Abstract
Extravascular lung water (EVLW) could increase by permeability pulmonary oedema, cardiogenic oedema, or both. Transthoracic echocardiography examination of a patient allows quantifying B-lines, originating from water-thickened interlobular septa, and the E/Ea ratio, related to pulmonary capillary wedge pressure. The aim of our study was to assess the correlation and the trending ability between EVLW measured by transpulmonary thermodilution and the B-lines score or the E/Ea ratio in patients with ARDS. Twenty-six intensive care unit patients were prospectively included. B-lines score was obtained from four ultrasound zones (anterior and lateral chest on left and right hemithorax). E/Ea was measured from the apical four-chamber view. EVLW was compared with the B-lines score and the E/Ea ratio. A linear mixed effect model was used to take account the repeated measurements. A p value <0.05 was considered significant. A total of 73 measurements were collected. The correlation coefficient between EVLW and B-lines score was 0.66 (EVLW = 0.71 B-lines + 7.64, R2 = 0.44, p = 0.001), versus 0.31 for E/Ea (p = 0.06). The correlation between EVLW changes and B-lines variations was significant (R2 = 0.26, p < 0.01), with a concordance rate of 74 %. A B-lines score ≥6 had a sensitivity of 82 % and a specificity of 77 % to predict EVLW >10 ml/kg, with an AUC equal to 0.86 (0.76–0.93). The gray zone approach identified a range of B-lines between four and seven for which EVLW >10 ml/kg could not be predicted reliably. The correlation between ultrasound B-lines and EVLW was significant, but the B-lines score was not able to track EVLW changes reliably.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Acute respiratory distress syndrome (ARDS) might be associated with an increase of extravascular lung water (EVLW), which is the amount of water contained in the lungs outside the pulmonary vasculature. That is the sum of interstitial, alveolar, intracellular, and lymphatic fluids, except pleural effusion. EVLW is an independent risk-factor of 28 day mortality in patients with ARDS [1]. Moreover, there was some evidence that the EVLW guided treatment reduced mortality rate in patients with permeability pulmonary oedema [2], therefore methods to accurately quantify the amount of EVLW may be of value to clinicians who treat patient with ARDS [3]. EVLW can be measured by devices using transpulmonary thermo-dilution. The estimation of EVLW by a single (cold) indicator has been shown closely correlated with the double indicator dilution technique (thermo-dye): the coefficient correlation was 0.96 and the mean bias (SD) was −0.5 (1.9) ml/kg [4].
Echographic examination of the lung surface may reveal B-lines artifact originated from water-thickened interlobular septa. The inter-rater reliability of quantifying pleural B-lines is acceptable with an intraclass coefficient correlation equal to 0.89 (0.87–0.91) [5]. The number of B-lines has been shown to correlate with EVLW and pulmonary capillary wedge pressure [6]. However, there are few studies evaluating the correlation between B-lines and EVLW in critically ill patients with ARDS [7]. Moreover, there is no validated model to estimate EVLW based on an ultrasound score in this setting, therefore the ability of B-lines score to predict EVLW and its changes in clinical practice is unknown.
In addition, a septic shock associated with ARDS could impair left ventricular relaxation and induce a diastolic dysfunction, which could lead to heart failure and pulmonary oedema [8]. Volume expansion, performed at the early phase of sepsis to improve organ perfusion, could increase EVLW by permeability pulmonary oedema, cardiogenic oedema, or both. The peak velocity of the mitral annulus early wave during diastole (Ea), measured by tissue Doppler imaging, was reduced in patient with impaired relaxation [9]. The ratio between the peak velocity of the mitral annulus early wave (E wave measured by pulse-Doppler) and Ea related well to pulmonary capillary wedge pressure [9, 10], which has been shown to correlate with the number of B lines [6, 11, 12] and therefore might be correlated with EVLW changes.
The primary aim of our study was to assess the correlation between B-lines score, E/Ea ratio and EVLW measured by transpulmonary thermodilution (TPTD) in patients with ARDS, and evaluate the accuracy of this model to predict an increase of EVLW. The secondary aim was to evaluate the ability of B-lines score and E/Ea ratio to detect a variation of EVLW.
2 Materials and methods
2.1 Population
This single centre prospective observational study was conducted in the intensive care of Narbonne Hospital (France). After institutional approval, 26 patients admitted in intensive care were included (Fig. 1). No additional invasive procedure or blood samples were necessary for this study, therefore the need for informed consent was waived by the Institutional Review Board of Narbonne Hospital [13]. The inclusion criteria were: ARDS defined in accordance with the Berlin definition [14] and septic shock (hypotension persisting after initial fluid challenge or blood lactate concentration ≥4 mmol/l) requiring an advanced hemodynamic monitoring by TPTD [15]. The etiology of ARDS included in our study was pneumonia. Patients were excluded if they were <18 years old, or if they had severe cardiac valvulopathy, femoral artery stenosis or major pleural effusion.
2.2 Measured variables
Patients characteristics (age, sex, height, and weight), Simplified Acute Physiology Score (SAPS2), use of vasoactive agents, hemodynamic data, i.e. cardiac output, EVLW, heart rate, mean arterial pressure were collected. All patients were ventilated with a tidal volume ranged between 6 and 8 ml/kg. A calibration of EV1000 system was made before each measurement. During the study, the investigators were blinded to each’s other results.
2.3 EVLW measurements
A central venous catheter was inserted into the left or right jugular vein and used for cold indicator injections. A VolumeView™ catheter (Edwards Lifesciences) was inserted through the left or right femoral artery and connected to the EV1000™ monitoring system (software version 1.4). Thermodilution measurements were performed in sets of at least three consecutive injections of 20 ml cold saline, randomly distributed over the respiratory cycle. Bolus sets that contained a bolus that differed by more than 15 % from the mean within the set were considered faulty and excluded from the analysis. The previous study of Bendjelid and coll. showed a good reproducibility with a coefficient of variation equal to 5.7 ± 4.2 % [16]. The exact algorithm to calculate the cardiac output and EVLW has been described elsewhere [16–18]. We used EVLW indexed to predicted body weight (PBW) because this value had been shown to correlate better with PaO2/FiO2 ratio than EVLW indexed to real body weight [19, 20]. PBW (kg) was calculated as 50 + 0.91 * (height in cm—152.4) for males and 45.5 + 0.91 * (height in cm—152.4) for females. Normally, EVLW is inferior to 10 ml/kg [19, 21].
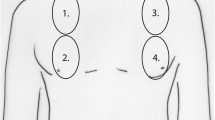
2.4 Ultrasound B-lines Lung Score
The ultrasound scanning of the anterior and lateral chest was obtained on left and right hemithorax, on the second intercostal space at the midclavicular line, and on the fourth intercostal space at the middle axillary line. The inclination of the probe was chosen to obtain a maximum number of B-lines on a frozen image. B-lines at lateral bases were not studied because they were observed in 27 % of healthy subjects [22]. Only four ultrasound zones for each patient were used in our study and the sum of the B-lines of each zone determined the B-lines score. The B-lines were counted in a single rib space at the moment when the most number of B-lines were seen on a frozen image [5]. The B-lines were defined as hyper-echoic, arising strictly from the pleural line, moving with lung sliding, spreading to the edge of the screen without fading, and erasing A lines (Fig. 2) [23]. At the pleural line, the distance between B-lines is roughly 7 mm. The number of B-lines observed in a single rib space was ranged between 0 and 5, therefore the total B-lines score of the four zones was ranged between 0 and 20. The examination was performed using an ultrasound system (“Sonosite™ MicroMaxx”) with a probe of 2–4 MHz.
2.5 Transthoracic echocardiographic measurements
From the apical four-chamber view, transmitral flow velocities were recorded with the pulse wave Doppler sample volume placed at the mitral tips. Peak early (E) and late (A) velocities were recorded, as well as E wave deceleration time (EDT). From the same view, mitral annulus velocities were obtained using tissue Doppler settings, with the Doppler sample volume placed at the lateral side of the mitral annulus. Myocardial systolic velocity (Sa) and early (Ea) velocities were measured, and the E/Ea ratio was calculated. The ejection fraction was measured using the Simpson method.
2.6 Statistical analysis
The normality of the quantitative data was verified using a Shapiro–Wilk test, and expressed as mean ± standard deviation (SD) or median [range]. Based on the previous study of Agricola and coll. [6], at least 26 measurements were needed to test a correlation coefficient of 0.5, with an α-risk of 0.05 and a power of 80 % (logiciel G*Power 3.1.5). Twenty-six patients were included in the study with one to four measures by patient, with a period of 1 day between each measurement. If a patient was weaned from mechanical ventilation, died or was transferred to another department for ExtraCorporeal Membrane Oxygenation, the inclusion of patient data was stopped, therefore a variable number of measurements was realized for each patient. To take account repeated measurements, a linear mixed effect model was used to assess the correlation between EVLW, B-lines score, E/Ea ratio and PaO2/FiO2 ratio [24]. A multivariate linear mixed effect model was used to test the correlation of EVLW with B-lines score and E/Ea ratio. The Akaike information criterion (AIC) was used to choose the optimal model. The normality of the data was verified and a bootstrap procedure (1000 permutations) was used to estimate coefficients if the distribution was not Gaussian. When three experimented operators were simultaneously available (B.B., P-E.M., P.C.), the intraclass correlation coefficients (ICC) of B-lines score and E/Ea ratio were evaluated on a random sample of 10 patients to assess the inter-observer reproducibility of the echographic measurements. Interobserver variability was calculated as the ratio (expressed as percentage) of the difference between the values obtained by each observer (expressed as absolute value) divided by the mean of the two values. Intraobserver variability was calculated by a similar approach.
A ROC curve, corrected for repeated measurements by a generalized linear mixed effect model [25], was used to determine the optimal B-lines threshold predicting EVLW >10 ml/kg and EVLW >15 ml/kg [21, 26]. The highest sum of sensitivity and specificity was considered as being the optimal threshold. The accuracy was defined as (true positive + true negative)/(positive + negative). The “gray zone” was determined using a 2-step procedure [27, 28]. The first step consisted of the determination of the optimal threshold for the B-lines score. The second step was conducted to determine the values for which the B-lines score did not provide conclusive information. We defined inconclusive responses for values presenting with either sensitivity <90 % or specificity <90 %. The gray zone was then defined as the values of the B-lines score that did not allow having 10 % of diagnosis tolerance. However, if the 95 % confidence interval of the optimal threshold was larger than the inconclusive zone, the values obtained during the first step were retained as gray zone.
A four quadrant plot was used to test the trending ability of the B-lines score [29]. The concordance rate was defined as the percentage of the total number of data point changing in the same direction (i.e. data points located in the upper right and lower left corners of Fig. 5). When a central exclusion zone of 15 % was used, a concordance rate superior to 90 % was considered acceptable [29].
A Jonckheere–Terpstra test was performed to test a relationship among EVLW, B-lines score, E/Ea ratio, and ARDS severity (determined based on the lowest PaO2/FiO2 ratio during the study period) [30]. For this analysis, only the data corresponding to the lowest value of PaO2/FiO2 for each patient were retained.
A p value <0.05 was considered significant. The statistical analysis was performed using R software (R Foundation, Vienna, Austria), Tanagra 1.4.45 (Rakotomalala, Lyon University, France) and SPSS 20 (Armonk, NY: IBM Corp).
3 Results
From January 2013 through February 2014, twenty-six patients with ARDS were included in this study (Fig. 1). No patient was excluded for an insufficient echogenicity. A total number of 73 measurements were analyzed. The demographic data were described in Table 1. The ICC, performed on a sample of 10 patients, was 0.93 (95 % CI 0.75–0.98) for the B-lines score and 0.94 (95 % CI 0.80–0.99) for the E/Ea ratio. For B-lines score, the interobserver variability was 11.3 ± 7.9 % (which represents a median [range] variation of 1 [0–3] B lines between 2 observers) and intraobserver variability was 8.8 ± 6.3 %. For E/Ea ratio, the interobserver variability was 6.1 ± 4.7 % and intraobserver variability was 4.2 ± 3.6 %.
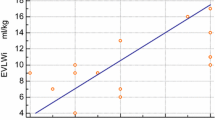
3.1 Correlations with EVLW
Analysis of the overall relationship between EVLW and B-lines score (Fig. 3) showed a significant correlation between EVLW and B-lines score (R2 = 0.44, AIC = 354, p = 0.001). There was no significant correlation between EVLW and E/Ea (R2 = 0.10, AIC = 387, p = 0.055). A multivariate linear mixed effect model, including B-lines score and E/Ea, did not improve the correlation with EVLW (R2 = 0.47, AIC = 354). The PaO2/FiO2 ratio appeared correlated with EVLW (R2 = 0.32, p = 0.001) and B-lines score (R2 = 0.18, p = 0.002), but not with E/Ea (R2 = 0.02, p = 0.32) (Table 2). No significant correlation was found between EVLW and the other parameters such as left ventricular ejection fraction, Sa, EDT or E/A ratio.
3.2 Receiver operating characteristic (ROC) analysis
A B-lines score ≥6 had a sensitivity of 82 % and a specificity of 77 % to predict EVLW >10 ml/kg (Fig. 4), with an accuracy of 81 % and an Area Under the Curve (AUC) equal to 0.86 (95 % CI 0.76–0.93, p < 0.001). The positive predictive value (PPV) was 94 % and the negative predictive value (NPV) was 48 %. The gray zone approach identified a range of B-lines between 4 and 7 for which EVLW >10 ml/kg could not be predicted reliably. A B-lines score ≥10 had a sensitivity of 83 % and a specificity of 79 % to predict EVLW >15 ml/kg, with an accuracy of 79 % and an AUC equal to 0.86 (95 % CI 0.76–0.93, p < 0.001). The PPV was 44 % and the NPV was 96 %. The gray zone predicting EVLW >15 ml/kg was ranged between 9 and 12 B-lines.
3.3 Trending ability
The linear mixed effect model showed a significant correlation between ΔEVLW and ΔB-lines (R2 = 0.26, p < 0.01). The concordance rate without data exclusion was 74 % (95 % CI 60–85 %) (n = 35/47): 26 % of variations in EVLW yielded opposite changes, i.e. negative variation with one technique and positive with the other. These data points are located in the upper left and lower right corners of Fig. 5. When a central exclusion zone of 15 % was used (i.e. ΔEVLW <2 ml/kg and ΔB lines <2), the concordance rate was 76 % (95 % CI 62–86 %) (n = 22/29). There was no significant correlation between ΔEVLW and ΔE/ΔEa (R2 = 0.04, p = 0.21).
3.4 Relationship among EVLW, B-lines score, E/Ea ratio, and ARDS severity
ARDS severity was determined based on the lowest PaO2/FiO2 ratio measured during the study period. The median [range] values of EVLW (ml/kg) for mild, moderate and severe ARDS were 10 [8–12], 13 [7.6–16.3] and 16.6 [10.4–27], respectively (p = 0.001). ARDS severity was associated with an increase of B-lines score (mild, 5 [1–8]; moderate, 9 [5–12]; severe, 11 [4–18]; p = 0.005; Fig. 6). There was no significant correlation between E/Ea ratio and ARDS severity (p = 0.97).
4 Discussion
To our knowledge, this is the first prospective observational study, conducted in critically ill patients with ARDS, assessing the accuracy of an echographic model to predict EVLW and its variations. We showed a significant correlation between the ultrasound B-lines score and EVLW (EVLW = 0.71 B-lines + 7.64, R2 = 0.44). A B-lines score ≥6 had a sensitivity of 82 % and a specificity of 77 % to detect a pathologic value of EVLW >10 ml/kg, with a gray zone between 4 and 7 B-lines.
In cardiac surgery setting, Agricola and coll. [6] had found a significant correlation between EVLW determined by the PICCO™ system and B-lines (R = 0.42). We have also observed a significant correlation between EVLW and B-lines (R = 0.66), even if our methodology was different: in the study of Agricola and coll. the patients with lung diseases were excluded, only 4 chest zones were included in our study to calculate the simplified B-lines score and the algorithm to determinate EVLW used by the EV1000™ system was slightly different of the PICCO™ algorithm [17]. The PICCO™ algorithm to calculate EVLW is based on the time of the temperature decay between two set points in the thermodilution curve, while the EV1000™ algorithm relies on maximum up-slope and maximum down-slope of the thermodilution curve.
The correlation between EVLW and E/Ea ratio was not significant in our study. The number of B-lines had been previously shown to correlate with wedge pressures (R = 0.48) [6] and the degree of diastolic dysfunction [31]. However, in patients with ARDS, the permeability pulmonary oedema is the primum movens of the increased EVLW and could explain the poor relationship between EVLW and E/Ea ratio. In addition, E/Ea variations, reflecting changes in wedge pressures, were not clinically relevant to track EVLW alterations, at least in ARDS setting.
The correlation between ΔEVLW and ΔB-lines was significant. This is coherent with the study of Noble and coll. [32]: the authors had shown that during dialysis every 500 ml volume removed induced a decrease of 2.7 B-lines. However, in our study, the concordance rate of 74 % was poor, therefore an invasive monitoring by TPTD seems necessary for an accurate evaluation of EVLW changes.
Our study had some limitations. The most significant was the use of an imprecise reference method. The measurement of EVLW is actually based on gravimetry [33, 34], pulmonary imaging [7] or transpulmonary dilution marker methods [4]. The gold standard for in vivo EVLW assessment is represented by quantitative computed tomography scan, which is often not feasible, requiring the transfer of a critical patient to the radiology department. Moreover the computed tomography scan employs ionizing radiations that do not allow repeating it to study EVLW changes. We have not compared EVLW measured with EV1000 with a chest radiographic score: the study of Brown and coll. [26] has clearly showed that the change in daily chest radiograph scores was not predictive of time to death, by contrast with PaO2/FiO2 ratio or EVLW changes measured by TPTD that predicted mortality. Likewise, the correlation between EVLW and the chest radiograph score was moderate (R = 0.35). Furthermore, the PaO2/FiO2 ratio, the level of PEEP and the value of EVLW might have slightly increased the bias of EVLW measurements [4]. Even if our model may be useful to estimate EVLW at the admission of a patient with acute respiratory failure, it is imperfect and an invasive monitor is necessary if an accurate EVLW measurement is needed. This was confirmed by the fact that the correlation between PaO2/FiO2 ratio and EVLW (R = −0.57) was better than the correlation between PaO2/FiO2 ratio and B-Lines score (R = −0.43) or E/Ea ratio (R = −0.16).
Moreover, the pulmonary capillary wedge pressure was not measured [35], and could be abnormally elevated and interfere with the diagnosis of ARDS. However, the E/Ea ratio was relatively low (7 ± 2) with a range between 4 and 13. An E/Ea threshold >15 has been previously shown predictive of a wedge pressure >15 mmHg [36, 37]. None of our patient had an E/Ea ratio >13, therefore a pure cardiogenic oedema was unlikely [12].
The results could have been operator-dependent or echograph-dependent. The ICC of B-lines score (ICC = 0.93) and E/Ea ratio (ICC = 0.94) were acceptable, therefore the influence of the operator was irrelevant. However, the model could have been different with another type of echograph: the B-lines are artifacts that depend of echographic parameters. In our study, only one echograph was used, with a probe of 2–4 MHz. The results were also limited by the range of EVLW between 6 and 28 ml/kg, therefore we cannot extrapolate to higher values.
In conclusion, in patients with ARDS, the correlation between ultrasound B-lines score and EVLW was significant and might be useful to detect a pathologic value of EVLW at ICU admission. However, the poor trending ability justifies an invasive monitoring by TPTD to track EVLW changes accurately.
References
Jozwiak M, Silva S, Persichini R, Anguel N, Osman D, Richard C, Teboul JL, Monnet X. Extravascular lung water is an independent prognostic factor in patients with acute respiratory distress syndrome. Crit Care Med. 2013;41:472–80.
Eisenberg PR, Hansbrough JR, Anderson D, Schuster DP. A prospective study of lung water measurements during patient management in an intensive care unit. Am Rev Respir Dis. 1987;136:662–8.
Sakka SG. Extravascular lung water in ARDS patients. Minerva Anestesiol. 2013;79:274–84.
Michard F, Schachtrupp A, Toens C. Factors influencing the estimation of extravascular lung water by transpulmonary thermodilution in critically ill patients. Crit Care Med. 2005;33:1243–7.
Anderson KL, Fields JM, Panebianco NL, Jenq KY, Marin J, Dean AJ. Inter-rater reliability of quantifying pleural B-lines using multiple counting methods. J Ultrasound Med. 2013;32:115–20.
Agricola E, Bove T, Oppizzi M, Marino G, Zangrillo A, Margonato A, Picano E. “Ultrasound comet-tail images”: a marker of pulmonary edema—a comparative study with wedge pressure and extravascular lung water. Chest. 2005;127:1690–5.
Baldi G, Gargani L, Abramo A, D’Errico L, Caramella D, Picano E, Giunta F, Forfori F. Lung water assessment by lung ultrasonography in intensive care: a pilot study. Intensive Care Med. 2013;39:74–84.
Bouhemad B, Nicolas-Robin A, Arbelot C, Arthaud M, Feger F, Rouby JJ. Isolated and reversible impairment of ventricular relaxation in patients with septic shock. Crit Care Med. 2008;36:766–74.
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30:1527–33.
Lamia B, Maizel J, Ochagavia A, Chemla D, Osman D, Richard C, Teboul JL. Echocardiographic diagnosis of pulmonary artery occlusion pressure elevation during weaning from mechanical ventilation. Crit Care Med. 2009;37:1696–701.
Agricola E, Picano E, Oppizzi M, Pisani M, Meris A, Fragasso G, Margonato A. Assessment of stress-induced pulmonary interstitial edema by chest ultrasound during exercise echocardiography and its correlation with left ventricular function. J Am Soc Echocardiogr. 2006;19:457–63.
Miglioranza MH, Gargani L, Sant’anna RT, Rover MM, Martins VM, Mantovani A, Weber C, Moraes MA, Feldman CJ, Kalil RA, Sicari R, Picano E, Leiria TL. Lung ultrasound for the evaluation of pulmonary congestion in outpatients: a comparison with clinical assessment, natriuretic peptides, and echocardiography. JACC Cardiovasc Imaging. 2013;6:1141–51.
Byerly WG. Working with the institutional review board. Am J Health Syst Pharm. 2009;66:176–84.
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637.
Bendjelid K, Giraud R, Siegenthaler N, Michard F. Validation of a new transpulmonary thermodilution system to assess global end-diastolic volume and extravascular lung water. Crit Care. 2010;14:R209.
Kiefer N, Hofer CK, Marx G, Geisen M, Giraud R, Siegenthaler N, Hoeft A, Bendjelid K, Rex S. Clinical validation of a new thermodilution system for the assessment of cardiac output and volumetric parameters. Crit Care. 2012;16:R98.
Sakka SG, Reuter DA, Perel A. The transpulmonary thermodilution technique. J Clin Monit Comput. 2012;26:347–53.
Berkowitz DM, Danai PA, Eaton S, Moss M, Martin GS. Accurate characterization of extravascular lung water in acute respiratory distress syndrome. Crit Care Med. 2008;36:1803–9.
Zhang Z, Lu B, Ni H. Prognostic value of extravascular lung water index in critically ill patients: a systematic review of the literature. J Crit Care. 2012;27(420):e1–8.
Tagami T, Sawabe M, Kushimoto S, Marik PE, Mieno MN, Kawaguchi T, Kusakabe T, Tosa R, Yokota H, Fukuda Y. Quantitative diagnosis of diffuse alveolar damage using extravascular lung water. Crit Care Med. 2013;41:2144–50.
Lichtenstein D, Meziere G, Biderman P, Gepner A, Barre O. The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med. 1997;156:1640–6.
Lichtenstein DA, Meziere GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134:117–25.
Glaser D, Hastings RH. An introduction to multilevel modeling for anesthesiologists. Anesth Analg. 2011;113:877–87.
Honghu L, Tongtong W. Estimating the area under a receiver operating characteristic curve for repeated measures design. J Stat Softw. 2003;8:1–18.
Brown LM, Calfee CS, Howard JP, Craig TR, Matthay MA, McAuley DF. Comparison of thermodilution measured extravascular lung water with chest radiographic assessment of pulmonary oedema in patients with acute lung injury. Ann Intensive Care. 2013;3:25.
Le Manach Y, Hofer CK, Lehot JJ, Vallet B, Goarin JP, Tavernier B, Cannesson M. Can changes in arterial pressure be used to detect changes in cardiac output during volume expansion in the perioperative period? Anesthesiology. 2012;117:1165–74.
Cannesson M, Le Manach Y, Hofer CK, Goarin JP, Lehot JJ, Vallet B, Tavernier B. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a “gray zone” approach. Anesthesiology. 2011;115:231–41.
Critchley LA, Lee A, Ho AM. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–92.
Kushimoto S, Endo T, Yamanouchi S, Sakamoto T, Ishikura H, Kitazawa Y, Taira Y, Okuchi K, Tagami T, Watanabe A, Yamaguchi J, Yoshikawa K, Sugita M, Kase Y, Kanemura T, Takahashi H, Kuroki Y, Izumino H, Rinka H, Seo R, Takatori M, Kaneko T, Nakamura T, Irahara T, Saito N. Relationship between extravascular lung water and severity categories of acute respiratory distress syndrome by the Berlin definition. Crit Care. 2013;17:R132.
Frassi F, Gargani L, Gligorova S, Ciampi Q, Mottola G, Picano E. Clinical and echocardiographic determinants of ultrasound lung comets. Eur J Echocardiogr. 2007;8:474–9.
Noble VE, Murray AF, Capp R, Sylvia-Reardon MH, Steele DJ, Liteplo A. Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest. 2009;135:1433–9.
Venkateswaran RV, Dronavalli V, Patchell V, Wilson I, Mascaro J, Thompson R, Coote J, Bonser RS. Measurement of extravascular lung water following human brain death: implications for lung donor assessment and transplantation. Eur J Cardiothorac Surg. 2013;43:1227–32.
Tagami T, Kushimoto S, Yamamoto Y, Atsumi T, Tosa R, Matsuda K, Oyama R, Kawaguchi T, Masuno T, Hirama H, Yokota H. Validation of extravascular lung water measurement by single transpulmonary thermodilution: human autopsy study. Crit Care. 2010;14:R162.
Sandham JD, Hull RD, Brant RF, Knox L, Pineo GF, Doig CJ, Laporta DP, Viner S, Passerini L, Devitt H, Kirby A, Jacka M. A randomized, controlled trial of the use of pulmonary–artery catheters in high-risk surgical patients. N Engl J Med. 2003;348:5–14.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–94.
Dokainish H, Zoghbi WA, Lakkis NM, Al-Bakshy F, Dhir M, Quinones MA, Nagueh SF. Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation. 2004;109:2432–9.
Conflict of interest
We disclose no conflicts of interest, past or future, from all the authors. Our work has not been funded by any source in addition to our regular and independent salary. We have no financial interest in the subject, in the materials or equipment used in the manuscript, or its competitors. All authors are in complete agreement with the contents of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bataille, B., Rao, G., Cocquet, P. et al. Accuracy of ultrasound B-lines score and E/Ea ratio to estimate extravascular lung water and its variations in patients with acute respiratory distress syndrome. J Clin Monit Comput 29, 169–176 (2015). https://doi.org/10.1007/s10877-014-9582-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9582-6