Abstract
Conditional cash transfer (CCT) and cognitive-behavioral treatments are evidence-based approaches to reduce stimulant use and sexual risk taking. We describe the adaptation and implementation of sequential behavioral interventions for Cambodian female entertainment and sex workers (FESW) who use amphetamine-type stimulants (ATS): (1) a 12-week CCT intervention; and (2) a 4-week cognitive-behavioral aftercare (AC) group. An ongoing cluster randomized stepped wedge trial in 10 Cambodian provinces is enrolling FESW with confirmed recent ATS use to examine the effectiveness of CCT + AC. In the first six provinces, 138 of the 183 eligible FESW (75 %) enrolled in CCT and completed a median of 25 (interquartile range 9–32) of the 36 urine screening visits. Of the 84 participants who were eligible for AC, 79 completed at least one session (94 %) and 57 completed three or more sessions (68 %). Culturally tailored behavioral interventions to reduce ATS use and optimize HIV prevention are feasible in resource-limited settings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the 1990s, Cambodia (officially, the Kingdom of Cambodia) was one of the most highly impacted countries in Southeast Asia by the HIV epidemic, coinciding with the country’s emergence from years of civil instability (Page et al., 2013; Saphonn et al., 2005, 2010). Comprehensive deployment of basic HIV prevention programs countrywide including condom use promotion, voluntary counseling and testing, and scaled up HIV treatment as prevention have contributed to large declines in HIV incidence and prevalence (Vun et al., 2014). Historically, female entertainment and sex workers (FESW) have been the group with the highest prevalence and incidence of HIV in Cambodia. In 2010, HIV prevalence estimates among direct or brothel-based female sex workers ranged from 13.9 to 17.4 % and from 3.6 to 9.8 % among indirect or entertainment-based workers (Couture et al., 2011; National Center for HIV/AIDS, Dermatology, and STDs, 2010). Sex work remains a high-risk trade in Cambodia where recent enforcement of an anti-trafficking law that included prosecution of condom possession created additional barriers to accessing HIV prevention and sexual health care services among FESW (Maher et al., 2015).
The use of amphetamine-type stimulants (ATS) is prevalent and has negative implications for HIV prevention. There are an estimated 19.3–54.8 million ATS users worldwide, and following cannabis it is the second most commonly used substance globally (United Nations Office on Drugs and Crime, 2015). Prevalence estimates for lifetime ATS use among Cambodian FESW were 42.5 % in 2007 and 30.1 % in 2009 with approximately one in four reporting ATS use in the past 3 months, 26.6 % in 2007 and 23.5 % in 2009 (Page et al., 2013). Prior research has documented that stimulant use is associated with engagement in condomless sex and greater rates of HIV seroconversion (Koblin et al., 2006; Ostrow et al., 2009; Plankey et al., 2007), but studies conducted to date have focused predominantly on men who have sex with men residing in industrialized countries. At the same time, there is emerging evidence that ATS use may be an important risk factor for HIV around the globe (Colfax et al., 2010).
Novel approaches are needed to target ATS use as a driver of the HIV epidemic with marginalized, underserved women such as FESW in Asia. Recent qualitative findings with FESW in Cambodia highlight that ATS may serve important occupational functions as a thnam kamlang (power drug) by assisting women with working longer hours and seeing more clients in the context of limited economic opportunities (Dixon et al., 2015; Maher et al., 2011). This may partially explain why ATS use is associated with greater odds of condomless sex and incident sexually transmitted infections in this population (Couture et al., 2011, 2012). The relevance of ATS use for engagement in condomless sex is further supported by similar qualitative findings with adolescent migrant girls in China and female sex workers in Vietnam (Ho et al., 2013; Zhang et al., 2015). Implementing evidence-based substance abuse interventions targeting ATS-using FESW could optimize HIV prevention in Southeast Asia and other resource-limited settings.
Conditional cash transfer (CCT) provides tangible rewards as positive reinforcement for performing behaviors relevant to health promotion (Fernald et al., 2008; Rasella et al., 2013). An extensive literature examining CCT as a substance abuse intervention, also referred to as contingency management, demonstrates that it is effective in reducing stimulant use (Prendergast et al., 2006). In addition to providing positive reinforcement for stimulant abstinence, cash payments delivered during CCT may also mitigate the effects of poverty as a key structural barrier to HIV prevention in resource-limited settings. This is supported in part by findings from a recent randomized controlled trial (RCT) in Malawi with never married, young women where CCT for school attendance and unconditional cash transfer achieved comparable reductions in herpes simplex virus type-2 and HIV prevalence versus no cash payments (Baird et al., 2012). Despite its possible benefits for decreasing stimulant use and optimizing HIV prevention, important questions remain regarding whether and how CCT can achieve long-term reductions in risk behaviors after the cash incentives end (Carrico et al., 2015).
Cognitive-behavioral interventions have the potential to augment the effectiveness of CCT by providing early recovery and relapse prevention skills to assist individuals with achieving sustained reductions in stimulant use and condomless sex. Based on the principles of relapse prevention (Carroll and Rawson, 2005), the Matrix Model is a 4-month, outpatient treatment for stimulant use disorders that includes individual cognitive-behavioral therapy (CBT), CBT skills groups, family education groups, and regular urine toxicology screening (Lee and Rawson, 2008; Rawson et al., 1995, 2002). A multi-site RCT in the United States observed that those receiving the Matrix Model were more engaged in treatment and had a greater number of urine samples that were negative for methamphetamine compared to treatment as usual (Rawson et al., 2004). There is also some evidence that a culturally tailored Matrix Model intervention with stimulant-using gay and bisexual men achieves greater decreases in condomless receptive anal sex during treatment and more pronounced reductions in methamphetamine use, compared to other behavioral interventions (Shoptaw et al., 2005, 2008). Further clinical research is needed to adapt the Matrix Model for resource-limited settings where it is often not feasible to deliver intensive outpatient substance abuse treatment (Becker and Kleinman, 2013).
Although a meta-analysis observed that delivering CCT with CBT yielded the best outcomes during treatment (Dutra et al., 2008), few RCTs have been conducted to date. It also remains unclear whether there are long-term benefits of this combined approach compared to CBT alone with stimulant users (Epstein et al., 2003; Rawson et al., 2006). Furthermore, relatively little is known about the sequential implementation of CCT and CBT interventions in resource-limited settings like Cambodia where formal substance abuse treamtent is often unavailable and structural factors are key determinants of ATS use (Dixon et al., 2015; Maher et al., 2011). The goal of this study was to document the adaptation and implementation of evidence-based behavioral interventions for ATS-using FESW in Cambodia. First, we describe the adaptation of a 12-week CCT intervention and 4-week cognitive-behavioral aftercare (AC) group based on the Matrix Model to meet the needs of FESW who use ATS. Then, we detail procedures employed to sequentially implement CCT + AC as part of an ongoing cluster randomized stepped wedge trial in 10 Cambodian provinces. Process data on enrollment as well as attendance of CCT urine screening visits and AC sessions from the first six provinces are also provided to index feasibility of these behavioral interventions with Cambodian FESW who use ATS.
Methods
Procedures
Adaptation of CCT and cognitive-behavioral AC was informed by the Assessment, Decision, Administration, Production, Topical experts, Integration, Training, and Testing (ADAPT-ITT) model for tailoring evidence-based HIV interventions for new target populations (Wingood & DiClemente ,2008). Cultural tailoring of CCT and AC proceeded in three distinct phases: development, training, and implementation. Consistent with the ADAPT-ITT model, the process of adaptation was iterative and the development phase was informed by qualitative feedback from FESW who use ATS, interviews with stakeholders such as service providers, and ongoing consultation with our non-governmental organization partners (FHI 360) who oversee the implementation of the SMARTGirl prevention program with this population (FHI 360, 2011). The protocol for the study was reviewed and approved by the National Ethics Committee for Health Research, Ministry of Health, Cambodia; the University of California, San Francisco; UNSW Australia; and FHI 360.
Outreach workers from non-governmental organization partners recruited eligible participants from SMARTGirl clubs, entertainment venues, and other locales where high-risk women are known to congregate or work. Eligible participants were Cambodian FESW who were: (1) biologically female; (2) ≥18 years of age; (3) reported ≥2 sexual partners or transactional sex within the last month; (4) able to understand spoken Khmer language; and (5) able to provide informed consent. Descriptive data on enrollment as well as attendance of CCT urine screening visits and AC group sessions were examined to index feasibility. Feasibility of recruitment was operationalized as an enrollment rate of 70 % or higher, an established standard in the literature (Crepaz et al., 2006). Feasibility of intervention delivery was operationalized as completing at least half of the 36 urine screening visits (i.e., >18 urine screening visits) and attending three-fourths of scheduled AC sessions (i.e., 3 of 4 sessions completed) on average.
Development
Assessment
included in-depth qualitative interviews with 30 FESW who reported using ATS. Participants were recruited using convenience sampling from five Cambodian provinces (i.e., Phnom Penh, Battambang, Banteay Meanchey, Siem Reap, and Kandal). Participants described possible barriers and facilitators to engagement in CCT as well as perceptions of potential AC components (Dixon et al. in press). A description of the detailed thematic analysis of these qualitative data is in progress, but some findings directly informed efforts to develop CCT and AC. With respect to CCT, participants highlighted that a $1 USD incentive would not be sufficient, particularly given the possibility of lost income when abstaining from ATS. Thus, the incentive was increased to $2 USD per urine sample and a weekly bonus was included to positively reinforce continuous abstinence from ATS. Participants also noted that transportation would be a key structural barrier to participating in CCT + AC, which prompted our team to provide transportation to CCT and AC visits. With respect to the content of AC, women were interested in participating in enjoyable group activities. However, some concerns about the feasibility of the proposed meditation and relaxation exercises were raised, which led our team to prioritize brief approaches that would be more easily accessible for this population.
Decision
processes in consultation with providers at FHI 360 at this early stage of adaptation were focused on finalizing the CCT protocol and identifying relevant exercises for the cognitive-behavioral AC group by reviewing treatment manuals for the Matrix Model (Center for Substance Abuse Treatment, 2006), Mindfulness-Based Relapse Prevention (Bowen & Chawla, 2011), and the World Health Organization’s Self Help Strategies for Substance Use (Word Health Organization, 2010). Because thrice weekly urine screening visits are required for biologically confirmed continuous abstinence from stimulants, we determined that CCT urine screening visits in each province should be conducted with two distinct schedules to maintain fidelity: (1) Monday, Wednesday, and Friday; and (2) Tuesday, Thursday, and Saturday. Relevant domains selected for AC content were: (1) enhancing social support for reducing stimulant use and its related harms; (2) providing cognitive-behavioral recovery skills; and (3) brief meditation and relaxation training. In consultation with FHI 360, we chose to deliver a 4-session AC group because this time-limited approach would increase the likelihood that the entire 16-week intervention could be implemented in Cambodia if CCT + AC ultimately proves to be effective.
Development of the cognitive-behavioral AC group protocol was informed by core elements the ADAPT-ITT model to achieve an initial draft of the treatment manual. Topical experts in CBT for stimulant use disorders, Drs. Rick Rawson and Steven Shoptaw, were consulted to assist with selecting Matrix Model cognitive-behavioral skills worksheets to tailor the intervention skills for this population (Center for Substance Abuse Treatment, 2006). Production entailed developing a comprehensive first draft of the manual that emphasized cognitive-behavioral processes relevant to early recovery and relapse prevention. At this stage, our team also focused on including culturally appropriate experiential group exercises (e.g., role plays) as well as meditation and relaxation training in the initial draft of the manual. The primary objectives of these components are to build group cohesion, facilitate observational learning, and assist participants with acquiring behavioral skills for managing triggers for ATS use.
Administration
was accomplished by completing cognitive interviewing with the first draft of the AC intervention manual where seven FESW who reported using ATS were asked to provide their interpretations of the intervention content and exercises. This provided important feedback regarding areas where further refinement of the presentation of cognitive-behavioral skills was necessary and helped to ensure cultural equivalency of the underlying cognitive-behavioral processes being targeted. Informed by this cognitive interviewing, integration entailed creating a second draft of the manual. This draft more adequately addressed key concepts (e.g., triggers) with culturally relevant terminology and there was an explicit focus on accommodating the relatively low literacy of the target population using pictorial representations where possible. The second draft of the manual was reviewed and edited by our team, which included Cambodian mental health professionals (EN and CS) to ensure cultural relevance while maintaining the core cognitive-behavioral skills. A third and final draft of the manual was created following the delivery of the AC groups in the first two provinces to clarify facilitation procedures for administering the sessions.
Training
The CCT staff training included a comprehensive overview of urine drug screening procedures such as sample collection, adulteration testing, and communicating results to participants. Staff members were provided with a general orientation to delivering low threshold, harm reduction services to substance users. This included role play exercises with scripted messages on how to communicate urine toxicology results. Staff were specifically instructed to deliver urine toxicology results that were positive for ATS (amphetamine or methamphetamine) in a factual, non-judgmental manner while encouraging participants to attend subsequent urine screening visits.
The AC groups were led by a master’s level Cambodian psychologist (EN) with expertise in CBT who supervised a co-facilitator with a bachelor’s degree in Psychology (PM). The co-facilitators completed all four of the AC groups sessions in one province with direct supervision from the Cambodian psychologist in order to be formally certified to deliver AC groups independently. The co-facilitators subsequently received a combination of direct observation and individual supervision sessions with the Cambodian psychologist to provide support for optimizing group process and delivery of the cognitive-behavioral skills.
Implementation
An ongoing cluster randomized stepped wedge trial is testing the effectiveness of the CCT + AC intervention that is being implemented sequentially in 10 Cambodian provinces with FESW who use ATS (www.clinicaltrials.gov; NCT01835574). To determine eligibility for CCT, participants completed a baseline assessment. Using the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), eligible participants were required to receive a score of four or higher (i.e., ≥4) on the ATS specific substance involvement subscale (Humeniuk et al., 2008), and provide a urine sample that was positive for ATS (amphetamine or methamphetamine). An ATS specific substance involvement score of four or higher was selected because it identifies women who are at least at moderate risk for a stimulant use disorder based on the ASSIST feedback card (Humeniuk et al., 2008). Among those enrolled in CCT, women who complete at least half of the 36 urine screening visits (i.e., ≥18) were eligible to participate in the AC group regardless of their urine test results.
CCT intervention
The CCT intervention included thrice weekly urine screening for 12 weeks (i.e., 36 possible urine screening visits). Participants were encouraged to attend urine screening visits at the study field site, but staff also conducted urine screening visits off site as needed to accommodate scheduling difficulties that were often related to sex work. At each urine screening visit, participants received $2 USD for providing a sample that was negative for ATS (amphetamine and methamphetamine). Each week where all three of urine samples were negative for ATS, participants received a cash bonus. This bonus was $2 USD in weeks 1–4, $4 USD in weeks 5–8, and $6 USD in weeks 9–12 to mitigate habituation to the CCT reward schedule. Cash incentives were provided to participants at each urine screening visit as an immediate, tangible reinforcement for ATS abstinence. This is consistent with prior research where more frequent receipt of cash incentives earned in CCT was associated with greater odds of abstinence at subsequent urine screening visits (Ling Murtaugh et al., 2013). Where participants provided a positive urine test for ATS, they did not receive the incentive for that visit or a cash bonus for that week. Urine testing results for each participant were systematically tracked on a CCT card that provided a visual representation of each urine screening visit where results were logged. Using the CCT card, the remaining possible incentive was reviewed with participants at each urine screening visit. Total possible reinforcement for ATS abstinence over the 12 weeks was $120 USD.
Cognitive-behavioral AC group
There were two main goals of the 4-session, cognitive-behavioral AC group. First, AC provided women with a supportive environment to discuss their experiences related to ATS use. In the AC group sessions, women can receive and provide social support for avoiding ATS use or reducing the harms that they experience related to ATS use. Social support is conceptualized as a key change process in AC for helping women avoid ATS use as well as to overcome feelings of guilt and shame related to being FESW who use ATS. Second, consistent with the cognitive-behavioral model, the AC group provided women with skills that are designed to change thoughts, feelings, and behaviors to more effectively manage triggers for ATS use.
Each AC group session includes four key components: (1) experiential group exercises; (2) didactic recovery skills training; (3) meditation and relaxation training; and (4) a “lucky draw” which is a form of CCT that provides positive reinforcement for group attendance. Group exercises were designed to facilitate cohesion and observational learning as well as provide opportunities for in vivo practice of skills that can assist with avoiding ATS use. Recovery skills training included cognitive-behavioral strategies to support early recovery and relapse prevention using worksheets for home practice. Because FESW did not receive any individual or group treatment during CCT, we chose to focus on delivering early recovery and relapse prevention skills that did not require experience with the cognitive-behavioral model. These activities were designed to raise awareness regarding internal and external triggers for ATS use as well as assist participants with examining ways to change thoughts, feelings, or behaviors to avoid ATS use. Meditation and relaxation training was delivered in each session to provide women an opportunity to practice techniques for managing negative emotions, cravings, and other internal triggers for ATS use.
A “lucky draw” occurred at the end of each AC group as positive reinforcement for attendance. Adapted from Petry’s prize-based incentive methodology for CCT (Olmstead et al., 2007), women drew one ticket from a prize bowl following each AC group session. With these tickets, participants received a reward in the form of a cash prize ($10, $5, or $2) or applause with positive affirmations from the group. For each 4-session AC group, prize bowls with 110 total tickets for the “lucky draw” included one $10 ticket, 11 $5 tickets, 48 $2 tickets, and 50 tickets for applause and positive affirmations from the group. Tickets were drawn without replacement. Lucky draw cash incentives are provided immediately. Table 1 provides a summary of the AC group content by session. AC groups included a maximum of 10 women and multiple AC groups were conducted where necessary.
Results
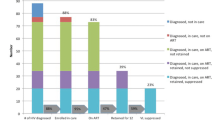
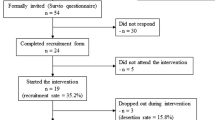
As shown in Fig. 1, 183 women with an ATS specific substance involvement score of four or higher on the ASSIST and biologically confirmed recent ATS use were eligible for CCT in the first six provinces. Of these, 158 accepted a CCT appointment (86 %) and 138 (75 %) enrolled in CCT by completing at least one urine screening visit. Half of these CCT-enrolled women (n = 72; 52 %) were between 23 and 30 years old (median = 27, Interquartile range [IQR]: 23–31). Fifty-one percent (n = 71) completed between 1 and 6 years of primary education. One quarter (n = 35; 25 %) reported never being married and more than half (n = 78; 57 %) had at least one child. In the past month, approximately one-third (n = 54; 39 %) conducted sex work in an entertainment-based venue, 43 % worked freelance, and 18 % were brothel-based FESW.
Women enrolled in CCT completed a median of 25 (IQR: 9–32) of the 36 urine screening visits. Eighty-four women completed at least half (i.e., `18) of the 36 CCT urine screening visits making them eligible for the cognitive-behavioral AC group. The vast majority of the 84 women who were eligible for AC completed at least one group session (n = 79; 94 %) and approximately two-thirds (n = 57; 68 %) completed three or more group sessions. Thus, 44 % of the total population of women who were eligible for CCT completed at least one AC session and approximately one-third (31 %) of the total number of eligible women completed at least three AC sessions.
Discussion
This formative study described the adaptation of a CCT and cognitive-behavioral AC group intervention for implementation as part of a cluster randomized stepped wedge trial with Cambodian FESW who use ATS. Guided by the ADAPT-ITT framework (Wingood & DiClemente, 2008), the iterative process of adapting these evidence-based behavioral interventions for this population was informed by qualitative observations regarding the role of poverty, working conditions, transportation difficulties, and low literacy as possible barriers to engagement. Findings indicate that CCT + AC is feasible to implement with Cambodian FESW who use ATS. More than 70 % of eligible participants enrolled in CCT, providing support for feasibility of recruitment. Process indicators from the first six provinces in this ongoing cluster randomized stepped wedge trial also demonstrate feasibility of intervention delivery such that participats completed a median of 25 of the 36 possible urine screening visits and two-thirds of participants who were eligible for AC completed three or more group sessions. The approach employed to develop CCT and AC provides insights into some best practices for adapting and implementing evidence-based, behavioral interventions in resource-limited settings.
Only a small fraction of the broader population of individuals with a substance use disorder receive treatment (Open Society Foundations, 2010), which is also evident in CCT + AC engagement (Fig. 1). Among the total population of FESW eligible for CCT + AC, half attended a sufficient number of CCT urine screening visits to participate in AC and approximately one-third completed three or more cognitive-behavioral AC sessions. This is consistent with previous findings from the United States where only one in ten individuals with a substance use disorder receive addiction treatment (Open Society Foundations, 2010) and three-fourths of those enrolled in substance abuse treatment drop out early (Loveland & Driscoll, 2014). Consistent with the HIV care cascade (Gardner et al., 2011), expanded efforts are needed to support the identification of individuals with substance use disorders followed by interventions to promote linkage to and retention in evidence-based substance abuse interventions. In resource-limited settings like Cambodia where formal substance abuse treatment is not available, CCT + AC represents a time-limited, potentially scalable approach to reduce ATS use and optimize HIV prevention with FESW.
Our findings should be interpreted in the context of some important limitations. Cognitive-behavioral substance abuse treatments for stimulant use disorders such as the Matrix Model are intensive approaches requiring a combination of up to 56 individual, group, and family sessions to achieve modest reductions in stimulant use (Colfax et al., 2010). Because the present study was conducted in a resource-limited setting, we developed a 4-session, cognitive-behavioral AC group with the goal of boosting and extending the effectiveness of CCT as an evidence-based intervention for reducing stimulant use (Prendergast et al., 2006). Although this approach appears to be feasible to implement, the number of AC session delivered represent less than 10 percent of those provided in the Matrix Model treatment. At the same time, there is some evidence that CCT alone achieves long-term reductions in stimulant use and condomless sex that may be comparable to the Matrix Model (Shoptaw et al., 2005). Our ongoing cluster randomized stepped wedge trial will examine the effectiveness of CCT + AC with Cambodian FESW who use ATS. Because ATS use assists FESW with seeing more clients, it is possible that CCT + AC may not adequately offset the lost earnings due to the relatively modest amount of the cash incentives. Further research is needed to examine whether and how behavioral interventions targeting ATS use can be paired with structural interventions such as microfinance that address poverty as a driver of ATS use and condomless sex in this population (Gupta et al., 2008). Finally, although findings from the present study highlight that it is feasible to deliver CCT + AC to Cambodian FESW who use ATS, further mixed methods research is needed to better characterize acceptability of this approach with FESW and service providers.
Despite these limitations, this study provides some of the first evidence regarding the feasibility of delivering behavioral interventions to reduce ATS use and condomless sex with FESW in Cambodia. An ongoing cluster randomized stepped wedge trial is examining the effectiveness of CCT + AC with ATS-using FESW in 10 Camobodian provinces. Because CCT + AC is time-limited, it represents a potentially scalable approach to target ATS use as a driver of the HIV epidemic if it ultimately proves to be effective.
References
Baird, S. J., Garfein, R. S., McIntosh, C. T., & Ozler, B. (2012). Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: A cluster randomised trial. Lancet, 379, 1320–1329.
Becker, A. E., & Kleinman, A. (2013). Mental health and the global agenda. New England Journal of Medicine, 369(1), 66–73.
Bowen, S., & Chawla, N. (2011). Mindfulness-based relapse prevetnion for addictive behaviors: A clinican’s guide. New York: Guilford Press.
Carrico, A. W., Gomez, W., Siever, M. D., Discepola, M. V., Dilworth, S. E., & Moskowitz, J. T. (2015). Pilot randomized controlled trial of an integrative intervention with methamphetamine-using men who have sex with men. Archives of Sexual Behavior, 44, 1861–1867.
Carroll, K. M., & Rawson, R. A. (Eds.). (2005). Relapse prevention for stimulant dependence. New York, NY: Guilford Press.
Center for Substance Abuse Treatment. (2006). Client’s handbook: Matrix intensive outpatient treatment for people with stimulant use disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Colfax, G., Santos, G. M., Chu, P., Vittinghoff, E., Pluddemann, A., Kumar, S., & Hart, C. (2010). Amphetamine-group substances and HIV. Lancet, 376, 458–474.
Couture, M. C., Evans, J. L., Sothy, N. S., Stein, E. S., Sichan, K., Maher, L., & Page, K. (2012). Correlates of amphetamine-type stimulant use and associations with HIV-related risks among young women engaged in sex work in Phnom Penh, Cambodia. Drug Alcohol Depend, 120, 119–126.
Couture, M. C., Sansothy, N., Sapphon, V., Phal, S., Sichan, K., Stein, E., & Page, K. (2011). Young women engaged in sex work in Phnom Penh, Cambodia, have high incidence of HIV and sexually transmitted infections, and amphetamine-type stimulant use: New challenges to HIV prevention and risk. Sexually Transmitted Diseases, 38, 33–39.
Crepaz, Nicole, Lyles, Cynthia M., Wolitski, Richard J., Passin, Warren F., Rama, Sima M., Herbst, Jeffrey H., & The HIV/AIDS Prevention Research Synthesis Team. (2006). Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS, 20, 143–157.
Dixon, T. C., Ngak, S., Stein, E., Carrico, A., Page, K., & Maher, L. (2015). Pharmacology, physiology and performance: Occupational drug use and HIV risk among female entertainment and sex workers in Cambodia. Harm Reduction Journal, 12, 33.
Dixon, T. C., Stein, S, Ngak, S., Srean, C., Maly, P., Sokunny, M., Carrico, A., Page, K., & Maher, L. (in press). Qualitative research and implementation science: Informing the acceptability and implementation of a trial of a conditional cash transfer intervention designed to reduce drug use and HIV risk. Methodological Innovations.
Dutra, L., Stathopoulou, G., Basden, S. L., Leyro, T. M., Powers, M. B., & Otto, M. W. (2008). A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry, 165, 179–187.
Epstein, D. H., Hawkins, W. E., Covi, L., Umbricht, A., & Preston, K. L. (2003). Cognitive-behavioral therapy plus contingency management for cocaine use: Findings during treatment and across 12-month follow-up. Psychology of Addictive Behaviors, 17, 73–82.
Fernald, L. C., Gertler, P. J., & Neufeld, L. M. (2008). Role of cash in conditional cash transfer programmes for child health, growth, and development: An analysis of Mexico’s Oportunidades. Lancet, 371, 828–837.
FHI 360. (2011). SMARTGirl: Program review. Retrieved from http://www.fhi360.org/resource/program-review-smartgirl-providing-hivaids-prevention-and-care-entertainment-workers.
Gardner, E. M., McLees, M. P., Steiner, J. F., Del Rio, C., & Burman, W. J. (2011). The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical Infectious Diseases, 52, 793–800.
Gupta, G. R., Parkhurst, J. O., Ogden, J. A., Aggleton, P., & Mahal, A. (2008). Structural approaches to HIV prevention. Lancet, 372, 764–775.
Ho, H. T., Le, G. M., & Dinh, T. T. (2013). Female sex workers who use amphetamine-type stimulants (ATS) in three cities of Vietnam: Use and sexual risks related to HIV/AIDS. Global Public Health, 8, 552–569.
Humeniuk, R., Ali, R., Babor, T. F., Farrell, M., Formigoni, M. L., Jittiwutikarn, J., & Simon, S. (2008). Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction, 103, 1039–1047.
Koblin, B. A., Husnik, M. J., Colfax, G., Huang, Y., Madison, M., Mayer, K., & Buchbinder, S. (2006). Risk factors for HIV infection among men who have sex with men. AIDS, 20, 731–739.
Lee, N. K., & Rawson, R. A. (2008). A systematic review of cognitive and behavioural therapies for methamphetamine dependence. Drug and Alcohol Review, 27, 309–317.
Ling Murtaugh, K., Krishnamurti, T., Davis, A. L., Reback, C. J., & Shoptaw, S. (2013). Spend today, clean tomorrow: Predicting methamphetamine abstinence in a randomized controlled trial. Health Psychology, 32, 958–966.
Loveland, D., & Driscoll, H. (2014). Examining attrition rates at one specialty addiction treatment provider in the United States: A case study using a retrospective chart review. Substance Abuse Treatment, Prevention, and Policy, 9, 41.
Maher, L., Dixon, T., Phlong, P., Mooney-Somers, J., Stein, E., & Page, K. (2015). Conflicting rights: How the Prohibition of human trafficking and sexual exploitation infringes the right to health of female sex workers in Phnom Penh, Cambodia. Health, and Human Rights, 17, E102–E113.
Maher, L., Phlong, P., Mooney-Somers, J., Keo, S., Stein, E., Couture, M. C., & Page, K. (2011). Amphetamine-type stimulant use and HIV/STI risk behaviour among young female sex workers in Phnom Penh, Cambodia. The International Journal of Drug Policy, 22, 203–209.
National Center for HIV/AIDS, Dermatology, and STDs (2010). HIV sentinel surveys 2010: Female entertainment workers (FEW) and antenatal care clinic (ACC) attendees. In Cambodia Ministry of Health (Ed.). Phnom Penh, Cambodia.
Olmstead, T. A., Sindelar, J. L., & Petry, N. M. (2007). Cost-effectiveness of prize-based incentives for stimulant abusers in outpatient psychosocial treatment programs. Drug and Alcohol Dependence, 87, 175–182.
Open Society Foundations. (2010). Defining the addiction treatment gap. https://www.opensocietyfoundations.org/publications/defining-addiction-treatment-gap-data-summary.
Ostrow, D. G., Plankey, M. W., Cox, C., Li, X., Shoptaw, S., Jacobson, L. P., & Stall, R. C. (2009). Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. Journal of Acquired Immune Deficiency Syndromes, 51, 349–355.
Page, K., Stein, E., Sansothy, N., Evans, J., Couture, M. C., Sichan, K., & Young Women’s Health Study, Collaborative. (2013). Sex work and HIV in Cambodia: Trajectories of risk and disease in two cohorts of high-risk young women in Phnom Penh, Cambodia. BMJ Open, 3, e003095.
Plankey, M. W., Ostrow, D. G., Stall, R., Cox, C., Li, X., Peck, J. A., & Jacobson, L. P. (2007). The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. Journal of Acquired Immune Deficiency Syndromes, 45, 85–92.
Prendergast, M., Podus, D., Finney, J., Greenwell, L., & Roll, J. (2006). Contingency management for treatment of substance use disorders: A meta-analysis. Addiction, 101, 1546–1560.
Rasella, D., Aquino, R., Santos, C. A., Paes-Sousa, R., & Barreto, M. L. (2013). Effect of a conditional cash transfer programme on childhood mortality: A nationwide analysis of Brazilian municipalities. Lancet, 382, 57–64.
Rawson, R. A., Huber, A., McCann, M., Shoptaw, S., Farabee, D., Reiber, C., & Ling, W. (2002). A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Archives of General Psychiatry, 59, 817–824.
Rawson, R. A., Marinelli-Casey, P., Anglin, M. D., Dickow, A., Frazier, Y., Gallagher, C., & Methamphetamine Treatment Project Corporate, Authors. (2004). A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction, 99, 708–717.
Rawson, R. A., McCann, M. J., Flammino, F., Shoptaw, S., Miotto, K., Reiber, C., & Ling, W. (2006). A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction, 101, 267–274.
Rawson, R. A., Shoptaw, S. J., Obert, J. L., McCann, M. J., Hasson, A. L., Marinelli-Casey, P. J., & Ling, W. (1995). An intensive outpatient approach for cocaine abuse treatment. The matrix model. Journal of Substance Abuse Treatment, 12, 117–127.
Saphonn, V., Chorvann, C., Heng, S., Luyna, U., & Sellava, R. (2010). The long run: Costs and financing of HIV/AIDS in Cambodia. In Report of Results for Development Institute (R4D) and the National Center for HIV/AIDS and STI (NCHADS).
Saphonn, V., Parekh, B. S., Dobbs, T., Mean, C., Bun, L. H., Ly, S. P., & Detels, R. (2005). Trends of HIV-1 Seroincidence Among HIV-1 Sentinel Surveillance Groups in Cambodia, 1999-2002. Journal of Acquired Immune Deficiency Syndromes, 39, 587–592.
Shoptaw, S., Reback, C. J., Larkins, S., Wang, P. C., Rotheram-Fuller, E., Dang, J., & Yang, X. (2008). Outcomes using two tailored behavioral treatments for substance abuse in urban gay and bisexual men. Journal of Substance Abuse Treatment, 35, 285–293.
Shoptaw, S., Reback, C. J., Peck, J. A., Yang, X., Rotheram-Fuller, E., Larkins, S., & Hucks-Ortiz, C. (2005). Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug and Alcohol Dependence, 78, 125–134.
United Nations Office on Drugs and Crime (2015). World drug report. New York, NY: United Nations. Retrieved from https://www.unodc.org/documents/wdr2015/World_Drug_Report_2015.pdf.
Vun, M. C., Fujita, M., Rathavy, T., Eang, M. T., Sopheap, S., Sovannarith, S., & Verbruggen, R. (2014). Achieving universal access and moving towards elimination of new HIV infections in Cambodia. Journal of the International AIDS Society, 17, 18905.
Wingood, G. M., & DiClemente, R. J. (2008). The ADAPT-ITT model: A novel method of adapting evidence-based HIV Interventions. Journal of Acquired Immune Deficiency Syndromes, 47, S40–S46.
Word Health Organization. (2010). Self-help strategies for cutting down or stopping substance use: A guide. Geneva, Switzerland. Retrieved from http://apps.who.int/iris/bitstream/10665/44322/1/9789241599405_eng.pdf.
Zhang, X. D., Kelly-Hanku, A., Chai, J. J., Luo, J., Temmerman, M., & Luchters, S. (2015). Sexual and reproductive health risks amongst female adolescents who use amphetamine-type stimulants and sell sex: A qualitative inquiry in Yunnan, China. Harm Reduction Journal, 12, 34.
Acknowledgments
This research was supported by the National Institute on Drug Abuse (NIDA), R01-DA033673 (Page & Stein, PIs). We would like to express our gratitude to Amy Weissman for supporting the implementation of this project, Chim Srean for coordinating data management in the field, and Phou Maly for serving as a facilitator for the aftercare groups. We would also like to thank Drs. Rick Rawson and Steve Shoptaw for their consultation with our team in adapting Matrix Model early recovery and relapse prevention skills for this population. Finally, we would like to express our gratitude for the ongoing support of numerous community-based organization who have made the implementation of this project possible: Cambodian Women for Peace and Development (CWPD), Phnom Srey Organization for Development (PSOD), Poor Family Development (PFD), and KHEMERA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Adam W. Carrico, Ean Nil, Chhit Sophal, Ellen Stein, Muth Sokunny, Neak Yuthea, Jennifer L. Evans, Song Ngak, Lisa Maher and Kimberly Page declare that they have no conflict of interest.
Human and animal rights and Informed consent
All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Carrico, A.W., Nil, E., Sophal, C. et al. Behavioral interventions for Cambodian female entertainment and sex workers who use amphetamine-type stimulants. J Behav Med 39, 502–510 (2016). https://doi.org/10.1007/s10865-016-9713-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-016-9713-2