Abstract
Background
IgA deficiency (IGAD) is the most common primary antibody deficiency. Although many affected individuals have no apparent symptom, selected patients suffer from recurrent mucosal infections, allergies, and autoimmune diseases. We aimed to investigate the clinical features in relation to immune function of Iranian patients with symptomatic IGAD.
Methods
Thirty-seven patients (21 male and 16 female), aged 4–32 years, were evaluated in this study. Patients were followed for a total of 131 patient years with a mean follow-up of 3.5 years per patient.
Results
The most prevalent presentations were recurrent infections occurring in 27 subjects, followed by allergy in eight cases and autoimmunity in two patients. However, during the follow-up period, 35 patients developed infections in respiratory and gastrointestinal tracts, necessitating medical care. Apart from infections, allergy was the most frequent complaint (31 cases); the major features were asthma, atopic dermatitis, and allergic rhinoconjunctivitis. Autoimmune diseases were documented in ten cases; thyroiditis was the most common. In 31 patients who received unconjugated pneumococcal polyvalent vaccine, antibody response against polysaccharide antigen was measured before and 28 days after vaccination. One fourth of vaccinated patients were hyporesponsive to vaccine; four of these patients developed bronchiectasis. The patients with IGAD were classified into two groups: group 1 (14 cases) consisted of patients with IGAD and other associated immune defects, such as immunoglobulin G (IgG) subclass deficiency and defective specific antibody production. Group 2 (23 cases) had isolated IGAD without other immunological abnormalities. There was a significantly increased number of lower respiratory tract infections in group 1 compared with group 2 (P = 0.006). Moreover, four patients of group 1 had bronchiectasis whereas none of the patients in group 2 developed this complication (P = 0.015).
Conclusion
Subclassification of IGAD regarding the existence of associated immune defects is useful in terms of morbidity and planning for medical care. IgA-deficient patients with concomitant immune defects such as defects in specific antibody production have higher rates of recurrent infections and bronchiectasis, which necessitates more effective monitoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Selective IgA deficiency (IGAD) is the most common primary antibody deficiency [1]. It is defined by serum levels of IgA less than 0.05 g/L in the presence of normal IgG and IgM in a patient older than 4 years [2, 3]. The incidence of IGAD varies from 1:396 to 1:15,000 in different regions [4–7]. Although the fundamental defect is elusive, an impaired terminal differentiation of B cells and defect in switching to IgA-producing plasma cells are presumed to be responsible. IGAD shares many features with common variable immunodeficiency (CVID) another prototypic primary antibody deficiency. A common genetic basis for IGAD and CVID has been suggested [1].
Most affected individuals are asymptomatic, whereas approximately one third of patients suffer from recurrent mucosal infections, allergies, and autoimmune diseases [8, 9]. The main involved organs are respiratory and gastrointestinal tracts [5, 7, 10]. Recurrent sinopulmonary infections are caused by extracellular encapsulated bacteria (e.g., Haemophilus influenzae, Streptococcus pneumoniae). Gastrointestinal diseases include giardiasis, nodular lymphoid hyperplasia, celiac disease, and inflammatory bowel disease [11, 12]. IgA-deficient patients may be frequently affected by allergies, the most common of which is asthma followed by allergic rhinitis and conjunctivitis, urticaria, atopic dermatitis, and food allergies [7, 13]. Autoimmune diseases associated with IGAD include immune thrombocytopenic purpura, autoimmune hemolytic anemia, rheumatoid arthritis, lupus erythematosus, thyroiditis, and vitiligo [8, 9, 14, 15].
In spite of several published studies on IgA deficiency, there are few surveys studying the correlation between clinical and immunological phenotypes of symptomatic IGAD patients. We aimed to investigate the clinical features in relation to immune function in 37 patients with IGAD.
Patients and Methods
Patients
Thirty-seven patients were enrolled in the study. Thirty five of them presented with or developed infections during the course of disease follow-up; only two patients were free of infection. Diagnosis of IGAD was based on low serum IgA level (less than 5 mg/dl) and normal IgG and IgM levels in patients older than 4 years old [3]. Other immunodeficiencies like ataxia-telangiectasia and drug-induced IgA deficiency have been excluded. Clinical and laboratory findings of each patient were recorded in a designed questionnaire.
Immunoglobulin Levels and Antibody Responses
Serum levels of IgG, IgA, IgM, and IgE were measured by nephelometry (Behring Nephelometer, Behringwerke, Marburg, Germany). Serum IgG1, IgG2, IgG3, and IgG4 levels and antibody response against diphtheria and tetanus toxoids were measured using an enzyme-linked immunosorbent assay (ELISA). All patients were fully immunized according to the national vaccination program including diphtheria and tetanus toxoids. The results were interpreted based on the previous established criteria: diphtheria antitoxin level of 0.01 IU/ml or greater and tetanus antitoxin level 0.1 IU/ml or greater were regarded as protective.
Thirty one out of 37 patients received unconjugated pneumococcus polysaccharide vaccine (PNEUMO 23® Aventis, Pasteur, France). Specific antibodies against whole pneumococcal antigen were measured using the protocol of the third generation ELISA assay format before and 4 weeks after vaccination [16]. Forty-five healthy volunteers, selected as the control group, were immunized with the same pneumococcal vaccine. Results were reported as end point titer determined by the highest dilution giving an optical density of ≥0.2. The median titers before and after vaccination in the control group were 70 and 450 U/mL, respectively. The lower limit of the two-tailed 90% probability interval of postimmunization-specific IgG was 129 U/mL, which is used as the minimum significant increase for adequate response in the patients’ group [17].
Pulmonary Evaluation
Pulmonary function was evaluated according to the American Thoracic Society guidelines [18] by using a computerized pneumotachograph (Jaeger, Germany) in patients 6 years and older who could cooperate. Forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FEV1/FVC, maximal midexpiratory flow were recorded.
In those with chronic pulmonary infections, high-resolution computed tomography scan was performed to confirm the presence of bronchiectasis.
Skin Prick Test
The allergy status of patients with a pertinent history was evaluated by skin prick test on the forearm, using 14 common standard allergen extracts (Stallergen, France). Histamine and normal saline were simultaneously used as positive and negative controls, respectively. A wheal formation ≥3 mm above negative control after 15–20 min was considered as positive.
Classification of Disease
The patients were classified in two groups: group 1 consisted of patients with concomitant low IgG subclass levels (IgG2, IgG3) or reduced IgG response to protein and polysaccharide antigens. Patients who had only selective IGAD with normal IgG subclass levels and specific antibody response were assigned as group 2. IgG4 deficiency was not considered as concomitant immune defect. Demographic and clinical data of patients in group 1 are depicted in Table I.
Statistical Analysis
Data were compared between the two groups using Fisher’s exact test and Mann Whitney U test for qualitative and quantitative measures, respectively. Data analysis was performed by SPSS statistical software package, version 14.0 (SPSS Inc, Chicago, IL, USA).
Results
Characteristics of Patients
Thirty-seven patients (21 male and 16 female from unrelated 36 families), aged 4–32 (median = 9) years, were evaluated. Patients were followed for a total of 131 patient years with a mean follow-up of 3.5 years per patient. During this period, two patients evolved to CVID (P35 and P36), which were started on intravenous immunoglobulin (IVIG). P35 was a 22-year-old girl presenting first with myasthenia gravis and IGAD that evolved to CVID over time [19]. Finally, she expired due to uncontrolled pulmonary failure. P36 is a 26-year-old man, presented first at 10 years with respiratory infections, developed bronchiectasis at age 23, and diagnosed as CVID. He is currently on regular IVIG with good clinical condition.
Clinical Manifestations
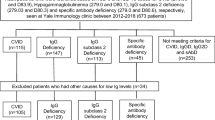
The most prevalent presentations were recurrent infections occurring in 27 subjects (73%), followed by allergy in eight cases (22%) and autoimmunity in two patients. However, during the follow-up period, 35 patients (94%) developed infections in respiratory and gastrointestinal tracts, necessitating medical care (Table II). Apart from infections, allergy was the most frequent complaint, observed in 84% of patients; the major features were asthma, atopic dermatitis, and allergic rhinoconjunctivitis (Table II). Autoimmune diseases were documented in ten cases; among which thyroiditis was the most common (four cases), followed by vitiligo, myasthenia gravis, celiac disease, autoimmune hemolytic anemia, Crohn’s disease, alopecia areata, and juvenile idiopathic arthritis. As illustrated in Fig. 1, most patients had overlapping manifestations.
Two patients had no infections and their clinical problems were either allergy or autoimmunity. The first case was diagnosed with IGAD during screening for asthma associated with atopic dermatitis at age of 4 years. The second one presented with diarrhea beginning at age of 3 years. Further investigation showed he had celiac disease associated with IgA deficiency.
Severe autoimmune hemolytic anemia occurred in a 5-year-old male patient necessitating hospital admission and blood transfusion.
In our series, a male patient, aged 4 years, presented with recurrent respiratory infections, microcephaly, hypertelorism, and low-set ears. Chromosomal karyotyping showed ring chromosome 18.
Family History
In 12 families, parents were consanguineous of which nine were first cousins. To investigate familial segregation of IgA deficiency, serum IgA levels of all parents and symptomatic siblings of affected patients were measured. During this screening, we found one new IGAD and two partial IGAD patients. These two individuals with partial IgA deficiency were not included in the study.
History of allergic disorders and autoimmune diseases were investigated in 633 family members of the studied patients: 43 family members (6.8%) had allergy, while 39 family members (6.2%) had autoimmunity.
Serum Immunoglobulins
All patients had serum IgA levels of less than 5 mg/dl, with normal serum IgG levels (mean = 1,360 ± 460 mg/dl). Although the mean serum IgM levels of these patients were in normal range (90 ± 50 mg/dl), 14 cases had elevated levels of IgM over two SD compared with age-matched controls. In addition to IgA deficiency, two patients lacked IgG2 subclass and two others had IgG3 deficiency. Eleven cases had associated IgG4 deficiency, which was not assumed as immunological defect.
Antibody Response
Antibody titers to tetanus and diphtheria proteins were measured in all patients. Five (13.5%) patients (P12, P21, P22, P26, P37) had nonprotective antibody titers.
In 31 patients who received unconjugated pneumococcus polyvalent vaccine, antibody response against polysaccharide antigen was measured before and 28 days after vaccination. Eleven (35%) out of 31 vaccinated patients were hyporesponsive to pneumococcal antigen (Table I) in comparison with normal controls. The lower limit of the two-tailed 90% probability interval of postimmunization-specific IgG was utilized as the minimum significant increase for adequate response in the patients.
Among 11 patients who were hyporesponsive to polysaccharide antigen, four patients (P28, P30, P35, P36), aged 14 to 26 years, developed bronchiectasis, whereas none of the patients younger than 10 years developed this complication.
All these bronchiectatic patients were started on monthly IVIG replacement therapy with 500–600 mg/kg with significant reduction in the rate of bacterial infections and chronic chest symptoms.
After treatment with IVIG, the incidence of pneumonia was reduced from 0.7 before treatment to 0.2 after treatment per patient per year.
Pulmonary Function Test
Twenty-four patients cooperated to perform a pulmonary function test (PFT) using spirometry. The volume and flows were normal in 18 subjects (75%). Abnormal PFTs included an obstructive pattern in three patients, a restrictive pattern in two cases, and a mixed pattern (obstructive–restrictive) in one.
Skin Prick Test
Skin prick test was performed for 31 patients whom had allergic symptoms using 14 common allergen extracts (Stallergen, France). Fifteen out of 31 (48%) showed positive results to at least one tested allergen. The most frequent detected allergens were weeds (15 cases) and Dermatophagoides pteronyssinus (15 cases) followed by cockroach (12 cases), cat fur (12 cases), Dermatophagoides farinaee (nine cases), and Alternaria alternata (nine cases). Other less frequent allergens were cow’s milk (six cases), mixed grasses (six cases), mixed trees (three cases), egg whole (three cases), and hazel nut (three cases).
Classification of Disease
The patients with IgA deficiency were classified into two groups of IgA deficiency with other associated immune defects (group 1) and IgA deficiency without other immunological abnormalities (group 2).
Twelve out of 14 patients (86%) in group 1 presented with recurrent infections compared to 15 out of 23 patients (65%) in group 2. There was a significantly increased number of upper and lower respiratory tract infections in group 1 compared with group 2 (Table II). Moreover, four patients of group 1 had bronchiectasis, whereas none of the patients in group 2 developed this complication (P = 0.015). There was no significant difference in the frequency of allergy and autoimmunity between the two groups. Mean serum IgM level in group 2 was significantly higher than group 1 (105 ± 55 vs. 75 ± 25 mg/dl, P = 0.035).
Discussion
IgA is a first line of immune protection at mucosal surfaces which are exposed to external potentially harmful agents. IGAD is the most common primary antibody deficiency, which could be seen either asymptomatic or symptomatic [8, 9]. A common genetic basis for IGAD and CVID has been suggested by their occurrence in members of the same family and the progression from IGAD to CVID that has been reported in several cases [19, 20].
Two studies have recently reported that coding variants in TNFRSF13B, which encodes transmembrane activator and CAML interactor (TACI), are associated with CVID and IGAD [21, 22]. Worldwide prevalence of IGAD varies between 1/396 in Finland and 1/15,000 in Japan [4–7, 23]. Although higher prevalence of IGAD was reported in Iranian Primary Immunodeficiency Registry based on data of symptomatic patients [24], frequency of one in 651 is estimated based on the study on Iranian blood donors [25]. However, if we take a look at selected patients with recurrent infections, IGAD frequency will be higher, as it is shown to be about 5.3% to 9.3% [26–28]. Here, we present the clinical and laboratory features of 37 symptomatic IGAD patients evaluated in our center.
In our series, 94% of patients experienced infections during the course of the disease which is in agreement with previous studies [10, 14] that showed 50–77% of patients with symptomatic IGAD experienced recurrent infections.
Although infections are the most prominent symptoms in symptomatic individuals with IGAD, a number of allergic and autoimmune diseases may represent as a common association [5, 29]. Sometimes, allergic manifestations could be the first presenting symptoms as we observed in 15 cases (40.5%). During follow-up period, a total number of 31 (83.7%) patients developed allergic symptoms in our study, which is much higher than the prevalence of allergic rhinitis and asthma among Iranian normal population (about 22–23% and 3–6%, respectively) [30–33]. In some instances, allergy and autoimmunity could be the only clinical manifestation of IgA deficiency as we observed in two patients who had just an atopic (P5) or autoimmune (P33) presentation without any infections. It has been suggested that 25% of patients with IgA deficiency could be identified during an allergy evaluation [5].
The majority of patients with IGAD also have deficiency of secretory IgA [5, 34]. Considering the blocking role of secretory IgA in mucosal surfaces, in an IgA deficiency state, aeroallergens and food antigens may pass through this barrier at the mucosal interface of respiratory and gastrointestinal tracts, respectively [5, 29, 35]. This justifies the higher association of allergies and infections among these patients. Measurement of serum IgA should be considered not only in patients with recurrent infections but also in the case of allergic and autoimmune diseases.
In the present study, patients were classified into group 1 and group 2 based on existence or absence of concomitant immune defects, respectively. Patients in group 1 who had associated immune defects showed more severe and frequent infections and chronic lung complications compared to group 2. These findings are supported by previous studies that showed patients with IgA deficiency who have an additional deficiency of one or more IgG subclasses or impaired antibody responses are at risk of more severe and frequent infections [14, 17, 36–39].
Given the development of bronchiectasis in four of 11 patients with concomitant IGAD and specific antibody deficiency (SAD), we suggest that all symptomatic IGAD patients should be evaluated for associated SAD. We noticed a reduced frequency of infections after introduction of prophylactic IVIG in bronchiectatic IGAD patients with associated SAD. Although the replacement of IVIG is controversial in isolated IGAD, it is recommended in symptomatic IGAD patients who have SAD as well.
In group 2 patients, a compensatory increased level of serum IgM was found. Lack of severe infections in these patients may be attributed partly to this increase in secretory IgM.
In summary, we have shown that subclassification of IgA-deficient patients regarding the existence of associated immune defects is useful in terms of morbidity and planning for IVIG replacement. IgA-deficient patients with concomitant immune defects such as defects in specific antibody production have higher rates of recurrent infections and bronchiectasis, which necessitates more sophisticated care.
References
Hammarstrom L, Vorechovsky I, Webster D. Selective IgA deficiency (SIgAD) and common variable immunodeficiency (CVID). Clin Exp Immunol. 2000;120(2):225–31. doi:10.1046/j.1365-2249.2000.01131.x.
Bonilla FA, Bernstein IL, Khan DA, et al. Practice parameter for the diagnosis and management of primary immunodeficiency. Ann Allergy Asthma Immunol. 2005;94(5):S1–63.
Conley ME, Notarangelo LD, Etzioni A. Diagnostic criteria for primary immunodeficiencies. Representing PAGID (Pan-American Group for Immunodeficiency) and ESID (European Society for Immunodeficiencies). Clin Immunol. 1999;93(3):190–7. doi:10.1006/clim.1999.4799.
al-Attas RA, Rahi AH. Primary antibody deficiency in Arabs: first report from eastern Saudi Arabia. J Clin Immunol. 1998;18(5):368–71. doi:10.1023/A:1023247117133.
Cunningham-Rundles C. Physiology of IgA and IgA deficiency. J Clin Immunol. 2001;21(5):303–9. doi:10.1023/A:1012241117984.
Kanoh T, Mizumoto T, Yasuda N, et al. Selective IgA deficiency in Japanese blood donors: frequency and statistical analysis. Vox Sang. 1986;50(2):81–6.
Schaffer FM, Monteiro RC, Volanakis JE, Cooper MD. IgA deficiency. Immunodefic Rev. 1991;3(1):15–44.
Burrows PD, Cooper MD. IgA deficiency. Adv Immunol. 1997;65:245–76. doi:10.1016/S0065-2776(08)60744-0.
Hanson LA, Bjorkander J, Carlsson B, Roberton D, Soderstrom T. The heterogeneity of IgA deficiency. J Clin Immunol. 1988;8(3):159–62. doi:10.1007/BF00917561.
Burgio GR, Duse M, Monafo V, Ascione A, Nespoli L. Selective IgA deficiency: clinical and immunological evaluation of 50 pediatric patients. Eur J Pediatr. 1980;133(2):101–6. doi:10.1007/BF00441577.
Crabbe PA, Heremans JF. The significance of local IgA in the physiology of the intestinal mucosa. Folia Med Neerl. 1969;12(3):100–6.
Heneghan MA, Stevens FM, Cryan EM, Warner RH, McCarthy CF. Celiac sprue and immunodeficiency states: a 25-year review. J Clin Gastroenterol. 1997;25(2):421–5. doi:10.1097/00004836-199709000-00004.
Sloper KS, Brook CG, Kingston D, Pearson JR, Shiner M. Eczema and atopy in early childhood: low IgA plasma cell counts in the jejunal mucosa. Arch Dis Child. 1981;56(12):939–42.
Edwards E, Razvi S, Cunningham-Rundles C. IgA deficiency: clinical correlates and responses to pneumococcal vaccine. Clin Immunol. 2004;111(1):93–7. doi:10.1016/j.clim.2003.12.005.
Strober W, Sneller MC. IgA deficiency. Ann Allergy. 1991;66(5):363–75.
Wernette CM, Frasch CE, Madore D, et al. Enzyme-linked immunosorbent assay for quantitation of human antibodies to pneumococcal polysaccharides. Clin Diagn Lab Immunol. 2003;10(4):514–9. doi:10.1128/CDLI.10.4.514-519.2003.
Vendrell M, de Gracia J, Rodrigo MJ, et al. Antibody production deficiency with normal IgG levels in bronchiectasis of unknown etiology. Chest 2005;127(1):197–204. doi:10.1378/chest.127.1.197.
Standardization of spirometry-1987 update. Statement of the American Thoracic Society. Am Rev Respir Dis. 1987;136(5):1285–98.
Aghamohammadi A, Mohammadi J, Parvaneh N, Rezaei N, Moin M, Espanol T, et al. Progression of selective IgA deficiency to common variable immunodeficiency. Int Arch Allergy Immunol 2008;147(2):87–92. doi:10.1159/000135694.
Schroeder HW Jr, Zhu ZB, March RE, et al. Susceptibility locus for IgA deficiency and common variable immunodeficiency in the HLA-DR3, -B8, -A1 haplotypes. Mol Med. 1998;4(2):72–86.
Castigli E, Wilson SA, Garibyan L, et al. TACI is mutant in common variable immunodeficiency and IgA deficiency. Nat Genet 2005;37(8):829–34. doi:10.1038/ng1601.
Salzer U, Chapel HM, Webster AD, et al. Mutations in TNFRSF13B encoding TACI are associated with common variable immunodeficiency in humans. Nat Genet. 2005;37(8):820–8. doi:10.1038/ng1600.
Hammarström LSC. Genetic approach to common variable immunodeficiency and IgA deficiency. In: Ochs HDSC, Puck JM, editors. Primary immunodeficiency diseases: a molecular and genetic approach. 2nd ed. New York: Oxford University Press; 2007. p. 313–25.
Rezaei N, Aghamohammadi A, Moin M, Pourpak Z, Movahedi M, Gharagozlou M, et al. Frequency and clinical manifestations of patients with primary immunodeficiency disorders in Iran: update from the Iranian Primary Immunodeficiency Registry. J Clin Immunol. 2006;26(6):519–32. doi:10.1007/s10875-006-9047-x.
Saghafi S, Pourpak Z, Aghamohammadi A, Pourfathollah AA, Samadian A, Farghadan M, et al. Selective immunoglobulin a deficiency in Iranian blood donors; prevalence, laboratory and clinical findings. Iran J Allergy Asthma Immunol. 2008;7(3):157–62.
Ozkan H, Atlihan F, Genel F, Targan S, Gunvar T. IgA and/or IgG subclass deficiency in children with recurrent respiratory infections and its relationship with chronic pulmonary damage. J Investig Allergol Clin Immunol. 2005;15(1):69–74.
Stead A, Douglas JG, Broadfoot CJ, Kaminski ER, Herriot R. Humoral immunity and bronchiectasis. Clin Exp Immunol. 2002;130(2):325–30. doi:10.1046/j.1365-2249.2002.01974.x.
Tabatabaie P, Aghamohammadi A, Mamishi S, Isaeian A, Heidari G, Abdollahzade S, MirSaeid Ghazi B, Yeganeh M, Cheraghi T, Abolhasani H, Saghafi S, Alizadeh H, Anaraki MR, et al. Evaluation of humoral immune function in patients with bronchiectasis. Iran J Allergy Asthma Immunol. 2008;7(2):69–77.
Stiehm RE. The four most common pediatric immunodeficiencies. Adv Exp Med Biol. 2007;601:15–26.
Golshan M, Mohamad-Zadeh Z, Zahedi-Nejad N, Rostam-Poor B. Prevalence of asthma and related symptoms in primary school children of Isfahan, Iran, in 1998. Asian Pac J Allergy Immunol. 2001;19(3):163–70.
Golshan M, Mohammad-Zadeh Z, Khanlar-Pour A, Iran-Pour R. Prevalence of asthma and related symptoms in junior high school children in Isfahan, Iran. Monaldi Arch Chest Dis. 2002;57(1):19–24.
Miri S, Farid R, Akbari H, Amin R. Prevalence of allergic rhinitis and nasal smear eosinophilia in 11- to 15 yr-old children in Shiraz. Pediatr Allergy Immunol. 2006;17(7):519–23. doi:10.1111/j.1399-3038.2006.00424.x.
Mirsaid Ghazi B, Imamzadehgan R, Aghamohammadi A, Darakhshan Davari R, Rezaei N. Frequency of allergic rhinitis in school-age children (7–18 Years) in Tehran. Iran J Allergy Asthma Immunol. 2003;2(4):181–4.
Ammann AJ, Hong R. Selective IgA deficiency: presentation of 30 cases and a review of the literature. Medicine 1971;60:223–36. doi:10.1097/00005792-197105000-00004.
Woof JM, Kerr MA. The function of immunoglobulin A in immunity. J Pathol. 2006;208(2):270–82. doi:10.1002/path.1877.
Bjorkander J, Bake B, Oxelius VA, Hanson LA. Impaired lung function in patients with IgA deficiency and low levels of IgG2 or IgG3. N Engl J Med. 1985;313(12):720–4.
Bossuyt X, Moens L, Van Hoeyveld E, et al. Coexistence of (partial) immune defects and risk of recurrent respiratory infections. Clin Chem. 2007;53(1):124–30. doi:10.1373/clinchem.2007.075861.
French MA, Denis KA, Dawkins R, Peter JB. Severity of infections in IgA deficiency: correlation with decreased serum antibodies to pneumococcal polysaccharides and decreased serum IgG2 and/or IgG4. Clin Exp Immunol. 1995;100(1):47–53.
Oxelius VA, Laurell AB, Lindquist B, et al. IgG subclasses in selective IgA deficiency: importance of IgG2-IgA deficiency. N Engl J Med. 1981;304(24):1476–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aghamohammadi, A., Cheraghi, T., Gharagozlou, M. et al. IgA Deficiency: Correlation Between Clinical and Immunological Phenotypes. J Clin Immunol 29, 130–136 (2009). https://doi.org/10.1007/s10875-008-9229-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-008-9229-9