Abstract
Introduction
We describe a girl presenting at age 6 years with a history of chronic ulcerating intestinal inflammation since 9 months of age. She exhibited a severe, steroid-dependent clinical course of intestinal inflammation over several years in the absence of serious infections.
Results and Discussion
Immunodeficiency was first considered at 6 years of age due to chronic lymphopenia. Immunophenotyping revealed low B and T cell counts with few naïve T cells, a skewed TCR repertoire, and TCR γ/δ T cell predominance, suggesting a defect of lymphocyte development. Genetic and functional analyses identified a hypomorphic mutation in the DCLRE1C (ARTEMIS) gene compromising V(D)J recombination efficiency, but allowing residual T and B cell development. Hematopoetic stem cell transplantation reconstituted the lymphocyte compartment and cured the inflammatory bowel disease.
Conclusion
This report illustrates that a genetic disorder of lymphocyte development can present with chronic inflammatory bowel disease as the dominant phenotype in the absence of severe infection susceptibility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of chronic “inflammatory bowel disease” (IBD) during infancy is rare. Differential diagnoses in this age group include intestinal infections, allergic proctocolitis, lymphonodular hyperplasia, but also primary immunodeficiencies such as chronic granulomatous disease, immunodysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) syndrome, Wiskott–Aldrich syndrome (WAS), anhidrotic ectodermal dysplasia with immunodeficiency (EDA-ID), or IL-10 receptor deficiency [1].
The pathogenesis of IBD still is incompletely understood. A central problem of IBD is the dysregulation of intestinal immune responses. In healthy individuals mucosal immune responses to foreign antigens are limited at various checkpoints preventing local inflammation. These checkpoints include integrity of the epithelium, innate immune mechanisms as well as tolerance of T and B cells [2]. In particular, a disturbed balance of different T cell populations can favor the occurrence of intestinal inflammation [3–6]. An important genetic illustration for this mechanism is provided by patients or mice with IPEX syndrome, who develop IBD due to the lack of regulatory T cells on the basis of FOXP3 deficiency [7, 8]. Paradoxically, IBD has also been observed in several mouse strains with severe lymphopenia due to defects in lymphoid development [9]. Impairment of both, central and peripheral tolerance mechanisms, may contribute to the pathogenesis of IBD under these conditions. Genetic defects in human lymphocyte development result in severe combined immunodeficiency (SCID) and persistent diarrhea is observed in a relevant proportion of these patients. However, the clinical picture is dominated by severe susceptibility to infection and therefore diarrhea and failure to thrive are mostly caused by infections. Older patients with mutations in SCID-causing genes and inflammatory bowel disease as key manifestation have so far not been described.
Materials and Methods
Informed consent for the performed studies was obtained from the patient’s family, in accordance with the guidelines of the local ethics committee.
Case Report
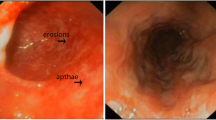
We report a 6-year-old girl born to consanguineous Lebanese parents. Her history was uneventful until the age of 9 months, when she presented with recurrent diarrhea and weight loss. In addition to a persistently increased stool frequency, she experienced episodes of bloody diarrhea and fever every 2 months. Stool was repeatedly negative for Shigella spp., Campylobacter spp., Yersinia spp., Salmonella spp., and Cryptosporidia. At a single timepoint at age 5 years picornavirus RNA was detected but was negative upon retesting as were assays for rotavirus, norovirus, and adenovirus. The girl was diagnosed with juvenile Crohn´s disease on the basis of intestinal biopsies showing patchy chronically active inflammation with superficial fissuring ulcerations. Her IBD responded well to steroids, but relapsed frequently upon steroid tapering despite the addition of azathioprine and sulfasalazin. Disease control improved after the initiation of tacrolimus. However, the girl still thrived poorly despite high caloric supplementation including hydrolyzed formula. Under immunosuppressive treatment the patient developed one episode of oral and intestinal candidiasis responding well to itraconazole. She had several upper respiratory tract infections per year, a third of which were treated with oral antibiotics. One episode of pneumonia at 5 years of age and a labial abscess at 4 years of age required hospitalization. In the context of the immunosuppressive treatment this infection history was not considered unusual.
Flow Cytometry
Lymphocyte phenotyping was performed by four-color flow cytometry using antibodies from BD Biosciences/Pharmingen (Heidelberg, Germany). T cell receptor (TCR) Vβ-staining was performed using antibodies from Coulter Immunotech (Krefeld, Germany). T cell proliferation was assessed by CFSE dilution as described [14]. Cells were analyzed on a BD FACSort using CellQuest Pro software version 4.0.2.
Spectratyping for the TCR-γ and TCR-δ Chains
Analysis of the γδ repertoire was performed as described [10, 14]. RNA was isolated from PBMCs and reverse transcribed by oligo-dT-priming. One of seven Vγ-sense primers and one Cγ-antisense primer were used for amplification of the TCRγ chain. One of six Vδ-sense primers and one Cδ-antisense primer served for amplification of the TCRδ chain. Primers and polymerase chain reaction (PCR) conditions are available upon request (paul.fisch@uniklinik-freiburg.de). Primer extension products were analyzed on an Avant 3100 capillary sequencer equipped with GeneScan 2.0 software (Applied Biosystems Inc., Lincoln, USA).
Isolation of Genomic DNA and Total RNA
For preparation of genomic DNA and total RNA from dermal primary fibroblasts and granulocytes the QIAamp DNA Blood Kit and RNeasy Mini Kit were used (Qiagen, Hilden, Germany).
Genetic Analysis
Coding sequences and exon/intron boundaries of the genomic DCLRE1C (ARTEMIS) gene were amplified using the Taq polymerase system (Qiagen). PCR products were sequenced directly using the BigDye Terminator v3.1 Cycle Sequencing Kit on an ABI PRISM 3100 Genetic Analyzer (Applied Biosystems, Foster City) and Primer (Thermo Scientific, Ulm, Germany). Primer sequences are available on request (ulrich.pannicke@uni-ulm.de).
Artemis cDNA Synthesis and Cloning
Two hundred nanograms of total RNA of fibroblasts from the patient were reverse transcribed with the SuperScript II Reverse Transcriptase Kit (Invitrogen, Carlsbad) using random hexamer priming. cDNAs were amplified via RT-PCR using Taq polymerase system (Qiagen) and primer ARTcDNAEx5F (5′-CTTACCAGCTGGTCACTGTCC-3′) and ARTcDNAEx11R (5′-AAGAAAAACAAGCTCTGATGAACTCTCTCC-3′) (Thermo Scientific). cDNAs were cloned into the TOPO-TA Cloning vector (Invitrogen) and sequenced with primer ARTcDNAEx5F. Numbers of identified clones are depicted. ARTEMIS cDNA from NHDF served as control. For construction of expression plasmids ARTEMIS cDNA variants were amplified by Pfu polymerase (Stratagene, La Jolla) using primer Kpn1ARTcDNA5′N (5′-GGGGTACCGCTATGAGTTCTTTCGAGGG-3′) and Not1ARTcDNA3′w/oSTOP (5′-ATAAGAATGCGGCCGCCAGGTATCTAAGAGTGAGC-3′) and cloned into the pcDNA6/myc-His Version A (Invitrogen) plasmid. ARTEMIS ORFs were verified by sequencing.
Western Blot
HEK293T cells were transfected by the calcium phosphate precipitation method with 4.5 µg pcDNA6/myc-His Version A plasmid, coding for either wild-type or mutated versions of ARTEMIS fused to the myc-His tag. Dermal primary fibroblasts were transfected using the Amaxa Cell Line Nucleofactor Kit V (Lonza, Cologne, Germany) with 10 µg pcDNA6/myc-His Version A plasmid. For determination of transfection efficiencies cells were co-transfected with 0.5 µg (HEK293T cells) or 1.0 µg (fibroblasts) pEGFP-C1 plasmid (Clontech, Mountain View) encoding the enhanced green fluorescent protein. After 24 (fibroblasts) or 48 h (HEK293T cells), cells were harvested and lysed in the lysis buffer (50 mM Tris–HCl pH 8.0, 62.5 mM EDTA, 1% (w/v) NP-40, 0.4% (w/v) sodium deoxycholate). Lysates were spun down in a microcentrifuge at 14,000×g to pellet insoluble debris. Protein concentrations of the lysates were determined by the BioRad Dc Protein assay (BioRad, Hercules). A 10 µg portion of each lysate was run on an 8% SDS–polyacrylamide gel. The proteins were transferred to PVDF membranes (Millipore, Billerica) and the blots were developed using a monoclonal mouse anti-myc (Invitrogen) and polyclonal rabbit anti rGFP (Clontech) antibodies. Secondary antibodies used were goat anti-mouse IgG (H+L)-HRP-conjugate and goat anti-rabbit IgG (H+L)-HRP-conjugate.
In Vitro V(D)J Recombination Assay
In vitro V(D)J recombination assays were performed as described in human primary dermal fibroblasts [11]. Fibroblasts of a healthy control and of a patient with DCLRE1C (ARTEMIS) null mutations as well as those of the IBD patient were co-transfected with an inversional V(D)J recombination substrate vector and expression plasmids coding for the RAG (RAG1 and RAG2) proteins. As negative control the same co-transfections without the expression plasmid coding for RAG2 (−RAG2) were performed. For assaying the particular patient Artemis cDNA variants Artemis-deficient fibroblasts were co-transfected with V(D)J recombination substrate vector and expression plasmids coding for the RAG (RAG1 and RAG2) proteins and wild-type Artemis (+ART) or mutant Artemis (+ARM87, +ARM88, +ARM82, and +ARM89) proteins, respectively. As negative control the same co-transfection without the expression plasmids coding for RAG2 (−RAG2) or Artemis (−ART) were performed. As positive control a pre-recombined substrate vector was transfected. In each assay 5 × 104 fibroblasts were analyzed by FACS and the mean percentages ±SD of recombination-positive cells out of the subpopulation of transfected fibroblasts are depicted.
Histology and Immunohistochemistry
Hematoxilin–eosin stained sections of formalin-fixed paraffin-embedded biopsy specimens were analyzed from the terminal ileum and colon. For immunohistochemistry, sections were deparaffinized and rehydrated through graded alcohols. The primary unconjugated antibodies included CD20 at 1:200 (L26, Dako, Glostrup, Denmark), CD3 at 1:50 (F7.7.38, Dako), CD38 at 1.200 (SPC32, Novocastra, Newcastle, UK), and TCR-ßF1 at 1:20 (8A3, Thermo-Scientific, Rockford, USA). Immunostaining with CD3 and TCR-ßF1 antibodies was done after digestion with 0.05% proteinase K (Sigma-Aldrich Chemie, Munich, Germany) in phosphate-buffered saline pH 7.4. Heat-mediated antigen-retrieval was performed for CD38 by boiling the sections in a steamer in target retrieval solutions (Dako). After incubation for 20 min with 10% blocking sera from the respective animal species (Biotrend, Cologne, Germany), sections were stained semiautomatically (Autostainer instrument, Dako) with the primary antibodies and biotinylated anti-mouse and anti-rabbit detection antibodies. Bound detection antibodies were detected based on the labeled streptavidin-biotin method (ChemMate K5005 Alkaline Phosphatase/Red detection kit, Dako). Nuclei were counterstained with Mayer’s hemalaun solution.
Results
At age 6 years the patient underwent an immunological evaluation because of persistent lymphopenia, which had originally been attributed to the immunosuppression. A review of intestinal biopsies taken at age 9 months showed acute and chronic inflammatory changes with skip areas, predominantly ileal involvement and a less pronounced inflammation in the colon, reminiscent of Crohn’s disease. Characteristic features included superficial fissures extending into the submucosa, aphtous lesions overlying lymphoid aggregates, rare histiocytic microgranulomas, and florid cryptitis. Abundant transmural lymphoid aggregates typical for classical Crohn’s disease were absent. Immunohistochemical analysis of lymphoid aggregates in the vicinity of the fissures revealed clusters of CD3+ T cells (Fig. 1b) which were, however, less dense than those observed in a representative biopsy of a Crohn’s patient (Fig. 1a). A TCRβ-F1+ subpopulation was abundant in the Crohn’s sample (Fig. 1c), but rare in our patient (Fig. 1d), suggesting γδ T cell predominance. Both specimens also showed aggregates of CD20+ B cells (Fig. 1e, f), a diffuse infiltration by CD38+ plasma cells (Fig. 1g, h) and clusters of CD68+ histiocytes.
Immunohistology of colon biopsies. Superficial fissuring ulceration of the mucosa with severe chronic inflammation and lymphoid aggregates in biopsies from a 15-year-old control patient with Crohn’s disease (a, c, e, g) and from the patient (b, d, f, h). Sections were stained with anti-CD3 (a, b), anti TCR-βF1 (c, d), anti-CD20 (e, f), and anti-CD38 (g, h)
The patient had severely reduced numbers of T and B lymphocytes (Table I). Only 2.5% of the patient’s CD4+ T cells were naïve (CD45RA+), but they proliferated normally to PHA, OKT3, IL-2, PWM, and ConA. More than 50% of the B cells were IgM− IgD− and 75% of B cells expressed CD27. The immunoglobulin levels were normal (IgG 791–1,210 mg/dl, IgM 101–308 mg/dl, IgA 67–280 mg/dl) with normal levels of IgG1 and IgG2, decreased levels of IgG4 and positive serological responses to tetanus, CMV, EBV, and VZV (data not shown). Vβ analysis of CD4+ T cells revealed mild skewing. More than 60% of T cells were γδ T cells expressing Vδ2 and Vγ9. Spectratyping of the TCRγ and δ transcripts showed a polyclonal γδ T cell repertoire with slightly less variability than in a healthy adult control (data not shown).
Due to the T low B low NK+ lymphopenia with decreased naïve T cells we sequenced the DCLRE1C (ARTEMIS) gene and found a novel homozygous point mutation at position exon 6+1 g>a (c.461+1 g>a; NM_001033855.1; splice donor site gt to at). Both parents were heterozygous for the mutation. In vitro V(D)J recombination assays revealed residual recombination activity compared to control fibroblasts with a null mutation (Fig. 2a). Analysis of Artemis mRNA showed several bands in patient’s cells, none of which was of normal size (Fig. 2c). The bands were subcloned and sequenced. Four of the six recovered sequences were in frame and displayed either a skipping of exon 6 or an insertion of either 12, 18, or 120 nucleotides. The 18-nucleotide insertion variant was predominantly expressed (data not shown). None of these alternative transcripts were expressed in cells from a healthy control. All in frame sequence variants were translated and detectable by Western blot (Fig. 2d). However, functional analysis of these variant proteins in an in vitro V(D)J recombination assay revealed that only the Artemis proteins carrying an insertion of six (ARM 82) and four amino acids (ARM 88) retain sufficient residual activity to recombine the substrate vector, whereas the insertion of 40 amino acids (ARM 89) and the deletion of exon 6 (ARM 87) lead to a complete loss of function (Fig. 2b).
Molecular and functional analysis of Artemis. a V(D)J recombination was tested by transfecting fibroblasts from a healthy control, a patient with DCLRE1C (ARTEMIS) null mutations and the IBD patient with an inversional V(D)J recombination substrate vector and expression plasmids coding for the RAG (RAG1 and RAG2) proteins. Co-transfections without the expression plasmid coding for RAG2 (−RAG2) served as negative controls. b V(D)J recombination assay in human Artemis-deficient fibroblasts co-transfected with a substrate vector and expression plasmids coding for RAG1/2, wild-type Artemis (+ART) or mutant Artemis proteins (ARM82, 87, 88, 89). As controls, the same co-transfections without the expressions plasmids coding for RAG2 (−RAG2) or wild-type ARTEMIS (−ART) were performed. c RT-PCR of Artemis depicting expression of different Artemis splice variants in fibroblasts of the patient. “1” depicts wt Artemis cDNA (Ex 5-11), whereas in the band number “2” a deletion of exon , in band number “3” an insertion of 12 and 18 bp and in band number “4” an insertion of 120 and 122 bp was indentified. d Expression of wild-type and mutant ARTEMIS proteins. HEK293T cells and ARTEMIS-negative fibroblasts were transfected with pcDNA6 expression plasmids coding for myc-His fusion proteins of either wild-type (ART-WT) or mutant (ARM82, 87, 88, 89) ARTEMIS. As controls, HEK293T and fibroblasts transfected either without plasmid (−) or with empty pcDNA6 vector (vector) were used. Additionally, except the control without plasmids (−), all cells were transfected with the pEGFP-C1 plasmid encoding the enhanced green fluorescent protein
Although the child had no relevant susceptibility to infection, the poorly controlled IBD in combination with failure to thrive and the increased lymphoma risk reported in patients with hypomorphic Artemis mutations [12] prompted us to perform hematopoetic stem cell transplantation (HSCT). The girl received a haploidentical, CD3- and CD19-depleted peripheral blood stem cell graft from her father. Immunological reconstitution was excellent. The diarrhea improved after day +25 and completely vanished eventually. Three years after HSCT, she is free of IBD symptoms without medication.
Discussion
In this study, we identified a mutation in a SCID-causing gene in a patient, who had suffered from chronic inflammatory bowel disease for several years in the absence of significant infections.
The patient carried a functionally relevant homozygous point mutation in DCLRE1C (ARTEMIS), a gene required for normal development of T and B lymphocytes. Although the patient did not express wild-type Artemis mRNA, some of the alternative mRNA-transcripts retained catalytic activity, allowing residual V(D)J recombination. These functional data indicate a hypomorphic mutation. The resulting immunological phenotype shows various features that have also been observed in patients with hypomorphic mutations in other SCID-causing genes [17]: Severely reduced naïve T cells, a skewed T cell repertoire, and γδ T cell predominance have been reported in RAG-, Ligase IV-, and IL2RG-deficient patients [10, 13, 14]. Normal or even elevated immunoglobulin levels and specific antibody responses have been documented in hypomorphic variants of SCID [12–18]. Seven patients with hypomorphic DCLRE1C (ARTEMIS) mutations have been reported and in addition to susceptibility to infections the manifestations included autoimmune cytopenias, lymphoma, and Omenn syndrome, a combination of lymphoproliferation, erythroderma and elevated IgE [12, 19, 20]. Development of IBD has so far not been documented.
Several lines of evidence indicate that the ARTEMIS mutation is causally related to the IBD in this patient. First, observations in humans and mice suggest that genetic defects allowing the development of limited numbers of T and B cells lead to a poorly regulated specific immune system prone to autoimmunity [21]. More specifically, mice with targeted deletions of the TCRα or TCRβ genes, who lack αβ T cells but retain γδ T cells, spontaneously develop IBD [9]. Furthermore, TCR β-deficient mice develop a more severe intestinal inflammation than TCR β/γ double-deficient mice supporting a potential role of γδ T cells in the pathogenesis of IBD, particularly under lymphopenic conditions [9]. Second, the IBD in our patient was poorly responsive to immunosuppressive therapy, but was cured by HSCT. These considerations are consistent with the interpretation that poorly regulated T cell responses in our lymphopenic patient led to the IBD, which was cured by the normal immunological reconstitution after HSCT. It is becoming more and more evident that chronic IBD may be the leading symptom of a primary immunodeficiency. This report extends the spectrum of differential diagnosis to atypical forms of SCID presenting beyond infancy. Clinical work-up of children with IBD should therefore include appropriate investigations, in particular with respect to the important consequences for therapy.
Abbreviations
- EDA-ID:
-
anhidrotic ectodermal dysplasia with immunodeficiency
- HSCT:
-
hematopoietic stem cell transplantation
- IBD:
-
inflammatory bowel disease
- IPEX:
-
immunodysregulation, polyendocrinopathy, enteropathy, X-linked
- TCR:
-
T cell receptor
- WAS:
-
Wiskott-Aldrich syndrome
References
Glocker EO, Kotlarz D, Boztug K, Gertz EM, Schäffer AA, Noyan F, et al. Inflammatory bowel disease and mutations affecting the interleukin-10 receptor. N Engl J Med. 2009;361:2033–45.
Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–34.
Powrie F, Leach MW, Mauze S, Caddle LB, Coffman RL. Phenotypically distinct subsets of CD4+ T cells induce or protect from chronic intestinal inflammation in C. B-17 scid mice. Int Immunol. 1993;5:1461–71.
Powrie F, Correa-Oliveira R, Mauze S, Coffman RL. Regulatory interactions between CD45RBhigh and CD45RBlow CD4+ T cells are important for the balance between protective and pathogenic cell-mediated immunity. J Exp Med. 1994;179:589–600.
Shull MM, Ormsby I, Kier AB, Pawlowski S, Diebold RJ, Yin M, et al. Targeted disruption of the mouse transforming growth factor-beta 1 gene results in multifocal inflammatory disease. Nature. 1992;359:693–9.
Kuhn R, Lohler J, Rennick D, Rajewsky K, Muller W. Interleukin-10-deficient mice develop chronic enterocolitis. Cell. 1993;75:263–74.
Bennett CL, Christie J, Ramsdell F, Brunkow ME, Ferguson PJ, Whitesell L, et al. The immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) is caused by mutations of FOXP3. Nat Genet. 2001;27:20–1.
Torgerson TR, Ochs HD. Immune dysregulation, polyendocrinopathy, enteropathy, X-linked: forkhead box protein 3 mutations and lack of regulatory T cells. J Allergy Clin Immunol. 2007;120:744–50. quiz 751-2.
Mombaerts P, Mizoguchi E, Grusby MJ, Glimcher LH, Bhan AK, Tonegawa S. Spontaneous development of inflammatory bowel disease in T cell receptor mutant mice. Cell. 1993;75:274–82.
Enders A, Fisch P, Schwarz K, Duffner U, Pannicke U, Nikolopoulos E, et al. A severe form of human combined immunodeficiency due to mutations in DNA ligase IV. J Immunol. 2006;176:5060–8.
Pannicke U, Ma Y, Hopfner KP, Niewolik D, Lieber MR, Schwarz K. Functional and biochemical dissection of the structure-specific nuclease ARTEMIS. EMBO J. 2004;23:1987–97.
Moshous D, Pannetier C, Chasseval Rd R, Deist Fl F, Cavazzana-Calvo M, Romana S, et al. Partial T and B lymphocyte immunodeficiency and predisposition to lymphoma in patients with hypomorphic mutations in Artemis. J Clin Invest. 2003;111:381–7.
de Villartay JP, Lim A, Al-Mousa H, Dupont S, Déchanet-Merville J, Coumau-Gatbois E, et al. A novel immunodeficiency associated with hypomorphic RAG1 mutations and CMV infection. J Clin Invest. 2005;115:3291–9.
Ehl S, Schwarz K, Enders A, Duffner U, Pannicke U, Kühr J, et al. A variant of SCID with specific immune responses and predominance of gamma delta T cells. J Clin Invest. 2005;115:3140–8.
Buck D, et al. Severe combined immunodeficiency and microcephaly in siblings with hypomorphic mutations in DNA ligase IV. Eur J Immunol. 2006;36(1):224–35.
Kumaki S, et al. Identification of anti-herpes simplex virus antibody-producing B cells in a patient with an atypical RAG1 immunodeficiency. Blood. 2001;98(5):1464–8.
Pasic S, et al. Recombinase-activating gene 1 immunodeficiency: different immunological phenotypes in three siblings. Acta Paediatr. 2009;98(6):1062–4.
Karaca NE, et al. Diverse phenotypic and genotypic presentation of RAG1 mutations in two cases with SCID. Clin Exp Med. 2009;9:339–42.
Ege M, Ma Y, Manfras B, Kalwak K, Lu H, Lieber MR, et al. Omenn syndrome due to ARTEMIS mutations. Blood. 2005;105:4179–86.
Peake J, Waugh A, Le Deist F, Priestley A, Rieux-Laucat F, Foray N, et al. Combined immunodeficiency associated with increased apoptosis of lymphocytes and radiosensitivity fibroblasts. Cancer Res. 1999;59:3454–60.
Villa A, Marrella V, Rucci F, Notarangelo LD. Genetically determined lymphopenia and autoimmune manifestations. Curr Opin Immunol. 2008;20:318–24.
Acknowledgements
This work was supported by the Bundesministerium für Bildung und Forschung (BMBF 01 EO 0803). We acknowledge the excellent technical assistance of S. Braun, I. Janz, and E. M. Rump.
Conflicts of Interest
No conflicts of interest exist for any author.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jan Rohr and Ulrich Pannicke contributed equally to this work.
Grant support list
K.S., S.E.: German Ministry of Education and Science (BMBF 01 EO 0803).
Rights and permissions
About this article
Cite this article
Rohr, J., Pannicke, U., Döring, M. et al. Chronic Inflammatory Bowel Disease as Key Manifestation of Atypical ARTEMIS Deficiency. J Clin Immunol 30, 314–320 (2010). https://doi.org/10.1007/s10875-009-9349-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-009-9349-x