Abstract
This study examined what is measured by adolescents’, mothers’, and fathers’ reports of adolescents’ adherence to the type 1 diabetes regimen and how such reports relate to HbA1c and daily blood glucose. Two-hundred fifty-two adolescents (M age = 12.49 at baseline), mothers, and 188 fathers completed an adapted Self-Care Inventory (LaGreca et al. in Child Health Care 19(3):132–139, 1990) every 6 months for 2.5 years, HbA1c was gathered from medical records, and daily number of blood glucose tests (BGT) and blood glucose mean (BGM) were obtained from glucose meters at one time point. A multitrait-multimethod approach decomposing adherence indicated that fathers’ reports reflected a stable perception across time, mothers’ reports a shared view within the family that varied with HbA1c across time, and adolescents’ reports a unique view. Fathers’ and mothers’ reports were related to HbA1c; adolescents’ reports were not, but were uniquely associated with BGT. Family members’ adherence reports capture different information across time, with implications for measuring adherence and for family processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adherence to the diabetes regimen is an important predictor of adolescent metabolic control and is crucial for maintaining health and preventing diabetes complications (Hood et al., 2009). Adherence involves a number of daily behaviors, including BGT, administering insulin, and calculating insulin dosages, all designed to keep blood glucose in a near-normal range (ADA, 2015). Adolescent adherence is frequently assessed by using adolescents’ or parents’ (typically mothers’) reports of adherence, with the associations among such reporters ranging from modest (Armstrong et al., 2011; Lewin et al., 2009) to high (DirecNet, 2005; Miller & Drotar, 2003). However, adolescents spend increasing amounts of time away from their parents’ presence where adherence behaviors may not be observable (Larson & Richards, 1991). Thus, adolescents, mothers, and fathers may have different perspectives regarding adherence behaviors across adolescence, perspectives that may relate more or less well to objective metrics of adherence (i.e., BGT) and metabolic control (e.g., HbA1c and BGM). Little is known, however, about what we are measuring when we assess adolescents’ and parents’ views of adolescents’ adherence across time and how they may differentially relate to HbA1c, BGT, and BGM. The present study examined what is captured when we measure multi-informant reports of adolescents’ adherence to the diabetes regimen, how reports relate to each other and to HbA1c across six time points during adolescence, as well as how these reports relate to daily BGT and BGM at one point in time.
A mixed picture emerges regarding the strength of association among family members’ reports of adolescent adherence. During preadolescence (ages 9–11), Armstrong et al. (2011) found modest associations (r = 0.31, p < 0.01) among preadolescent and parent reports on the Self-Care Inventory (SCI; LaGreca et al., 1990). Somewhat stronger associations (r’s of 0.47–0.63) have been found between mother and teen reports during mid- to late-adolescence (DirecNet Study Group, 2005; Lewin et al., 2009; Miller & Drotar, 2003) on the SCI and Diabetes Self-Management Profile (DSMP). Adolescents’ and parents’ reports may become more similar as adolescents gain a more coherent view of their illness across time (Fortenberry et al., 2014). These correlations amongst reporters suggest that in addition to considerable overlap in perceptions of adherence, adolescents and parents may also contribute unique information. For example, adolescents’ and their parents’ reports may be based on different information with adolescents having more access than their parents to the daily behaviors (eating, BGT) that make up adherence.
To address these differing perspectives among adolescents and parents, researchers have frequently combined measures of adherence (e.g., global self-report and 24-recall diary) from multiple reporters (e.g., mother and adolescent) to obtain one latent indicator of adherence reflecting variance in adherence that is shared across reporters (Herge et al., 2012; Mackey et al., 2011). Such multi-informant assessments of adherence may strengthen the observed relationship between adherence and glycemic control. However, some have questioned whether such strategies, which treat the unique, or nonshared, perspectives of each informant as error, remove information about adherence that is important for understanding glycemic control and other diabetes outcomes (Holmbeck et al., 2002). As a whole, these studies raise issues as to what we are measuring when we assess adolescents’ and their parents’ reports of adherence across the period of adolescence (Holmbeck et al., 2002) and how such reports relate to objective metrics of adherence behaviors and metabolic control such as HbA1c, BGM, and BGT.
In the present study, we adopt the multitrait multimethod (MTMM) approach to explore what we are measuring when we assess adolescents’ and parents’ reports of adherence across adolescence. MTMM allows for an examination of how multi-informants’ adherence reports vary across time. We included HbA1c as part of the MTMM model to link variation in adherence to HbA1c, thereby decomposing variance in adherence to portions consistent with metabolic control, a frequently used marker of how well diabetes is medically managed. Linking adherence behaviors to HbA1c is important as HbA1c is commonly used in clinic settings to evaluate the adequacy of the current treatment regimen and may be used by families to evaluate how well the adolescent is following the treatment regimen. The MTMM approach is specifically designed to address and evaluate construct validity issues (Campbell & Fiske, 1959). Specifically, MTMM methods use multiple reporters and multiple concepts to identify convergent validity (the extent to which the construct of adherence has evident and consistent measurement) and discriminant validity (the extent to which the different reporters indicate unique measurement of adherence).
Through Confirmatory Factor Analysis (Joreskog, 1978; Widaman, 1985), our application of MTMM (see Fig. 1) separates variation in adherence and HbA1c into three components: source (i.e., representing that which is stable across time), time (i.e., representing that which is in common at a particular time point across measures, but changing across time), and what is unique (i.e., representing that which is not captured by source or time, typically thought of as error variance). Representing source, the latent constructs of each source (adolescent, mother, father) across time capture consistent reporter effects. As described below, we also included HbA1c as a source variable given its importance in marking how well diabetes is medically controlled. Representing time, the latent constructs at each time point are shared among sources at that specific point in time, representing what is common across reporters of adherence and consistent with HbA1c at that time point.
As HbA1c is included in these MTMM models, we can also address the extent to which reporters’ views of adherence are related to HbA1c across time. Associations among reporters’ views and between reporters’ views and HbA1c may differ for several reasons. Mothers, fathers, and adolescents play different roles in the management of diabetes, and may utilize different information as they form perceptions of adherence. Adolescents may not fully understand what HbA1c means (Patino-Fernandez et al., 2009). Mothers are often more involved in and aware of the day-to-day tasks of diabetes management than are fathers (Berg et al., 2008), and there is reason to believe that fathers utilize adolescents’ HbA1c as a way to gauge their involvement (Hilliard et al., 2011a, b; Sood et al., 2012). As a result, fathers’ reports of adherence may be more linked to HbA1c (Auslander et al., 1993), while mothers and adolescents may utilize information from daily management activities in addition to HbA1c. Mothers and adolescents may also differ from each other in the extent to which they are aware of different daily adherence behaviors. As adolescents spend increasing time away from parents (Larson & Richards, 1991), they have information about the full range of their day-to-day diabetes management activities that may not be available to mothers or fathers (Osborn et al., 2013).
Although not included in the MTMM models described above, there has also been great interest in understanding links between adherence reports and daily BGM and frequency of BGT (Guilfoyle et al., 2011; Kichler et al., 2012), with adolescents, and perhaps mothers, being more “in the know” about these daily metrics than fathers. Adolescents’ reports of their adherence may be uniquely associated with daily frequency of BGT and BGM compared to mothers’ or fathers’ reports of adherence, as increasing time spent from their home and parents gives adolescents unique knowledge of their testing behaviors. Adolescents may also use this knowledge of BGT and BGM as a gauge for assessing other aspects of their adherence behaviors, especially as frequency of BGT is linked to maintaining good HbA1c across adolescence and is a target for interventions to improve adherence (Hilliard et al., 2013).
The primary aim of the present study was to examine what we measure in multi-informant reports of adherence across time and how those reports relate to markers of metabolic control and daily BGT and BGM. Adolescents, mothers, and fathers reported on adolescents’ adherence across six time points during adolescence; HbA1c was gathered from medical records at each time point. A MTMM analysis was conducted to assess what portion of variability in adherence is consistent with the reporter across time (source), what portion is changing across time but consistent with other reporters and HbA1c (time), and what portion is unique to each reporter/source at each time point (unique).
We predicted that all reports of adherence would be a function of all three of these portions of variability, but in differing amounts and related to HbA1c in different ways. First, we predicted that fathers’ reports would be characterized by greater source (i.e., stability across time), due to their more distal role in daily diabetes management (Berg et al., 2008), whereas adolescents’ reports would be characterized by more uniqueness (separate from a stable view across time or shared view with parents) due to their greater access to their own behaviors that change across adolescence (King et al., 2014). Second, we predicted parents’ reports would be more related to HbA1c (both across and at each time point) than adolescents’ reports. Finally, we examined the association between the average daily BGM and frequency of BGT and multi-informant reports at one time point where glucometer downloads were collected. We predicted that adolescents’ reports would be most consistent with these daily markers of BG levels and testing behaviors, as these provide information on a daily basis that adolescents have greater access to than their parents.
Methods
Participants
Participants included 252 adolescents (M = 12.49 years, SD = 1.53, 53.6 % females) diagnosed with type 1 diabetes mellitus, their mothers, and 188 fathers, recruited from a university/private partnership clinic (85 %) and a community-based private practice (15 %), that followed similar treatment regimens and clinic procedures. Eligibility criteria included that adolescents were between 10 and 14 years of age, had diabetes more than 1 year (M = 4.13 years, SD = 2.98), and were able to read and write either English or Spanish. For each adolescent, one mother and one father were eligible to participate. At the beginning of the study, approximately half (50.8 %) of adolescents were on an insulin pump, with the remainder prescribed multiple daily injections (MDI); by the end of the study (approximately 2.5 years later), 63 % of adolescents were on an insulin pump. Mothers of adolescents on MDI reported that physicians recommended an average of 4.14 insulin injections (SD = 1.81, range = 0–10) and 5.53 BGT per day (SD = 1.70, range = 1–11).
Of the qualifying individuals approached, 66 % agreed to participate in the study. Reasons for refusal included distance of commute (18 %), too busy (21 %), not interested (30 %), uncomfortable with being studied (14 %), and the time commitment involved with participation (5 %). Comparisons of eligible adolescents who participated versus those who did not indicated that participants versus non-participants were older [12.5 vs. 11.6, t(367) = 6.2, p < 0.01, η2 = 0.10] but did not differ on gender, pump status, HbA1c or time since diagnosis (p values > 0.20). Families were largely Caucasian (91 %) and middle class, with most (63.5 %) reporting household incomes averaging $50,000 or more annually; 52.4 % of mothers and 44 % of fathers reported education levels of associate’s (2-year college) degrees or higher, and an average Hollingshead Index (1975) value of 41.19, indicating the sample was on average medium business, minor professional, or technical status. Eighty-four percent of participating mothers and 95 percent of participating fathers reported being married.
Procedure
This study was approved by the appropriate Institutional Review Board. Adolescents provided written assent and mothers and fathers provided written informed consent and parental permission.
Participants were recruited for the study at their diabetes clinic and received a packet of questionnaires and consent/assent forms that were to be completed individually and returned at a later laboratory appointment. For questionnaires completed at home, reporters were given separate packets and instructed to complete the questionnaires separately; clarifications were to be directed to investigators rather than family members. Families completed assessments every 6 months for a period of 2½ years. HbA1c was gathered from medical records. Across all 6 time points, the HbA1c was assessed an average of 10.37 days (SD = 14.84) before adolescents’ and mothers’ adherence reports and 9.46 days (SD = 27.13) before fathers’ adherence reports. At the second assessment only (Time 2) adolescents’ glucometer readings were obtained.
A total of 215 adolescents, 214 mothers, and 170 fathers provided data at Time 2. At Time 3 (approximately 1 year after the first assessment), 194 adolescents, 194 mothers, and 140 fathers provided data; at Time 4 (M time since Time 3 = 5.69 months), 183 adolescents, 180 mothers, and 138 fathers provided data; at Time 5 (M time since Time 4 = 5.13 months), 186 adolescents, 184 mothers, and 138 fathers provided data; at Time 6 (M time since Time 5 = 6.14 months), 198 adolescents, 196 mothers, and 148 fathers provided data (see Wiebe et al., 2014 for details about the sample at each time point). There were no significant differences in age, gender, or adherence at the first time point between families who did and did not participate at each time point. Reasons for withdrawing from the study included changes in family circumstances (19 %), including the adolescent no longer living with the mother/deaths in the family, being too busy (12 %), and study demands (12 %). Some families skipped time points (e.g., did not participate at Time 3 but returned to participate at Time 4). Reasons for “skipping” were not collected.
Measures
Adherence
Adherence to various aspects of the diabetes regimen over the preceding month was assessed with a 16-item adapted version of the Self-Care Inventory (LaGreca et al., 1990). The adaptations, which were made after consultation with a certified diabetes educator and a person with diabetes, involved adding two items (i.e., “How well have you followed recommendations for counting carbohydrates?” and “How well have you followed recommendations for calculating insulin doses based on carbohydrates in meals and snacks?”) and updating the wording of existing items to capture current treatment standards (e.g., “How well have you followed recommendations for checking blood glucose with monitor?”). Adolescents, mothers, and fathers responded to items concerning adolescents’ adherence behaviors on a scale from 1 (never did it) to 5 (always did it as recommended without fail). Average scores across items were analyzed. Across time points and reporters, α ≥ 0.86.
Daily blood glucose tests and BG means
For 14 consecutive days at Time 2, adolescents monitored daily blood glucose using a glucometer provided by researchers, resulting in date- and time-stamped records. Glucometers were returned at the end of the 14 days, after the Time 2 adherence measures were collected. A total of 207 adolescents provided diary data at this time point. Twenty-seven adolescents did not provide usable daily blood glucose readings, and thus were dropped from analyses involving BGT and BGM. These 27 participants did not differ from the remaining 180 on measures of adherence (p > 0.65) nor HbA1c (p > 0.14). Reasons for missing data included glucometer not returned (n = 6), experimenter failure to issue a meter (n = 6), software malfunction (n = 5), declined the use of our meter and/or failed to provide readings from their own meter (n = 8), and unknown (n = 2). Tests that occurred within 15 min of one another were deleted, with the later of the proximate readings retained. This procedure arose from consultations with pediatric endocrinologists, who indicated that repeated glucose tests likely reflected adolescents’ efforts to confirm the initial reading, as measurement can become increasingly inaccurate at abnormally high or low glucose levels (Saudek et al., 2006). Daily BGM was calculated by averaging across the adolescent’s glucose meter reading each day (average BGM of 206.25 (SD = 57.06), which is above the 180 mg/dL level considered hyperglycemic, American Diabetes Association, 2015). Very few of the daily blood glucose values represented low values (i.e., only 1.95 % of the daily average blood glucose levels were below 80). Thus, when interpreting daily blood glucose averages, higher readings are interpreted as indicating poorer management. Frequency of Daily BGT were calculated by summing up the number of tests each day. Adolescents completed an average of 4.34 BGT each day (SD = 1.88).
Metabolic control
As part of the routine clinic visit, adolescents’ HbA1c levels were obtained (M = 8.31, SD = 1.4, range = 4.9–13.9). HbA1c reflects average blood glucose levels over the preceding 2–3 months and is the current standard to index achievement of diabetes treatment goals (higher levels indicate poorer metabolic control). At all clinics, clinic staff obtained adolescents’ HbA1c using the Bayer DCA2000.
Analytic strategy
Our initial analyses were conducted using Structural Equation Modeling in Mplus 7.11. We used Full Maximum Likelihood to account for missing data. Our follow-up analyses regarding number of BGT were conducted in SPSS using available data at Time 2 as this was the only time that BGT were collected. In all cases, significance was reported by investigating if the 95 % confidence interval did not include 0 or the equivalent hypothesis test at alpha = 0.05, two tailed. We now describe the Structural Equation Model in detail.
We tested a MTMM structure where variation in each measure was a function of one of four source factors unchanging through time (mother-reported adherence, father-reported adherence, adolescent-reported adherence, HbA1c) and a function of one of six time points, changing over time (which we will call time points). Source factors were allowed to freely correlate and time points were also allowed to correlate (known as a Correlated Trait Correlated Methods or CTCM model; see Widaman, 1985). Consistent with MTMM architecture, the source factors and the time factors were not allowed to correlate with each other. Error variances for each outcome were uncorrelated. This model is illustrated in Fig. 1.
The CTCM model is a measurement model that has several advantages for understanding the relationships of the various reports of adherence to each other and to HbA1c. Each measure at each point in time is allowed to load onto two latent factors simultaneously and these two latent factors must be uncorrelated. Thus, it decomposes each measure of adherence and HbA1c into a portion that is stable across time akin to individual difference levels (i.e., the source factors), a portion that is associated with the other reports of adherence and HbA1c at that particular time point (i.e., the time factors), and a portion that is unique or not shared (i.e., the error variance) that captures unique variations that are not associated with time or source.
The total variation for a given measure at a specific point in time is the sum of these three sources of variation (source, time, unique). From the standardized results, the proportion of variation can be taken from the squared loadings. In standardized metric, these three portions of variance sum to one. For example, for the measure of adolescent-reported adherence at Time 1, the total variation is:
From this, we can observe what portion of variation in an informant’s view is a function of stable individual differences (i.e., source factor), what portion is changing with the other indicators of diabetes management together through time (i.e., time factor), and what portion is unrelated or unique (i.e., unique factor, what is left over in the error variance). The source factors (adolescent, mother, father, HbA1c) indicate what is stable about the reporters’ view of adherence across time. HbA1c is included as a source as it captures the important link between variation in adherence and HbA1c. This approach is mathematically similar to the approach of including HbA1c as an outcome, but better reflects our circumstance where adherence reports were not temporally prior to HbA1c measurement. Further, its inclusion provided an interpretable solution, reducing the problem frequently found with MTMM models of identifying a stable and interpretable solution (Mash & Bailey, 1991). The time point factors (Time 1–Time 6) are a function of all four measures at a specific time and thus represent how adherence reports and HbA1c relate to each other at a given time point. Thus, we can interpret the loadings onto the time point factors (one at each time point) as the extent to which a given adherence reporter or HbA1c is consistent with the other reporters at that time.
Finally, the extent to which the source factors are correlated with one another indicates that the reporters share perspectives across time and/or share variance with HbA1c. For example, if the mother-report adherence source factor correlates with the HbA1c source factor, this indicates that the stable portion of mothers’ adherence report across time relates to the stable portion of HbA1c across time.
Results
Source, time, and uniqueness in reports of adherence
The Confirmatory Factor Model fit was good, Chi-sq (207df) = 287.973, p < 0.001, CFI = 0.972, RMSEA 90 % CI (0.028 < 0.039 < 0.050), with no values out of range (see Marsh & Bailey, 1991). Table 1 contains the standardized loadings with 95 % confidence intervals. The HbA1c measures loaded most strongly on source and time, with the negative time loadings reflecting that higher HbA1c was associated with lower adherence ratings by all reporters. The loadings for father indicate that fathers’ reports of adherence had high loadings for source (range 0.65–0.86), moderate loadings for time (range 0.23–0.48) and for uniqueness (range 0.45–0.62). All loadings may be directly compared, illustrating when a given report of adherence is more a function of source, time, or uniqueness. For example, from Table 1, fathers’ Time 1 source loading was 0.86 with a lower limit of 0.80 and upper limit of 0.93. Fathers’ time loading at Time 1 is 0.23, which lies outside of the confidence interval for source at Time 1, indicating that fathers’ adherence reports at Time 1 were more captured by source than time. Fathers’ uniqueness loading was 0.45, which also lies outside of the source confidence interval, and the confidence interval for time (which ranged from 0.06 to 0.39). This means that at this time point, fathers’ adherence reports were more a function of source, a stable time-invariant report of adherence, than time or uniqueness. Fathers’ source loadings were larger than time and uniqueness at all time points. Similarly, mothers’ reports of adherence demonstrated high loadings for source (range 0.61–0.76), moderate loadings for time that were somewhat higher than fathers’ (range 0.43–0.64) and moderate loadings for uniqueness (range 0.39–0.58). Adolescents, however, had somewhat lower loadings for source (0.50–0.78), with loadings for time intermediate to those of parents and increasing across the six time points (moving from 0.28 at Time 1 to 0.62 at Time 6) and much higher loadings for uniqueness (range 0.53–0.82) than parents. These higher loadings for uniqueness for adolescents were especially apparent at Time 1 in that the confidence interval of the unique loadings for the adolescent (LL = 0.75 to UL = 0.89) exclude the corresponding source (0.50) and time point loadings (0.28).
We interpret these results to reflect that fathers’ views of adherence were mostly captured by source indicating a stable view of adherence that was less influenced by changes across time. Mothers’ views were captured more by time reflecting views that were shared among reporters and HbA1c. Adolescents’ views were more guided by unique factors that were not captured either by source (i.e., their own stable views of adherence) or time.
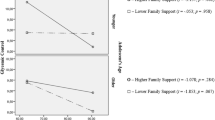
Figures 2a–c show the decompositions of each measure at each time point into the three sources of variance: source (stable across time), time point (shared with other reporters and HbA1c at a particular time point), and uniqueness. Consistent with the loadings mentioned above, fathers’ reports were mainly captured by source (Fig. 2a) and mothers’ by both source and time (Fig. 2b). Adolescents’ adherence reports (Fig. 2c) were increasingly captured by time reflecting that their reports were increasingly associated with parents’ reports and HbA1c over time. This is also captured in the loadings shown in Table 1. That is, the confidence intervals of the first three time point loadings for adolescent exclude the values of the last three with the exception of the comparison between the third and the fourth time points. Correspondingly, the proportion of unique variance for adolescents’ reports of adherence was larger than for mothers’ and fathers’ reports and for HbA1c, but declined across time. Notably, these large unique loadings could indicate meaningful variation in adherence sensitive to other sources of diabetes management, measurement error, or some combination of the two.
Relationship among adherence reports and HbA1c
Table 2 contains the correlations among the source factors. Significant associations were found among all reporters, with the association between mothers’ and fathers’ reports (r = 0.54) somewhat larger than between mothers’ and adolescents’ (r = 0.48) or fathers’ and adolescents’ (r = 0.36). As one would expect, the source factors for adherence (i.e., reporters) correlate larger with each other than with the HbA1c source factor. Notably, only mothers’ and fathers’ source factors correlated with the HbA1c source factor (r = −0.28 and −0.29 respectively). For adolescents, their source factor did not correlate with HbA1c (i.e., zero is contained within the confidence interval), suggesting that the stable portion of adolescents’ reports of adherence is linked with something other than HbA1c.
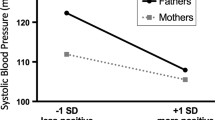
Reports of adherence associated with daily BGT and BGM
In order to explore why adolescents’ reports of adherence were less reflective of HbA1c than mothers’ or fathers’ reports, we examined whether adolescents’ reports were associated with their daily number of BGT or BGM, daily metrics of adherence and metabolic control. Correlations were found among all informant reports of adherence and BGT and BGM (see Table 3), indicating that higher adolescents’, mothers’, and fathers’ reports of adherence occurred when BGT were more frequent and BGM was lower. To understand the unique association between adherence reports and these daily metrics, two multiple regressions were performed with adolescents’, mothers’, and fathers’ reports of adherence at Time 2 as the independent variables predicting the average BGM and number of BGT over the 14-day period. For BGM, only mothers’ reports were uniquely associated with daily BGM (β = −0.22, t = −2.42, p < 0.01), with adolescents’ (p > 0.22) and fathers’ (p > 0.29) reports not uniquely associated with daily BGM. For BGT, only adolescents’ reports of adherence were significantly associated with the number of daily BGT, with better adherence reported when a greater number of tests occurred (β = 0.22, t = 2.42, p < 0.01). Neither mothers’ (p > 0.10) nor fathers’ reports of adherence (p > 0.37) were associated with number of BGT recorded on glucometers.
Discussion
The results indicate that adolescents’, mothers’, and fathers’ reports of adherence across time provide somewhat different information. Fathers’ views of adherence across time were represented by a fairly stable or unchanging view of adherence, whereas mothers’ views were represented by shared views of adherence with other reporters and HbA1c at each time point. Thus, mothers’ views may potentially be taking in the entire picture of diabetes management, including indices of glycemic control across time. Adolescents’ views were represented most by uniqueness and least by stable views or shared common views at each time point, although adolescents’ views became more shared in common with mothers’ and fathers’ views and HbA1c across time. Mothers’ and fathers’ views of adherence were associated with Hba1c, whereas adolescents’ views were not. Rather adolescents’ views of adherence were uniquely associated with their daily frequency of BGT.
The results hold important implications for how we measure adherence within a family system and how we conceptualize shared or unique perspectives across time. The current model parsed variance of adherence into three components (source, time, and uniqueness). A relatively common practice when assessing multiple reporters is to construct a latent variable or sum score across the various reporters implying that such a metric is a more reliable or less biased measure than any single reporter (Herge et al., 2012; Mackey et al., 2011). Specifically, the consistency in reporters is thought to capture truth, while the inconsistency in reporters is considered bias. Our results lie in contrast to this view, instead revealing how each reporter may base their reports of adolescent adherence to the diabetes regimen on different information. For example, adolescents’ reports, while being more unique, were related to a key marker of adherence, daily BGT, but were not related to HbA1c. In fact, adolescents’ reports were uniquely associated with BGT, suggesting that daily regimen behaviors that are enacted are key to their views of adherence. Fathers’ adherence reports were associated with HbA1c primarily through the source or non-changing portion of father’s adherence. This suggests that father’s reports were more characterized by a stable view of adherence across time, which is not updated by new HbA1c values as they occur over time. It is possible that fathers are not receiving these updates if they are not attending the healthcare visit. Fathers’ reports were, however, related to daily BGT and BGM indicating that such daily information is informative for their reports. Mothers’ reports seemed to fall in between reflecting changing levels of HbA1c that were captured through the time factor. Thus, mothers’ reports were more in sync with the HbA1c values at each time point and also shared with other family members’ reports of adherence. Mothers’ reports were also related to daily BGT and were uniquely associated with BGM indicating that for her the level of metabolic control may be key to her perspective of adherence. Taken together, each reporter captured different information across time.
From our perspective, the question is not “Who is the best reporter of adherence?”, but rather what information does each reporter provide about adherence across time. Diabetes adherence occurs daily and its success in facilitating better blood glucose control can be measured both in the short-term (e.g., BGM) and on a longer time scale (e.g., HbA1c). Our results suggest that adolescents,’ mothers’ and fathers’ reports reflect aspects of daily management (correlated with both BGM and BGT), but that only parents’ reports capture longer term aspects of blood glucose control such as HbA1c. Adolescents’ reports increasingly were shared with parents’ views and HbA1c over time (seen by the increasing portions of variance captured by the time factors). This increasingly shared view of adolescents and parents may reflect that adolescents are developing a greater awareness of the multiple adherence behaviors required for good diabetes management. Adolescents may also be developing a more coherent understanding of their illness (Fortenberry et al., 2014), one that acknowledges the role of HbA1c as a metric of diabetes management (Patino-Fernandez et al., 2009). The choice of whose report to use requires a nuanced understanding of what adherence reports reflect within the family system across time.
The finding that each family informant provided different information about adherence across time cautions researchers against using informants interchangeably and raises questions about the meaning of self-report measures of adolescent adherence. In particular, both father and (to a lesser extent) mother reports included a stable global perception about the adolescent’s level of adherence that was more closely linked to HbA1c, while adolescent reports were less linked to HbA1c. Such patterns could occur for a variety of reasons. HbA1c carries great meaning for families managing type 1 diabetes given its emphasis in clinic visits and its importance for the adolescent’s long term health (Auslander et al., 1993). It is possible that parents attend most closely to and accurately report on longer-term patterns in adherence behaviors that have the strongest influence on glycemic control. However, it is also possible that parental ratings of adherence are framed by their knowledge of the adolescent’s level of glycemic control, while adolescents’ ratings are based more directly on their recent behaviors. Behavioral diabetes researchers commonly measure adherence as an important predictor of glycemic control, but the latter scenario raises the possibility that adherence ratings—especially parental ratings—are also affected by HbA1c information. Research methods that allow one to disentangle these complex, bidirectional influences (e.g., objective measures of adherence; longitudinal studies) are necessary to understand accurately the role of self-reported adherence in glycemic control.
The present findings must be considered in the context of certain limitations. First, the sample consisted of largely Caucasian, intact families from middle to high socioeconomic backgrounds. It is possible that the pattern of associations found for reports of adherence could function differently in non-intact families than for the largely intact families included in this study. Findings may not generalize to racial and ethnic minorities or those of lower socioeconomic status. Second, the measure of adherence used in this study was a brief questionnaire. Future studies should include more extensive measures of adherence, such as parent and adolescent interviews. Despite the Self Care Inventory’s relation to these other assessment methods (such as the 24 h Recall Interview, Lewin et al., 2009), it is possible that more in-depth measures could provide additional information not captured by the SCI, illuminating a different pattern of findings. Third, adherence reports were gathered after HbA1c was tested, but before daily BGM and BGT. Future research is needed to ascertain how adherence reports change in response to receiving such metabolic control information. Further, we do not have information in this study as to whether all reporters were aware of this metabolic information nor whether they recalled such information accurately. At the current time, little attention is given in the field to the timing of adherence assessments in relation to HbA1c (especially as HbA1c is typically gathered from medical records), nor whether informants are accurately aware of metabolic control information. Careful attention to this timing may be important in understanding family members’ reports of adherence and the information they are using to make adherence judgments. Finally, BGT and BGM were only gathered at one point in time and future research is needed to understand adolescents’ and parents’ views of adherence as related to BGT and BGM across time.
In sum, family members provide differing perspectives of adolescent diabetes adherence that relate in important, yet different, ways to metrics of glycemic control. Family members’ differing perspectives may be a source of conflict, which could be problematic given that diabetes-related conflict escalates during adolescence and is related to poorer adherence and metabolic control (Hilliard et al., 2011a, b, 2013). The results may hold implications for family-based interventions that focus on improving communication among parents and adolescents (e.g., Wysocki et al., 2008). Such interventions may benefit from discussions regarding adherence behaviors as adolescents, mothers, and fathers come to a more shared perspective about the frequency of those behaviors. Such interventions could involve a regular family check-up (Dishion et al., 2003) where adolescents and parents use daily check-ins regarding BGT to calibrate their understanding of an important adherence behavior. Understanding that family members may differ in their judgments of adherence may assist families in the difficult task of managing diabetes across adolescence.
References
American Diabetes Association (2015). Treatment and care. http://www.diabetes.org/living-with-diabetes/treatment-and-care/?loc=lwd-slabnav. Accessed November 8, 2015.
Armstrong, B., Mackey, E. R., & Streisand, R. (2011). Parenting behavior, child functioning, and health behaviors in preadolescents with type 1 diabetes. Journal of Pediatric Psychology, 36, 1052–1061. doi:10.1093/jpepsy/jsr039
Auslander, W. F., Bubb, J., Rogge, M., & Santiago, J. V. (1993). Family stress and resources: Potential areas of intervention in children recently diagnosed with diabetes. Health and Social Work, 18, 101–113.
Berg, C. A., Butler, J. M., Osborn, P., King, G., Palmer, D., Butner, J., et al. (2008). The role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care, 31, 678–683.
Campbell, D. T., & Fiske, D. W. (1959). Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin, 56, 81–105.
Diabetes Research in Children Network (DirecNet) Study Group. (2005). Diabetes self-management profile for flexible insulin regimens: Cross-sectional and longitudinal analysis of psychometric properties in a pediatric sample. Diabetes Care, 28, 2034–2035.
Dishion, T. J., Nelson, S. E., & Kavanagh, K. (2003). The family check-up with high-risk young adolescents: Preventing early-onset substance use by parent monitoring. Behavior Therapy, 34, 553–571.
Fortenberry, K., Berg, C. A., King, P. S., Stump, T., Butler, J. M., Pham, P. K., et al. (2014). Longitudinal trajectories of illness perceptions among adolescents with type 1 diabetes. Journal of Pediatric Psychology, 39, 687–696.
Guilfoyle, S. M., Crimmins, N. A., & Hood, K. K. (2011). Blood glucose monitoring and glycemic control in adolescents with type 1 diabetes: Meter downloads versus self-report. Pediatric Diabetes, 12, 560–566.
Herge, W. M., Streisand, R., Chen, R., Holmes, C., Kumar, A., & Mackey, E. R. (2012). Family and youth factors associated with health beliefs and health outcomes in youth with type 1 diabetes. Journal of Pediatric Psychology, 37, 980–989.
Hilliard, M. E., Guilfoyle, S. M., Dolan, L. M., & Hood, K. K. (2011a). Prediction of adolescents’ glycemic control 1 year after diabetes-specific family conflict: The mediating role of blood glucose monitoring adherence. Archives of Pediatric Adolescent Medicine, 165, 624–629.
Hilliard, M. E., Rohan, J. M., Carle, A. C., Pendley, J. S., Delamater, A., & Drotar, D. (2011b). Fathers’ involvement in preadolescents’ diabetes adherence and glycemic control. Journal of Pediatric Psychology, 36, 911–922. doi:10.1093/jpepsy/jsr020
Hilliard, M. E., Wu, Y. P., Rausch, J., Dolan, L. M., & Hood, K. K. (2013). Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. Journal of Adolescent Health, 52, 28–34.
Holmbeck, G. N., Li, S. T., Schurman, J. V., Friedman, D., & Coakley, R. M. (2002). Collecting and managing multisource and multimethod data in studies of pediatric populations. Journal of Pediatric Psychology, 27, 5–18.
Hood, K. K., Peterson, C. M., Rohan, J. M., & Drotar, D. (2009). Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics. doi:10.1542/peds.2009-0207
Joreskog, K. G. (1978). Structural analysis of covariance and correlation matrices. Psychometrika, 43, 443–477.
Kichler, J. C., Kaugars, A. S., Maglio, K., & Alemzadeh, R. (2012). Exploratory analysis of the relationships among different methods of assessing adherence and glycemic control in youth with type 1 diabetes mellitus. Health Psychology, 31, 35–42.
King, P. S., Berg, C. A., Butner, J., Butler, J. M., & Wiebe, D. J. (2014). Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents’ adherence. Health Psychology, 33, 424–432.
LaGreca, A. M., Follansbee, D., & Skyler, J. S. (1990). Developmental and behavioral aspects of diabetes management in youngsters. Children’s Health Care, 19, 132–139.
Larson, R., & Richards, M. H. (1991). Daily companionship in late childhood and early adolescence: Changing developmental context. Child Development, 62, 284–300.
Lewin, A. B., LaGreca, A. M., Geffken, G. R., Williams, L. B., Duke, D. C., Storch, E. A., et al. (2009). Validity and reliaiblity of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The Self-Care Inventory (SCI). Journal of Pediatric Psychology, 34, 999–1007.
Mackey, E. R., Hilliard, M. E., Berger, S. H., Streisand, R., Chen, R., & Holmes, C. (2011). Individual and family strengths: An examination of the relation to disease management and metabolic control in youth with type 1 diabetes. Families, Systems, & Health, 29, 314–326.
Marsh, H. W., & Bailey, M. (1991). Confirmatory factor analyses of multitrait-multimethod data: A comparison of alternative models. Applied Psychological Measurement, 15, 47–70.
Miller, V. A., & Drotar, D. (2003). Discrepancies between mother and adolescent perceptions of diabetes-related decision-making autonomy and their relationship to diabetes-related conflict and adherence to treatment. Journal of Pediatric Psychology, 28, 265–274.
Osborn, P., Berg, C. A., Hughes, A. E., Pham, P., & Wiebe, D. J. (2013). What mom and dad don’t know can hurt you: Adolescent disclosure to and secrecy from parents about type 1 diabetes. Journal of Pediatric Psychology, 38, 141–150. doi:10.1093/jpepsy/jss102
Patino-Fernandez, A. M., Eidson, M., Sanchez, J., & Delamater, A. M. (2009). What do youth with type 1 diabetes know about the HbA1c test? Children’s Health Care, 38, 157–167.
Saudek, C. D., Derr, R. L., & Kalyani, R. R. (2006). Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. Journal of the American Medical Association, 295, 1688–1697. doi:10.1001/jama.295.14.1688
Sood, E. D., Pendley, J. S., Delamater, A. M., Rohan, J. M., Pulgaron, E. R., & Drotar, D. (2012). Mother-father informant discrepancies regarding diabetes management: Associations with diabetes-specific family conflict and glycemic control. Health Psychology, 31, 571–579.
Widaman, K. F. (1985). Hierarchically nested covariance structure models for multitrait-multimethod data. Applied Psychological Measurement, 9, 1–26.
Wiebe, D. J., Chow, C. M., Palmer, D. L., Butner, J., Butler, J. M., Osborn, P., et al. (2014). Developmental factors associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescence. Journal of Pediatric Psychology, 39, 532–541.
Wysocki, T., Harris, M. A., Buckloh, L. M., Mertlich, D., Lochrie, A. S., Taylor, A., et al. (2008). Randomized, controlled trial of behavioral family systems therapy for diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behavior Therapy, 39, 33–46.
Acknowledgments
The project was supported by R01DK063044 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health. We thank the families who participated, the staff of the Utah Diabetes Center and Michael Swinyard’s practice, as well as the additional members of the ADAPT team (David Donaldson, Rob Lindsay, Mary Murray, Mike Swinyard). We also thank Meagan Ramsey and Travis Wilshire for reviewing a previous draft of this paper.
Funding
The project was supported by R01DK063044 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Cynthia A. Berg, Jonathan E. Butner, Sara L. Turner, Amy Hughes Lansing, Pamela King, and Deborah J. Wiebe declare that they have no conflicts of interest.
Human and animal rights and Informed consent
All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Berg, C.A., Butner, J.E., Turner, S.L. et al. Adolescents’, mothers’, and fathers’ reports of adherence across adolescence and their relation to HbA1c and daily blood glucose. J Behav Med 39, 1009–1019 (2016). https://doi.org/10.1007/s10865-016-9771-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-016-9771-5