Abstract
Little research exists on the impact of behavior change interventions in disadvantaged communities. We conducted a prospective study to explore the effectiveness of motivational interviewing on physical activity change within a deprived community and the social- psychological and motivational predictors of change in physical activity including stage of change, self-efficacy, social support, and variables from self-determination theory and the theory of planned behavior. Five motivational interviewing counsellors recruited 207 patients and offered motivational interviewing sessions to support physical activity behavior change. At 6-months there were significant improvements in physical activity, stage of change, and social support. A dose–response relationship was evident; those who attended 2 or more consultations increased their total physical activity, stage of change and family social support more than those who attended just one. Hierarchical regression analyses indicated that number of sessions and change in stage of change predicted 28.4 % of the variance in change in total physical activity and, with social support from friends, 21.0 % of the variance in change walking time. Change in perceived behavioral control and attitudes, friend social support, and number of sessions predicted 16.8 % of the variance in change in vigorous physical activity. Motivational interviewing is an effective approach for promoting physical activity amongst lower socio-economic status groups in the short term. The study demonstrates good translational efficacy, and contributes to a limited number of physical activity interventions targeting low income groups in the UK.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Physical inactivity presents substantial risks to public health and an estimated 60–70 % of the adult population in the UK do not engage in sufficient physical activity to prevent chronic illness (Blair, 2009). There is now considerable evidence supporting the benefits of regular physical activity in the primary prevention of chronic diseases (Warburton et al., 2006; Orozco et al., 2008) and in the secondary prevention of illness in individuals with existing medical conditions (Wood et al., 2008; Wolin et al., 2009). Epidemiological studies have established that leading a sedentary lifestyle increases the incidence of at least 17 medical conditions (Helmerhorst et al., 2009; Katzmarzyk, 2009). Currently, it is reported that 39 % of men and 29 % of women meet the recommended levels of physical activity in the UK (The Health and Social Care Information Centre, 2010). However, accelerometer data taken from the 2008 Health Survey for England found that of those claiming to meet recommendations, only a mere 6 % of men and 4 % of women actually did (Craig et al., 2009). Therefore, sedentary behavior, and the medical conditions to which it gives rise, is likely to be more widespread than current reports indicate and represent a significant proportion of the disease burden facing the National Health Service (NHS). At a local level, the average healthcare cost of physical inactivity per Primary Care Trust is approximately £5 million per year (Department of Health, 2009).
Physical activity participation also varies by socio-economic status; individuals of a lower socio-economic status are less likely to adopt and maintain a healthy lifestyle (McNeill et al., 2006; Kamphuis et al., 2009). Subsequently, a positive relationship has been found to exist between socioeconomic position and physical activity status (Saavedra et al., 2008; Sallis et al., 2009), with social class, income, and education all found to be significantly related to participation (Stamatakis & Chaudhury, 2008). The inverse association between socio-economic status and health is now well established (Kamphuis et al., 2007); with individuals of a lower socio-economic status having higher risks for both morbidity and all-cause mortality than their higher socio-economic status counterparts (Huisman et al., 2005; Mackenbach et al., 2008). For example, between 2001 and 2006 the death rate from coronary heart disease in the 20 % most deprived areas in England was nearly 60 % higher than the rate in the 20 % least deprived (British Heart Foundation, 2009). The socially disadvantaged also experience a disproportionate increase in the prevalence of most chronic diseases (Everson-Rose & Lewis, 2005; James et al., 2006) and psychosocial stress (Latkin & Curry, 2003). Despite the compelling evidence of the need to target socially disadvantaged groups, reviews point to the paucity of data on the impact of behavior change interventions amongst disadvantaged communities (Michie et al., 2009), with only three (Sykes & Marks, 2001; Lowther et al., 2002; Steptoe et al., 2003) randomized controlled trials (RCTs) conducted within the UK, two in the USA (Rosamond et al., 2000; Emmons et al., 2005), and one in Canada (O’Loughlin et al., 1999). Furthermore, there have been few interventions that target low socio-economic status individuals within primary care (Dutton et al., 2007; Parra-Medina et al., 2010). Therefore, building evidence towards the ‘what works and for whom’ requirement among disadvantaged groups is in its infancy (Michie et al., 2009).
Interventions adopting motivational interviewing, a one-to-one client-centred counselling technique, have shown promise in promoting physical activity in comparison to standard treatments or controls (Hardcastle et al., 2008; Benbassat et al., 2008; Miller & Beech, 2009). Reviews and syntheses of research using motivational interviewing have revealed that both number and duration of motivational interviewing sessions are related to behavior change. For example, a meta-analytic synthesis of 72 RCTs using motivational interviewing in health-related contexts (e.g., weight reduction, alcohol and smoking cessation) revealed that the technique was more effective in improving behavioral (e.g., number of cigarettes, alcohol consumption) and health related (e.g., body mass index, cholesterol) outcomes relative to usual care control groups (e.g., advice giving) in 80 % of studies (Rubak et al., 2005). The size of the motivational interviewing effect was large for direct indexes of behavior (e.g., number of cigarettes, d = 1.32; alcohol consumption, d = 14.64) and small-to-medium for outcomes associated with behavior change (e.g., body mass index, d = 0.72; cholesterol, d = 0.27) relative to usual care. Of motivational interviewing encounters lasting 60 min, 81 % of studies demonstrated an effect compared to only 64 % of studies with an encounter equal to or less than 20 min. Furthermore, an effect was found in only 40 % of studies with only one counselling session, but in 87 % of studies with more than five. Previous motivational interviewing research has included the use of ‘adaptations’ of motivational interviewing as opposed to ‘pure’ motivational interviewing and the optimal dose to promote autonomous forms of motivation and sustained physical activity change is unclear (Martins & McNeil, 2009). Furthermore, many studies have combined motivational interviewing with other strategies (e.g., a pedometer), making it difficult to determine the unique contribution of motivational interviewing to behavior change (Martins & McNeil, 2009). In addition, there remains a dearth of evidence as to how and why motivational interviewing interventions might work (Burke et al., 2003).
Motivational interviewing is recognised as technique that is not based on any one particular theory. It has been linked to constructs from a number of social-psychological models of health behavior and represents an integrated set of theory-based components (Hagger, 2009; Orbell et al., 2006). Specifically, motivational interviewing has been shown to provide three of the key components that support psychological needs based on self-determination theory (Deci & Ryan, 1985, 2000; Markland et al., 2005), to enhance self-efficacy from social cognitive theory (Bandura, 1977; Rohsenow et al., 2004), and to increase attitudes and perceived behavioral control from the theory of planned behavior (Ajzen, 1985; Hagger & Chatzisarantis, 2009; McEachan et al., 2011).
Motivational interviewing has been explicitly linked with self-determination theory in that its key components provide support for each of the psychological needs for competence, autonomy, and relatedness (Markland et al., 2005; Markland & Vansteenkiste, 2007). The structure provided by the practitioner, such as helping the client develop appropriate goals and providing positive feedback, targets the psychological need for competence. The provision of autonomy support by using client-centred strategies like rolling with resistance, exploring options, and letting the client make decisions, all support the need for autonomy. The involvement of the client by the practitioner in terms of expressing empathy, demonstrating an understanding of the client’s position, and avoiding judgemental talk, supports the need for relatedness. Together, the satisfaction of these needs through motivational interviewing is likely to foster increased autonomous motivation to engage in physical activity and result in increased behavioral engagement and adherence.
In addition to these explicit links between psychological need satisfaction and motivational interviewing components, there are also components that explicitly support the situational promotion autonomous motivation through the behaviors of social agents in the actor’s environment. In the case of motivational interviewing, the motivational interviewer is the ‘social agent’ and the client is the ‘actor’. In a seminal study of autonomy support, Deci et al. (1994) suggested that the provision of choice, acknowledging difficulties and conflict, and exploring reasons and rationales for engaging in a given behavior were all important components of autonomy support and would promote autonomous motivation for that behavior. The ‘menu of strategies’ and guiding principles typically adopted by motivational interviewers include encouraging client choice (e.g., ‘eliciting change talk’), acknowledging difficulties and conflicts (e.g., ‘rolling with resistance’), and providing reasons and rationale (e.g., ‘exploring pros and cons’) as options. This means that typical aspects of motivational interviewing are likely to foster autonomous forms of motivation and, as a consequence, promote increased autonomous motivation.
Based on this theory, interventions with autonomy-supportive components, like motivational interviewing, are proposed to be effective in promoting behavioral engagement and adherence because they evoke a concomitant change in levels of autonomous motivation (Chatzisarantis & Hagger, 2009). Researchers have frequently adopted measures of autonomous motivation to ascertain whether such strategies are effective in producing change in the psychological mediators of behavior change (e.g., Williams, 2002). According to self-determination theory, motivation is typically reflected in four forms or types ordered on a continuum from autonomous to controlled (Ryan & Connell, 1989). Intrinsic motivation is the prototypical form of autonomous motivation where behavior is driven by choice (e.g., exercising for enjoyment). Identified regulation is an autonomous form of regulation, but reflects acting to obtain some externally-referenced goal which is personally valued (e.g., exercising to gain fitness). Introjected regulation is a controlled form of motivation, and reflects acting to obtain some externally-referenced outcome (e.g., exercising to improve appearance or to avoid guilt). Finally, external regulation is the prototypical form of controlled motivation and reflects behaving for external reinforcement (e.g., exercising to gain a reward). Investigations involving autonomy-supportive components have typically used a single index of autonomous motivation based on a weighted average of the four types of motivation, known as a relative autonomy index. This provides a measure of the degree to which an individual feels his or her environment supports autonomy. A comparatively recent addition to the conceptualization of forms of motivation is amotivation, which reflects individuals who lack intention or drive and therefore a complete lack of both types of motivation from self-determination theory (Deci & Ryan, 2000).
Motivational interviewing has also been closely linked with self-efficacy and constructs from the theory of planned behavior, particularly attitudes and perceived behavioral control. With respect to self-efficacy, setting personally-relevant goals, providing individualized feedback, and using visual imagery to compare the current and desired outcomes of physical activity are all motivational interviewing components that have been adopted to enhance self-efficacy. Indeed, the enhancement of self-efficacy is proposed to be one of the mechanisms by which motivational interviewing changes physical activity behavior (Miller & Rollnick, 2002). Research has demonstrated that motivational interviewing interventions lead to increases in self-efficacy (Chen et al., 2011; Rohsenow et al., 2004), although, to date, there is limited data to demonstrate its role as a mechanism despite researchers acknowledging its potential role (Shaikh et al., 2011; Walpole et al., 2011). In terms of the theory of planned behavior, motivational interviewing incorporates techniques designed to promote increased attitudes toward the target behavior such as dispelling negative beliefs through change talk (Bertholet et al., 2011) and empowering individuals to overcome with barriers (Ridge et al., 2012) have been mooted as means to change behavior by targeting attitudes and perceived behavioral control respectively.
Research to examine whether intervention effects are due to changes in the previously-reviewed theoretical constructs is relatively sparse (Lewis et al., 2006). As such, the current study measures some of the most likely social-psychological and motivation predictors of behavior change hypothesized to mediate the effects of our motivation interviewing intervention (Amireault et al., 2008; Lorentzen et al., 2007). Specifically, we included measures of self-efficacy (Lewis et al., 2006; Burke et al., 2008), social support (Parks et al., 2003), autonomous forms of motivation from SDT (Chatzisarantis & Hagger, 2009) and attitudes and perceived behavioral control from the Theory of Planned Behavior (Courneya & Bobick, 2000) as important candidate social-psychological and motivational mediators of the effects of our motivation interviewing intervention on physical activity.
Based on the evident health and cost implications of leading an inactive lifestyle, the robust findings linking lower socio-economic status to undesirable lifestyle behaviors and consequently poorer health, as well as the limitations of previous motivational interviewing research, the purpose of this study was threefold: (1) to investigate the effectiveness of using motivational interviewing within the primary care setting to increase physical activity amongst lower socio-economic groups, (2) to examine the degree of support needed to facilitate physical activity, and (3) to explore the social-psychological and motivational predictors of physical activity behavioral change.
Method
Participants and recruitment
Participants were recruited via opportunistic and purposive sampling procedures. Qualified healthcare professionals (e.g., family physicians, practice nurses) referred eligible participants to the ‘lifestyle change facilitation service’. The inclusion criteria were patients that were either sedentary, insufficiently or moderately active who did not exhibit contra-indications for physical activity. Insufficient physical activity was defined as not meeting the recommendations as outlined in the Chief Medical Officer’s report (Department of Health, 2004), namely, less than 5 × 30 min of moderate-intensity physical activity per week. Essentially, General Practitioners referred patients to the lifestyle change facilitation service on the basis that their physical and mental health could benefit from increased physical activity. Since the focus of the study was to explore the efficacy of the intervention in disadvantaged communities, we recruited participants from electoral districts with overall low socio-economic status (NHS East Sussex Downs & Weald, 2009). Healthcare professionals selected eligible patients that met the inclusion criteria for the study during routine consultations.
We conducted an analysis to ensure a sufficiently-large sample was recruited so that our study was adequately-powered to find hypothesized effects. Given previous research and meta-analytic findings that have typically found medium effects for motivational interviewing on health-related behavioral outcomes (Rubak et al., 2005), including physical activity (Armstrong et al., 2011), we aimed to detect an effect of the motivational interviewing intervention on the primary outcome physical activity outcomes (total, moderate, vigorous, and walking) of medium size with power (beta) set at 0.80 (beta level) and probability (alpha level) set at 0.05. Other than the pre- and post-trial comparisons, we also included independent variables of attendance and socioeconomic status as independent variables, reflecting our mixed 2 (time: baseline vs. 6-month follow-up) × 2 (socio-economic status: high vs. low) × 2 (attendance status: high vs. low) ANOVA design. Based on these criteria, we estimated that the minimum sample size was for a two-tailed hypothesis was 128. Given an expected 6-month drop-out rate of in participants from comparable motivational interviewing studies of approximately 40 % (Brug et al., 2007; Hardcastle et al., 2008; DiMarco et al., 2009; West et al., 2007), we estimated a minimum sample size at recruitment (baseline) of 180.
During an initial appointment, patients were introduced to the research and given a participant information sheet. Once consent was obtained, patients were required to complete a questionnaire. Following the initial appointment, a follow up appointment lasting between 45 min and 1 h was offered, with the number and frequency of follow up sessions at the patient’s discretion (with a maximum of 12). Six months following a patient’s initial appointment, questionnaires were posted for self-completion. Approval was obtained from Brighton West NHS Ethics Committee and the Sussex NHS Research Consortium prior to the commencement of the study.
Counselling intervention
The behavior change intervention known as the ‘lifestyle change facilitation service’ is delivered across selected health practices within the Hastings and Rother district in the South East of England targeting wards with the lowest life expectancy. Based on the application of motivational interviewing (Miller & Rollnick, 2002), in conjunction with the Transtheoretical Model (Prochaska & DiClemente, 1983), the lifestyle change facilitation service seeks to provide patients with one-to-one behavior change counselling (Hastings & Rother Primary Care Trust, 2008). Motivational interviewing was implemented by five Lifestyle Change Facilitators. Patients were not told reasons for change;Footnote 1 instead, the focus was on exploring ambivalence and eliciting self-directed ‘change talk’ (Amrhein et al., 2003). Strategies to build autonomous motivation in those ambivalent about change such as agenda setting, decisional balance and eliciting change talk were practiced, alongside strategies for those sufficiently motivated to strengthen commitment to change and negotiate a change plan (Hardcastle et al., 2008). Typical strategies adopted by the counsellors included agenda setting/typical day, exploration of the pros and cons, importance and confidence rulers and the ‘two possible futures’ strategy (looking over the hypothetical fence). Such strategies were learned on the advanced course on motivational interviewing and have been found to help elicit change talk, develop discrepancy and enhance readiness, and commitment for change. When patients were ready to change, a general discussion would ensue typically around planning and realistic goal setting (first steps). Sometimes a change plan worksheet would be used but mostly it was discussed informally. A discussion around planning would involve considering potential obstacles/barriers and enlisting social support to help support behavior change efforts. As an example of strategy, the importance and confidence ruler technique promoted by Rollnick (1997) began with two questions: (1) “On a scale of 1–10 (with 10 being the highest), how important is it for you to increase your physical activity level?” and (2) “On a scale of 1 to 10, if you did want to increase your physical activity level, how confident are you that you could do so?” Following the patient’s response, the facilitators followed with two probing questions: (1) “Why did you not choose a lower number?” to elicit positive motivational statements from patients and (2) “What would it take for you to give a score of 9 or 10?” to elicit the barriers that the patients typically experienced. The lifestyle change facilitators then summarized the patient’s responses and, if barriers were cited by the patient, prompted the patient to identify potential solutions, whilst seeking permission to list additional resolutions. Where appropriate, the consultation ended with a goal set by the patient, linked to the solutions discussed (Resnicow et al., 2001). The nature of each consultation was unique to the patient and visit, with different strategies employed depending on patient need and readiness to change.
Intervention fidelity
All Lifestyle Change Facilitators participated in two motivational interviewing courses; delivered by an accredited MINT (Motivational Interviewing Network of Trainers) trainer. The first was a 2-day introduction, whilst the second was a 4-day advanced course. Both events focused on the principles of motivational interviewing and emphasized the key underlying spirit (Emmons & Rollnick, 2001). All Lifestyle Change Facilitators were then required to perform an audio-taped consultation session and have it assessed by the independent MINT trainer using the MITI 3.1(Motivational Interviewing Treatment Integrity). The MITI (Moyers et al., 2010) is a one-pass behavioral coding system designed to measure treatment fidelity using a 20-min segment of a motivational interviewing session. The manager of the lifestyle change facilitation service observed all facilitators on a further three separate occasions to assess their adherence to and confidence in delivering motivational interviewing. Lifestyle change facilitators were given written feedback. The assessment undertaken by the service manager followed the approach advocated by Miller and Mount (2001). This assessment included the degree to which the facilitators adhered to the spirit of motivational interviewing, their use of key skills and of motivational interviewing consistent and inconsistent responses. Lifestyle Change Facilitators also attended monthly team meetings and bi-monthly clinical supervision in which discussion of motivational interviewing implementation could take place. Finally, lifestyle change facilitators gained at least 6 months experience within routine consultations prior to the start of data collection.
Measures
Physical activity
Self-reported physical activity was assessed using the short version of the international physical activity questionnaire (IPAQ); Booth, 2000). The IPAQ collects data on the intensity, frequency, and duration of physical activity in the previous 7 days. Median MET-minutes for varying intensity physical activity are calculated. A total physical activity score is calculated by adding up scores from the various intensity domains. The IPAQ has acceptable reliability and criterion validity (against the MTI accelerometer) (Craig et al., 2003). Data cleaning and scoring followed the procedures outlined in the guidelines for use of the IPAQ (The IPAQ Group, 2012).
Psychological variables
Physical Activity Stage of Change was assessed using the physical activity Stages of Change flow chart (Blair et al., 2001) which classified participants as either in pre-contemplation, contemplation, preparation, action, or maintenance, based on their ‘yes’ or ‘no’ response to five questions. Self-efficacy was assessed with the Self Efficacy for Exercise Scale, a revision of McAuley’s (1990) Self Efficacy Barriers to Exercise measure, consisting of nine situations that might affect participation in exercise (example items include “tired”, “busy”, “weather”, and “bored”) with responses given on a 5-point scale ranging from 1 (not at all) to 5 (very much). The scale displayed high internal consistency (Cronbach alpha, α = 0.86). Behavioral Regulation in Exercise was assessed with the BREQ-2 (Markland and Tobin, 2005) which operationalizes exercise motivation along a self-determination continuum and includes measures of external, introjected, identified, and intrinsic regulation, and a measure of amotivation. The sub-scales displayed acceptable internal consistency (Internal consistency for external regulation, α = 0.71; introjected regulation, α = 0.68; identified regulation, α = 0.65; intrinsic motivation, α = 0.89; amotivation, α = 0.63). The variables from the motivational continuum were used to compute a single relative autonomy index through a weighting procedure with amotivation being assigned a weight of −3, external regulation a weight of −2, introjected regulation a weight of −1, identified regulation a weight of +2, and intrinsic regulation a weight of +3. It was, therefore, considered separately in current analyses. Attitude was assessed via response to the statement “For me, exercising over the next 2 weeks would be…” This statement was then paired with six bipolar, 7-point adjective scales to assess both instrumental and affective attitudes. Instrumental attitude was assessed by responses on three items (useless–useful, foolish-wise, harmful-beneficial), whilst affective attitude was measured via responses to the remaining three items (un-enjoyable-enjoyable, boring-interesting, stressful-relaxing). The scale displayed acceptable internal consistency (α = 0.68). Perceived Behavioral Control (PBC) was measured along three dimensions using 7-point Likert scales. The questions used were “How confident are you over the next 2 weeks that you could exercise regularly if you wanted to do so?” (Very unconfident–very confident), “How much personal control do you feel you have over exercising regularly over the next 2 weeks?” (Very little control-complete control), and “How much I exercise in the next 2 weeks is completely up to me?” (Strongly agree-strongly disagree). The scale displayed high internal consistency (α = 0.86). Social Support was assessed using the Social Support for Physical Activity Scale (Sallis et al., 1987). The scale lists 13 statements in which participants are required to score the frequency in which the statement has occurred over the last month in relation to both friends and family, using a six point scale ranging from 0 (does not apply) to 5 (very often). Scores for each category were totalled in order to give two separate scores (between 0 and 65). The scale displayed high internal consistency with (internal consistency for Social Support from Friends, α = 0.82; Social Support from Family, α = 0.85). Health Care Climate Questionnaire (Williams et al., 1999) was administered at the 6-month follow-up to measure patients’ perceptions of the degree to which their lifestyle change facilitator was autonomy supportive. The purpose of this measure was to provide an indication as to whether patients perceived the lifestyle change facilitators had adhered to the spirit of motivational interviewing within the consultations. The Health Care Climate Questionnaire contains 15 items. Scores are calculated by averaging the individual item scores. Prior to averaging item scores, the score of item 13 is reversed. Higher average scores represent a higher level of perceived autonomy support.
Socio-economic status
Occupation, education, and income are traditionally used to indicate socio-economic status and have been consistently shown to be very useful in describing and evaluating health inequalities. In the current study we collected multiple indicators of socio-economic status in order to ensure that we were able to clearly identify participants as representative of disadvantaged groups. These included highest educational attainment, occupation, and household income. Highest educational attainment was measured according to highest educational qualification on five levels (University degree or higher degree; A levels, National Vocational Qualification level 3, O level/CSE/GCSE or National Vocational Qualification 1 or 2; other qualification and no qualifications. Occupation was based on participants selecting a particular type (e.g., admin, clerical, managerial, routine manual, unskilled manual, homemaker etc.). Income was based on average household income per year before taxes and participants were asked to tick one of the following options: <£10,000; £10,001–£15,000; £15,001–£20, 000; £20,001–£30,000; £30,001–£50,000; £50,001–£100,000; >£100,000.
Criteria used to characterise the SES of the sample
In order to confirm that participants in the current sample were from low socio-economic status backgrounds, we identified household income as the primary criterion. Household income was used as the primary indicator of socio-economic status because it has a dose-relationship with health and is one of the best indicators of living standards (Lynch et al., 2000). In order to be classified as a member of the ‘lower SES group’ the reported annual household income had to be £20,000 or less. On this basis, 120 participants met this criterion and were classified as low socio-economic status. A further 34 participants responded to the income question with ‘prefer not to say’ and could not be classified according to income. We therefore used additional indicators (occupation and highest educational attainment) to confirm whether these participants were from ‘lower’ socio-economic status backgrounds. Those who were unemployed (n = 6) were also added to the ‘lower’ socio-economic group. Participants (n = 17) reporting an education level of ‘no qualifications’ or ‘other qualifications’ were included in the ‘lower socio-economic status group’. The other (n = 11) participants did not meet the criteria for the ‘lower socio-economic status group’ on either occupation or educational attainment.
Data analysis
Using a last observation carried forward intent to treat analysis throughout, we planned a series of 2 (time: baseline vs. 6-month follow-up) × 2 (socio-economic status: high vs. low) × 2 (attendance status: high vs. low) ANCOVAs with repeated measures on the first factor were used to determine whether (1) there was a significant effect for the intervention on the key outcome variables, namely, the physical activity and psychological variables related to behavior change from baseline to 6-month follow-up, (2) socio-economic status and attendance status influenced the outcome variables, and (3) there were interactive effects of the intervention with socio-economic status and attendance on the outcomes. We planned to include physical activity status, defined as whether participants achieved the minimum guidelines for physical activity at baseline, as a covariate in the analyses. We calculated change scores on all behavioral and psychological variables by subtracting baseline scores from follow-up scores. A one-way ANOVA was used to explore the effect of motivational interviewing dose (1–6 sessions) on physical activity change. Where appropriate, univariate follow-up F-tests were used to examine the location of the differences. Finally, hierarchical regression analyses were conducted to explore the predictors of change in physical activity.
Results
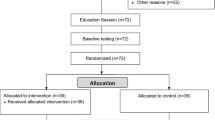
A total of 207 patients participated in the study, of which 64 were allocated to the ‘higher socio-economic status group’ and 143 to the ‘lower socio-economic status group’. The majority (84 %) of the ‘lower’ group had a household income of £20,000 or less, with 29 % (n = 41) reporting a household income of £10–15,000, and 43 % receiving an annual household income of less than £10,000. Sixty-five percent (n = 135) of those recruited were female and 70 % were aged over 50 years. With respect to the ethnic makeup of the sample, 94 % classified themselves as White-British; a further 3 % classified themselves as White-other; 1 % described themselves as White-Irish, and 1 % described themselves as from different racial groups (Asian-Bangladeshi, Asian-Indian, and Mixed race). With respect to physical activity, 60 % were insufficiently active at baseline (i.e., not meeting the recommendations as outlined in the Chief Medical Officer’s report; Department of Health, 2004). Sixty-five percent (n = 134) of patients completed both assessments. Of the 134 completing both assessments, 64.18 % (n = 86) were insufficiently physically active at baseline. Participants that completed both assessments attended a significantly greater number of motivational interviewing sessions (M = 2.50 sessions, SE = 0.13, p < .001), and tended to be less physically active at baseline (M = 952.62 MET-minutes, SE = 135.97, p = .05), compared to those who completed only one assessment.
Regarding engagement with the intervention, participants attended an average of 2.16 (SE = 0.10) counselling sessions over the 6-months intervention period, with 45 % (n = 91), 23, 15, 8, 5, and 4 % attending 1, 2, 3, 4, 5, or 6 plus consultations respectively. A sub-sample of participants that attended the 6-month follow up (n = 66) completed the Health Care Climate Questionnaire (Williams et al., 1999). Participants were found to highly endorse the autonomy supportive style of the sessions (M = 6.81, SE = .06) and scores for the scale were significantly greater than the mid-point of the scale (t (65) = 47.15, p < .001, d = 11.70).
Table 1 shows the baseline characteristics for all participants and for the ‘lower’ and ‘higher’ socio-economic status groups. Participants in the higher socio-economic status group had significantly higher levels of perceived behavioral control and lower stage of change and relative autonomy index for physical activity compared to the lower socio-economic status group. As a consequence, we controlled for the effect of variations in socio-economic status in our regression analyses along with other demographic variables in the first step prior to testing hypotheses of the predictors of physical activity variables.
Table 2 displays the baseline and 6-month follow-up scores for all variables. A series of 2 (time: baseline vs. 6-month follow-up) × 2 (socio-economic status: high vs. low) × 2 (attendance status: high vs. low) ANCOVAs with repeated measures on the first factor were conducted to examine the main and interactive effects of socio-economic status and number of motivational interviewing sessions on the psychological and behavioral variables before and after the intervention and physical activity status at baseline as a covariate.
Results revealed a significant main effect for time on total physical activity (F(1,199) = 42.87, p < .001, \( \eta_{\text{p}}^{2} = .18 \)), vigorous physical activity (F(1,199) = 3.48, p = .06, \( \eta_{\text{p}}^{2} = .02 \)), moderate physical activity(F(1, 199) = 10.68, p < .001, \( \eta_{\text{p}}^{2} = .05 \)),walking (F(1, 199) = 34.00, p < .001, \( \eta_{\text{p}}^{2} = .15 \)),stages of change (F(1,198) = 115.41, p < .001, \( \eta_{\text{p}}^{2} = .37 \)), self-efficacy (F(1,193) = 4.99, p = .03, \( \eta_{\text{p}}^{2} = .03 \)), social support-friends (F(1,190) = 23.23, p < .001, \( \eta_{\text{p}}^{2} = .11 \)), and social support-family (F(1,189) = 33.61, p < .001, \( \eta_{\text{p}}^{2} = .15 \)); a significant main effect for socio-economic status on self-efficacy (F(1,193) = 5.87, p = .016, \( \eta_{\text{p}}^{2} = .03 \)); a significant time x attendance status interaction effect on total physical activity (F(1,199) = 8.32, p = .004, \( \eta_{\text{p}}^{2} = .04 \)), vigorous physical activity (F(1,199) = 5.04, p = .03, \( \eta_{\text{p}}^{2} = .03 \)), walking (F(1,199) = 4.87, p = .03, \( \eta_{\text{p}}^{2} = .02 \)),stages of change (F(1,198) = 10.07, p = .002, \( \eta_{\text{p}}^{2} = .05 \)), and social support-family (F(1,189) = 3.38, p = .07, \( \eta_{\text{p}}^{2} = .02 \)); and a significant time × socioeconomic status interaction effect on perceived behavioral control (F(1,193) = 12.52, p < .001, \( \eta_{\text{p}}^{2} = .06 \)).
The ANCOVAs indicate that the intervention was effective in increasing physical activity levels, as well as the psychological mediators, as evidenced by the main effects for time supporting our primary hypotheses. Importantly, the significant interaction effects for time and attendance provides sharp confirmation of the increased effectiveness of the intervention on the physical activity and key psychological variables among participants who attended 2 h or more of motivational interviewing sessions relative to those who attended 1 h or less. In addition, there were relatively few interactive effects of the intervention and socio-economic status on the psychological variables and no effects on the behavioral outcomes indicating that the effect of the intervention on the behavioral variables was relatively uniform across socio-economic status. In sum, considering the raft of psychological variables measured in the current study, it is apparent that the salient effects are those for the intervention, and its interaction with attendance, on the behavioral outcomes and key psychological mediators.
The time × attendance interaction effect on physical activity notwithstanding, it is important to note that the intervention was still effective among lower attendees. We also conducted a follow-up analysis to establish a more fine-grained examination of the relationship between number of sessions attended and change in physical activity. We therefore used a one-way ANOVA to further explore the effect of motivational interviewing dose (1 to 6 sessions) on total physical activity change. A significant dose–response relationship was found (F (5, 194) = 4.74, p < .001, \( \eta_{\text{p}}^{2} = 0.11 \)) such that the higher the number of motivational interviewing consultations, the greater the increase in physical activity. Post hoc least significant difference tests were conducted to identify the location of the differences. Table 3 displays the difference scores for mean change in total physical activity (MET-minutes) for groups defined by number of motivational interviewing consultations attended. The main trends indicate that differences lie between the lower sessions (1 and 2) and higher sessions (4 and 5). There were no significant differences found between 1 and 2 sessions or between 1 or 2 and 3 sessions. Furthermore, there were generally no significant differences in total physical activity change for those attending 6 sessions compared to those attending 2, 3, 4, or 5 sessions. Therefore, the data suggests that the optimal number of motivational interviewing consultations to increase total physical activity appears to be four or five sessions.
Finally, hierarchical regression analyses were conducted to explore the predictors of change in physical activity between baseline and 6-month follow-up. Prior to the analyses, we computed zero-order correlations among study variables in order to check for potential problems associated with multicolinearity. The correlations are presented in Table 4. We found no correlations of a magnitude substantive enough to warrant concern and therefore proceeded with the analyses. The design of the regression was such that demographic and non-psychological variables (gender, age estimation, socio-economic status, number of motivational interviewing consultations) were entered in the first step, change in psychological variables from the theory of planned behavior, transtheoretical model and social support variables were entered in the second step, and finally, change in relative autonomy from self-determination theory was included in the final step. This regression model was used in each analysis predicting the four physical activity outcome variables (total physical activity, vigorous physical activity, moderate physical activity, and walking).
Focusing first on the model with total physical activity as the dependent variable, results indicated that the overall model predicted 28.3 % of the variance in total physical activity (R2 = .28, F (11,174) = 6.25, p < .001). The only predictor in the first step was number of motivational interviewing consultations (β = 0.31, p < .001). In the second step, change in stage of change was a significant predictor (β = 0.38, p < .001) along with number of consultations (β = 0.20, p < .01). The inclusion of the relative autonomy index in the final step resulted in no significant step change in the R2 leaving number of sessions (β = 0.21, p < .01) and change in stage of change (β = 0.37, p < .001) as the only significant predictors.
For vigorous physical activity, the overall model predicted 16.0 % of the variance in physical activity change (R2 = .16, F (1,211, 177) = 3.05, p < .001). The number of sessions was the only significant predictor is the first step (β = 0.18, p < .05). Change in attitudes (β = 0.29, p < .001), perceived behavioral control (β = 0.19, p < .05), social support (friends) (β = 0.23, p < .01), and age (β = −0.18, p < .05) along with number of consultations (β = 0.18, p < .05) significantly predicted vigorous physical activity change in step two. In the final step, there was no significant increase in amount of variance explained. Change in perceived behavioral control (β = 0.19, p < .05), attitudes (β = 0.33, p < .001), social support (friend) (β = 0.25, p < .01), and number of sessions (β = 0.17, p < .05) significantly predicted vigorous physical activity change.
For moderate physical activity, the overall model predicted 9 % of the variance in physical activity change and the overall equation was not significant (R2 = .09, F (11,177) = 1.54, p = .12). There were no predictors except for change in stage of change at steps two and three (final β = 0.19, p < .05), but this effect was relatively small.
Finally, the overall model predicted 21.0 % of the variance in walking change (R2 = 0.21, F (11,177) = 4.27, p < .001). In step one, number of sessions was a significant predictor (β = 0.29, p < .01). Number of sessions (β = 0.20, p < .01), change in stage of change (β = 0.28, p < .001), and social support (friends) (β = 0.17, p < .05) were significant predictors at step two. In the final step, there was no significant increment in the R2 value such that number of sessions (β = 0.20, p < .01), change in stage of change (β = 0.28, p < .001), and change in social support (friends) (β = 0.16, p < .05) were the only significant predictors of changes in walking.
Discussion
The three aims of the current study were to (1) investigate the effectiveness of using motivational interviewing within the primary care setting to increase physical activity amongst lower socio-economic status groups; (2) examine the degree of support needed to facilitate physical activity; and (3) explore the social-psychological and motivational predictors of physical activity behavioral change. In summary, there were significant increases in total physical activity, walking, vigorous physical activity, stage of change, and social support from baseline to follow-up. High attendees significantly increased total physical activity, walking, stage of change and family social support and reduced external regulation compared to low attendees. The social-psychological and motivational predictors of change in total physical activity were stage of change and number of motivational interviewing consultations. Predictors for walking were change in stage of change, social support friends, and number of consultations. The predictors of change in vigorous physical activity included change in attitudes, perceived behavioral control, social support, and number of motivational interviewing consultations.
In relation to the first aim, the significant increase in physical activity at 6-months found in the present research corroborates the findings of similar studies that have found motivational interviewing to lead to significant increases in physical activity (Benbassat et al., 2008; Hardcastle et al., 2008). Findings of the current study are in contrast to some studies that have reported null findings for the effect of intensive motivational interviewing (e.g., 3 to 6 sessions) on physical activity compared to standard care (Whittemore et al., 2009; Groeneveld et al., 2010). To speculate, possible reasons for this difference may lie in variations in methodological approach and study design. In terms of methodological approach, there are clear differences in the intensiveness of the training of the facilitators. For example, the lifestyle change facilitators in the present study received a total of 6 days training compared to the 3 days cited by Groeneveld et al. (2010). Furthermore, it seems that the facilitators in the current research had greater experience compared to other studies. For example, the facilitators employed in the present study had been implementing motivational interviewing for over 6 months prior to the start of data collection while facilitators in the Groeneveld et al. study underwent a 6-week pilot in which to practice motivational interviewing. It is therefore possible that motivational interviewing experience may have contributed to the differences in intervention effectiveness observed across these studies. However, it is also important to note that the current study adopted a non-controlled design while those finding null effects (e.g., Groeneveld et al., 2010) included a control group, precluding the ability to make definitive comparisons that unequivocally point to facilitator training and experience as moderating factors.
Our findings suggest that motivational interviewing is effective in facilitating physical activity behavior change in lower socio-economic status groups and is in contrast with previous research that has found interventions to increase physical activity in low socio-economic status groups to be of limited effectiveness or ineffective (Yancey et al., 2006; Dutton et al., 2007; Keyserling et al., 2008). Although the current sample was recruited from areas with overall high social deprivation, we went to some effort to ensure that our participants could be characterised as members of a ‘lower’ socio-economic status group; the majority (69 %) of the sample were classified into this group based on our primary criterion of household income, followed by employment status and education. We used this classification to control for the effect of variations in socio-economic status in all analyses. However, the sample as a whole could be considered representative of lower socio-economic status. Indeed, the UK national household income has been calculated to be between £32,000 and £36,000 (Oguz & Knight, 2010) and, in the current study, 76 % of participants declared a household income of less than £30,000.Footnote 2 This is unsurprising given that Hastings (the recruitment area) ranks amongst the 10 % most deprived areas in the country (East Sussex County Council, 2010). On this basis, we are confident that the current intervention is effective in a population with predominantly low levels of socioeconomic status and comparatively high levels of social deprivation.
In relation to the second aim, the current findings support previous findings that have identified a dose–response relationship for motivational interviewing within health research (Burke et al., 2003; Rubak et al., 2005). For example, in a meta-analysis of adapted motivational interviewing in treating problem behaviors, Burke et al. (2003) found high-dose studies to yield larger effect sizes. A meta-analysis by Rubak et al. (2005) also found a significant effect in 40 % of studies with just one counselling session, but in 87 % of studies where individuals received more than five encounters. However despite such research, several authors (e.g., Bennett et al., 2008; Greaves et al., 2008) have been unable to replicate this relationship. For example, although Hardcastle et al. (2008) found high attendees (3–5 sessions) to increase their vigorous physical activity, walking, and overall physical activity compared to low attendees (2 or less MI sessions), no significant dose response relationship was identified. Another study (Harland et al., 1999) including four intensity-related intervention groups or control, also found no significant effect as a result of attending more than one motivational interviewing interview.
To our knowledge, the current study is the first to demonstrate a clear dose–response effect within physical activity research using multiple motivational interviewing intervention sessions. The optimum number of sessions would appear to be 4 or 5 h/sessions of motivational interviewing. High attendees also reported significantly increased stage of change and perceived family social support across the intervention compared to low attendees. This provides some preliminary evidence that the intervention had an impact on key psychological mediators of physical activity change amongst high attendees.
A lack of research on the active ingredients of motivational interviewing (Burke et al., 2003) has made it difficult to draw firm conclusions regarding how motivational interviewing facilitates behavior change. In relation to the final aim, the current study sought to explore the predictors of physical activity behavior change, and, in particular, the degree to which change in autonomous motivation from self-determination theory, change in attitudes and perceived behavioral control from the theory of planned behavior, change in self-efficacy and social support (social cognitive theory) and change in motivational readiness (transtheoretical model) predicted change in physical activity. The main psycho-social predictors of physical activity change were number of sessions and change in stage of change. The finding that change in stage of change predicted physical activity change (both for total physical activity and walking) is consistent with a central purpose of motivational interviewing; that is, to increase client readiness to change (Miller & Rollnick, 2002).
Change in stage of change, social support (from friends and family) and self-efficacy were the key psychological variables that significantly increased as a result of the intervention. This is consistent with the theoretical underpinnings of motivational interviewing and the common strategies adopted within motivational interviewing. Specifically, we would expect readiness to change (and hence motivation) to increase given the emphasis placed on strategies to build motivation for change including agenda setting, decisional balance, assessing importance and eliciting change talk. ‘Two possible futures’ was also used as a tool to build motivation for change by evoking and strengthening patient’s personal reasons for change. According to Rollnick et al. (2008) increasing client confidence is an explicit aim of motivational interviewing and self-efficacy has been implicated as a key mediator of change in behavioral outcomes. For example, one of the key principles of motivational interviewing is that of supporting self-efficacy (by empowering the patient and encouraging optimism and hope) and key strategies include the assessment of confidence, confidence building, positive feedback, and development of appropriate goals.
Recent research has also shown motivational interviewing to significantly increase self-efficacy within self-management of diabetics (Chen et al., 2011) and in the area of substance abuse (Rohsenow et al., 2004). The finding that social support significantly increased in the current study is not unsurprising given the supportive and relational elements of motivational interviewing. Rollnick and Miller (1995) describe the ‘spirit’ of motivational interviewing to be a critical component of its efficacy. The ‘spirit’ is described as collaborative rather than authoritarian and one that respects the client’s autonomy. Through the expression of empathy, through exploration of client’s concerns and options and through autonomous decision-making, it is likely that patients felt supported by the lifestyle change facilitators. Adherence to the spirit of motivational interviewing has been shown to be a strong predictor of behavior change (Moyers et al., 2005) and it is likely that these relational aspects contribute to outcomes via feeling supported and valued. In addition, the lifestyle change facilitators may have addressed social support directly with patients and encouraged them to recruit family members and friends to support their attempts at behavior change. It may also be the case that the facilitators were considered as a ‘friend’ helping patients in their efforts to change.
The predictors of vigorous physical activity change were perceived behavioral control, social support from friends, and attitudes. These findings support previous research that perceived behavioral control is a significant predictor of physical activity behavior change (Lorentzen et al., 2007; Kamphuis et al., 2009). Meta-analyses of the theory of planned behavior applied to multiple behavioral outcomes (Armitage & Conner, 2001) and specific to physical activity (Hagger & Chatzisarantis, 2009) have shown perceived behavioral control to have a medium to large effect size with attitudes and perceived behavioral control to be significantly correlated with intention. The finding that increased social support from friends predicted change in both vigorous physical activity and walking is consistent with recent research pointing to the significance of social support in both decreasing saturated fat intake and increasing time spent in physical activity (Burke et al., 2008) and to research suggesting that social support in a key predictor of self-regulation of physical activity in older adults (Umstattd et al., 2006).
Present findings have important implications for practitioners in public health contexts with a remit to promote physical activity among people who are insufficiently or moderately active and from underprivileged backgrounds. Current results support the effectiveness of motivational interviewing to promote increased physical activity in disadvantaged communities with low levels of physical activity. The provision of motivational interviewing training among healthcare professionals tasked with promoting physical activity would also be an important endeavour. In addition, a targeted process of referral, by healthcare professionals within primary care appears to be an important pathway through which such participants gain access to motivational interviewing for health promotion. Although the current research suggests that any exposure to the intervention promoted increased physical activity, an important implication of the current study is that attendance to multiple sessions, with an optimal number appearing to be four to five sessions, leads to significantly greater physical activity participation relative to fewer sessions. Practitioners delivering motivational interviewing should, therefore, encourage patients to attend multiple sessions in order to maximise potential gains.
Strengths and limitations
The present study has numerous strengths including the adoption of a theory-based client-centred intervention technique known to be effective in changing behavior; the inclusion of a gamete of theory-based social-psychological and motivational mediators of physical activity behavior change (Dombrowski et al., 2011), and the adoption of an intention-to-treat analyses. In addition, the present study also included comprehensive training of the practitioners delivering the intervention involving advanced motivational interviewing training, ongoing supervision and feedback. Furthermore, there were five lifestyle change facilitators, collecting data across 15 practices which helps to rule out issues of research bias both in terms of practitioner and ‘type’ of patient. Finally, the intervention was conducted in a participant group from a low socio-economic status community which is a difficult to reach and insufficiently-studied group and was such that it could be easily integrated into routine practice to demonstrate good translational efficacy (Dunn, 2009). Together these unique features demonstrate the importance of the current research in contributing to knowledge and understanding of interventions to promote behavior change in physical activity in this often neglected population.
However, it would be remiss not to mention some of the limitations of the current research including the reliance on self-report measures, particularly for physical activity, and the absence of a standard-care control group. Due to organizational barriers and resource implications, the research was unable to access alternative health practices to form a control arm for the study. There were also no interim measures of the psychological variables, meaning that potential changes in the psychological variables could have been diluted due to the time lag between baseline and the 6-month follow-up. However, this time lag also had the effect of demonstrating the sustained effects of the intervention on these psychological mediators as well as providing a relatively conservative estimate of the power of the effect. Limited resources also prevented the assessment of treatment integrity over the course of the intervention. We therefore cannot guarantee that facilitator’s effectively employed motivational interviewing consistently during the intervention. However, given the intensive level of training (6 days), feedback and monitoring, as well as the 6 months experience of practicing motivational interviewing within routine consultations prior to the start of the research study, we are confident in their ability to use motivational interviewing consistently and effectively with patients.
Conclusions
The present study adds to the growing literature supporting the effectiveness of motivational interviewing in promoting physical activity behavior change, and is one of the first to demonstrate a clear dose–response relationship between motivational interviewing and physical activity change. Findings of this research contribute towards both “gaps in the evidence” in relation to brief interventions in primary care and the effect of an intervention across lower socioeconomic groups (National Institute for Health and Clinical Excellence, 2007; Blaxter, 2007), but also to a limited number of physical activity interventions targeting low income groups within the UK (Michie et al., 2009).
Notes
It is important to acknowledge that it is possible that General Practitioners may have provided some information on reasons for change during the course of their consultations with the patients prior to referral. However, this information provision would have been informal and the decision to access the lifestyle change facilitation service would be the decision of the patient. It is unlikely that the informal information given at the General Practitioner referral stage would have any lasting effect next to the more formal, intensive, focused, and systematic intervention approach used in the motivational interviewing session. The process of referral from the healthcare professional is an integral part of many one-to-one counselling approaches to behaviour change, such as motivational interviewing. The method followed in the current study therefore represents an authentic referral-intervention approach.
This is a conservative estimate given that 34 participants did not report their income and returned a ‘prefer not to say’ response. Taking the latter into consideration, it is likely that the percentage classified with an income would be higher.
References
Ajzen, I. (1985). From intentions to actions: A theory of planned behavior. In J. Kuhi & J. Beckmann (Eds.), Action-control: From cognition to behavior (pp. 11–39). Heidelberg: Springer.
Amireault, S., Godin, G., Vohl, M., & Perusse, L. (2008). Moderators of the intention behaviour and perceived behavioural control-behaviour relationships for leisure-time physical activity. International Journal of Behavioural Nutrition and Physical Activity, 5, 1–11.
Amrhein, P. C., Miller, W. R., Yahne, C. E., Palmer, M., & Fulcher, L. (2003). Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology, 71, 862–878.
Armitage, C. J., & Conner, M. (2001). Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology, 40, 471–499.
Armstrong, M. J., Mottershead, T. A., Ronksley, P. E., Sigal, R. J., Campbell, T. S., & Hemmelgarn, B. R. (2011). Motivational interviewing to improve weight loss in overweight and/or obese patients: A systematic review and meta-analysis of randomised controlled trials. Obesity Reviews, 12, 709–723.
Bandura, A. (1977). Self-efficacy: The exercise of control. New York: Freeman
Benbassat, D. O., Dos Reis, P. C., Vandriette, Y. M., De Nutte, N., & Corten, P. (2008). Motivational interviewing increases physical activity in depressed inpatients. European Psychiatry, 23, S299.
Bennett, J. A., Young, H. M., Nail, L. M., Winters-Stone, K., & Hanson, G. (2008). A telephone-only motivational intervention to increase physical activity in rural adults: A randomised controlled trial. Nursing Research, 57, 24–32.
Bertholet, N., Faouzi, M., Gmel, G., Gaume, J., & Daeppen, J. B. (2011). Change talk sequence during brief motivational intervention, towards or away from drinking. Addiction, 105, 2106–2112.
Blair, S. N. (2009). Physical inactivity: The biggest public health problem of the 21st century. British Journal of Sports Medicine, 43, 1–2.
Blair, S. N., Dunn, A. L., Marcus, B. H., Carpenter, R. A., & Jaret, P. (2001). Active living everyday: 20 weeks to lifelong vitality. Champaign, Ill: Human Kinetics.
Blaxter, M. (2007) Evidence for the effects on inequalities in health of interventions designed to change behaviour. Available online www.nice.org.uk/nicemedia/pdf/evidencefortheeffectoninequalitiesdesignedtochangebehaviour.pdf
Booth, M. (2000). Assessment of physical activity: An international perspective. Research Quarterly in Exercise and Sport, 71, 114–120.
British Heart Foundation. (2009).UK coronary heart disease statistics 2009–2010. London: British Heart Foundation.
Brug, J., Spikmans, F., Aartsen, C., Breedveld, B., Bes, R., & Ferreira, I. (2007). Training dietitians in basic motivational interviewing skills results in changes in their counseling style and in lower saturated fat intakes in their patients. Journal of Nutrition Education and Behavior, 39, 8–12.
Burke, B. L., Arkowitz, H., & Menchola, M. (2003). The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology, 71, 843–861.
Burke, V., Beilin, L. W., Cutt, H. E., Mansour, J., & Mori, T. A. (2008). Moderators and mediators of behaviour change in a lifestyle programme for treated hypertensives: A randomized controlled trial (ADAPT). Health Education Research, 23, 583–591.
Chatzisarantis, N. L. D., & Hagger, M. S. (2009). Effects of an intervention based on self-determination theory on self-reported leisure-time physical activity participation. Psychology and Health, 24, 29–48.
Chen, S. M., Creedy, D., Lin, H. S., & Wollin, J. (2011). Effects of a motivational interviewing intervention on self-management, psychological and glycemic outcomes in type 2 diabetics: A randomised controlled trial. International Journal of Nursing Studies. doi:1016/J.iJnurstu.2011.11.011.
Courneya, K. S., & Bobick, T. M. (2000). Integrating the theory of planned behaviour with the processes and stages of change in the exercise domain. Psychology of Sport and Exercise, 1, 41–56.
Craig, C. L., Marshall, A., Sjostrom, M., Bauman, A. E., Booth, M., Ainsworth, B. E., et al. (2003). International physical activity questionnaire: 12 country reliability and validity. Medicine and Science in Sports and Exercise, 35, 1381–1395.
Craig, R., Mindell, J., & Hirani, V. (2009). Health survey for England 2008: Physical activity and fitness. Leeds: The Health and Social Care Information Centre.
Deci, E. L., Eghrari, H., Patrick, B. C., & Leone, D. R. (1994). Facilitating internalization: The self-determination theory perspective. Journal of Personality, 62, 119–142.
Deci, E. L., & Ryan, R. M. (1985). Intrinsic motivation and self-determination in human behaviour. New York: Plenum Press.
Deci, E. L., & Ryan, R. M. (2000). The “What” and “Why” of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry, 11, 227–268.
Department of Health. (2004). Choosing health; making healthier choices easier. London: The Stationary Office.
Department of Health. (2009). Be active, be healthy: A plan for getting the nation moving. London: Department of Health.
DiMarco, I. D., Klein, D. A., Clark, V. L., & Wilson, G. T. (2009). The use of motivational interviewing techniques to enhance the efficacy of guided self-help behavioral weight loss treatment. Eating Behaviors, 10, 134–136.
Dombrowski, S. U., Sniehotta, F. F., Avenell, A., Johnston, M., MacLennan, G., & Araújo-Soares, A. (2012). Identifying active ingredients in complex behavioural interventions for obese adults with additional risk factors: A systematic review. Health Psychology Review, 6, 7–32.
Dunn, A. L. (2009). The effectiveness of physical activity interventions to reduce cardiovascular disease. American Journal of Lifestyle Medicine, 3, 11S–18S.
Dutton, G. R., Martin, P. D., Welsch, M. A., & Brantley, P. J. (2007). Promoting physical activity for low-income minority women in primary care. American Journal of Health Behaviour, 31, 622–631.
East Sussex County Council. (2010). Focus on east sussex 2010 annual monitor. http://www.eastsussexinfigures.org.uk/Documents/LatestFocus.pdf
Emmons, K. M., & Rollnick, S. (2001). Motivational interviewing in health care settings: Opportunities and limitations. American Journal of Preventive Medicine, 20, 68–74.
Emmons, K. M., Stoddard, A. M., Fletcher, R., Gutheil, C., Suarez, E. G., Lobb, R., et al. (2005). Cancer prevention among working class, multiethnic adults: Results of the healthy directions-health centers study. American Journal of Public Health, 95, 1200–1205.
Everson-Rose, S. A., & Lewis, T. T. (2005). Psychosocial factors and cardiovascular diseases. Annual Review of Public Health, 26, 469–500.
Greaves, C. J., Middlebrooke, A., O’Loughlin, L., Holland, S., Poper, J., Steele, A., et al. (2008). Motivational interviewing for modifying diabetes risk: A randomised controlled trial. British Journal of General Practice, 58, 535–540.
Groeneveld, I. F., Proper, K. I., van der Beek, J. A., & van Mechelen, W. (2010). Sustained body weight reduction by an individual based lifestyle intervention for workers in the construction industry at risk for cardiovascular disease: Results of a randomised controlled trial. Preventive Medicine, 51, 240–246.
Hagger, M. S. (2009). Theoretical integration in health psychology: Unifying ideas and complimentary explanations. British Journal of Health Psychology, 14, 189–194.
Hagger, M. S., & Chatzisarantis, N. L. D. (2009). Integrating the theory of planned behaviour and self-determination theory in health behaviour: A meta-analysis. British Journal of Health Psychology, 14, 275–302.
Hardcastle, S., Taylor, A., Bailey, M., & Castle, R. (2008). A randomized controlled trial on the effectiveness of a primary health care based counselling intervention on physical activity, diet and CHD risk factors. Patient Education and Counselling, 70, 31–39.
Harland, J., White, M., Drinkwater, C., Chinn, D., Farr, L., & Howel, D. (1999). The Newcastle exercise project: A randomised controlled trial of methods to promote physical activity in primary care. British Medical Journal, 319, 828.
Hastings and Rother Primary Care Trust. (2008). Improving health, increasing life: 2007–2008, Director of public health- annual report. East Sussex, Hastings and Rother Primary Care trust.
Helmerhorst, H. J. F., Wijndaele, K., Brage, S., Wareham, N., & Ekelund, U. (2009). Objectively measured sedentary time may predict insulin resistance independent of moderate and vigorous intensity physical activity. Diabetes, 58, 1776–1779.
Huisman, M., Kunst, A. E., Bopp, M., Borgan, J. K., Borrell, C., Costa, G., et al. (2005). Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet, 365, 493–500.
James, S. A., Hoewyk, J. V., Belli, R. F., Strogatz, D. S., Williams, D. R., & Raghunathan, T. E. (2006). Life-course socioeconomic position and hypertension in African American men: The Pitt county study. American Journal of Public Health, 96, 812–817.
Kamphuis, C. B. M., van Lenthe, F. J., Giskes, K., Brug, J., & Machenbach, J. P. (2007). Perceived environmental determinants of physical activity and fruit and vegetable consumption among high and low socioeconomic groups in the Netherlands. Health and Place, 13, 493–503.
Kamphuis, C. B. M., van Lenthe, F. J., Giskes, K., Huisman, M., Brug, J., & Mackenbach, J. P. (2009). Socioeconomic differences in lack of recreational walking among adults: The role of neighbourhood and individual factors. International Journal of Behavioural Nutrition and Physical Activity, 6, 1–11.
Katzmarzyk, P. T. (2009). Sitting time and mortality from all causes, cardiovascular disease and cancer. Medicine and Science in Sports and Exercise, 41, 998–1005.
Keyserling, T. C., Hodge, C. D. S., Jilcott, S. B., Johnston, L. F., Garcia, B. A., Gizlice, Z., et al. (2008). Randomized trial of a clinic based, community-supported lifestyle intervention to improve physical activity and diet: The North Carolina enhanced WISEWOMEN project. Preventive Medicine, 46, 499–510.
Latkin, C. A., & Curry, A. (2003). Stressful neighbourhoods and depression: A prospective study of the impact of neighbourhood disorder. Journal of Health and Social Behaviour, 44, 34–44.
Lewis, B. A., Forsyth, L. H., Pinto, B. M., Bock, B. C., Roberts, M., & Marcus, B. H. (2006). Psychosocial mediators of physical activity in a randomized controlled intervention trial. Journal of Sport and Exercise Psychology, 28, 193–204.
Lorentzen, C., Ommundsen, Y., Jenum, A. K., & Holma, I. (2007). The Romsas in Motion community intervention: programme exposure and psychosocial mediated relationships to change in stages of change in physical activity. The International Journal of Behavioural Nutrition and Physical Activity, 4, 15–27.
Lowther, M., Mutrie, N., & Scott, E. M. (2002). Promoting physical activity in a socially and economically deprived community: A 12 month randomized control trial of fitness assessment and exercise consultation. Journal of Sport Sciences, 20, 577–588.
Lynch, J. W., Smith, G. D., Kaplan, G. A., & House, J. S. (2000). Income inequality and mortality: Importance on health of individual income, psychosocial environment, or material conditions. British Medical Journal, 320, 1200–1204.
Mackenbach, J. P., Stirbu, I., Roskam, A. R., Schaap, M. M., Menvielle, G., Leinsau, M., et al. (2008). Socioeconomic inequalities in health in 22 European countries. The New England Journal of Medicine, 358, 2468–2481.
Markland, D., Ryan, R. M., Tobin, V. J., & Rollnick, S. (2005). Motivational interviewing and self-determination theory. Journal of Social and Clinical Psychology, 24, 811–831.
Markland, D., & Tobin, V. J. (2005). A modification to behavioural regulation in exercise questionnaire to include an assessment of a motivation. Journal of Sport and Exercise Psychology, 26, 191–196.
Markland, D., & Vansteenkiste, M. (2007). Self-determination theory and motivational interviewing in exercise. In M. S. Hagger & N. L. D. Chatzisarantis (Eds.), Intrinsic motivation and self-determination in exercise and sport (pp. 167–180). Champaign, Ill: Human Kinetics.
Martins, R. K., & McNeil, D. W. (2009). Review of motivational interviewing in promoting health behaviours. Clinical Psychology Review, 29, 283–293.
McAuley, E. (1990). Self-efficacy measures. Unpublished raw data.
McEachan, R. R. C., Conner, M. T., Taylor, N., & Lawton, R. J. (2011). Prospective prediction of health-related behaviors with the theory of planned behavior: A meta-analysis. Health Psychology Review, 5, 97–144.
McNeill, L. H., Kreuter, M. W., & Subramanian, S. V. (2006). Social environment and physical activity: A review of concepts and evidence. Social Science and Medicine, 63, 1011–1022.
Michie, S., Jochelson, K., Markham, W. A., & Bridle, C. (2009). Low income groups and behaviour change interventions: A review of intervention content, effectiveness and theoretical frameworks. Journal of Epidemiology and Community Health, 63, 610–622.
Miller, S. T., & Beech, B. M. (2009). Rural healthcare providers question the practicality of motivational interviewing and report varied physical activity counselling experience. Patient Education and Counselling, 76, 279–282.
Miller, W. R., & Mount, K. A. (2001). A small study of training in motivational interviewing: Does one workshop change clinician and client behaviour? Behavioural and Cognitive Psychotherapy, 29, 457–471.
Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: preparing people for change (2nd ed.). New York: The Guildford Press.
Moyers, T. B., Martin, T., Manuel, J., Miller, W., & Ernst, D. (2010). Revised global scales: Motivational interviewing treatment integrity 3.1 (MITI 3.1). University of New Mexico: Center on Alcoholism, Substance Abuse and Addictions (CASSA).
Moyers, T. B., Miller, W. R., & Hendrickson, S. M. (2005). How does motivational interviewing work? Therapist interpersonal skill predicts client involvement with motivational interviewing sessions. Journal of Consulting and Clinical Psychology, 73, 590–598.
National Institute for Health and Clinical Excellence. (2007). Behaviour change at population, community and individual levels. London: NICE.
NHS East Sussex Downs and Weald. (2009). Joint Strategic Needs Assessment. Lewes: NHS East Sussex Downs and Weald ONS.
O’Loughlin, J., Paradis, G., Gray-Donald, K., & Renaud, L. (1999). The impact of a community-based heart disease prevention program in a low-income, inner-city neighbourhood. American Journal of Public Health, 89, 1819–1826.
Oguz, S., & Knight, J. (2010). Regional economic indicators with a focus on gross disposable household income. Economic and Labour Market Review, 4, 51–66.
Orbell, S., Hagger, M. S., Brown, V., & Tidy, J. (2006). Comparing two theories of health behavior: A prospective study of non-completion of treatment following cervical cancer screening. Health Psychology, 25, 604–615.
Orozco, L. J., Buchleitner, A. M., Gimeriez-Perez, G., Rogue, I., Figuls, M., Richter, B., et al. (2008). Exercise or exercise and diet for preventing type 2 diabetes mellitus. The Cochrane Library, 3, 1–3.
Parks, S. E., Housemann, R. A., & Brownson, R. C. (2003). Differential correlates of physical activity in urban and rural adults of various socioeconomic backgrounds in the United States. Journal of Epidemiology and Community Health, 57, 29–35.
Parra-Medina, D., Wilcox, S., Wilson, D. K., Addy, C. L., Felton, G., & Poston, M. B. (2010). Heart healthy and ethnically relevant (HHER) lifestyle trial for improving diet and physical activity in underserved African American women. Contemporary Clinical Trials, 31, 92–104.
Prochaska, J. O., & Diclemente, C. C. (1983). Stages and processes of self-change of smoking: Towards an integrative model of change. Journal of Consulting and Clinical Psychology, 51, 390–395.
Resnicow, K., Jackson, A., Wang, T., De, A. K., McCarthy, F., Dudley, W. N., et al. (2001). A motivational interviewing intervention to increase fruit and vegetable intake through black churches: Results of the eat for life trial. American Journal of Public Health, 9, 1686–1693.
Ridge, K., Treasure, J., Forbes, A., Thomas, S., & Ismail, K. (2012). Themes elicited during motivational interviewing to improve glycaemic control in adults with Type 1 diabetes mellitus. Diabetic Medicine, 29, 148–152.
Rohsenow, D. J., Monti, P. M., Martin, R. A., Colby, S. M., & Myers, M. G. (2004). Motivational enhancement and coping skills training for cocaine abusers: Effects on substance abuse outcomes. Addiction, 99, 862–874.
Rollnick, S. (1997). Whither motivational interviewing? Journal of Substance Misuse, 2, 1–2.
Rollnick, S., & Miller, W. R. (1995). What is motivational interviewing? Behavioural and Cognitive Psychotherapy, 23, 325–334.
Rollnick, S., Miller, W. R., & Butler, C. (2008). Motivational interviewing in Health Care. Helping people change behaviour. New York: Guilford Press.
Rosamond, W. D., Ammerman, A. S., Holliday, J. L., Tawney, K. W., Hunt, K. J., Keyserling, T. C., et al. (2000). Cardiovascular disease risk factor intervention in low-income women: The North Carolina WISEWOMAN project. Preventive Medicine, 31, 370–379.
Rubak, S., Sandbaek, A., Lauritzen, T., & Christensen, B. (2005). Motivational interviewing: A systematic review and meta-analysis. British Journal of General Practice, 55, 305–312.
Ryan, R. M., & Connell, J. P. (1989). Perceived locus of causality and internalization: Examining reasons for acting in two domains. Journal of Personality and Social Psychology, 57, 749–761.
Saavedra, J. M., Torres, S., Caro, B., Escalante, Y., De la Cruz, E., Duran, M. J., et al. (2008). Relationship between health-related fitness and education and income levels in Spanish Women. Public Health, 122, 794–800.
Sallis, J. F., Grossman, R. M., Pinski, R. B., Patterson, T. L., & Nader, P. R. (1987). The development of scales to measure social support for diet and exercise behaviours. Preventive Medicine, 16, 825–836.
Sallis, J. F., Saelens, B. E., Frank, L. D., Conway, T. L., Slymen, D. J., Cain, K. L., et al. (2009). Neighbourhood built environment and income: Examining multiple health outcomes. Social Science and Medicine, 68, 1285–1293.
Shaikh, A. R., Vinokur, A. D., Yaroch, A. L., Williams, G. C., & Resnicow, K. (2011). Direct and mediated effects of two theoretically based interventions to increase consumption of fruits and vegetables in the healthy body healthy spirit trial. Health Education and Behaviour, 38, 492–501.
Stamatakis, E., & Chaudhury, M. (2008). Temporal trends in adults’ sports participation patterns in England between 1997 and 2006: The health survey for England. British Journal of Sports Medicine, 42, 901–908.
Steptoe, A. L., Perkins-Porras, E. A., McKay, C., Rink, E., Hilton, S., & Cappuccio, F. P. (2003). Behavioural counselling to increase consumption of fruit and vegetables in low income adults: Randomised trial. British Medical Journal, 326, 855–858.
Sykes, C. M., & Marks, D. F. (2001). Effectiveness of a cognitive behaviour therapy self-help programme for smokers in London. Health Promotion International, 16, 255–260.
The Health and Social Care Information Centre. (2010). Statistics on obesity, physical activity and diet. Leeds: The Health and Social Care Information Centre.
The IPAQ Group. (2012). International physical activity questionnaire. Retrieved March 1, 2012, from http://www.ipaq.ki.se/
Umstattd, M. R., Saunders, R., Wilcox, R., Volois, R. F., & Dowda, M. (2006). Correlates of self-regulation for physical activity among older adults. American Journal of Health Behaviour, 30, 710–719.
Walpole, B., Dettmer, E., Morrongiello, B., McCrindle, B., & Hamilton, J. (2011). Motivational Interviewing as an intervention to increase adolescent self-efficacy and promote weight loss: Methodology and design. BMC Public Health, 11, 459.
Warburton, D. E. R., Nicol, C. W., & Bredin, S. S. D. (2006). Health benefits of physical activity: The evidence. Canadian Medical Association Journal, 174, 801–809.
West, D. S., DiLillo, V., Bursac, Z., Gore, S. A., & Greene, P. G. (2007). Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care, 30, 1081–1087.
Whittemore, R., Melkus, G., Wagner, J., Dziura, J., Northrup, V., & Grey, M. (2009). Translating the diabetes prevention program to primary care: A pilot study. Nursing Research, 58, 2–12.
Williams, G. C. (2002). Improving patients’ health through supporting the autonomy of patients and providers. In E. L. Deci & R. M. Ryan (Eds.), Handbook of self-determination research (pp. 233–254). Rochester, NY: University of Rochester Press.
Williams, G. C., Cox, E. M., Kouides, R., & Deci, E. L. (1999). Presenting the facts about smoking to adolescents: The effects of an autonomy supportive style. Archives of Paediatrics and Adolescent Medicine, 153, 959–964.
Wolin, K. Y., Yan, Y., Colditz, G. A., & Lee, I. M. (2009). Physical activity and colon cancer prevention: A meta- analysis. British Journal of Cancer, 100, 611–616.
Wood, D. A., Kotseva, K., Connolly, S., Jennings, C., Mead, A., Jones, J., et al. (2008). Nurse-coordinated multidisciplinary, family based cardiovascular disease prevention programme for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: A paired, cluster-randomised controlled trial. The Lancet, 371, 1999–2012.
Yancey, A. K., Ory, M. G., & Davis, S. M. (2006). Dissemination of physical activity promotion interventions in underserved populations. American Journal of Preventive Medicine, 31, S82–S91.
Acknowledgments
The authors thank Hastings and Rother Primary Care Trust who provided the funding to support the study, the healthcare professionals who recruited patients, the lifestyle change facilitators, and the patients who volunteered to take part in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hardcastle, S., Blake, N. & Hagger, M.S. The effectiveness of a motivational interviewing primary-care based intervention on physical activity and predictors of change in a disadvantaged community. J Behav Med 35, 318–333 (2012). https://doi.org/10.1007/s10865-012-9417-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-012-9417-1