Abstract
Genetic testing plays a critical role in diagnosis for many primary immunodeficiency diseases. The goals of this report are to outline some of the challenges that clinical immunologists face routinely in the use of genetic testing for patient care. In addition, we provide a review of the types of genetic testing used in the diagnosis of PID, including their strengths and limitations. We describe the strengths and limitations of different genetic testing approaches for specific clinical contexts that raise concern for specific PID disorders in light of the challenges reported by the clinical immunologist members of the CIS in a recent membership survey. Finally, we delineate the CIS’s recommendations for the use of genetic testing in light of these issues.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Genetic testing has been used in varied forms over the last 30 years for early diagnosis, treatment, and prevention of severe and lethal diseases. The first use of genetic testing in primary immunodeficiency (PID) dates to 1993 more than 40 years after the initial description of X-linked agammaglobulinemia, with the identification of mutations in the BTK gene (Bruton’s Tyrosine Kinase) [1]. Since then, and to a greater extent since massive parallel sequencing became available, the number of genes known to cause immunodeficiency and immune dysregulation disorders has grown tremendously. Improved understanding of the underlying genetic alternation, when combined with clinical data and immune function analysis of a patient with PID can result in faster and more accurate diagnosis. This is facilitated by performing targeted sequencing of candidate genes suspected of causing the patient’s clinical presentation. At the same time, and also as a result of the expanding spectrum of genetic disorders with overlapping clinical presentations, a semi-targeted sequencing approach has been developed using gene panels to sequence multiple candidate genes associated with a relevant symptomatology. When targeted and semi-targeted, sequencing approaches fail or an unbiased approach to testing is advantageous, other tools can be used in an attempt to establish a diagnosis. These include whole exome sequencing, whole genome sequencing or “next generation” sequencing panels that cover subsets or even all-known, clinically relevant genes. In PID, the ability to identify the correct, underlying molecular diagnosis has a direct impact on prognosis and is an important guide for precision management and counseling of the affected patient and family [2].
The goals of this report are to:
-
1.
Outline some of the challenges that clinical immunologists face routinely in the use of genetic testing for patient care
-
2.
Provide a review the of types of genetic testing used in the diagnosis of PID, including their strengths and limitations
-
3.
Describe the strengths and limitations of different genetic testing approaches for specific clinical contexts that raise concern for specific PID disorders in light of the challenges reported by the clinical immunologist members of the CIS
-
4.
Delineate the CIS’s recommendations for the use of genetic testing in light of these issues
Challenges to Using Genetic Testing
The three major challenges to using genetic testing for evaluation of PID are cost, accessibility, and interpretation. Genetic testing expense can vary significantly dependent on the form of testing used. For example, a simple karyotype analysis may cost under $100 whereas genomic approaches currently can cost over $10,000. There is also significant variation between lab pricing and between insurance policies, making it very challenging to predict or anticipate the costs of a specific test for a specific patient. The expense of genetic testing is decreasing as technology improves, but the need for testing at present price points has created some challenges. For example, in a clinical commercial lab, list prices for sequencing a single SCID related gene are as much as $2000, while a panel of several genes associated with SCID is $4000. Therefore, if more than two genes are considered to be diagnostic possibilities, it would cost less to order the panel. Similarly, if the presentation is broad enough that multiple genes or gene panels might be considered, the cost of whole exome (WES) testing as a trio test with parental comparisons can become the most cost-effective strategy despite list prices approaching $10,000 or more. When compared to whole genome sequencing (WGS), WES is less expensive with faster results because of the greater simplicity of analysis (both from the challenges of the sheer amount of raw data in WGS in addition to our limited understanding of the range of normal and the full range of possible deleterious variations in non-exonic DNA included in WGS).
The second challenge, accessibility, is affected by many aspects of the health care system. While genetic testing has become more broadly commercially available and accepted for diagnosis of disease, insurance companies have restricted what will be a covered benefit for their customers, leaving patients to shoulder a significant portion of the bill, or to forgo testing that can significantly impact on prognosis and therapy choices [3]. Although some commercial clinical genetic labs will work with a given insurance plan and ensure that lower costs are passed on to a patient, not all insurers engage in such a process and, therefore, there is not uniform access to genetic testing for patients, particularly those with limited financial resources. This financial burden creates disparity in the ability to prescribe targeted therapy for patients with PID. Outside of the USA, costs of WES and WGS can be prohibitive, and collaborative efforts to make these forms of advanced testing available are essential for their application to optimize patient care. In addition, some institutions will restrict the ability of the clinical immunologist to directly order genetic testing, requiring a formal consultation with a clinical geneticist. Waiting for this second consultation can contribute to delays in diagnosis. It is essential to determine the appropriateness of genetic testing for each patient based on the clinical phenotype and context, age, cost, and other clinical and non-clinical factors that would ideally represent a personalized medicine approach. The clinical immunologist is most qualified to evaluate the need for genetic testing and, therefore, should make the decisions on testing.
The third challenge inherent to some forms of genetic testing is the challenge of interpreting the results, particularly in the case of next generation sequencing (NGS) including WES or WGS approaches to testing. NGS involves sequencing many short DNA fragments and using algorithms to put them together to determine the overall sequence. Interpretation of genetic test results requires correlation between a positive finding and the clinical disease phenotype. Finding a change in a specific gene or chromosome does not always translate into a disease or a specific diagnosis and not all changes will have the same effect. For example, the differences between loss of function and gain of function STAT3 mutations have become strikingly clear. Generally, changes in DNA sequence are referred to as “variants,” which highlights the large number of variants in each individual, the vast fraction of which do not cause disease or harm to the individual. With the use of WES in clinical immunology, beyond identifying known clinically relevant pathologic variants, WES may also be useful to foster novel gene discovery as well as increasing depth of understanding of a given gene, i.e., identifying new variants in previously implicated genes associated with a clinical phenotype or identifying new genetic defects that cause a given clinical phenotype. However, with novel variants, it remains challenging to decipher which variants are disease-causing and proving their association with specific phenotypic patterns. With a novel mutation in a gene, it is possible that a given mutation can cause gain-of-function or loss-of-function (or even have no effect on clinical presentation), so simply identifying a known target gene, but finding a novel variant, may not be informative without additional investigation.
In an effort to understand the perspective and challenges faced by practicing immunologists surrounding genetic testing, the membership of the CIS was surveyed in 2016. Members reported that the most common clinical testing denied by insurers was genetic testing and the top 3 clinical scenarios leading to a recommendation for genetic testing were clinical primary immunodeficiency of unclear etiology, severe combined immunodeficiency (SCID), and antibody disorders. There was not a perceived difference in rates of denial across different types of testing, including chromosomal microarray, single gene Sanger sequencing, gene panels by Sanger sequencing, gene panels by NGS and whole exome sequencing. Finally, when asked about factors that are perceived barriers to genetic testing, including time needed to explain the test, out of pocket costs to patients, provider comfort with interpretation of results, and availability of genetic counselors, CIS members frequently indicated that out of pocket costs to patients were a barrier always or most of the time.
Genetic Testing Types
Chromosomal Microarray
Chromosomal microarray analysis (CMA), also known as array comparative genomic hybridization (aCGH), is one of the most frequently used microarray technologies in clinical genetic laboratories. CMA detects chromosomal losses and gains (copy number variants, CNV) throughout the genome [4] through relative quantification of the amount of DNA in a given region by comparing hybridization intensities between a patient’s DNA and a normal control’s DNA [5]. Most current CMAs utilize oligonucleotide platforms and can identify gene deletions and duplications of approximately 200 kb or 200,000 nucleotides. This provides greater analytical sensitivity than conventional cytogenetics such as karyotyping. CMA allows the detection of copy number variations (CNVs), microdeletions, microduplications and most unbalanced rearrangements of chromosome structure (translocations, etc.) [6, 7]. Depending on the technique used or “platform,” CMA may also detect excessive homozygosity (loss of heterozygosity, LOH), suggestive of consanguinity, with increased risk for recessive disease or imprinting disorders, triploidy and other duplications of entire chromosome(s). An additional advantage of CMA is that it enables the detection of losses and/or gains of chromosomal material that are submicroscopic, and because CMA analyzes DNA extracted from uncultured cells from many different sources, it is both easier to obtain samples and most often has a shorter reporting time compared to chromosomal analysis [5]. CMA does NOT detect small changes in the sequence of single genes (e.g., point mutations), very small duplications and deletions of DNA segments within a single gene, or balanced chromosomal rearrangements (either translocations or inversions) [8]. It also does not detect intermediate CNVs of one to few exons, which requires a high-resolution CMA that is not as frequently used clinically. CMA is most useful as an initial genetic test when the clinical phenotype is too non-specific to identify a single causal gene or a narrow gene panel [9]. CMA can also inform the analysis/filtering of WES/WGS data because of its ability to detect areas of excessive homozygosity and insertions and deletions which may yield insight into mutations identified on a single chromosome (when phenotypes are associated with homozygous mutations) or patients with deletions that include genes of interest (which would be missed by WES). Note that SNP arrays, which are the gold standard for CMA, are very useful as an adjunct to a WES to ensure that CNV are not contributing to a clinical phenotype; the two tests complement each other in their strengths and weaknesses.
Microarray technology in immunodeficiency has been used to study gene expression in patients with known defects to better understand the basic biology of the affected pathways, and to expand understanding of the pathophysiology of the disease [10]. CMA is commonly used in the diagnosis of 22q11 microdeletion syndrome (DiGeorge Syndrome). In addition, CNV analysis has been performed in CVID to understand the genetic etiology of this heterogeneous immunological disorder [11, 12]. A new immunodeficiency associated with hyperdiploidy of the IL25 gene locus [13] has been reported, highlighting another example of the value of CNV analysis in understanding the pathogenesis of PID. CNVs have also been reported in some of the complement genes as well as other genes associated with PIDs and autoimmunity [14].
Single Gene Sanger Sequencing
Sanger sequencing is considered the 1st generation and gold standard of genetic sequencing dating back to 1977 [15]. In this technique, single-stranded DNA is replicated in vitro with labeled deoxynucleoside triphosphates (dNTPs) that terminate DNA strand elongation and these varied length strands can be used to “read” off the DNA sequence by concatenating the last (labeled) base from the longest to the shortest strands. Although it is expensive, laborious and time consuming, it is a highly accurate form of genetic sequencing. It is able to detect not just point mutations in a coding sequence, but also intronic mutations, and some deletions and duplications. However, some deletions may be missed and, depending on the complexity of the gene and the primers used, some intronic regions may also not be detected. In primary immunodeficiency, single gene Sanger sequencing is a reliable method for diagnosis when there is one clear gene that is most likely causative. For example, sequencing of BTK in a male patient with lack of immunoglobulin production and B cells but otherwise normal immunologic studies. Single gene Sanger sequencing is also a reliable and cost effective method for assessing family members of an affected patient for known mutations in monogenic forms of PID. Finally, it is a necessary part of the clinical laboratory pipeline for technical confirmation of variants detected using WES.
Gene Panels by Sanger Sequencing vs. Next Generation
In the setting of clinical syndromes and phenotypes that are well characterized and have a high likelihood of belonging to a subset of known genetic mutations (or known genes with many possible mutations), gene panels can be a useful strategy. Depending on the gene(s) suspected and the clinical laboratory, there are panels available utilizing Sanger sequencing and some that use NGS. There are positives and negatives to each method.
Gene panels performed using Sanger sequencing technique have higher sensitivity and specificity versus NGS testing, but may miss mosaicism (a rare situation wherein patients may have mutations only in certain tissues or a subset of progenitor cells; as seen in the skin in Incontinentia Pigmenti). In addition, it can be challenging to detect large deletions, duplications or inversions with Sanger sequencing. It is also not possible to assess whether multiple variants within a single gene are from the same parent or not if parental comparison samples are not sequenced in tandem. In addition, beyond the technical limitations and benefits, Sanger sequencing can be more expensive and more time consuming than NGS panels. NGS is similar to Sanger sequencing in that it sequences DNA fragments, but in NGS the process is massively parallel, allowing millions of fragments to be sequenced in a single run. Thus, NGS provides more expedient testing, though for now may be less sensitive than Sanger sequencing.
The utility of gene panels is inherently limited no matter the underlying technique used due to the focus only on the list of included genes versus whole exome or whole genome studies which are not restricted to a set list of target genes. This is a limitation because we do not yet have a complete understanding, in PID, of all the genes that can yield a given phenotype and, as our understanding of PID rapidly evolves, it is challenging for panels to be updated quickly enough to keep pace. In addition, with many gene panels, we may not be able to easily detect splice site or regulatory mutations in known genes due to the technical details of the procedure. Currently, most gene panels are faster and cheaper than WES/WGS but the exact cost threshold will shift over time as NGS WES/WGS strategies continue to become less expensive.
In a newborn diagnosed with SCID following a positive newborn screen in whom multiple possible genes could underlie the diagnosis and a fairly rapid result is desired, gene panels are a reasonable initial approach to testing. In addition to commercially available panels for SCID, there are also several commercially available and clinically reliable panels for hemophagocytic lymphohistiocytosis (HLH), chronic granulomatous disease (CGD), antibody deficiency, hyper IgE syndromes, or other common PID disorders with monogenic etiologies.
Whole Exome Sequencing
WES examines the approximately 1% of the human genome that is responsible for synthesized proteins that make up the human body (i.e., the exons). Exomes are sequenced using oligonucleotide probes (“baits”) that bind to the exome and are then captured for sequencing. NGS techniques are used to sequence the set of fragments and the resulting short “reads” are aligned to the whole exome using complex computer algorithms. Ideally, WES is performed as a TRIO, with submission of samples from the proband and both biologic parents to allow determination of maternal or paternal inheritance. This also allows the analysis team to leverage the known inheritance pattern (i.e., is the phenotype shared with a parent, or known to travel in the family) to include or exclude variants shared with a parent as appropriate (i.e., with an affected child of an affected parent, only shared variants would be likely to be informative). WES, as a non-biased genetic testing approach, allows detection of non-traditional phenotypes of known genetic mutations or novel genetic mutations. Variants detected via WES should be confirmed with Sanger sequencing. The detection and confirmation of variants of unknown significance can represent a particularly fraught situation, where functional studies of the variant to determine its true likelihood of being associated with the expressed phenotype can be challenging in some circumstances, but every effort should be made use currently available functional studies paired with the knowledge of the expected impact on protein function to determine if variants are in fact pathologic or benign.
Note that if a single mutation is identified in a gene that causes a similar phenotype to that exhibited in the proband when homozygous recessive mutations are present, the proband may or may not have a normal second copy of the gene. In this case, deletion/duplication Sanger sequencing of the gene of interest is particularly important to complete the evaluation because large deletions and duplications are not optimally detected in WES. If the second copy of the gene of interest is deleted, the patient would effectively be homozygous for the recessive variant identified on WES. Additionally, in the era when the use of WES is rapidly increasing, it is important to note that there can be false-positives for copy-number variation (CNV) detection from WES [16]. Depending on the platform, WES may not accurately detect large insertions and deletions, large CNV and structural chromosome rearrangements due to the short sequence read lengths fundamental to the methodology, though new open-access bioinformatics tools are emerging for CNV analysis from WES data [17, 18]. The paired use of a SNP array so that larger deletions/duplications are not missed, to allow copy-number variant evaluation can overcome some of the limitations of the WES [19]. Specifically, a SNP array is useful as an adjunct to a WES to ensure that CNV is not contributing to a clinical phenotype; the two tests complement each other [2, 16].
It is important to note that WES will also assess unrelated genes, which allows for discovery of novel immune phenotype associated genes, but will also reveal mutations in non-related pathways (i.e., genes associated with increased risk of malignancy or cardiovascular disease), with resulting ethical and medical issues that attend the reporting of unanticipated genetic findings.
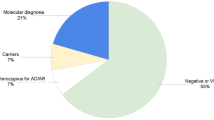
As reported recently, ~ 25% of the known monogenic causes of primary immunodeficiency were identified in individual patients, rather than large families [20]. By only focusing on the genes already known to be associated with primary immunodeficiency in patients with complex phenotypes, the possibility of discovering novel diseases is lost. In addition, many gene panels may not be able to easily detect splice site or regulatory mutations in known genes (panels vary widely by vendor and it is difficult for vendors to keep their panels up to date with the literature). Neither of these problems are an issue with WES. In the first study of 250 consecutive WES, 21% of patients had an underlying genetic defect identified, both in conditions with stable, classic phenotypes and those with variable, less predictable phenotypes [21]. In a recent report taking an unbiased approach to a large cohort of PID patients, the diagnostic rate using WES approached 40%, with some further increase given by pairing WES with tandem CMA [2].
While we may broaden the phenotypes of the known genetic causes of PID and discover novel monogenic causes of PID, there is also the potential for overlap scenarios, in which patients have complex, non-specific phenotypes due to multiple contributing genes. In fact, in 6% of patients with a genetic etiology identified in Yang et al., multiple variants were thought to be causative. The same was recently identified to be the case in PID [2].
Whole Genome Testing
The benefits of whole genome testing, vs. WES, rest on the assessment of the entire genome, rather than the limited subset portion of the genome captured in exome sequencing. Specifically, WGS evaluates the majority of the 99% of non-exonic content missed by WES. Since the exon “baits” used to identify the exons for WES are based on prior knowledge, they are limited to what is known and can miss novel exons or poorly understood regions and thus not completely cover even the exome [22]. In addition, with WGS, it is possible to more confidently assess for non-coding variants (i.e., intronic mutations, splice site mutations, and other regulatory, non-exonic mutations) as well as deletions and duplications that can be missed in WES testing.
Theoretically, this additional data has the potential to yield novel diagnoses for families and patients with primary immunodeficiency.
Currently, WGS is not widely used clinically. The limitations are the increase in cost (though this is decreasing rapidly) and analysis complexity and time, as well as data storage needs. In addition, while we are continually expanding our knowledge of the genetics of human disease, our understanding of the implications of variations in non-exonic DNA remain limited, so projected benefits to diagnosis may be delayed by our scientific understanding. However, large studies are already being done for example, in CVID [23] and families in whom a specific PID had not been previously diagnosable [24]. With further technological and scientific progress, this seems likely to be the future of genetic analysis of immunodeficiency. While the fact that approximately one quarter of patients with clear phenotypes are found to have matching genetic variants on WES seems to indicate that WGS would at least increase that hit rate, there are, as of yet, no prospective studies of cohorts or examinations of patients with negative or inconclusive WES who were subsequently studied by WGS.
Use of Genetic Testing in Primary Immunodeficiency
Prenatal Diagnosis
Genetic testing can be used for both pre-implantation and post-conception testing of known mutations or genetic abnormalities in families with a history of a genetically defined immunodeficiency [25, 26]. For example, in a family with SCID due to IL2RG, genetic sequencing can be performed [25] on embryos prior to implantation with use of in vitro fertilization, or via chorionic villus sampling (CVS) or amniocentesis for established pregnancies. Similarly, in a parent known to have deletion of 22q11.2 CMA could be performed from a fetal or embryonic sample or more recently, via a maternal blood sample using cell free fetal DNA technology [27]. Knowledge of the immunodeficiency, either via pre-implantation diagnosis or with post-conception prenatal testing prior to birth, can be used to guide prognostic counseling for the family and can lead to more effective use of preventative measures including plans for specific treatments post-delivery to reduce the risk of infant morbidity and mortality [26, 28]. Prenatal genetic testing is of uncertain, if any, value for families that have experienced primary immunodeficiency without a known molecular diagnosis, such as CVID without a known genetic abnormality.
Prognostic Indicator
Identification of a specific mutation that explains the patient’s phenotype can aid in the prediction of the clinical course. Examples of PIDs in which this genotype/phenotype correlation exists include chronic granulomatous disease (CGD) [29, 30] and Wiskott-Aldrich Syndrome (WAS) [31]. WAS is an example of a primary immunodeficiency with variable clinical phenotypes that warrant very different management plans. For example, identification of a nonsense mutation leading to absence of protein expression predicts a severe clinical course with significant risk of the development of autoimmunity and malignancy. Conversely, when a patient’s mutation is known to allow for production of small amounts of WASp, these individuals are more likely to have the X-linked thrombocytopenia (XLT) phenotype rather than the severe phenotype associated with the WAS, and their treatment regimens are different [31, 32]. While clinical scoring systems have been developed to assist in making distinctions between XLT and WAS, the use of these prior to age 2 may incorrectly predict a milder clinical course [31]. Therefore, genetic testing could lead to improved treatment paradigms. However, it is important to keep in mind that early genotyping in isolation may not allow an accurate prediction of natural history and prognosis. Therefore, the proper place and application of genetic testing is likely to evolve over time.
Similarly, CGD patient prognosis is impacted by the nature of the mutation. CGD is primarily diagnosed by recognition that a patient’s clinical phenotype suggests the disease combined with screening laboratory testing that demonstrates an inability of phagocytes to undergo a respiratory burst to form reactive oxygen species. Evaluation cannot stop there, since it is impossible to definitively distinguish between the X-Linked and autosomal recessive forms of the disease based on functional flow-cytometric assays that are widely available as screening tools (though some laboratories do have protein level flow assays for the components of the NADPH oxidase). Among the forms of CGD, X-CGD tends to be associated with lower residual oxidative capacity and therefore has a clinical course that is more severe than the course of AR-CGD genotypes, with significant differences in age at diagnosis and mean survival age [29, 33]. There is also recent data on the importance of identifying and following carrier sisters and mothers, given the demonstrated impact on their health [34].
In addition to the potential for differing prognosis based on the specific mutation associated with a given immunodeficiency as described above, definitive diagnosis via genetic testing for patients with an atypical presentation of other immunodeficiencies can allow clinicians to better counsel patients on the expected disease course, avoid further unnecessary diagnostic testing, and direct therapy. For example, we now know that in some patients with combined immunodeficiency, previously managed as more severe common variable immunodeficiency patients, mutations in genes known to be associated with SCID are the underlying reason for their symptoms ([35, 36] new references). Over the last 10 years, a broadening spectrum of the phenotypes associated with these and other molecularly immunodeficiencies has been described. Some patients may benefit in terms of quality of life from the knowledge of the cause of their symptoms. Conversely, others may feel that having a genetic diagnosis is undesirable for personal or professional reasons, which should be discussed in the process of counseling and obtaining informed consent for genetic testing.
Treatment Implications
Genetic testing for primary immunodeficiency by the methods described previously is fully in line with the AAAAI practice parameter for the diagnosis and management of PID immunodeficiency [37] because we expect that determining the molecular cause of the disease will often impact management. In fact, we expect this link to become increasingly common as more molecular mechanisms are discovered leading to targeted therapeutic development. Genetic testing is also an essential part of diagnosing conditions with immune dysregulation and should be considered a medically necessary part of the comprehensive evaluation for overlap disorders of immune dysfunction including inflammasome disorders, lymphoproliferative disease, and disordered immunity with significant autoimmunity as the presenting feature. Also, disorders due to gain of function (GOF) mutations, such as autosomal dominant GOF in STAT1 or STAT3, are best diagnosed using genetic testing. The presenting phenotypes are not always sufficiently definitive to allow for targeted gene testing. It is important to note again here that it may be most cost and time efficient to consider WES if the need to study multiple panels or single genes is anticipated.
With the advent of population based genetic testing of TRECs as a newborn screen for SCID, affected infants are increasingly diagnosed prior to development of infectious complications or a family history. Genetic testing is necessary to be able to differentiate the cause of the near absence of T cells in these patients because of the importance of genotype in determining therapeutic approach. While many will have true SCID, also high on the differential diagnosis list are disorders associated with thymic agenesis, which are not amenable to hematopoietic cell transplantation (HCT). In contrast, HCT has been the mainstay of therapy for SCID for decades. The differences in outcomes make it crucial to understand the underlying cause of the absence of T cells. In addition, there are clear differences in late effects of HCT of SCID including survival, durability of T cell immune reconstitution and B cell function that are impacted by genotype [38,39,40].
Patients with SCID due to recombinase activating gene defects (RAG1/2) and adenosine deaminase defects (ADA) have been shown to have poorer T cell reconstitution after HCT [41], but patients with defects in the common gamma chain of IL2R, or Jak3 usually have engraftment of T cells with poor engraftment of B cells in the absence of pre-transplant conditioning [38]. SCID due to mutations in CD3ƺ or IL7 receptor α chain are more likely to have functioning B cells despite a lack of donor chimerism and are more likely to be able to discontinue immunoglobulin supplementation after transplant even without conditioning [38, 39]. SCID caused by mutations associated with radiosensitivity include DCLREIC (Artemis), PRKDC, Lig4 (Ligase4), NHEJI (Cernnunos), and NBS1 (Nijmegen breakage syndrome) [42]. Among this group, those with defects in LIG4, NHEJI, and NBS1 have an increase in early mortality associated with myeloablative conditioning prior to transplant [42]. Patients with Artemis SCID are more likely to have growth failure and other late toxicities with exposure to alkylator based conditioning regimens. In comparison, RAG gene defects do not appear to increase susceptibility to DNA damage after exposure to alkylating agents (such as Busulfan) and ionizing radiation. Thus, pre-transplant conditioning regimens as well as donor selection may be affected by the distinction between these genotypes. Enzyme replacement therapy is uniquely available as a bridge to definitive therapy for ADA SCID. Finally, gene therapy is in clinical trials for ADA SCID and IL2RG forms of SCID and is under development for other SCID genotypes, which lends further support for the routine use of genetic testing prior to HCT in SCID, because the safety and effectiveness of HCT, and of different conditioning and treatment regimens may be drastically changed by knowledge of the genetic etiology of the disease [43].
In addition to SCID, many other primary immune deficiencies may be treated with HCT. Although it is desirable to have a genetic diagnosis prior to transplant, supportive treatment is usually initiated prior to transplant based on characteristic immunologic functional abnormalities. In some cases, such as CTLA-4 haploinsufficiency or STAT3-GOF mutations, knowing the underlying genetic diagnosis can also help to guide choice of highly specific biologic supportive therapy (i.e., in CVID, abatacept for LRBA [44] or rapamycin for CTLA-4 haploinsufficiency [45]. In addition, diagnosis of genetic defects such as deficiency in IL1R antagonist (DIRA) have led to significant improvements in therapy using targeted therapy with the recombinant IL1R antagonist, anakinra [46].
Most primary immune deficiencies are caused by single gene mutations and are lifelong disorders requiring uninterrupted therapy. In these cases, delaying or interrupting the therapy pending the completion of genetic testing constitutes an unreasonable risk to the welfare of the patient. An example of this scenario is XLA. XLA, caused by mutations in Bruton’s tyrosine kinase, results in a complete absence of B cells and affected patients have a lifelong defect in producing immunoglobulins and antibodies. They are susceptible to overwhelming bacterial and certain viral infections. IgG replacement is efficacious in treating this immune deficiency and must be continued throughout life since there is no possibility of spontaneous improvement in B cell production in these patients. The absence of B cells and the inability to make antibodies plus the absence of the BTK protein on flow cytometry in a male patient is diagnostic. Thus, in this disease, a requirement for genetic testing to demonstrate the need for gamma globulin therapy is an unnecessary burden and can delay needed therapy. However, other genetic forms of agammaglobulinemia can present similarly, and there is, therefore, a role for genetic testing to allow for appropriate genetic counseling of the affected patient and family members. Many other PID, such as CGD and WAS, require lifelong therapy and are diagnosed by non-genetic tests. Delaying or interrupting therapy to require completion of genetic testing is not an absolute requirement for making the diagnosis, nor selecting the appropriate therapy.
Family Planning
The benefit of a molecular diagnosis extends far beyond the affected individual. The obvious benefit of accurate genetic testing is that it allows for the prediction of a clinical course and selection of a treatment modality for a unique patient. It also facilitates carrier detection and allows for genetic counseling. In those diseases with both X linked and AR forms (such as CGD), distinguishing between the two forms can have implications for relatives of the patient who may be carriers. In X-linked CGD, carriers exhibit a characteristic set of signs and symptoms [34] and can be at risk for development of CGD symptoms if there is skewed lyonization. However, in the AR forms, carriers have completely normal phagocyte function; therefore, functional assays are also normal. Knowing carrier status and understanding the risks with future pregnancies can allow for family planning decisions that may greatly reduce the risk of having affected children and therefore may reduce healthcare costs.
Concluding Recommendations
In conclusion, the Clinical Immunology Society puts forth the following summary statements and consensus based recommendations to guide the use of genetic testing for the evaluation and care of primary immunodeficiency patients by the practicing clinical immunologist.
-
1.
The Clinical Immunology Society supports the use of genetic testing by clinical immunologists to provide state of the art diagnosis and precision treatment to primary immunodeficiency patients. Practicing clinical immunologists have the necessary clinical knowledge to counsel patients regarding the use of genetic testing in the course of an evaluation for primary immunodeficiency and to determine which genes should be considered as well as the scope of testing needed to potentially determine a conclusive diagnosis. The membership of the CIS has identified genetic testing as particularly desirable for, but not limited to use in, patients with poorly defined primary immunodeficiency (including immune dysregulation), severe combined immunodeficiency and humoral immunodeficiency.
-
2.
Genetic testing provides the ability to make a definitive diagnosis, defines and assesses the influence of genotype-phenotype associations on prognosis, identifies patients for gene specific therapy, and informs family planning decisions. There are multiple benefits for patients who are able to have their primary immunodeficiency molecularly defined, including the ability to have a comparison population for prognosis and to allow consideration of personalized and targeted therapy, including gene therapy. Once a proband is diagnosed, testing should also be offered to family members who may also be affected, as well as potential carriers of primary immunodeficiency genetic abnormalities to inform their family planning process as well as those carriers who have potential risk for disease (e.g., CGD).
-
3.
Genetic counseling should be provided before and after genetic testing with an immunologist or genetic counselor with expertise in primary immunodeficiency. Clinical immunologists who order genetic testing for patients should be prepared to discuss (or refer the patient to a genetic counselor for discussion of) the test results, the consequences and nature of the disease, the probability of developing additional symptoms or transmitting the disease, and the options open to them in management and family planning.
-
4.
The choice of which genetic test to use for a given patient should be made by the clinical immunologist based on the patient’s clinical history and other functional results. Genetic tests should be ordered based on the initial presenting clinical history and initial functional studies that raise concern for primary immunodeficiency. The initial choice to start genetic testing should be discussed with the patient with an understanding that no single study is an appropriate first test in all cases, and that secondary testing such as CMA followed by gene panel or WES may be necessary.
-
5.
The use and application of individual Sanger tests, gene panels, and genomic approaches has different and rapidly changing costs and turn-around-times. The choice of one vs. another test needs to be based upon the greatest likelihood of obtaining the diagnosis within a clinically acceptable timeframe with the most judicious use of financial resources. Since the technical, cost, and completion time variables are changing so rapidly, it is not appropriate to put forward a specific algorithm or paradigm. These variables should be considered on a case-by-case basis within the patient’s clinical context. When, potentially, mutations in a large number of genes could be involved, a gene panel or whole genomic approach may be more cost effective and timely than single gene analysis.
-
6.
In patients where initial genetic testing is not conclusive, follow up testing may be needed to determine a conclusive diagnosis. In patients where there is significant concern for primary immunodeficiency, genetic testing may need to be performed using a tiered approach or combination of genetic testing methods. In addition, the finding of variants (including a single pathologic variant or variants of undetermined significance) may require follow up functional studies to demonstrate the association of the implicated gene with the expressed phenotype or to confirm that there are two mutations present in the case of diseases associated with autosomal recessive inheritance.
-
7.
Genetic testing should not be a pre-requisite confirmatory test to initiate supportive therapy such as immunoglobulin replacement in patients in whom clinical testing demonstrates a need for the therapy. In primary immunodeficiencies where functional testing demonstrates a conclusive need for supportive therapy such as immunoglobulin replacement or antibiotic prophylaxis, such therapies should not be withheld while genetic testing results are pending. Similarly, in patients with a genetically defined primary immunodeficiency requiring supportive therapy, the therapy should be continued lifelong without interruptions to reassess immune function or demonstrate continued need for the therapy.
Change history
21 May 2018
The original version of this article unfortunately contained mistakes in some of the author names and affiliations. The correct list of author names and affiliations is below, with the corrections in bold.
References
Vetrie D, Vorechobsky I, Sideras P, Holland J, Davies A, Flinter F, et al. The gene involved in X-linked agammaglobulinemia is a member of the src family of protein-tyrosine kinases. Nature. 1993;361:226–33.
Stray-Pedersen A, Sorte HS, Samarakoon P, Gambin T, Chinn IK, Coban Akdemir ZH, et al. Primary immunodeficiency diseases: genomic approaches delineate heterogeneous Mendelian disorders. J Allergy Clin Immunol. 2017;139:232–45.
Zielinski SL. As genetic tests move into the mainstream, challenges await for doctors and patients. JNCI J Natl Cancer Inst. 2005;97(5):334–6. https://doi.org/10.1093/jnci/97.5.334.
Zarrei M, MacDonald JR, Merico D, Scherer SW. A copy number variation map of the human genome. Nat Rev Genet. 2015;16:172–83.
Bi W, Borgan C, Pursley AN, Hixson P, Shaw CA, Bacino CA, et al. Comparison of chromosome analysis and chromosomal microarray analysis: what is the value of chromosome analysis in today’s genomic array era? Genet Med. 2013;15:450–7.
Kang SH, Shaw C, Ou Z, Eng PA, Cooper ML, Pursley AN, et al. Insertional translocation detected using FISH confirmation of array-comparative genomic hybridization (aCGH) results. Am J Med Genet A. 2010;152A:1111–26.
Neill NJ, Ballif BC, Lamb AN, Parikh S, Ravnan JB, Schultz RA, et al. Recurrence, submicroscopic complexity, and potential clinical relevance of copy gains detected by array CGH that are shown to be unbalanced insertions by FISH. Genome Res. 2011;21:535–44.
Manning M, Hudgins L, Practice Professional, and Committee Guidelines. Array-based technology and recommendations for utilization in medical genetics practice for detection of chromosomal abnormalities. Genet Med. 2010;12:742–5.
Miller DT, Adam MP, Aradhya S, Biesecker LG, Brothman AR, Carter NP, et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet. 2010;86:749–64.
Qin H, Yamada M, Tian L, Stewart DM, Gulino AV, Nelson DL. Tracking gene expression in primary immunodeficiencies. Curr Opin Allergy Clin Immunol. 2003;3:437–42.
Keller M, Glessner J, Resnick E, Perez E, Chapel H, Lucas M, et al. Burden of copy number variation in common variable immunodeficiency. Clin Exp Immunol. 2014;177:269–71.
Orange JS, Glessner JT, Resnick E, Sullivan KE, Lucas M, Ferry B, et al. Genome-wide association identifies diverse causes of common variable immunodeficiency. J Allergy Clin Immunol. 2011;127:1360–7. e6
Green MR, Camilleri E, Gandhi MK, Peake J, Griffiths LR. A novel immunodeficiency disorder characterized by genetic amplification of interleukin 25. Genes Immun. 2011;12:663–6.
Olsson LM, Nerstedt A, Lindqvist AK, Johansson SC, Medstrand P, Olofsson P, et al. Copy number variation of the gene NCF1 is associated with rheumatoid arthritis. Antioxid Redox Signal. 2012;16:71–8.
Sanger F, Nicklen S, Coulsen AR. DNA sequencing with chain terminating inhibitors. PNAS. 1977;74(2):5463–7.
Retterer K, Scuffins J, Schmidt D, Lewis R, Pineda-Alvarez D, Stafford A, et al. Assessing copy number from exome sequencing and exome array CGH based on CNV spectrum in a large clinical cohort. Genet Med. 2015;17:623–9.
Fromer M, Purcell SM. Using XHMM software to detect copy number variation in whole-exome sequencing data. Curr Protoc Hum Genet. 2014;81:7.23.1–21.
Magi A, Tattini L, Cifola I, D'Aurizio R, Benelli M, Mangano E, et al. EXCAVATOR: detecting copy number variants from whole-exome sequencing data. Genome Biol. 2013;14:R120.
Cirulli ET, Goldstein DB. Uncovering the roles of rare variants in common disease through whole-genome sequencing. Nat Rev Genet. 2010;11(6):415–25.
Casanova JL, Conley ME, Seligman SJ, Abel L, Notarangelo LD. Guidelines for genetic studies in single patients: lessons from primary immunodeficiencies. J Exp Med. 2014;211(11):2137–49.
Yang Y, Muzny DM, Reid JG, Bainbridge MN, Willis A, Ward PA, et al. Clinical whole-exome sequencing for the diagnosis of mendelian disorders. N Engl J Med. 2013;369(16):1502–11.
Chou J, Ohsumi TK, Geha RS. Wuse of wole exome and genome sequencing in the identification of fenetic causes of primary immunodeficiencies. Curr Opin Allergy Clin Immunol. 2012;12:623–6.
Van Schouwenburg PA, Davenport EE, Kienzler AK, et al. Application of whole genome and RNA sequencing to investigate the genomic landscape of common variable immunodeficiency disorders. Clin Immunol. 2015;160:301–14.
Mousallem T, Urban TJ, McSweeney KM, Kleinstein SE, Zhu M, Adeli M, et al. Clinical application of whole-genome sequencing in patients with primary immunodeficiency. J Allergy Clin Immunol. 2015;136(2):476–9.
Puck JM, Middelton L, Pepper AE. Carrier and prenatal diagnosis of X-linked severe combined immunodeficiency: mutation detection methods and utilization. Hum Genet. 1997;99(5):628–33.
Lee WI, Huang JL, Yeh KW, Cheng PJ, Jaing TH, Lin SJ, et al. The effects of prenatal genetic analysis on fetuses born to carrier mothers with primary immunodeficiency diseases. Ann Med. 2016;48(1–2):103–10.
Yaron Y, Jani J, Schmid M, Oepkes D. Current status of testing for microdeletion syndromes and rare autosomal trisomies using cell-free DNA technology. Obstet Gynecol. 2015;126(5):1095–9.
Giliani S, Fiorini M, Mella P, Candotti F, Schumacher RF, Wengler GS, et al. Prenatal molecular diagnosis of Wiskott-Aldrich syndrome by direct mutation analysis. Prenat Diagn. 1999;19(1):36–40.
Winkelstein JA, Marino MC, Johnston RB Jr, Boyle J, Curnutte J, Gallin JI, et al. Chronic granulomatous disease. Report on a national registry of 368 patients. Medicine. 2000;79:155–69.
Kuhns DB, Alvord WG, Heller T, Feld JJ, Pike KM, Marciano BE, et al. Residual NADPH oxidase and survival in chronic granulomatous disease. N Engl J Med. 2010;363(27):2600–10.
Jin Y, Mazz C, Christie JR, et al. Mutations of the Wiskott-Aldrich Syndrome Protein (WASP): hotspots, effect on transcription, and translation and phenotype/genotype correlation. Blood. 2004;104(13):4010–9.
Bryant N, Watts T. Thrombocytopenic syndromes masquerading as childhood immune thrombocytopenic purpura. Clin Pediatr. 2011;50(3):225–30.
Van den Berg JM, van Koppen E, Ahlin A, et al. Chronic granulomatous disease: the European experience. PLoS One. 2009;4:e5234.
Cale CM, Morton L, Goldblatt D. Cutaneous and other lupus-like symptoms in carriers of x-linked CGD: incidence and autoimmune serology. Clin Exp Immunol. 2007;148(1):79–84.
Volk T, Pannicke U, Reisli I, Bulashevska A, Ritter J, Björkman A, et al. DCLRE1C (ARTEMIS) mutations causing phenotypes ranging from atypical severe combined immunodeficiency to mere antibody deficiency. Hum Mol Genet. 2015;24(25):7361–72.
Avila EM, Uzel G, Hsu A, Milner JD, Turner ML, Pittaluga S, et al. Highly variable clinical phenotypes of hypomorphic RAG1 mutations. Pediatrics. 2010;126(5):e1248–52. https://doi.org/10.1542/peds.2009-3171.
Bonilla FA, Khan DA, Ballas ZK, Chinen J, Frank MM, Hsu JT, et al. Practice parameter for the diagnosis and management of primary immunodeficiency. J Allergy Clin Immunol. 2015;136:1186–205.
Buckley RH, Win CM, Moser BK, Parrott RE, Sajaroff E, Sarzotti Kelsoe M. Post-transplantation B cell function in different molecular types of SCID. J Clin Immunol. 2013;33:96–110.
Haddad E, Leroy S, Buckley RH. B-cell reconstitution for SCID: should a conditioning regimen be used in SCID treatment? JACI. 2013;131:994–1000.
Heimall J, Puck J, Buckley R, Fleisher TA, Gennery AR, Neven B, et al. Current knowledge and priorities for future research in late effects after hematopoietic stem cell transplantation (HCT) for severe combined immunodeficiency patients: a consensus statement from the second pediatric blood and marrow transplant consortium international conference on late effects after pediatric HCT. Biol Blood Marrow Transplant. 2017;23(3):379–87.
Sarzotti-Kelsoe M, Win CM, Parrott RE, Cooney M, Moser BK, Roberts JL. Thymic output, T cell diversity and T-cell function in long term human SCID chimeras. Blood. 2009;114:1445–53.
Cowan MJ, Gennery AC. Radiation-sensitive severe combined immunodeficiency: the argmuents for and against conditioning before hematopoietic cell transplantation – what to do? JACI. 2015;136:1178–85.
Gaspar B. Bone marrow transplantation and alternatives for adenosine deaminase deficiency. Immunol Allergy Clin North Am. 2010;30:221–36.
Lo B, Zhang K, Lu W, et al. Autominnue disease. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science. 2015;6246:436–40.
Kuehn HS, Ouyang W, Lo B, Deenick EK, Niemela JE, Avery DT, et al. Immune dysregulation in human subjects with heterozygous germline mutations in CTLA4. Science. 2014;345:1623–7.
Goldbach-Mansky R, Kastner DL. Autoinflammation: the prominent role of IL-1 in monogenic autoinflammatory disease and implications for common illnesses. JACI. 2009;124:1141–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declared that they have no conflict of interest, except for the following:
Jennifer Heimall, MD: ADMA Consultant; CSL Behring speaker panel
Sarah Henrickson, MD, PhD: Horizon Pharmaceuticals advisory board
Kenneth Paris, MD, MPH: Shire Advisory Board Participant, Speaker, Clinical Trial Investigator; CSL Behring Advisory Board Participant
Troy Torgerson, MD, PhD: Director Seattle Children’s Immunology Diagnostic Lab, Seattle, WA
Jordan Orange, MD, PhD: Shire Consultant, Grifols Consultant
Additional information
Summary Statements
1. The Clinical Immunology Society (CIS) supports the use of genetic testing by clinical immunologists to provide state of the art diagnosis and precision treatment for primary immunodeficiency patients.
2. Genetic testing provides the ability to make a definitive diagnosis, project prognosis based on genotype-phenotype association, utilize available targeted therapy and inform family planning decisions.
3. Genetic counseling should be provided before and after genetic testing with an immunologist or genetic counselor with expertise in primary immunodeficiency.
4. The choice of genetic test for a given patient should be made by the immunologist within the context of the patient’s clinical history and other phenotypic and functional results.
5. The use and application of individual Sanger sequencing tests, gene panels and broader genomic approaches has different and rapidly changing cost and turn-around-time implications.
6. In patients in whom initial genetic testing is not conclusive, follow up testing may be needed to determine a conclusive diagnosis.
7. Genetic testing should not be a pre-requisite confirmatory test to initiate or continue disorder-specific or supportive therapy such as immunoglobulin replacement in patients where the clinical history and routine testing demonstrate a clear need for the therapy.
Rights and permissions
About this article
Cite this article
Heimall, J.R., Hagin, D., Hajjar, J. et al. Use of Genetic Testing for Primary Immunodeficiency Patients. J Clin Immunol 38, 320–329 (2018). https://doi.org/10.1007/s10875-018-0489-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-018-0489-8