus of ephedrine was applied to restore MAP to the target level.
Cerebral desaturation was defined as a reduction of rSO2 to lower than 80 % of baseline for ≥15 s. When cerebral desaturation occurred, a two-step treatment was planned: The first step was to check and correct anesthesia circuit, fraction of inspired O2, Et-CO2 and MAP. If the first step failed to restore an acceptable rSO2, propofol and remifentanil infusion doses were decreased and MAP was increased with intravascular fluid administration and ephedrine.
The cognitive function of the patients was assessed using the MMSE test 1 day before and 1 day after surgery. A decrease in the MMSE score ≥2 points from baseline was considered as an index of decline in cognitive function.
The duration of surgery, duration of anesthesia, number of patients for whom nitroglycerin infusion was required and the time that desaturation occurred were also recorded.
2.2 The INVOS system
We used an INVOS 5100C oximeter (Somanetics, Covidien, Minneapolis, USA), which provides a continuous, non-invasive, real-time measurement of cerebral oxygenation. The INVOS 5100 is a two-channel (right + left) NIRS cerebral oximeter which automatically registers which sensor it is connected to and uses sensor-dependent algorithms for the calculation of rSO2.
2.3 Statistical analysis
The normality assumption was checked using the Shapiro–Wilk test. The paired-samples Wilcoxon test was used to compare MMSE. Nonparametric Spearman correlation analysis was used to analyse the relationship between MAP and rSO2. The distribution of gender among desaturated patients were analysed by Fisher’s exact test. For all analyses, IBM SPSS version 21.0 was used and the statistical significance was set at p < 0.05.
3 Results
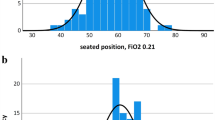
The demographic data and duration of anesthesia and surgery of the non-desaturated and desaturated patients are presented in Table 1. The changes in HR, MAP, SpO2, and rSO2 are shown in Fig. 1.
Cerebral desaturation was observed in 5 out of 50 patients (10 %) during hypotensive anesthesia. The greatest decrease from baseline was 28 % when MAP was 57 mmHg. None of the episodes of cerebral desaturation which occurred during hypotensive anesthesia were associated with a reduction in SpO2 or a decrease in Et-CO2. In patients with cerebral desaturation, rSO2 recovered to acceptable values with ephedrine and intravascular fluid administration.
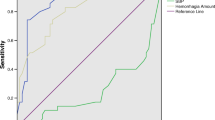
Preoperative and postoperative MMSE scores of all patients are shown in Table 2. In both non-desaturated and desaturated patients, postoperative MMSE scores were significantly lower than preoperative scores (p < 0.001 and p = 0.042, respectively). There was a 4 % decrease in the non-desaturated patients and a 7 % decrease in the desaturated patients when preoperative and postoperative MMSE scores were compared. A decline in cognitive function 1 day after surgery was observed in 23 patients (46 %) and in all patients with intraoperative cerebral desaturation. To evaluate whether there was any individual change in rSO2 response to a lowering of MAP, right rSO2 and left rSO2 were correlated with MAP each time. A correlation between rSO2 and MAP could not be established during hypotensive anesthesia.
4 Discussion
The initial studies of controlled hypotensive anesthesia during rhinoplasty published in 1968 by Chayen and Kaplan [11]. In this area they have focused on the types of anesthetics and their effect on controlled hypotension during surgery. One commonality in the studies is the conclusion: controlled hypotensive anesthesia is essential in rhinoplasty. Unlike previous examples in the literature, our study aims to examine the limits of controlled hypotensive anesthesia, and as such, is the first of its kind in rhinoplasty literature. Additionally, the findings of the study can be extended beyond rhinoplasty to any procedures, which require controlled hypotensive anesthesia.
The goal of controlled hypotension is to maintain a pressure which is sufficiently low to allow a reduction in bleeding without suppressing the microcirculatory autoregulation of the vital organs (i.e. the brain, heart or kidney) [1]. A reduction of MAP to 55–65 mmHg or a decrease of 30 % from baseline is safe in terms of end organ perfusion and oxygen delivery [12].
To apply controlled hypotension, some anesthetic drugs such as propofol, inhalation anesthetics and opioids are used alone or in combination [1]. Propofol has become popular in providing controlled hypotension; it has the characteristics of rapid onset and recovery times with a short half-life and duration of action. Propofol seems to be more effective in reducing blood loss than volatile anesthetics [13]. Remifentanil, a short-acting rapid-onset and offset opioid, has a hypotension effect [14] that provides a bloodless operative field in inducing controlled hypotension with no need for additional potent hypotensive agents [15]. Total intravenous anesthesia (TIVA) with remifentanil and propofol is a more effective technique to obtain reduced bleeding in rhinoplasty than fentanyl combined with inhalation anesthesia [16]. In addition, TIVA can reduce pressure to the desired level and maintain a bloodless operative field when used for controlled hypotension in ear surgery [2]. Many clinical studies have shown that, TIVA with propofol and remifentanil is useful to achieve controlled hypotension.
Cerebral oxygenation can be measured using invasive or non-invasive methods. Unlike invasive methods such jugular bulb oximetry and brain tissue oxygen tension sensors, NIRS is applied easily. NIRS and invasive methods of monitored cerebral oxygenation have similar effects [17–19].
Absolute rSO2 below 40 and a decline of more than 25 % from the baseline are associated with neurologic dysfunction and adverse outcomes [20]. A reduction of 15–20 % from the baseline or a reduction below 50 has been used as a critical threshold for concern and initiation of interventions [21, 22]. Therefore, in our study, a reduction in rSO2 of 20 % from the baseline was accepted as threshold and when a decline of more than 20 % occurred, controlled hypotension was stopped and rSO2 recovered to acceptable values.
In a study which investigated the effects of beach-chair position and induced hypotension on rSO2 in patients undergoing arthroscopic shoulder surgery, the beach-chair position combined with induced hypotension decreased rSO2; moreover, cerebral desaturation was seen in two cases whose MAP value decreased below 60 and 55 mmHg. However, a decline in cognitive function measured by MMSE was not observed in any of the patients [8]. In an another study which assessed the effects of controlled hypotension by using nitroglycerin and nicardipine on rSO2 and postoperative cognitive function in patients undergoing orthognathic surgery, when MAP values were reduced to 60–65 mmHg, cerebral desaturation or decreased MMSE scores were not observed in any of the patients [23]. In the present research, when MAP decreased to 50–60 mmHg, cerebral desaturation was observed in five patients.
During controlled hypotension, if MAP reduces to the extent that it impairs cerebral autoregulation, postoperative cognitive dysfunction (POCD) could occur. The possible risk factors contributing to the development of POCD include age, postoperative cognitive function (POCF), operation time, hypoperfusion, embolism, postoperative pain, respiratory complications and infections [24]. In a study which assessed cognitive outcomes after controlled hypotension where MAP was reduced to 45–55 or 55–70 mmHg in 235 elderly patients when compared with preoperative neuropsychological testing, no impairment in POCF was noted at 1 week or 4 months postoperatively [25]. None of these studies reported that controlled hypotension decreased MMSE scores with or without the observation of cerebral desaturation [5, 23]. In contrast to these studies, in the present research, when compared with preoperative baseline MMSE scores, a significant decline in cognitive function was noted at 1 day postoperatively in both desaturated and non-desaturated patients. Moreover, this decline was more pronounced in desaturated patients.
The limitations of the current study are that we only evaluated cognitive function using the MMSE test and assessed the MMSE test postoperatively only once, at 1 day after surgery and there wasn’t a control group to compare effects of controlled hypotension among the patients with hypotension or not.
In conclusion, the results of the current study showed that even if SpO2 is in the normal range, there might be a decrease of more than 20 % in cerebral oxygen saturation during controlled hypotension. Furthermore, for NIRS-based cerebral oximetry during controlled hypotension, the INVOS cerebral oximeter may be a helpful monitoring tool for detecting real-time rSO2 changes.
References
Degoute CS. Controlled hypotension: a guide to drug choice. Drugs. 2007;67:1053–76.
Degoute CS, Ray MJ, Manchon M, Dubreuil C, Banssillon V. Remifentanil and controlled hypotension; comparison with sodium nitroprusside or esmolol during tympanoplasty. Can J Anesth. 2001;48:20–7.
Jacobi KE, Bohm BE, Rickauer AJ, Jacobi C, Hemmerling TM. Moderate controlled hypotension with sodium nitroprusside does not improve surgical conditions or decrease blood loss in endoscopic sinus surgery. J Clin Anesth. 2000;12:202–7.
Koşucu M, Omür S, Beşir A, Uraloğlu M, Topbaş M, Livaoğlu M. Effects of perioperative remifentanil with controlled hypotension on intraoperative bleeding and postoperative edema and ecchymosis in open rhinoplasty. J Craniofac Surg. 2014;25:471–5.
Tuncel U, Turan A, Bayraktar MA, Erkorkmaz U, Kostakoglu N. Efficacy of dexamethasone with controlled hypotension on intraoperative bleeding, postoperative oedema and ecchymosis in rhinoplasty. J Craniomaxillofac Surg. 2013;41:124–8.
Tobias JD. Cerebral oxygenation monitoring: near-infrared spectroscopy. Expert Rev Med Devices. 2006;3:235–43.
Yao FS, Tseng CC, Ho CY, Levin SK, Illner P. Cerebral oxygen desaturation is associated with early postoperative neuropsychological dysfunction in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18:552–8.
Lee JH, Min KT, Chun YM, Kim EJ, Choi SH. Effects of beach-chair position and induced hypotension on cerebral oxygen saturation in patients undergoing arthroscopic shoulder surgery. Arthroscopy. 2011;27:889–94.
Li XM, Shao MT, Wang JJ, Wang YL. Relationship between post-operative cognitive dysfunction and regional cerebral oxygen saturation and β-amiloid protein. J Zhejiang Univ Sci B. 2014;15:870–8.
Casati A, Fanelli G, Pietropaoli P, Proietti R, Tufano R, Danelli G, Fierro G, De Cosmo G, Servillo G. Continuous monitoring of cerebral oxygen saturation in elderly patients undergoing major abdominal surgery minimizes brain exposure to potential hypoxia. Anesth Analg. 2005;101:740–7.
Chayen M, Kaplan I. Methoxyflurane and controlled hypotension in corrective rhinoplasty. Br J Plast Surg. 1968;21:168–9.
Petrozza PH. Induced hypotension. Int Anesth Clin. 1990;28:223–9.
Boonmak S, Boonmak P, Laopaiboon M. Deliberate hypotension with propofol under anesthesia for functional endoscopic sinus surgery (FESS). Cochrane Database Syst Rev. 2013;6:CD006623. doi:10.1002/14651858.CD006623.pub2.
Patel SS, Spencer CM. Remifentanil. Drugs. 1996;52:417–28.
Degoute CS, Ray MJ, Gueugniaud PY, Dubreuil C. Remifentanil induces consistent and sustained controlled hypotension in children during middle ear surgery. Can J Anaesth. 2003;50:270–6.
Tirelli G, Bigarini S, Russolo M, Lucangelo U, Gullo A. Total intravenous anaesthesia in endoscopic sinus-nasal surgery. Acta Otorhinolaryngol Ital. 2004;24:137–44.
McLeod AD, Igielman F, Elwell C, Cope M, Smith M. Measuring cerebral oxygenation during normobaric hyperoxia: a comparison of tissue microprobes, near-infrared spectroscopy and jugular venous oximetry in head injury. Anesth Analg. 2003;97:851–6.
Kim MB, Ward DS, Cartwright CR, Kolano J, Chlebowski S, Henson LC. Estimation of jugular venous O2 saturation from cerebral oximetry or arterial O2 saturation during isocapnic hypoxia. J Clin Monit Comput. 2000;16:191–9.
Daubeney PE, Pilkington SN, Janke E, Charlton GA, Smith DC, Webber SA. Cerebral oxygenation measured by near-infrared spectroscopy: comparison with jugular bulb oximetry. Ann Thorac Surg. 1996;61:930–4.
Edmonds HL Jr, Ganzel BL, Austin EH III. Cerebral oximetry for cardiac and vascular surgery. Semin Cardiothorac Vasc Anesth. 2004;8:147–66.
Samra SK, Dy EA, Welch K, Dorje P, Zelenock GB, Stanley JC. Evaluation of a cerebral oximeter as a monitor of cerebral ischemia during carotid endarterectomy. Anesthesiology. 2000;93:964–70.
Rigamonti A, Scandroglio M, Minicucci F, Magrin S, Carozzo A, Casati A. A clinical evaluation of near-infrared cerebral oximetry in the awake patient to monitor cerebral perfusion during carotid endarterectomy. J Clin Anesth. 2005;17:426–30.
Choi SH, Lee SJ, Jung YS, Shin YS, Jun DB, Hwang KH, Liu J, Kim KJ. Nitroglycerin- and nicardipine-induced hypotension does not affect cerebral oxygen saturation and postoperative cognitive function in patients undergoing orthognathic surgery. J Oral Maxillofac Surg. 2008;66:2104–9.
Krenk L, Rasmussen LS, Kehlet H. New insights into the pathophysiology of postoperative cognitive dysfunction. Acta Anaesthesiol Scand. 2010;54:951–6.
Williams-Russo P, Sharrock NE, Mattis S, Liguori GA, Mancuso C, Peterson MG, Holllenber J, Ranawat C, Salvati E, Sculco T. Randomized trial of hypotensive epidural anesthesia in older patients. Anethesiology. 1999;91:926–35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Erdem, A.F., Kayabasoglu, G., Tas Tuna, A. et al. Effect of controlled hypotension on regional cerebral oxygen saturation during rhinoplasty: a prospective study. J Clin Monit Comput 30, 655–660 (2016). https://doi.org/10.1007/s10877-015-9768-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9768-6