Abstract
Purpose
Autosomal recessive hyper-IgE syndrome is a rare combined immunodeficiency characterized by susceptibility to viral infections, atopic eczema, high serum IgE and defective T cell activation. The genetic etiologies are diverse. Null mutations in DOCK8 and TYK2 are responsible for many cases. This study aims to provide a detailed clinical and immunological characterization of the disease and explore the underlying genetic defects among a large series of patients followed by a single center. The available data might improve our understanding of the disease pathogenesis and prognosis.
Methods
Clinical data of twenty-five patients diagnosed with AR-HIES were collected. Seventeen patients screened for STAT3, TYK2 and DOCK8 mutations.
Results
Sinopulmonary infections, dermatitis, hepatic disorders, cutaneous and systemic bacterial, fungal and viral infections were the most common clinical features. The rate of hepatic disorders and systemic infections were high. Twelve patients died with a median age of 10 years. CMV infection was the only statistically significant predicting factor for poor prognosis (early death). Three novel DOCK8 mutations and two large deletions were found in thirteen patients. No mutations found in STAT3 or TYK2 genes.
Conclusion
Autosomal recessive hyper-IgE syndrome is a combined immunodeficiency disease characterized by high morbidity and mortality rate. The different genetic background and environmental factors may explain the more severe phenotypes seen in our series. DOCK8 defect is the most common identified genetic cause. Patients with no identified genetic etiology are likely to carry mutations in the regulatory elements of genes tested or in novel genes that are yet to be discovered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyper IgE syndrome [HIES] is a complex primary immunodeficiency disorder characterized by the clinical triad of chronic eczema, recurrent skin and pulmonary infections and high serum IgE concentration [1]. Two forms of inheritance have been described. An autosomal dominant form caused by dominant-negative mutations in STAT3 [2, 3], and an autosomal recessive form which seems to include multiple clinical phenotypes caused by different molecular mechanisms [1, 4].
The autosomal dominant hyper IgE syndrome[AD-HIES] is a multisystem disorder that affects skin, skeletal, vascular and immune systems as well as connective tissues. Affected individuals are mainly prone to staphylococcal cutaneous and pulmonary infections which are usually complicated by pneumatoceles. Mucocutaneous candidiasis is common and they are at risk of haematological malignancies [1–3].
Although clinically overlapping, autosomal recessive HIES [AR-HIES] is distinct from AD-HIES. Patients have more severe phenotypes with higher mortality rate at younger age. They have higher incidence of viral cutaneous infections, sepsis and neurological complications. They tend not to develop pneumatoceles after pneumonia and somatic features are rarely reported[4]. TYK2 null mutation was identified in two patients with AR-HIES associated with mycobacterial and viral infections [5, 6]. Recently, the clinical phenotype in some patients was attributed to loss of function mutations affecting DOCK8 (dedicator of cytokinesis 8) gene [7, 8]. However, the underlying molecular cause of many patients still not yet identified [8, 9].
Dock8 protein belongs to the DOCK180-related family of atypical guanine nucleotide exchange factors [GEFs] with two conserved Dock homology regions [DHRs]. It is highly expressed in the immune system especially in lymphocytes. It is also expressed in the placenta, kidney, lung, and pancreas [10]. Although the mechanism by which dock8 exerts its function is not well understood, the DOCK180-related family member activates the Rho GTPases such as CDC42 and/or RAC1 by the removal of GDP. These GTPases play an important role in regulating actin cytoskeletal organization and gene expression [11]. DOCK8-mutant mice have demonstrated failure to sustain antibody response. They do not develop marginal zone B cells and have no germinal center B cell persistence [12]. Both B and T cell immune synapse are defective [12, 13]. In those animal models, T cell lymphopenia is noticed with decrease in mature CD4 thymocytes egress and CD8 T cell memory survival [14]. In DOCK8 knockout mice, the migration of interstitial dendritic cells to lymph nodes is defective which will affect the T cell priming process [15].
Our population is highly inbred with 56 % consanguinity rate which predispose to increasing incidence of autosomal recessive diseases [16]. The aim of this study is to characterize AR-HIES in Saudi patients.
Methods
Twenty-five patients from fourteen families with AR-HIES who have been followed up at King Faisal Specialist Hospital and Research Centre [KFSH&RC] were enrolled. Patients with recurrent infections, chronic eczema, eosinophilia [eosinophil count > 500cells/micl] and serum IgE levels ≥ 2,000 IU/ml were included. Patients with high serum IgE levels and eczema but no recurrent infections as well as patients with findings suggestive of AD-HIES [i.e. somatic features and pneumatocele] were excluded.
The clinical and immunological characteristics of the patients were recorded. The median of each of the following values was calculated for each patient: the eosinophil count, serum immunoglobulins, the lymphocyte subsets and the in vitro lymphocyte proliferation response. HIES scores were calculated as previously described [17].
Seventeen patients whom their DNA was available were screened for STAT3, TYK2 and DOCK8 mutations. The dock8 protein expression was assessed whenever it is possible and indicated. The study was approved by the Office of Research Affairs at KFSH&RC, and a written consent was obtained for each of the participating patients.
Statistical Analysis
We did statistical analysis to find out if CMV infection, bronchiectasis, CNS vasculitis and low IgM level, IgE level, CD3, CD4 and the in vitro proliferative response may predict worse prognosis (early death) in AR-HIES in general and dock8 deficiency (DIDS) in particular. We also compared between the previously reported DIDS and Saudi DIDS.
The statistical analysis of the data is done by using the software package SAS version 9.2 [Statistical Analysis System, SAS Institute Inc., Cary, NC, USA]. All continuous variables are compared by using Student’s t-test and the categorical variables are compared by chi-square test. The level of significance is set at p < 0.05.
Results
Twenty-five patients from 14 families not previously reported were fulfilling the criteria [Table I] [online supplementary materials: Figure E1]. The most common manifestations include dermatitis [inclusion criteria] [100 %], sinopulmonary infections [80 %] and failure to thrive [52 %]. The causative organisms included haemophillus influenza (33 %), streptococcal pneumonia (25 %), staphylococcal aureus (25 %) and group A streptococcus (17 %). The recurrent pneumonia led to bronchiectasis in 28 %. Sepsis was documented in 3 patients caused by streptococcal pneumonia, E.coli, klebsiella oxytoca and methicillin resistant staphylococcal aureus. Systemic fungal infections were acquired in 2 patients that included disseminated aspergillous infections and candidemia. Mucocutaneous candidiasis and fungal fingernail infections occurred in 28 %. About 44 % acquired cutaneous viral infections caused by human papilloma virus, herpes simplex virus or molloscum contagiosum. EBV and/ or CMV infections were documented in 10 patients [40 %]. Nine patients [36 %] acquired liver diseases; four with cryptosporidial sclerosing cholangitis, two with hepatitis B and C and one with possible viral-induced hepatitis caused by his EBV and CMV infection. The remaining two patients had no identified infectious etiology, however, no further investigation or liver biopsy done to role out other possibilities.. Autoimmune-mediated phenomena occurred in 3 cases, 2 with autoimmune hemolytic anemia and one with hypothyroidism. One patient developed giant thoracoabdominal aortic aneurysm. Three patients had malignancies including anaplastic B cell lymphoma, adrenal leiomyoma and carcinoma in situ of the perianal area. That carcinoma in situ developed on top of extensive human papilloma virus (HPV) infection of the perianal area. Five patients had neurological symptoms mainly hemiparesis and seizures. Neuroimaging demonstrated evidence of moyamoya disease in one patient, middle cerebral artery syndrome in another one and brain infarctions in the remaining three patients. Allergic disorders were common [70 %]. The commonest was food allergy (70 %) followed by asthma (47 %), drug allergy (17 %) and allergic rhinitis (12 %). No case developed anaphylaxis. Unfortunately 12 patients [48 %] succumbed to severe pneumonia and/ or sepsis with a median age of 10 years [3-16 years].
All patients have eosinophilia with a median of 1,560 cells/micl [range: 670–8,110 cells/micl]. The median serum IgE level was 9,650 IU/ml [IQR 4,632–16,028]. Low serum IgM levels were documented in 8 patients [32 %] in spite of normal number of B cells. Four cases [16 %] have poor antibody response to both pneumococcal and tetanus toxoid vaccine and hence immunoglobulin replacement therapy was commenced. Nine patients showed progressive decline in T lymphocytes count affecting CD4 more than CD8 cells. In vitro lymphocyte proliferation response was depressed in 10 individuals [40 %]. Seventeen patients were DOCK8 deficient as confirmed by genetic study [13patients] or based on assumption due to similar clinical presentation and confirmed affected siblings [4patients].
One patient, F7P2, underwent hematopoietic stem cell transplantation from genoidentical sibling with no conditioning at 8 years of age. Pretransplantation, he was critically ill with eosinophilic pneumonitis, bronchiectasis, hypoxemia, severe diarrhea, cryptococcal sclerosing cholangitis, as well as CMV and EBV infection. He received 4.1 x 106/kg of CD34. Donor cells engraftment using STR showed 13 % myeloid engraftment and 15.6 % lymphocyte engraftment. Although donor cell engraftment resulted in the control of his viral and cryptococcal infections with decreasing IgE level to 330 IU/L, he unfortunately succumbed to severe graft versus host disease of skin and GUT that were proved by tissue biopsy.
Genetic Analysis
Seventeen patients were screened for mutations in DOCK8, STAT3 and TYK2 genes (see Table II). No mutations were found in STAT3 or TYK2. DOCK8 mutations that lead to stop codons were found in 10 patients belonging to 6 families from 5 unrelated tribes. Seven patients [Fig. 1, F1P1, F2P1, F2P2, F2P3, F3P1, F3P2, F3P3] from three unrelated families have an identical mutation in exon 44 [5,625 T > G; Y1875X], two patients [Fig. 2, F4P1 and F5P1] from two families, belonging to the same tribe, have another unique mutation in exon 40 [5,132 C > A; S1711X] and one patient [Fig 3, F13P1] carry a splice site mutation at the 3' end of exon 7 [c. 827 + 6 T > C]. The mutation and exon numbers presented above are based on Variant one [NM_203447.3]. All of the three mutations resulted in a stop codon leading to a truncated protein. The first two mutations (Y1875X and S1711X) are located in the C-terminus of Dock 8 protein between the DHR1 and DHR2 domains and the resulting proteins would lack the DHR2 domain [online supplementary materials: Figure E2]. The third mutation is a splice-site mutation located at the 3' end of exon 7 [c. 827 + 6 T > C]. To assess the effect of this mutation on the splicing and dock8 protein expression, cDNA from this patient was prepared and sequenced. As indicated in Fig. 3c, the cDNA sequence showed clearly exon 7 skipping. Analysis of the amino acid [aa] sequence that would result from such aberrant splicing would result in three aa change followed by a stop codon [Fig. 3d] resulting in a truncated protein [online supplementary materials: Figure E2]. We expected that this mutation would result in the absence of dock8 protein. To confirm this, we performed western blot analysis [Fig. 5] on this patient and found no Dock8 protein was expressed as compared with her father. The mutations described above have not been described previously and were not listed in the Human Gene Mutation Database [HGMD] [http://www.hgmd.org/] web site.
p.Y1875XMutation: a Schematic representation of the exons containing the mutation from each of the protein-coding splice variants. Numbers within the boxes indicate the exon numbers. Vertical arrow point from the affected exon to the electrograms showing the mutation. b Electrograms of the seven family members sequenced as indicated. The line along the electrograms is placed next to the mutation site. ; [C] DNA and protein sequences of normal and affected individuals
p. S1711X Mutation: a Schematic representation of the exons containing the mutation from each of the protein-coding splice variants. Numbers within the boxes indicate the exon numbers. Vertical arrow point from the affected exon to the electrogram showing the mutation. b Electrogram of the sequences of each family member sequenced as indicated. The line along the electrograms is placed next to the mutation site. [C] DNA and protein sequences of normal and affected individuals
c. 827 + 6 T > C Mutation: a Schematic representation of the exons containing the mutation from each of the protein-coding splice variants. Numbers within the boxes indicate the exon numbers. Vertical arrow points from the affected exon to the electrogram showing the mutation. b Electrogram of the sequences of each family member sequenced as indicated. The line along the electrograms is placed next to the mutation site. c Electrogram of the patient cDNA sequence showing the skipping of exon 7. d The cDNA and protein sequences of normal and affected individuals
The remaining 7 patients from 6 families, whom no mutations were detected by sequencing, were screened for micro-deletion using 2.7 M Cytogenetic Microarray. Deletions were found in 3 patients [F6P1, F7P1, and F10P1] belonging to 3 families as shown in Fig. 4. Regarding the deletion of F6P1 and F7P1, it starts from codon 209,111 and ends at codon 338,227 with a size of 129 kbp. For F10P1, the deletion starts from codon 209,111 and ends at codon 6,27, 670 with a size of approximately 419 kbp. The marker counts within these regions are 82 [99 % confidence] and 304 [88 % confidence] respectively. Both deletions are located in P24.3 region at the tip of chromosome 9. Unfortunately, the first marker in this region is located at codon 209,111. Hence, the deletion boundary at 5' end cannot be defined accurately. The deletions could extend further 5' making the deletion larger than indicated. The remaining 4 patients have no deletion that we were able to detect [online supplementary materials: Figure E3]. However, one patient [F8P1] has three copies of the region 440829 to 433626. No DNA was available from her parents for similar analysis. This extra copy span 7.2 kb within the DOCK8 gene [online supplementary materials: Figure E3]. It is hard to assess how this extra copy is distributed over the two alleles. Moreover, the sequencing of this region did not indicate such duplication. Unfortunately, this patient was lost to follow up and we were not able to obtain more blood samples from the patient or her family member.
ChAS output showing the areas of deletions: The DOCK8 deletions of the patients and their relatives are shown as indicated. F = Family; P = Patient. For each individual, the boxed line with an arrow head in the middle indicates the extent of the deletion. Below the boxed line is 5 rows of dots. Each row represents the copy state from zero to 4 copies. The solid lines connecting the dots over a region represent the copy state of that region for the indicated individual. At the bottom of the output, the genes in the covered region are mapped. The green boxes indicate whether the gene is reported to associate with disease. Numbers below the green boxes indicate the distance in kilo bases [kb]
We planned to assess whether the remaining 3 patients [no deletion and no mutations were detected] belonging to two families still express the Dock8 protein by western blot analysis [Fig. 5]. However, we were able to collect blood from only one patient and his family members [F12P1]. The other two patients [F14P1 and F14P2] were lost to follow up. Family 7 is included here as negative control as no Dock8 protein would be expected to be expressed. As expected, F7P1 had no Dock8 expression as compared to his parents. F12P1 expressed Dock8 protein indicating that the genetic cause of HIES in this patient is due to another gene. The patients [F3P3, F6P2, F6P3 and F7P2] were considered Dock8 deficient since they have siblings with confirmed DOCK8 mutation and similar clinical presentation but no available DNA to perform the analysis.
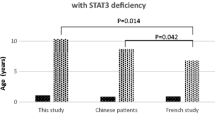
In our statistical analysis CMV infection was found to be the only statistically significant factor predicting poor prognosis (early death) [p value 0.0302] in patients with AR-HIES but not in DIDS patients. Comparing Saudi DIDS with previously reported cases [Table III] [10, 18, 19], our patients have less rate of cutaneous viral infections [p value: 0.0019 ]. However, they have significantly higher susceptibility to systemic viral infections and liver diseases [p value: 0.0008 and 0.0014 respectively]. Low IgM is less frequent in Saudi DIDS [ P value: 0.0319].
Discussion
This is the largest single center series describing the detailed clinical, immunological and molecular characterization of AR-HIES. Sino-pulmonary infections, eczema as well as cutaneous viral, bacterial and fungal infections were the most common manifestations. Neurological complications, malignancies and immune mediated pathologies including autoimmune hemolytic anemia and vasculitis may develop. These clinical findings are consistent with the previously reported cases [Table II] [4, 7, 8]. However, a noteworthy observation is the statistically significant high rate of systemic viral infections as well as the tendency to acquire cryptosporidial infections which may indicate more severe T cell dysfunction. This could be related to the different genetic background. Environmental factors may also have a role but unfortunately we do not have data regarding the prevalence of such infections in our community. Although the clinical phenotype and the high mortality rate point to a significant combined cellular and humoral immune defect, variable immunological findings were observed. Although it is difficult to conclude from this small cohort, CMV infection seems to predict poor prognosis (early death) in patients with AR-HIES probably indicating more severe T cell dysfunction. We failed to prove a similar role for CMV infection in documented Dock 8 deficient patients. One explanation is that our untested AR-HIES patients had other genetic defects that predisposed to uncontrolled CMV infection.
Dock8 deficiency is the most common identified genetic cause of AR-HIES in Saudi patients. We have identified three novel mutations that introduce a stop codon two of which lie between DHR1 and DHR2 domains. Any protein made from transcripts carrying these mutations would be truncated to exclude the DHR2 domain. While DHR1 is required for downstream signaling and biological activity, DHR2 domain was shown to contain the actual catalytic sites for GEF [11]. We conclude that the lack of the catalytic site would impair the Dock8 function and all downstream signaling. The lack of DHR2 domain in the mutant DOCK8 would result in the failure to activate the Rho GTPases. The third mutation was a splice site mutation and was located upstream of DHR1. We showed by cDNA sequencing that this mutation resulted in exon 7 skipping which led to a stop codon. We showed the absence of any Dock8 protein expression in the patient carrying this mutation.
Moreover, we detected large deletion in three patients [Fig. 4 and 5] all of which start upstream of DOCK8 gene eliminating the promoter and the 5' exon or the entire DOCK8 gene in one family. This deletion will abolish any Dock8 protein expression. In addition, in one patient, we observed a duplication that may affect protein expression if part of the inserted DNA located on the two alleles. However, we have no means of assessing its effect in that regard.
Biological data was available from only one patient with undetected DOCK8 mutation. In that patient, we showed normal Dock8 protein expression indicating the possible involvement of other gene downstream of Dock8 signaling pathway. We planned to follow up this family to recruit more affected individuals as they become available for linkage and homozygocity studies.
The fact that none of our patient harbor a TYK2 mutation is in favor of the argument that Tyk2 deficiency is one of IL-12 and INF-α signaling defects with inherited susceptibility to viral and mycobacterial disorders rather than primarily AR-HIES etiology [1]. Those patients whom we failed to detect mutations on them may have sequence alterations that cannot be detected by sequence analysis not covered by our test [e.g. deep intronic mutations]. Another explanation is the presence of other molecular defects that may operate in the remaining cases pointing to the possible genetic heterogeneity of this disorder.
How DOCK8 defect can explain the immunological derangement in DIDS is not fully understood. In humans, investigators demonstrated the association between DOCK8 mutations and impaired T cell activation [7]. It has critical role in T cells survival and persistence of CD8 memory cells [14]. The number of TRECs was found low in DIDS patients which point to possible impaired thymopoiesis and efflux from the thymus. This may result in a restricted diversity of peripheral T cell repertoire [20] . Patients exhibit defective TH17 differentiation that involves the terminal steps as well as their long term persistence [21].
The risk of malignancy in DIDS could be explained by failure of immune surveillance with decreased CD8 function and chronic antigenic stimulation. However, in human, there is evidence that Dock8 may act as tumor suppressor factor since loss of Dock8 expression in different malignancies may contributes to carcinogenesis [11].
With the recent realization of the combined immune defect nature of AR-HIES, there is a tendency to offer HSCT as definite treatment for the affected patients. Five patients successfully engrafted after conditioned hematopietic stem cell transplantation are reported in the literature [22–26]. Our patient, who turned to be Dock8 deficient, was unlucky because of pretransplantation morbidities as well as the severe GVHD he developed. However, the documented engraftment with no conditioning as well as the development of GVHD deliver another strong evidence of the severity of T cell dysfunction in those patients.
One valuable observation in patients with autosomal recessive hyper IgE syndrome in general and DOCK8 deficiency in particular is the high incidence rate of atopy and food allergy. This may base further exploration for the role of DOCK8 in allergic disorders. Indeed, a recent study by Al-Herz et al. demonstrated a selective Th2 bias in Dock8 deficiency which may explain the high rate of atopy [19].
References
Freeman AF, Holland SM. The hyper IgE syndrome. Immunol Allergy Clin North Am. 2008; 28(2):277–viii.
Grimbacher B, Holland SM, Gallin JI, Greenberg F, Hill SC, Malech HL, Miller JA, O'Connell AC, Dent B, Puck JM. Hyper-IgE syndrome with recurrent infections-an autosomal dominant multisystem disorder. N Engl J Med. 1999;340:692–702.
Minegishi Y, Saito M, Tsuchiya S, Tsuge I, Takada H, Hara T, Kawamura N, Ariga T, Pasic S, Stojkovic O, Metin A, Karasuyama H. Dominant-negative mutations in the DNA-binding domain of STAT3 cause hyper-IgE syndrome. Nature. 2007;448:1058–62.
Renner ED, Puck JM, Holland SM, Schmitt M, Weiss M, Frosch M, Bergmann M, Davis J, Belohradsky BH, Grimbacher B. Autosomal recessive hyperimmunoglobulin E syndrome: a distinct disease entity. J Pediatr. 2004;144:939.
Minegishi Y, Saito M, Morio T, Watanabe K, Agematsu K, Tsuchiya S, Takada H, Hara T, Kawamura N, Ariga T, Kaneko H, Kondo N, Tsuge I, Yachie A, Sakiyama Y, Iwata T, Bessho F, Ohishi T, Joh K, Imai K, Kogawa K, Shinohara M, Fujieda M, Wakiguchi H, Pasic S, Abinun M, Ochs HD, Renner ED, Jansson A, Belohradsky BH, Metin A, Shimizu N, Mizutani S, Miyawaki T, Nonoyama S, Karasuyama H. Human tyrosine kinase 2 deficiency reveals its requisite roles in multiple cytokine signals involved in innate and acquired immunity. Immunity. 2006;25(5):745–55.
Zhang Q, Su HC. hyper immunoglobulin E in pediatrics. Current Openion in Pediatrics. 2011.
Zhang Q, Davis JC, Lamborn IT, Freeman AF, Jing H, Favreau AJ, Matthews HF, Davis J, Turner ML, Uzel G, Holland SM, Su HC: Combined Immunodeficiency Associated with DOCK8 Mutations. N Engl J Med 2009; 19; 361(21): 2046–2055.
Engelhardt KR, McGhee S, Winkler S, Sassi A, Woellner C, Lopez-Herrera G, Chen A, Kim HS, Lioret MG, Schulze I, et al. Large deletions and point mutations involving DOCK8 in the autosomal recessive form of the Hyper-IgE syndrome. J Allergy ClinImmunol. 2009;124(6):1289.
Lee W, Huang J, Lin S, Yeh K, Chen L, Hsieh M, Huang Y, Kuo H, Yang KD, Yu H, Jaing T, Yang C: Clinical Aspects and Genetic Analysis of Taiwanese Patients with the Phenotype of Hyper-Immunoglobulin E Recurrent Infection Syndromes [HIES]. J ClinImmunol 2010 Dec 1[online].
Su HC. Dedicator of cytokinesis 8 [DOCK8] deficiency. Current Opinion in Allergy and Clinical Immunology. 2010;10:515–20.
Zhang Q, Davis JC, Dove CG, Su HC. Genetic, clinical and laboratory markers for Dock8 immunodeficiency syndrome. Disease Markers. 2010;29:131–9.
Randall KL, Lambe T, Johnson AL, Treanor B, Kucharska E, Domaschenz H, et al. Dock8 mutations cripple B cell immunological synapses, germinal centers and long-lived antibody production. Nat Immunol. 2009;10(12):1283–91.
Fung I, Russell SM, Oliaro J. Interplay of polarity proteins and GTPases in T-Lymphocyte function. Clin Dev Immunol. 2012;2012:417485.
Lambe T, Crawford G, Johnson AL, Crockford TL, Bouriez-Jones T, Smyth AM, et al. DOCK8 is essential for T-cell survival and the maintenance of CD8+ T-cell memory. Eur J Immunol. 2011;41(12):3423–35.
Harada Y, Tanaka Y, Terasawa M, Pieczyk M, Habiro K, Katakai T, et al. DOCK8 is a Cdc42 activator critical for interstitial dendritic cell migration during immune responses. Blood. 2012;119(19):4451–61.
El Mouzan MI, Al Salloum AA, Al Herbish AS, Qurachi MM, Al Omar AA. Consanguinity and major genetic disorders in Saudi children: a community-based cross-sectional study. Ann Saudi Med. 2008;28(3):169–73.
Grimbacher B, Schäffer AA, Holland SM, Davis J, Gallin JI, Malech HL, et al. Genetic linkage of hyper-IgE syndrome to chromosome 4. Am J Hum Genet. 1999;65(3):735–44.
Sanal O, Jing H, Ozgur T, Ayvaz D, Strauss-Albee DM, Ersoy-Evans S, et al. Additional diverse findings expand the clinical presentation of DOCK8 deficiency. J Clin Immunol. 2012;32(4):698–708.
Al-Herz W, Ragupathy R, Massaad MJ, Al-Attiyah R, Nanda A, Engelhardt KR, Grimbacher B, Notarangelo L, Chatila T, Geha RS. Clinical, immunologic and genetic profiles of DOCK8-deficient patients in Kuwait. Clin Immunol. 2012;143(3):266–72.
Dasouki M, Okonkwo KC, Ray A, Folmsbeel CK, Gozales D, Keles S, Puck JM, Chatila T: Deficient T Cell Receptor Excision Circles [TRECs] In autosomal recessive hyper IgE syndrome caused by DOCK8 mutation: Implications for pathogenesis and potential detection by newborn screening. Clinical immunology. 2011;article in press.
Al Khatib S, Keles S, Garcia-Lloret M, Karakoc-Aydiner E, Reisli I, Artac H, Camcioglu Y, Cokugras H, Somer A, Kutukculer N, Yilmaz M, Ikinciogullari A, Yegin O, Yüksek M, Genel F, Kucukosmanoglu E, Baki A, Bahceciler NN, Rambhatla A, Nickerson DW, McGhee S, Barlan IB, Chatila T: Defects along the T[H]17 differentiation pathway underlie genetically distinct forms of the hyper IgE syndrome. JACI 2009;124(2):342–8, 348.e1-5
Gatz SA, Benninghoff U, Schütz C, Schulz A, Hönig M, Pannicke U, Holzmann KH, Schwarz K, Friedrich W. Curative treatment of autosomal-recessive hyper-IgE syndrome by hematopoietic cell transplantation. Bone Marrow Transplantation. 2011;46:552–6.
Bittner TC, Pannicke U, Renner ED, Notheis G, Hoffmann F, Belohradsky BH, Wintergerst U, Hauser M, Klein B, Schwarz K, Schmid I, Albert MH. Successful long-term correction of autosomal recessive hyper-IgE syndrome due to DOCK8 deficiency by hematopoietic stem cell transplantation. KlinPadiatr. 2010;222(6):351–5.
McDonald DR, Massaad MJ, Johnston A, Keles S, Chatila T, Geha RS, Pai SY. Successful engraftment of donor marrow after allogeneic hematopoietic cell transplantation in autosomal-recessive hyper-IgE syndrome caused by dedicator of cytokinesis 8 deficiency. J Allergy Clin Immunol. 2010;126(6):1304–5.
Barlogis V, Galambrun C, Chambost H, Lamoureux-Toth S, Petit P, Stephan JL et al.: Successful allogenic hematopoietic stem cell transplantation for DOCK8 deficiency. J Allergy Clin Immunol. 2011; 128(2):420–22.e2.
Metin A, Tavil B, Azik F, Azkur D, Ok-Bozkaya I, Kocabas C, Tunc B, Uckan D. Successful bone marrow transplantation for DOCK8 deficient hyper IgE syndrome. Pediatr Transplant. 2012;16(4):398–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
Hamoud Al-Mousa and Abbas Hawwari share senior co-authorship.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
Esm 1
(DOCX 17.8 kb)
Fig. S1
The family pedigrees. Note the high rate of death. (PPT 148 kb)
Fig. S2
Schematic representation of the wild-type variant 1 DOCK8 protein and the expected effect of the indicated mutations on the structure of the protein. Yellow and red boxes indicate the locations of the main domains of the DOCK8 protein. (PPT 72 kb)
Rights and permissions
About this article
Cite this article
Alsum, Z., Hawwari, A., Alsmadi, O. et al. Clinical, Immunological and Molecular Characterization of DOCK8 and DOCK8-like Deficient Patients: Single Center Experience of Twenty Five Patients. J Clin Immunol 33, 55–67 (2013). https://doi.org/10.1007/s10875-012-9769-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-012-9769-x