Abstract
There have been conflicting reports on whether propofol prolongs, shortens, or does not change QT interval. The aim of this study was to determine the effect of target-controlled infusion (TCI) of propofol on heart rate-corrected QT (QTc) interval during anesthetic induction. We examined 50 patients undergoing lumbar spine surgery. Patients received 3 μg/kg of fentanyl and were randomly allocated to one of the following 2 groups. Group S patients received 5 mg/kg of thiamylal followed by sevoflurane, 5 % at the inhaled concentration. Group P patients received propofol using TCI system at 5 μg/mL for 2 min followed by 3 μg/mL. Tracheal intubation was performed after vecuronium administration. Heart rate (HR), mean arterial pressure (MAP), bispectral index score (BIS), and QTc interval in 12-lead electrocardiogram were recorded at the following time points: just before fentanyl administration (T1), 2 min after fentanyl injection (T2), 1 min after thiamylal injection or 2 min after the start of TCI (T3), just before intubation (T4), and 2 min after intubation (T5). BIS and MAP significantly decreased after anesthetic induction in both groups. HR decreased after anesthetic induction and recovered after tracheal intubation in group P, whereas it did changed in group S throughout the study period. QTc interval was shortened at T3 and T4 in group P, but prolonged at T3, T4, and T5 in group S, as compared with T1. Propofol TCI shortens QTc interval, whereas sevoflurane prolongs QTc interval during anesthetic induction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The QT interval of electrocardiogram (ECG) represents myocardial depolarization and repolarization. Prolongation of heart rate-corrected QT (QTc) interval is associated with life-threatening dysrhythmias such as polymorphic ventricular tachycardia called “torsade de pointes.” Thus, it is important to determine whether the anesthetics used prolong QTc interval. Volatile anesthetics, including sevoflurane, are known to prolong QT interval significantly [1]; further, thiopental and thiamylal can also cause marked prolongation of QT interval [2, 3]. However, there have been conflicting reports on whether propofol prolongs [4, 5], shortens [3, 6], or does not change QTc interval [1]. Kim et al. [5] reported that target-controlled infusion (TCI) of propofol prolonged QTc interval. In their study, patients received TCI of propofol at an effect-site concentration of 5 μg/mL for 15 min, while the depth of anesthesia [e.g., using bispectral index score (BIS)] was not evaluated. This study was limited by the fact that the anesthetic dose was not titrated to effect. Our previous study showed that initial (1.5 mg/kg) and additional (0.5 mg/kg) boluses of propofol to maintain bispectral index score (BIS) around 50 shortened the QTc interval during anesthetic induction [3]. Propofol can be administered as a bolus, a continuous infusion, or TCI. Although TCI using compartment pharmacokinetic model (e.g., Marsh model) has the failure to accurately predict the time course of arterial propofol concentrations during the early stages of administration (i.e., anesthetic induction), propofol is administered using TCI techniques and has been proven to be satisfactorily accurate during anesthesia [7].
QT dispersion (QTD), the difference between maximum and minimum QT intervals in a 12-lead ECG, is considered as a measure of repolarization inhomogeneity of the left ventricle and might represent an electrophysiological index for increased ventricular dysrhythmias [8]. Yildirim et al. [9] reported that sevoflurane, isoflurane, and desflurane prolonged QTc interval and QTc dispersion (QTcD). However, Emin et al. reported that sevoflurane and desflurane prolonged the QTc interval but did not influence the QTD [10]. Our previous study showed that bolus administration of propofol did not change QTcD [3].
The aim of this randomized, open-label, clinical study was to determine the effects of propofol and sevoflurane on QTc interval and QTcD during anesthetic induction by setting a comparable depth of anesthesia.
2 Methods
2.1 Patients
We studied 50 American Society of Anesthesiologists (ASA) physical status 1 or 2 patients aged 20–79 years who had undergone elective lumbar spine surgeries such as laminectomy, microscopic discectomy, microendoscopic discectomy, or spinal fusion under general anesthesia between July 2008 and March 2009. The study protocol was approved by the Institutional Research and Ethic Committee, and a written informed consent was obtained from each participant. The exclusion criteria included medical history of diabetes, ischemic heart disease, preoperative ECG abnormalities and preoperative medications known to prolong QTc interval such as β-adrenergic antagonists, and antiarrhythmic agents. None of the patients received any preanesthetic medication.
2.2 Study protocol
In the operation theater, pulse oximetry, 3-lead ECG, non-invasive blood pressure (BP), and BIS (A2000 BIS Monitoring System; Aspect Medical System, Natick, USA) were monitored as the standard procedure for the patients receiving general anesthesia. The lead II of ECG was recorded continuously for analyzing the incidence of dysrhythmia. A 12-lead ECG was attached to the patients before anesthetic induction. Standard 12-lead ECG was recorded at a paper speed of 25 mm/s at each measurement time by using a computerized ECG recorder (model FX-7432; Fukuda Denshi, Tokyo, Japan). The ECG data was also recorded at a sample rate of 2 ms digitally. QT intervals were measured by a software (QTD-1; Fukuda Denshi, Tokyo, Japan) that detects the onset of the QRS complex and the end of the T wave [3, 11].
QT intervals were corrected for heart rate by using the Fridericia formula [12].
If the QT interval could not be measured reliably due to T-wave morphology, the data were excluded from analysis. A minimum of 6 leads were considered necessary for the analysis. QTcD was defined as the difference between the maximum and minimum QTc values in all leads. A mean QTc interval value was calculated from all available QTc intervals averaged from 3 consecutive cycles in all leads during the measurement time. An investigator blinded to the anesthetic agent examined and analyzed the ECGs.
Patients were randomly divided by sealed envelope assignment into 2 groups, i.e., group S (n = 25) and group P (n = 25). The patients inhaled oxygen via face mask at a flow rate of 5 L/min for 2 min; subsequently, they received 3 μg/kg fentanyl. Two minutes after fentanyl injection, group S received 5 mg/kg of thiamylal followed by sevoflurane at an inhaled concentration of 5 %, and group P received propofol at 5 μg/mL for 2 min followed by 3 μg/mL of an effect-site concentration using TCI infusion system (TCI pump, Marsh’s model, TE-371, Terumo, Tokyo, Japan). Group S received vecuronium, 0.15 mg/kg 1 min after thiamylal injection, whereas group P received it 2 min after the start of TCI, to facilitate tracheal intubation of vecuronium. This time delay was necessary to achieve loss of consciousness. After loss of verval response, the eyelash refrex was continuously tested, and it’s loss was defined as the loss of consciousness [13]. To maintain the BIS score around 50 after loss of consciousness, the inhaled concentration of sevoflurane was controlled at 3–5 % in group S, and the effect-site concentration of propofol was maintained at 3–5 μg/mL in group P. Tracheal intubation was performed 2.5 min after vecuronium injection. The inhaled concentration of sevoflurane was decreased to 1 % after tracheal intubation in group S. Heart rate (HR), mean arterial pressure (MAP), BIS, end-tidal sevoflurane concentration (ETSevo), the corresponding predicted propofol effect-site concentration and cumulative dose of propofol displayed by the TCI pump, and 12-lead ECG were recorded at the following time points: just before fentanyl injection (baseline: T1), 2 min after fentanyl injection (T2), 1 min after thiamylal injection or 2 min after start of TCI (T3), 2.5 min after vecuronium injection (T4), and 2 min after intubation (T5).
2.3 Statistical analysis
The results are expressed as median (IQR[range]). A two-factorial analysis of variance with repeated measures was performed for analyzing the interaction between time and the 2 groups. Post-hoc comparison between the groups at each time point and among the repeated measures in each group was performed by Bonferroni/Dunn procedure, if appropriate. Continuous data for patient characteristics were analyzed using Mann–Whitney U test. Dichotomous variables were analyzed with either Fisher’s exact probability test or Chi square test. A p value less than 0.05 was considered statistically significant.
Sample size was determined on the basis of the previous study (SD, 23 ms) [1], which indicated that, with 22 patients in each group, a power of 90 % would be required to detect a difference of 23 ms in the mean QTc interval between the 2 groups at a significance level of 5 %.
3 Results
Our study included 53 patients, i.e., 37 men and 16 women. Of these, 2 men (1 from each group) and 1 woman (from group S) were excluded because their ECG data were wrongly entered in the software; therefore, 50 patients were included in the study. None of the participants needed vasopressors throughout the study. Table 1 shows patients’ characteristics. There were no significant differences between the 2 groups.
Table 2 shows the incidence of dysrhythmias (APC, VPC). There was no significant difference in the incidence between the 2 groups.
Table 3 shows ETSevo, and predicted effect site concentration and cumulative dose of propofol.
Table 4 shows BIS values and circulatory variables in both the groups. BIS and MAP significantly decreased after anesthetic induction in both the groups. HR in group P significantly decreased after anesthetic induction in group P, and it recovered at T5. QTcD at T5 in group S was significantly prolonged as compared to that at T1, and it was significantly longer than that in group P.
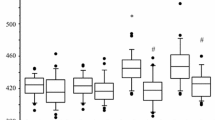
Figure 1 shows the QTc intervals in groups S and P at each time point. Analysis of variance indicates significant effects of both agents (p < 0.0471) and time points (p < 0.0001). The interaction between the anesthetic agent and time was also significant (p < 0.0001). These findings were confirmed by post hoc test. QTc intervals at T3, T4, and T5 were significantly prolonged compared with that at T1 in group S (p = 0.0048, p < 0.0001 and p < 0.0001, respectively). In group P, QTc interval was significantly shortened at T3 (p < 0.0001) and T4 (p = 0.0049), compared to that at T1, but returned to the T1 level at T5. QTc intervals at T3, T4, and T5 in group P were significantly shorter than those in group S (p = 0.0061, p = 0.0006, and p = 0.0124, respectively).
Heart rate corrected QT (QTc) interval in group propofol and sevoflurane at each time point. White boxes represent group sevoflurane, and gray boxes represent group propofol. Values are expressed as median (line inside the boxes), IQR (boxes), and 10–90 percentiles (whiskers). T1, baseline; T2, after fentanyl injection; T3, 2 min after propofol start or 1 min after thiamylal injection; T4, 2 min after vecuronium injection; T5, 2 min after intubation; *p < 0.05 versus T1 values; † p < 0.05 versus group sevoflurane
4 Discussion
Our results suggest that TCI of propofol shortens QTc interval, whereas sevoflurane prolongs it during anesthetic induction; further, QTcD increases after tracheal intubation in patients receiving sevoflurane but is unchanged in the patients receiving propofol.
Our previous [3] and present results are inconsistent with those of Kim et al. [5]. This discrepancy could be explained based on the following reasons. First, our data on QT interval were collected as average leads, whereas Kim et al. obtained the data from a single lead. Second, we used the Fridericia formula, whereas they used the Hodges formula. Third, we evaluated the depth of anesthesia using BIS to maintain adequate anesthetic depth, whereas they administered TCI of propofol at effect-site concentration of 5 μg/mL for 15 min without BIS. Forth, we added bolus of fentanyl to releave the stimulus of tracheal intubation during anesthetic induction.
The average value from 12-lead was selected because of the interlead differences in the QT interval [14]. Bazett’s formula is most widely used for heart rate correction, but it is known to overcorrect QT interval and can lead to a false diagnosis of prolonged QTc interval [12]. Hodges and Fridericia formulae showed similar QTc heart rate dependence at both slower and faster heart rates in normal and prolonged QT interval patient groups [15]. QT interval was corrected for heart rate using Fridericia correction, in accordance with International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use E14 guidance [16].
The changes in QTc interval caused by drugs and anesthetic depth would be the result of the effects on ionic currents in cardiac myocytes. There exist at least 6 distinct potassium currents in cardiac myocytes [17], with the delayed rectifier (IK) and inward rectifier (IK1) potassium currents being the main currents. IK1 is the prime determinant of resting conductance of cardiac myocytes. IK is the key determinant of action potential duration (APD). Inhibition of IK prolongs repolarization and QT interval. It was shown that propofol caused significant depression of IK but had no effect on IK1 at 5 μg/mL (28 μM) [17]. IK current consists of the rapid component (IKr) and the slow component (IKs). Sevoflurane was shown to inhibit IKr channels, which contribute significantly to prolong APD [18]. A recent study showed that propofol caused a concentration-dependent inhibition of IKs in guinea-pig ventricular myocytes but did not inhibit IKr [19]. Furthermore, propofol predominantly suppresses L-type calcium currents (ICa) in a concentration-dependent manner and shortens APD [19]. QTc interval was shortened by 30 μM of propofol in a rabbit heart experimental model [20]. The IC50 s for the effects of propofol to block IKs and ICa were 23 and 9.8 μM, respectively [19]. The anesthetic effect is maintained with blood concentrations ranging from 3.4 (19 μM) to 4.5 (25 μM) μg/mL in humans [20]. The shortening of APD caused by propofol would result from the combined effects on ICa and IKs.
The propofol-induced shortening of QTc interval may be beneficial for patients with prolonged QTc interval undergoing cardioverter–defibrillator implantation in order to prevent further QTc interval prolongation [21]. Kleinsasser et al. [6] reported that sevoflurane-associated QTc interval prolongation was reversible with propofol.
During laryngoscopy and intubation, QTc prolongation may become exacerbated due to sympathetic stimulation. Fentanyl may have prevented QTc prolongation to some extent by attenuating the sympathetic stimulus during intubation. Chang et al. [22] reported that pretreatment with 2 μg/kg of fentanyl significantly attenuated QTc prolongation, while laryngoscopy and tracheal intubation was performed during propofol induction.
Previous studies have shown that QTcD increased in patients with ischemic heart disease [23, 24], and it could be a predictor of dysrhythmic events in congestive heart failure [4]. There have been conflicting reports on whether sevoflurane prolongs QTcD [9, 10]. QT dispersion increases during tracheal intubation in patients with coronary artery disease [25]. The results of this study suggest that QTcD was not affected by sevoflurane alone but was increased by tracheal intubation under sevoflurane anesthesia.
In conclusion, propofol TCI shortens but sevoflurane prolongs QTc interval during anesthetic induction. Unlike propofol, anesthesia with sevoflurane increased QTcD after tracheal intubation. Propofol TCI would be suitable for induction of anesthesia in patients with a risk of ventricular dysrhythmia.
References
Kleinsasser A, Kuenszberg E, Loeckinger A, Keller C, Hoermann C, Lindner KH, Puehringer F. Sevoflurane, but not propofol, significantly prolongs the QT interval. Anesth Analg. 2000;90:25–7.
Lindgren L, Yli-Hankala A, Randell T, Kirvela M, Scheinin M, Neuvonen PJ. Haemodynamic and catecholamine responses to induction of anaesthesia and tracheal intubation: comparison between propofol and thiopentone. Br J Anaesth. 1993;70:306–10.
Higashijima U, Terao Y, Ichinomiya T, Miura K, Fukusaki M, Sumikawa K. A comparison of the effect on QT interval between thiamylal and propofol during anaesthetic induction. Anaesthesia. 2010;65:679–83.
Saarnivaara L, Klemora UM, Lindgren L, Rautiainen P, Suvanto A. QT interval of the ECG, heart rate and arterial pressure using propofol, methohexital or midazolam for induction of anaesthesia. Acta Anaesthesiol Scand. 1990;34:276–81.
Kim DH, Kweon TD, Nam SB, Han DW, Cho WY, Lee JS. Effects of target concentration infusion of propofol and tracheal intubation on QTc interval. Anaesthesia. 2008;63:1061–4.
Kleinsasser A, Loeckinger A, Lindner KH, Keller C, Boehler M, Puehringer F. Reversing sevoflurane-associated Q-Tc prolongation by changing to propofol. Anaesthesia. 2001;56:248–50.
Masui K, Upton RN, Doufas AG, Coetzee JF, Kazama T, Mortier EP, Struys MMRF. The performance of compartmental and physiologically based recirculatory pharmacokinetic models for propofol: a comparison using bolus, continuous, and target-controlled infusion data. Anesth Analg. 2010;111:368–79.
Higham PD, Campbell RWF. QT dispersion. Br Heart J. 1994;71:508–10.
Yildirim H, Adanir T, Atay A, Katircioglu K, Savaci S. The effects of sevoflurane, isoflurane, and desflurane on QT interval of the ECG. Eur J Anaesth. 2004;21:566–70.
Silay E, Kati I, Tekin M, Guler N, Huseyinoglu UA, Coskuner I, Yagmur C. Comparison of the effects of desflurane and sevoflurane on the QTc interval and QT dispersion. Acta Cardiol. 2005;60:459–64.
Ichinomiya T, Terao Y, Miura K, Higashijima U, Tanise T, Fukusaki M, Sumikawa K. QTc interval and neurological outcomes in aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2010;13:347–54.
Charbit B, Samain E, Merckx P, Funck-Brentano C. QT interval measurement. Evaluation of automatic QTc measurement and new simple method to calculate and interpret corrected QT interval. Anesthesiology. 2006;104:255–60.
Kreuer S, Bruhn J, Larsen R, Hoepstein M, Wilhelm W. Comparison of alaris AEP index and bispectral index during propofol-remifentanil anaesthesia. Br J Anaesth. 2003;91:336–40.
Cowan JC, Yusoff K, Moore M, Amos PA, Gold AE, Bourke JP, Tansuphaswadikul S, Campbell RWF. Importance of lead selection in QT interval measurement. Am J Cardiol. 1988;61:83–7.
Chiladakis J, Kalogeropoulos A, Arvanitis P, Koutsogiannis N, Zagli F, Alexopoulos D. Heart rate-dependence of QTc intervals assessed by different correction methods in patients with normal or prolonged repolarization. PACE. 2010;33:553–60.
Darpo B, Nebout T, Sager PT. Clinical evaluation of QT/QTc prolongation and proarrhythmic potential for nonantiarrhythmic drugs: the international conference on harmonization of technical requirements for registration of pharmaceuticals for human use E14 guideline. J Clin Pharmacol. 2006;46:498–507.
Baum VC. Distinctive effects of three intravenous anesthetics on the inward rectifier (IK1) and delayed rectifier (IK) potassium currents in myocardium: implications for the mechanism of action. Anesth Analg. 1993;76:18–23.
Whyte SD, Booker PD, Buckley DG. The effects of propofol and sevoflurane on the QT interval and transmural dispersion of repolarization in children. Anesth Analg. 2005;100:71–7.
Hatakeyama N, Sakuraya F, Matsuda N, Kimura J, Kinoshita H, Kemmotsu O, Yamazaki M, Hattori Y. Pharmacological significance of the blocking action of the intravenous general anesthetic propofol on the slow component of cardiac delayed rectifier K+ current. J Pharmacol Sci. 2009;110:334–43.
Wu MH, Su MJ, Sun SSM. Age-related propofol effects on electrophysiological properties of isolated hearts. Anesth Analg. 1997;84:964–71.
Michaloudis D, Fraidakis O, Kanoupakis E, Flossos A, Manios E. Idiopathic prolonged QT interval and QT dispersion: the effects of propofol during implantation of cardioverter-defibrillator. Eur J Anaesth. 1999;16:842–7.
Chang DL, Kweon TD, Nam SB, Lee JS, Shin CS, Park CH, Han DW. Effects of fentanyl pretreatment on QTc interval during propofol induction. Anaesthesia. 2008;63:1056–60.
Pekdemir M, Karaca I, Cevic Y, Yanturali S, Ikay E. The diagnostic value of QT dispersion for acute coronary syndrome in patients presenting with chest pain and nondiagnostic initial electrocardiograms. Mt Sinai J Med. 2006;73:813–7.
Mirvis DM. Spatial variation of the QT intervals in normal persons and patients with acute myocardial infarction. J Am Coll Cardiol. 1985;5:625–31.
Ay B, Fak AS, Toprak A, Gogus YF, Oktay A. QT dispersion increases during intubation in patients with coronary artery disease. J Electrocardiol. 2003;36:99–104.
Acknowledgments
This research was supported, in part, by research funds of the Japan Labor Health and Welfare Organization to promote function.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oji, M., Terao, Y., Toyoda, T. et al. Differential effects of propofol and sevoflurane on QT interval during anesthetic induction. J Clin Monit Comput 27, 243–248 (2013). https://doi.org/10.1007/s10877-012-9420-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-012-9420-7