Abstract
Objectives
To investigate the immunological phenotypes detected in children with recurrent upper and lower respiratory infections that have normal total immunoglobulin concentrations.
Methods
A cohort of over 60 children with recurrent respiration infections was evaluated for specific antibody deficiencies (SAD) and for memory B-cell abnormalities. A control group of children without recurrent infections was also evaluated. Evaluation included a detailed history of immunizations with pneumococcal vaccines; determination of IgM, IgG, IgA, and IgE concentrations; measurement of anti-pneumococcal polysaccharide antibody levels by ELISA and expression of CD27, IgD, and IgM on peripheral CD19+B cells by flow cytometry to determine the proportions of naive, IgM-memory B cells, and class-switched memory B cells.
Results
Patients were classified as having a SAD to either pure polysaccharides (PPV-SAD) or to conjugate polysaccharides (PCV-SAD) based on the number of polysaccharides to which they developed an adequate antibody response. A normal response to only 2 or fewer of 7 PCV or PPV serotypes was considered as evidence of SAD. Forty-one patients without SAD and 26 with SAD were identified. IgM-memory B cells were low in 3 of 41 patients without SAD; in 3 of 5 PPV-SAD patients; and in 10 of 21 PCV-SAD patients. Class-switched memory B cells were low in 19 of 41 patients without SAD; in all 5 patients with PPV-SAD; and in 11 of 21PCV-SAD patients.
Conclusions
Patients with recurrent infection with or without SAD may have low IgM- and/or class-switched memory B cells. Ongoing research aims to determine the prognostic implications of these differences in patients with SAD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Specific antibody deficiency (SAD) is a common antibody immunodeficiency manifested by recurrent respiratory infections such as sinusitis, otitis, or pneumonia. These manifestations are similar in all immunoglobulin deficiencies. SAD was originally defined based on a poor antibody response to unconjugate pneumococcal polysaccharides (PPV) present in the 23-valent pneumococcal vaccine (PPV23-SAD). We have also defined a specific antibody deficiency that affects only the responses to conjugate pneumococcal polysaccharides (PCV-SAD). In both SAD forms, all immunoglobulin concentrations, including IgG subclasses, are normal. In most patients with either form of SAD, the responses to protein antigens (e.g., tetanus toxoid or diphtheria toxoid) and the conjugate Haemophilus influenzae type b vaccine are also normal (Sorensen RU, unpublished observations).
SAD can be found in association with many primary immunodeficiency diseases (PIDD), including IgG subclass deficiencies, the Wiskott-Aldrich syndrome, partial DiGeorge syndrome, asplenia, hyper-IgE syndrome, and selective IgA deficiency without IgG subclass deficiency [1].
Normal infants have a developmental condition that resembles PPV-SAD. Children in the first year of life are unable to develop a protective response to PPV23-SAD. Antibodies to protein antigens and to some conjugate polysaccharides develop normally in this age group. For PPV-SAD patients who resemble the developmental status of normal infants, it is important to determine if PPV-SAD is just a prolongation of a normal physiologic status of human development or if it points to a different underlying immunological abnormality. Clinically, these two conditions differ, since only SAD patients have frequent infections and require antibiotics for improvement.
Conventional immunologic evaluation does not always detect abnormalities in the antibody-mediated immunity of patients evaluated for recurrent infections. Other PIDD affecting different immunologic functions are much less frequent and usually have a different clinical presentation. Susceptibility of patients to infections may be due to other, as yet undetected, immune abnormalities.
Peripheral blood B cells have been subdivided into 3 subpopulations on the basis of CD27 and IgD expression: IgD+CD27- naive B cells, IgD+CD27+ non-switched memory B cells, and IgD-CD27+ class-switched memory B cells [2, 3]. Another subpopulation, the IgM memory B cell, which is CD27+ IgM+, has been recently identified and proposed to be the splenic marginal zone (MZ) B cell. It has been shown that memory B cells, especially switched memory B cells and IgM memory B cells, are affected in some primary immunodeficiencies, including common variable immunodeficiency (CVID) and X-linked hyper IgM syndrome (X-HIGM). Their reduced percentages in peripheral blood have been associated with clinical complications [2, 4–8].
In this study we explored the presence of the different subtypes of circulating memory B cells in normal children and in children with recurrent infections, with or without SAD. Among children with SAD, we differentiated between patients with PPV-SAD and with PCV-SAD. In each group, there are individuals and patients with what appears to be abnormally low class-switched memory B cells and/or IgM memory B cells.
Our results show general trends in levels of circulating memory B cells in groups of both normal children and patients.
Materials and Methods
Patient Population
We studied a cohort of otherwise normal children with recurrent respiratory infection, requiring antibiotic treatment for improvement, 2 years of age or older of both genders (Table I), referred to the allergy/immunology clinics of Children’s Hospital, New Orleans. Subjects were recruited regardless of race or ethnic background.
Patients were evaluated in the clinic according to a standard protocol, which includes a detailed history of infections, antibiotic use, and a laboratory evaluation that includes immunoglobulin and IgG subclass determinations and the measurement of IgG antibodies specific to 14 pneumococcal polysaccharide serotypes. As part of their evaluation, patients in this study received one dose of a 23-valent pneumococcal vaccine (Pneumovax 23; Merck, Whitehouse Station, NJ, USA) [9]. Anti-pneumococcal polysaccharide antibodies were measured before and 4–6 weeks after immunization. Patients were enrolled into the study at the time of the post-immunization samples, before knowing the outcome of their responses to immunization. Thus, in patients diagnosed with SAD and eventually treated with IgG replacement therapy, all studies were performed on blood samples taken prior to immunoglobulin replacement therapy.
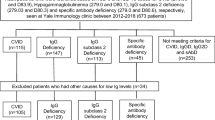
For analysis, subjects were divided into 2 groups: 26 patients with diagnosis of SAD and 41 patients without SAD. Patients with SAD were defined as having normal IgG, IgM, IgA, and IgG subclass levels, but poor IgG antibody responses to pneumococcal vaccines. Patients with immunoglobulin deficiencies, acute infections, or debilitating conditions were excluded from the study. One 10-cc peripheral blood sample, collected in a sodium heparin tube, was obtained 4–6 weeks after pneumococcal immunization, at the time of laboratory re-evaluation of the patient’s immune status. A control group of 43 healthy children recruited at a well-check clinic was included in the study. Consent from each subject’s legally authorized representative was obtained by the attending physician. Assent was obtained from children 7 years of age or older.
Measurement of IgG Anti-Pneumoccocal Antibody Levels by ELISA
IgG antibody level against serotypes 1, 3, 4, 6B, 7F, 9V, 11, 12F, 14, 15, 18C, 19F, 23F, and 33 was performed by a standardized enzyme-linked immunosorbent assay (ELISA) method calibrated against the FDA 89SF reference sample. Serum samples were pre-absorbed with pneumococcal C polysaccharide (CPS) and Ser 22 F [10].
Adequate IgG Antibody Response
For the purposes of establishing the diagnosis of SAD, an adequate IgG antibody response to an individual serotype was arbitrarily defined as a post-immunization antibody concentration of 1.3 μg/mL or greater. An adequate response was defined according to the percentage of serotypes in the vaccine to which the patient responded. Children 2 to 5 years of age were expected to have an adequate response to more than 50 % of the serotypes tested. Patients 6 years or older were expected to respond to more than 70 % of the serotypes tested [11]. A normal response to only 2 or fewer of 7 PCV (4, 6B, 9V, 14, 18C, 19F, 23F) or PPV (1, 3, 7F, 11, 12F, 15, 33) serotypes was considered evidence of PCV-SAD or PPV-SAD, respectively).
Cell Preparation
Peripheral blood mononuclear cells (PBMC) were isolated from blood samples by Ficoll-Hypaque (Histopaque-1077, Sigma, St. Louis, MO, USA) gradient centrifugation. PBMCs were washed, counted, and resuspended in RPMI-1640. PBMC (2 × 106/mL) were used for flow cytometry staining of memory B cells. Some of the blood samples were stained for flow cytometry using a whole blood technique, after performing a correlation testing with the PBMC technique [12].
Flow Cytometry Determination of B-cell Subpopulations
Percentages of B-cell subsets—naive (CD27‾ IgD+), non-switched memory (CD27+ IgD+), switched memory (CD27+IgD‾), and IgM memory (CD27+IgM+) B cells were determined by staining 100 μL of PBMC or whole blood samples for the expression of CD19-PerCPCy5.5, CD27-PE, IgD-FITC, or IgM-FITC and were analyzed using a FACSCanto II Flow Cytometer with the DIVA software (BD Biosciences, San Jose, CA, USA). Analysis was performed by gating on CD19+ B cells.
Statistical Analysis
Statistical analysis was performed using the GraphPad Prism software. Differences between patient groups were analyzed for statistical significance using the Mann–Whitney test. The threshold of significance was set at a P value of <0.05.
Approval for the study was obtained from the Louisiana State University Health Science Center and from the Children’s Hospital Institutional Review Board Offices.
Results
We determined percentages of peripheral blood memory B cell subsets in 43 healthy children (controls) and compared them with those of 67 patients with recurrent respiratory infections. Patients were classified based on the number of polysaccharides to which they developed an arbitrarily defined adequate antibody response. This resulted in 4 groups: 43 healthy children (controls) and 67 patients with recurrent respiratory infections: 41 without SAD (No SAD), 5 patients with PPV-SAD and 21 patients with PCV-SAD. There was no difference in severity of infections among SAD and No SAD patients.
Results in Fig. 1 show that the differences in switched memory B cells between controls and No SAD and controls and PCV-SAD were not significant, while switched memory B cells were reduced in patients with PPV-SAD.
Percentages of switched memory B cells in patients with SAD, without SAD, and controls. Though percentages are similar, switched memory B cells are markedly lower in patients with SAD compared with controls and in patients without SAD. Those sub-classified as PPV SAD showed lower switched memory B cells in comparison with PCV SAD patients. SAD indicates specific antibody deficiency, PPV-SAD, specific antibody deficiency to unconjugate pneumococcal polysaccharides, PCV-SAD, specific antibody deficiency to conjugate pneumococcal polysaccharides
Percentages of IgM memory B cells in patients with SAD were not significantly different from those of healthy donors or patients without SAD (Fig. 2). However, when the patients were sub-classified into PPV- and PCV-SAD, the PPV-SAD patients showed significantly lower percentages of IgM memory B cells.
Percentages of IgM memory B cells in patients with SAD, without SAD, and controls. Percentages were not significantly different from those of healthy donors or patients without SAD. However, when the patients were sub-classified into PPV-SAD and PCV-SAD, the PPV-SAD patients showed significantly lower percentages of IgM memory B cells. SAD indicates specific antibody deficiency, PPV-SAD specific antibody deficiency to unconjugate pneumococcal polysaccharides, PCV-SAD, specific antibody deficiency to conjugate pneumococcal polysaccharides
Discussion
Numerous B cell subsets have been identified in the peripheral blood; these are believed to represent different stages of development of naive B cells into memory B cells. Recent evidence indicates that CD27 is regarded as a memory B cell marker and that the loss of IgM and IgD surface expression is a sign for class switch from IgM to IgG, which identifies the switched memory B cell subset [13]. These cells are known to differentiate in the germinal centers, where they undergo somatic hypermutation and differentiate into plasma cells [3, 14]. More recently, another subset—the IgM memory B cell, identified in peripheral blood by the expression of CD27 and IgM, has been characterized as an important subset present in the marginal zone (MZ) of the spleen. These IgM memory B cells produce natural antibodies and are necessary for the T-independent response against encapsulated bacteria [15, 16].
The differentiation of B cells both from germinal centers (switched memory B cells) and from the recirculating pool of the MZ phenotype (IgM memory B cells) has been proposed to make an important contribution to the repertoire of B cells that respond to polysaccharide antigens [17].
Our results show overall trends in the levels of memory B cells in normal and patient groups, as well as the presence of very low or very high levels in some individuals in each group. Our normal children (controls) show percent ranges of both switched memory and IgM memory B cells, comparable to those in previous studies [4, 18, 19].
Our results show that controls and patients with recurrent respiratory infections without SAD are very similar and lack individual low values, while patients with SAD, as a group, clearly tend to have lower switched memory B cells. The percentages of class-switched memory B cells in these patients are clearly abnormal; the lowest values are found in the PPV-SAD group, reinforcing our observation that PPV-SAD and PCV-SAD are due to differences in activation pathways.
The difference in IgM memory B cells between controls and patients with recurrent infections suggests that the latter can respond to infections by increasing some cells involved in antibody production. Both controls and patients with SAD have lower IgM memory B cells and a significant proportion of very low individual values. Recent reports indicate that IgM memory B cells are absent in cord blood, slowly increase during the first year of life, and continue to increase with age [15]. The presence of very low values in SAD patients in our study now raises the question of whether the low levels in these clinically different groups are due to the same cause. It could be that some SAD patients are unable to respond with increased IgM memory B cells, while normal children may not be as stimulated as are patients with recurrent infections without SAD. The much lower levels of IgM memory B cells in PPV-SAD patients seems to suggest that this group may have a defect in the development pathway for IgM memory B cells.
Thus far, differences in antibody responses to polysaccharide and conjugate polysaccharide vaccines have been attributed to different antigen presentation mechanisms in each case [20, 21]. Our observation in SAD patients suggests that the development of the B-cell response may also play an important role that needs to be explored. In addition to this question, ongoing research in our laboratory aims to determine the prognostic implications of differences in switched and IgM memory B cells in a much larger cohort of controls and patients with SAD.
References
Knutsen AP. Patients with Igg subclass and/or selective antibody deficiency to polysaccharide antigens: initiation of a controlled clinical trial of intravenous immune globulin. J Allergy Clin Immunol. 1989;84(4 Pt 2):640–5. discussion 645–7.
Warnatz K, Denz A, Drager R, Braun M, Groth C, Wolff-Vorbeck G, et al. Severe deficiency of switched memory B cells (CD27(+)IgM(−)IgD(−)) in subgroups of patients with common variable immunodeficiency: a new approach to classify a heterogeneous disease. Blood. 2002;99(5):1544–51.
Sanz I, Wei C, Lee FE, Anolik J. Phenotypic and functional heterogeneity of human memory B cells. Semin Immunol. 2008;20(1):67–82.
Alachkar H, Taubenheim N, Haeney MR, Durandy A, Arkwright PD. Memory switched B cell percentage and not serum immunoglobulin concentration is associated with clinical complications in children and adults with specific antibody deficiency and common variable immunodeficiency. Clin Immunol. 2006;120(3):310–8.
Agematsu K, Nagumo H, Shinozaki K, Hokibara S, Yasui K, Terada K, et al. Absence of IgD-CD27(+) memory B cell population in X-linked hyper-IgM syndrome. J Clin Invest. 1998;102(4):853–60.
Piqueras B, Lavenu-Bombled C, Galicier L, Bergeron-van der Cruyssen F, Mouthon L, Chevret S, et al. Common variable immunodeficiency patient classification based on impaired B cell memory differentiation correlates with clinical aspects. J Clin Immunol. 2003;23(5):385–400.
Carsetti R, Rosado MM, Donnanno S, Guazzi V, Soresina A, Meini A, et al. The loss of IgM memory B cells correlates with clinical disease in common variable immunodeficiency. J Allergy Clin Immunol. 2005;115(2):412–7.
Ko J, Radigan L, Cunningham-Rundles C. Immune competence and switched memory B cells in common variable immunodeficiency. Clin Immunol. 2005;116(1):37–41.
Orange JS, Ballow M, Stiehm ER, Ballas ZK, Chinen J, De La Morena M, et al. Use and interpretation of diagnostic vaccination in primary immunodeficiency: a working group report of the basic and clinical immunology interest section of the American academy of allergy, asthma & immunology. J Allergy Clin Immunol. 2012;130(3 Suppl):S1–24.
Sorensen R, Leiva L, Javier F, Sacerdote D, Bradford N, Butler B, et al. Influence of age on the response to Streptococcus pneumoniae vaccine in patients with recurrent infections and normal immunoglobulin concentrations. J Allergy Clin Immunol. 1998;102:215–21.
Paris K, Sorensen RU. Assessment and clinical interpretation of polysaccharide antibody responses. Ann Allergy Asthma Immunol. 2007;99(5):462–4.
Ferry BL, Jones J, Bateman EA, Woodham N, Warnatz K, Schlesier M, et al. Measurement of peripheral B cell subpopulations in common variable immunodeficiency (CVID) using a whole blood method. Clin Exp Immunol. 2005;140(3):532–9.
Agematsu K, Nagumo H, Yang FC, Nakazawa T, Fukushima K, Ito S, et al. B cell subpopulations separated by CD27 and crucial collaboration of CD27+ B cells and helper T cells in immunoglobulin production. Eur J Immunol. 1997;27(8):2073–9.
Agematsu K, Kobata T, Yang FC, Nakazawa T, Fukushima K, Kitahara M, et al. CD27/CD70 Interaction directly drives B cell IgG and IgM synthesis. Eur J Immunol. 1995;25(10):2825–9.
Kruetzmann S, Rosado MM, Weber H, Germing U, Tournilhac O, Peter HH, et al. Human immunoglobulin M memory B cells controlling Streptococcus pneumoniae infections are generated in the spleen. J Exp Med. 2003;197(7):939–45.
Tangye SG, Good KL. Human IgM + CD27+ B cells: memory B cells or “memory” B cells? J Immunol. 2007;179(1):13–9.
Vinuesa CG, Sze DM, Cook MC, Toellner KM, Klaus GG, Ball J, et al. Recirculating and germinal center B cells differentiate into cells responsive to polysaccharide antigens. Eur J Immunol. 2003;33(2):297–305.
Huck K, Feyen O, Ghosh S, Beltz K, Bellert S, Niehues T. Memory B-cells in healthy and antibody-deficient children. Clin Immunol. 2009;131(1):50–9.
Smet J, Mascart F, Schandene L. Are the reference values of B cell subpopulations used in adults for classification of common variable immunodeficiencies appropriate for children? Clin Immunol. 2011;138(3):266–73.
Siber GR. Pneumococcal disease: prospects for a new generation of vaccines. Science. 1994;265(5177):1385–7.
Pletz MW, Maus U, Krug N, Welte T, Lode H. Pneumococcal vaccines: mechanism of action, impact on epidemiology and adaption of the species. Int J Antimicrob Agents. 2008;32(3):199–206.
Acknowledgments
This work was partially supported by Talecris Biotherapeutics and The Jeffrey Modell Diagnostic Center for Primary Immunodeficiencies.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leiva, L.E., Monjure, H. & Sorensen, R.U. Recurrent Respiratory Infections, Specific Antibody Deficiencies, and Memory B Cells. J Clin Immunol 33 (Suppl 1), 57–61 (2013). https://doi.org/10.1007/s10875-012-9814-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-012-9814-9