Abstract
Benefits of anti-retroviral therapy (ART) depend on consistent HIV care attendance. However, appointment non-adherence (i.e. missed appointments) is common even in programs that reduce financial barriers. Demographic, health/treatment, and psychosocial contributors to appointment non-adherence were examined among men who have sex with men (MSM) attending HIV primary care. Participants (n = 503) completed questionnaires, and HIV biomarker data were extracted from medical records. At 12 months, records were reviewed to assess HIV primary care appointment non-adherence. Among MSM, 31.2% missed without cancellation at least one appointment during 12-month study period. Independent predictors (P < 0.05) were: low income (OR = 1.87); African American (OR = 3.00) and Hispanic/Latino (OR = 4.31) relative to non-Hispanic White; depression (OR = 2.01); and low expectancy for appointments to prevent/treat infection (OR = 2.38), whereas private insurance (OR = 0.48) and older age (OR = 0.94) predicted lower risk. Low self-efficacy predicted marginal risk (OR = 2.74, P = 0.10). The following did not independently predict risk for non-adherence: education, relationship status, general health, time since HIV diagnosis, ART history, post-traumatic stress disorder, HIV stigma, or supportive clinic staff. Appointment non-adherence is prevalent, particularly among younger and racial/ethnic minority MSM. Socioeconomic barriers, depression and low appointment expectancy and self-efficacy may be targets to increase care engagement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For HIV-infected individuals, the benefits of anti-retroviral therapy (ART) depend on consistent access to HIV care. Routine medical visits allow providers to assess markers of disease progression and treatment response and to monitor adverse effects. Visits also present opportunities to reinforce medication adherence and HIV prevention messages (Centers for Disease Control and Prevention [CDCP], 2003; Fisher et al., 2006; Gardner et al., 2008). However, while visits are recommended to be every three to four months for most adults on ART (CDCP, 2003), suboptimal appointment adherence is common (Giordano et al., 2003, 2007; Israelski et al., 2001; Mellins et al., 2003; Mugavero et al., 2009a, b; Sohler et al., 2007). A recent study of HIV primary care patients reported that 40% missed at least one in every four visits (Mugavero et al., 2009a).
Missed appointments have extensive implications. At the practice level, they disrupt staff productivity (Fischer et al., 2009; Moore et al., 2001). Reduced efficiency presents a burden for systems in which staff and financial resources are already limited. At the provider level, missed appointments impede continuity of care (Torian & Wiewel, 2011) and influence decision-making such as inclusion of patients in HIV clinical trials (King et al., 2007). For patients, missed appointments predict elevated risk for HIV progression (Berg et al., 2005; Mugavero et al., 2009a; Park et al., 2007; Rastegar et al., 2003) and excess mortality (Giordano et al., 2007; Mugavero et al., 2009b), independent of demographic and medical risk factors.
Given the risks of HIV care disengagement, more work is needed to identify predictors of missed appointments. This research has been conducted more extensively in other medical settings (e.g., general practice, diabetes care), and a number of factors have emerged. For one, socioeconomic barriers consistently predict poorer appointment adherence (Neal et al., 2001; Trenouth & Hough, 1991; Van der Meer & Loock, 2008). Living alone may also be a risk factor (Fischer et al., 2009). Among psychological factors, depression is one of the largest predictors of missed appointments (Cashman et al., 2004; Weinger et al., 2005). Patient-reported self-efficacy has also received attention as a consistent predictor of adherence to self-care behaviors and a target of chronic disease management models (Curtin et al., 2008; Sol et al., 2011; Swendeman et al., 2009); however, this work has not identified whether self-efficacy predicts appointment adherence in particular. In the few studies that assessed other patient perceptions, more missed appointments were found among those who perceived that prescribed treatments would not be effective (i.e. low outcome expectancy; Fischer et al., 2009).
Limited research in HIV supports that socioeconomic factors such as public health insurance status (Mugavero et al., 2009a) and lower income (Israelski et al., 2001) increase risk for HIV care disengagement. Younger patients (Catz et al., 1999; Giordano et al., 2007; Israelski et al., 2001; Mugavero et al., 2009b), those of racial minority status (Israelski et al., 2001; Mugavero et al., 2009a), and those who are not on ART (Bodenlos et al., 2007) may also be at greater risk. With regard to psychological factors, depression has been suggested to elevate risk (Weiser et al., 2006) although other work has not found this relationship (Bodenlos et al., 2007). Understanding the impact of depression is important because individuals with HIV are at least three times as likely to experience depression relative to the general population (Asch et al., 2003; Bing et al., 2001). Other emerging evidence indicates that perceptions of poorer support from HIV care providers present barriers to appointment adherence (Bakken et al., 2000; Beach et al., 2006). While HIV stigma outside of the clinic also has been linked with poorer treatment adherence (Stutterheim et al., 2011) and retention in care (McGuire et al., 2010), the association of HIV stigma specifically with appointment adherence has not yet been tested.
Current evidence supporting psychosocial risk factors in HIV should be interpreted with caution. For one, non-adherence is often measured for periods preceding the patient assessment, precluding causal inference. Much of this work also has not adjusted adequately for the influence of control variables such as socioeconomic factors. Furthermore, while depression has received some attention, other relevant psychiatric conditions such as post-traumatic stress disorder (PTSD) remain overlooked. As with depression, PTSD prevalence (10–54%) is higher than general population rates, particularly among HIV subgroups such men who have sex with men (MSM; Kelly et al., 1998; Kessler et al., 2005; Tsao et al., 2004). Since anxiety can increase withdrawal in stressful situations (Kagan et al., 1989, 1987; Rosenbaum et al., 1983; van Ameringen et al., 1998), it is plausible that MSM with PTSD may miss appointments to avoid activating negative affect (Martin & Knox 1997).
Objective
Links between socioeconomic factors and patient care disengagement have been established across chronic illnesses, including HIV (Mugavero et al., 2009a; Neal et al., 2001; Trenouth & Hough, 1991; Van der Meer & Loock, 2008). However, as prior researchers have noted, reducing the financial burden of HIV care is not enough to increase engagement among at-risk patients (Giordano et al., 2003; Kissinger et al., 1995). The current study aimed to identify risk factors for missed HIV primary care visits, to inform efforts toward increasing care engagement. To extend prior work, HIV-relevant factors including demographic (younger age, racial minority status, living alone), health/treatment (poor health, no ART history, shorter duration since HIV diagnosis), psychiatric (depression, PTSD), and patient perception factors (HIV stigma, poor support from clinic staff, low appointment expectancy, and low self-efficacy for keeping appointments) were tested as risk factors for appointment non-adherence over a 12-month period, controlling for socioeconomic indicators.
This study focused specifically on MSM in HIV primary care. In the US, MSM continue to account for over half of new HIV infections and the largest group of people living with HIV, and they are the only group in which new infections have consistently increased over the past two decades (CDCP, 2010). As HIV treatment-as-prevention models emerge (Cohen et al., 2011), identifying barriers and facilitators to HIV care engagement among risk groups such as MSM is a key priority in these efforts (Mayer, 2011).
Methods
Participants
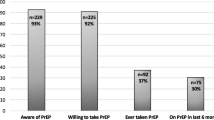
Participants were Fenway Health (FH) patients who were screened for enrollment in behavioral intervention trials related to HIV transmission risk (Knauz et al., 2007). FH is the largest outpatient HIV care provider in New England and traditionally has served sexual minority patients. Eligible patients included adults (ages 18 and older) who self-identified as MSM and who had been HIV-infected for at least 3 months.
Study design
Recruitment
Between 2004 and 2007, the approximate number of HIV primary care patients seen per annum at FH was 1,100. During this window, we recruited FH patients via several methods to optimize study reach, including specific in-house recruitment drives, medical provider referrals, distribution of study flyers throughout FH, and informational tables set up in clinic lobbies. Research assistants also approached patients at HIV primary care clinic appointments. Adult patients (ages 18 and older) who self-identified as MSM and who had been HIV-infected for at least 3 months were invited to complete a screening assessment at FH.
Participation
All participants signed institutional review board-approved informed consent forms prior to study screening. As part of the screening assessment, participants completed a computer-assisted questionnaire that included demographic items, mental health screens, and perceptions about healthcare and HIV. Participants received monetary compensation for time and effort. Data on HIV biological markers were extracted from electronic medical records, using the most proximate clinical report within a 3-week window to each participant’s screening date. At 12 months post-assessment, medical records were reviewed again by trained study staff to assess appointment attendance. For the current analysis we utilized assessment and medical record data from all participants who completed the screening assessment.
Measurements
HIV medical appointment non-adherence
Data on HIV medical appointment attendance were collected from electronic medical records for the 12-month period following study assessment. Of note, Fenway provides reminder phone calls to all patients 1 day prior to their scheduled appointments. Non-adherence was defined as at least one instance in which the participant missed or did not provide 24-h cancellation notice for an appointment. Consistent with previous research, clinical subspecialty appointments and missed appointments that were cancelled in advance were not included (Catz et al., 1999; Keruly et al., 2002; Melnikow & Kiefe, 1994; Mugavero et al., 2009a). While there are several other possible strategies for defining non-adherence, the current method was selected based on prior adherence research (Mellins et al., 2003) and on evidence that one missed visit within a 1-year period was a risk factor for new AIDS-defining illness or death following ART initiation (Park et al., 2007). This method also allowed us to avoid estimating an optimal number of appointments per year for all participants, as this figure may vary based on factors such as current health status and new treatment initiation (Department of Health and Human Services, 2011). We also did not analyze non-adherence as a continuous variable as these data are not normally distributed.
Socioeconomic and demographic factors
Participants completed items on education, yearly income, health insurance type, age, relationship status, and racial/ethnic group identification.
Health and treatment factors
Subjective health was assessed by an item derived from the Medical Outcomes Study Short Form-36 (SF-36; Ware & Sherbourne, 1992); participants identified their general health on a 5-point scale from “poor” to “excellent”. Time since HIV diagnosis and history of ever being on ART were identified via self-report. Values for plasma HIV RNA concentration (copies/mL) and peripheral blood CD4+ T cell count (cells/μL) were extracted from medical records to help characterize the baseline sample.
Psychiatric screens
Brief instruments were used to screen for clinical depression and post-traumatic stress disorder (PTSD). The nine-item Patient Health Questionnaire (PHQ; (Spitzer et al., 1999) was used to assess symptom severity during the past 2 weeks. This scale has demonstrated adequate sensitivity (75%) and specificity (90%) with clinician-diagnosed major depressive disorder (MDD; Spitzer et al., 1999). For this study, PHQ criteria were used to categorize participants by depression status (0 = negative screen, 1 = positive screen).
PTSD was assessed with the SPAN (Meltzer-Brody et al., 1999), which measures the extent to which respondents were distressed by four key symptoms (Startle, Physiologic arousal, Anger, and Numbness) during the past week. In a sample of trauma survivors, these items yielded 88% accuracy with structured clinician interview (Meltzer-Brody et al., 1999). In the current study, a SPAN score ≥5 in the presence of a traumatic event was used to identify positive PTSD screens, and PTSD status was coded as: 0 = negative screen, 1 = positive screen.
Patient perceptions
Four patient perception items were selected based on prior work testing psychosocial predictors of care disengagement (Bakken et al., 2000; Beach et al., 2006; Fischer et al., 2009; Mellins et al., 2003; Park et al., 2007). HIV stigma was measured as, “I feel ashamed that I have HIV”. Perceived HIV clinic support was assessed as, “The staff at this clinic understands what it is like to live with HIV in my community”. Perceived appointment outcome expectancy was assessed as “Keeping medical appointments will prevent or quickly treat infections related to HIV”. In each case, participants were asked to indicate their agreement by selecting one of five or seven responses ranging from “strongly disagree” to “strongly agree”. Self-efficacy for appointment adherence was assessed as “How sure are you that you could always schedule and keep your HIV appointments in the next year?” Participants completed this item by selecting one of five responses ranging from “very unsure” to “very sure”. Based on non-normal data distributions, all four patient perception items were dichotomized and analyzed as categorical variables.
Data analysis
Simple (bivariate) logistic regression was used to test predictors of risk for appointment non-adherence. Factors that predicted risk of appointment non-adherence at a two-sided P < 0.25 were then entered in a multivariable logistic regression model of non-adherence. Non-adherence (0 = no missed visits, 1 = one or more missed visits) was identified as the dependent variable. A two-sided P < 0.05 was used to establish statistical significance in the multivariate model.
Results
Sample characteristics
The sample comprised 503 MSM (see Table 1). Mean participant age was 41.9 years (SD = 8.3). Participants predominantly self-identified as non-Hispanic White (NHW; 75.1%), with 11.3% as African American (AA) and 8.9% as Hispanic/Latino (H/L). More than one-half of participants had obtained a college degree (51.7%), and over one-third (35.0%) reported a yearly income of ≤$20,000. Most (77.5%) had a history of ever being on ART. At study entry, 61.2% had a CD4+ T cell count ≥400 cells/μL and 58.1% had an undetectable HIV viral load (<75 copies/mL).
Appointment adherence over the study period
During 12 months post-assessment, 157 participants (31.2%) were appointment non-adherent. Specifically, 71 (14.1%) missed one appointment, 39 (7.8%) missed two, 17 (3.4%) missed three, 11 (2.2%) missed four, and 19 (3.8%) missed five or more.
Bivariate analyses
Several predictors of non-adherence were identified (see Table 2). Among the socioeconomic indicators, both lower income (<$20,000; OR = 2.77, 95% CI = 1.87–4.11) and lower education level (<bachelors degree; OR = 2.30, 95% CI = 1.56–3.39) predicted greater risk of non-adherence, whereas having private/HMO insurance predicted lower risk relative to public or no insurance (OR = 0.33, 95% CI = 0.22–0.48).
Among other demographic factors, older age predicted lower risk (OR = 0.94, 95% CI = 0.92–0.97) and AA and H/L participants showed greater risk relative to NHW participants (AA: OR = 2.61, 95% CI = 1.48–4.61; H/L: OR = 2.17, 95% CI = 1.15–4.07). Overall, 27.0% of NHW, 44.4% of H/L, and 49.1% of AA were non-adherent. Having no domestic partner/spouse marginally predicted greater risk (OR = 1.51, 95% CI = 0.98–2.31).
Health/treatment factors showed mixed results. Reporting fair or poor health (versus good, very good or excellent health) predicted greater risk for non-adherence (OR = 2.01, 95% CI = 1.17–3.45) whereas time since HIV diagnosis (OR = 0.96, 0.97–1.02) and history of ever being on ART (OR = 0.72, 95% CI = 0.47–1.13) did not predict risk of non-adherence.
Among non-adherent participants, 21.3 and 41.3% screened positive for clinical depression and PTSD, respectively, compared with 9.2 and 31.8% of adherent participants. Positive screens for depression (OR = 2.67, 95% CI = 1.56–4.57) and for PTSD (OR = 1.51, 95% CI = 1.01–2.26) each predicted greater risk for non-adherence.
With regard to patient perceptions, 60.9% of non-adherent participants reported HIV stigma compared with 52.8% of adherent participants. Both groups reported high rates of clinic staff support (non-adherent = 91.0%, adherent = 87.8%), appointment expectancy for preventing/treating infections (non-adherent = 88.2%, adherent = 93.5%) and self-efficacy for keeping all scheduled appointments (non-adherent = 84.3%, adherent = 92.3%). Among these factors, lower appointment expectancy (OR = 1.93, 95% CI = <1.00–3.71) and lower self-efficacy (OR = 2.24, 95% CI = 1.24–4.05) predicted greater risk for non-adherence. HIV stigma marginally predicted greater risk for non-adherence (OR = 1.40, 95% CI = 0.95–2.05) whereas perceived staff support did not predict risk (OR = 0.72, 95% CI = 0.38–1.35).
Multivariable logistic regression analysis
In the multivariable model, a number of factors remained independent predictors of risk for non-adherence (see Table 2). Among socioeconomic indicators, lower income (≤$20,000) remained a risk factor (OR = 1.87, 95% CI = 1.06–3.30) whereas having private/HMO insurance (versus public, other or no insurance) remained a protective factor (OR = 0.48, 95% CI = 0.27–0.85). Lower education (<bachelor’s degree) did not predict risk for non-adherence (OR = 1.35, 95% CI = 0.82–2.20).
With regard to other demographic and health/treatment factors, older age predicted lower risk for non-adherence (OR = 0.94, 95% CI = 0.91–0.97) whereas living without a domestic partner did not predict risk (OR = 0.90, 95% CI = 0.53–1.53). AAs (OR = 3.00, 95% CI = 1.50–5.99), and H/Ls (OR = 2.14, 95% CI = 1.04–4.40) showed greater risk relative to NHWs. Subjective health (OR = 1.06, 95% CI = 0.53–2.13) and history of being on ART (OR = 0.96, 95% CI = 0.55–1.68) did not predict risk of non-adherence.
Among psychiatric variables and patient perceptions, MSM who screened positive for clinical depression were approximately two times as likely as those with negative screens to be non-adherent (OR = 2.01, 95% CI = 1.01–3.99) whereas screening positive for PTSD did not predict risk (OR = 1.09, 95% CI = 0.66–1.79). Low appointment expectancy (OR = 2.38, 95% CI = 1.07–5.30) predicted greater risk for non-adherence whereas self-efficacy for keeping appointments predicted marginal risk (OR = 1.35, 95% CI = 0.89–3.80). HIV stigma did not predict risk for non-adherence (OR = 1.35, 95% CI = 0.83–2.20).
Discussion
The current study examined non-adherence to HIV primary care visits among MSM in care at Fenway Health (FH). During the year following study assessment, almost one-third of participants missed at least one appointment without cancelling. This rate is consistent with prior work showing that appointment non-adherence is common in HIV-infected groups (Giordano et al., 2003, 2007; Israelski et al., 2001; Mellins et al., 2003; Mugavero et al., 2009a, b; Sohler et al., 2007). This study is also the first to extend findings to HIV-infected MSM specifically.
Controlling for college degrees, non-adherent MSM had higher prevalence of income falling at or below $20,000 and lower prevalence of private/HMO insurance coverage relative to adherent MSM. These findings are not surprising, given that socioeconomic factors are key predictors of missed appointments (Israelski et al., 2001; Mugavero et al., 2009a; Neal et al., 2001; Palacio et al., 1999; Trenouth & Hough, 1991; Van der Meer & Loock, 2008). However, HIV appointment non-adherence persists even in programs that reduce financial barriers to care (Giordano et al., 2007; Kissinger et al., 1995; Sohler et al., 2007), highlighting the need to identify additional risk factors in the context of socioeconomic disadvantage.
Among demographic factors, younger age and racial/ethnic minority status (African American and Hispanic/Latino versus non-Hispanic White) independently predicted elevated risk for appointment non-adherence. These findings support that the risks associated with age and racial/ethnic minority status cannot be solely explained by socioeconomic factors. The association of younger age with appointment non-adherence has been reported in prior work (Catz et al., 1999; Israelski et al., 2001); researchers have speculated that younger patients may be less adherent due to irregular schedules or lower perceived susceptibility to sickness (Catz et al., 1999), although these hypotheses have not been tested. Determinants of racial/ethnic group differences in appointment non-adherence also merit more attention. Mugavero et al. (2009a) reported that higher rates of appointment non-adherence among African Americans relative to non-Hispanic Whites partially explained racial disparities in rates of virologic failure. Other work has suggested that elevated rates of disease progression among African Americans and Hispanics/Latinos reflect both greater delays in initiation of ART and lower treatment adherence (Giordano et al., 2010). As African Americans and Hispanic/Latinos are disproportionately infected with HIV and underrepresented in clinical trials (CDCP, 2008; Gifford et al., 2002), strategies to increase access and engage patients in treatment early on may be critical to reducing disparities in HIV outcomes.
The current results further substantiate that depression may be a key factor in care disengagement (Cashman et al., 2004; Weinger et al., 2005; Weiser et al., 2006), independent of socioeconomic status. MSM who screened positive for clinical depression were approximately two times as likely to be non-adherent than those with negative screens. Depression assessment and management is part of current standard care guidelines at FH. However, it is plausible that hopelessness and self-isolation may lead MSM with depression to disengage from care. Missed appointments, in turn, decrease opportunities for providers to detect and treat depression, creating a cycle with downstream effects on HIV health. Prior work has shown that cognitive-behavioral therapy can be adapted to improve both depression and medication adherence in HIV (Safren et al., 2009). Current findings show that this dual target approach may be relevant to a range of self-care behaviors including care engagement.
In comparison to screens for depression, positive PTSD screens were more prevalent in the non-adherent group relative to the adherent group but did not independently predict risk for non-adherence in the multivariable model. This study was the first to test this relationship, and more work is needed to understand how PTSD may impact barriers to HIV care. For instance, it is possible that some symptoms (e.g., hypervigilance) may preserve health behaviors whereas others (e.g., withdrawal) may increase risk. The importance of this work is highlighted by the high prevalence of trauma history and PTSD among HIV-infected MSM; in the current sample, 41% of non-adherent MSM and 32% of adherent MSM screened positive for this disorder.
With regard to patient perceptions, low appointment expectancy predicted higher risk for non-adherence. This finding extends prior work examining perceptions of care (Beach et al., 2006; Fischer et al., 2009). Results suggest that education about the purpose of HIV care may hold benefit as a target for change. Findings also showed that more than half of the sample endorsed shame about being HIV-infected. However, the overwhelming majority felt the clinic staff understood the challenges of living with HIV, and neither factor independently predicted adherence status. Importantly, while MSM were highly likely to endorse that they would be able to keep all scheduled appointments during the next year, this belief was only marginally related to subsequent risk for non-adherence. Intervening to enhance problem-solving skills may increase care engagement for patients whose perceived health efficacy does not translate to actual behaviors.
Current findings should be interpreted with attention to study limitations. This study focused on MSM in care at FH, and it is unknown whether results would generalize to other groups or to MSM in other types of care settings. Also, since recruitment was conducted on-site at FH during a 3.5-year recruitment window, more frequent visit attendance might have increased the likelihood of being approached for recruitment, leading to possible underestimation of non-adherence in this study sample. Within the current sample, patient perceptions were such that most MSM endorsed good health, positive attitudes about staff, and strong sense of appointment expectancy and self-efficacy. This relative lack of variability, as well as limited psychometric data supporting these items may have limited our ability to detect actual risks associated with these perceptions.
For the current analysis, hypothesized risk factors were selected based on prior research but do not represent an exhaustive list. Other suggested influences such as co-infection with hepatitis C (Giordano et al., 2003) or practical barriers such as lack of transportation to clinic visits were not addressed. Furthermore, we did not collect data on patient-reported reasons for non-adherence, and some missed appointments may have reflected specific circumstances such as inpatient hospitalizations of which the clinic was not advised. It is possible that risk factors for appointment non-adherence may vary among subsets of patients such as those with or without serious health problems or cognitive or functional impairment related to HIV and comorbid conditions. These hypotheses should be tested in future work identifying risk factors for appointment adherence and subsequent HIV outcomes.
In sum, findings indicate that missing HIV medical appointments is prevalent among HIV-infected MSM, even in settings where clinic staff members are perceived as supportive and sexual minority stigmatization is minimized. Socioeconomic barriers to care need to be addressed but represent only a portion of risk for care disengagement. MSM who are younger or of racial/ethnic minority status are at greater risk for missing appointments, independent of socioeconomic factors. Depression and low appointment expectancy and self-efficacy represent risks that may be amenable to intervention. The current findings help identify patients who may benefit from more intensive assessment and intervention to reduce depression symptoms and problem-solve healthcare barriers.
References
Asch, S. M., Kilbourne, A. M., Gifford, A. L., Burnam, M. A., Turner, B., Shapiro, M. F., et al. (2003). Underdiagnosis of depression in HIV: Who are we missing? Journal of General Internal Medicine, 18, 450–456.
Bakken, S., Holzemer, W. L., Brown, M. A., Powell-Cope, G. M., Turner, J. G., Inouye, J., et al. (2000). Relationships between perception of engagement with health care provider and demographic characteristics, health status, and adherence to therapeutic regimen in persons with HIV/AIDS. AIDS Patient Care and STDS, 14, 189–197.
Beach, M. C., Keruly, J., & Moore, R. D. (2006). Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? Journal of General Internal Medicine, 21, 661–665.
Berg, M. B., Safren, S. A., Mimiaga, M. J., Grasso, C., Boswell, S., & Mayer, K. H. (2005). Nonadherence to medical appointments is associated with increased plasma HIV RNA and decreased CD4 cell counts in a community-based HIV primary care clinic. AIDS Care, 17, 902–907.
Bing, E. G., Burnam, M. A., & Longshore, D. (2001). Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry, 58, 721–728.
Bodenlos, J. S., Grothe, K. B., Whitehead, D., Konkle-Parker, D. J., Jones, G. N., & Brantley, P. J. (2007). Attitudes toward health care providers and appointment attendance in HIV/AIDS patients. Journal of the Association of Nurses in AIDS Care, 18, 65–73.
Cashman, S., Savageau, J., Lemay, C., & Ferguson, W. (2004). Patient health status and appointment keeping in an urban community health center. Journal of Health Care for the Poor and Underserved, 15, 474–488.
Catz, S. L., McClure, J. B., Jones, G. N., & Brantley, P. J. (1999). Predictors of outpatient medical appointment attendance among persons with HIV. AIDS Care, 11, 361–373.
Centers for Disease Control and Prevention. (2003). Incorporating HIV prevention into the medical care of persons living with HIV. Recommendations of CDC, the Health Resources and Services Administration, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recommendations and Reports, 52(RR-12), 1–24.
Centers for Disease Control and Prevention. (2008). HIV prevalence–United States, 2006. MMWR, 57, 1073–1076.
Centers for Disease Control and Prevention. (2010). HIV among gay, bisexual and other men who have sex with men (MSM). Available at: http://www.cdc.gov/hiv/topics/msm/pdf/msm.pdf. Accessed September 25, 2010.
Cohen, M. S., Chen, Y. Q., McCauley, M., Gamble, T., Hosseinipour, M. C., Kumarasamy, N., et al. (2011). Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine, 365, 493–505.
Curtin, R. B., Walters, B. A., Schatell, D., Pennell, P., Wise, M., & Klicko, K. (2008). Self-efficacy and self-management behaviors in patients with chronic kidney disease. Advances in Chronic Kidney Disease, 15, 191–205.
Department of Health and Human Services. (2011). Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Retrieved from http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf
Fischer, M. J., Scharloo, M., Abbink, J. J., van ‘t Hul, A. J., van Ranst, D., Rudolphus, A., et al. (2009). Drop-out and attendance in pulmonary rehabilitation: the role of clinical and psychosocial variables. Respiratory Medicine, 103, 1564–1571.
Fisher, J. D., Fisher, W. A., Cornman, D. H., Amico, R. K., Bryan, A., & Friedland, G. H. (2006). Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. Journal of Acquired Immune Deficiency Syndrome, 41, 44–52.
Gardner, L. I., Marks, G., O’Daniels, C. M., Wilson, T. E., Golin, C., Wright, J., et al. (2008). Implementation and evaluation of a clinic-based behavioral intervention: Positive steps for patients with HIV. AIDS patient care and STDs, 22, 627–635.
Gifford, A. L., Cunningham, W. E., Heslin, K. C., Andersen, R. M., Nakazono, T., Lieu, D. K., et al. (2002). Participation in research and access to experimental treatments by HIV-infected patients. New England Journal of Medicine, 346, 1373–1382.
Giordano, T. P., Bartsch, G., Zhang, Y., Tedali, E., Absalon, J., Mannheimer, S., et al. (2010). Disparities in outcomes for African American and Latino subjects in the flexible initial retrovirus suppressive therapies (FIRST) trial. AIDS Patient Care and STDs, 24, 287–295.
Giordano, T. P., Gifford, A. L., White, A. C., Jr., Suarez-Almazor, M. E., Rabeneck, L., Hartman, C., et al. (2007). Retention in care: A challenge to survival with HIV Infection. Clinical Infectious Diseases, 44, 1493–1499.
Giordano, T. P., White, A. C., Jr., Sajja, P., Graviss, E. A., Arduino, R. C., Adu-Oppong, A., et al. (2003). Factors associated with the use of highly active antiretroviral therapy in patients newly entering care in an urban clinic. Journal of Acquired Immune Deficiency Syndromes, 32, 399–405.
Israelski, D., Gore-Felton, C., Power, R., Wood, M. J., & Koopman, C. (2001). Sociodemographic characteristics associated with medical appointment adherence among HIV-seropositive patients seeking treatment in a county outpatient facility. Preventive Medicine, 33, 470–475.
Kagan, J., Reznick, J. S., & Gibbons, J. (1989). Inhibited and uninhibited types of children. Child Development, 60, 838–845.
Kagan, J., Reznick, J. S., & Snidman, N. (1987). Physiology and psychology of behavioral inhibition. Child Development, 58, 1459–1473.
Kelly, B., Raphael, B., Judd, F., Perdices, M., Kernutt, G., Burnett, P., et al. (1998). Posttraumatic stress disorder in response to HIV infection. General Hospital Psychiatry, 20, 345–352.
Keruly, J. C., Conviser, R., & Moore, R. D. (2002). Association of medical insurance and other factors with receipt of antiretroviral therapy. American Journal of Public Health, 92, 852–857.
Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., & Walters, E. E. (2005). Prevalence, severity and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62, 617–627.
King, W. D., Defreitas, D., Smith, K., Andersen, J., Perry, L. P., & Adeyemi, T. (2007). Attitudes and perceptions of AIDS clinical trials group site coordinators on HIV clinical trial recruitment and retention: A descriptive study. AIDS Patient Care and STDS, 21, 551–563.
Kissinger, P., Cohen, D., Brandon, W., Rice, J., Morse, A., & Clark, R. (1995). Compliance with public sector HIV medical care. Journal of the National Medical Association, 87, 19–24.
Knauz, R. O., Safren, S. A., O’Cleirigh, C., Capistrant, B. D., Driskell, J. R., Aguilar, D., et al. (2007). Developing an HIV-prevention intervention for HIV-infected men who have sex with men: Project enhance. AIDS and Behavior, 5, S117–S126.
Martin, J. I., & Knox, J. (1997). Loneliness and sexual risk behavior in gay men. Psychological Reports, 81, 815–825.
Mayer, K. H. (2011). Antiretrovirals for HIV prevention: Translating promise into praxis. Lancet, 378, 206–208.
McGuire, M., Muyenyembe, T., Szumilin, E., Heinzelmann, A., Le Paih, M., Bouithy, N., et al. (2010). Vital status of pre-ART and ART patients defaulting from care in rural Malawi. Tropical Medicine and International Health, 15, 55–62.
Mellins, C. A., Kang, E., Leu, C. S., Havens, J. F., & Chesney, M. A. (2003). Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care and STDS, 17, 407–416.
Melnikow, J., & Kiefe, C. (1994). Patient compliance and medical research: Issues in methodology. Journal of General Internal Medicine, 9, 96–105.
Meltzer-Brody, S. E., Churchill, E., & Davidson, J. R. T. (1999). Derivation of the SPAN: A brief diagnostic screening test for post-traumatic stress disorder. Psychiatry Research, 88, 63–70.
Moore, C. G., Wilson-Witherspoon, P., & Probst, J. C. (2001). Time and money: Effects of no-shows at a family practice residency clinic. Family Medicine, 33, 522–527.
Mugavero, M. J., Lin, H. Y., Allison, J. J., Giordano, T. P., Willig, J. H., Raper, J. L., et al. (2009a). Racial disparities in HIV virologic failure: Do missed visits matter? Journal of Acquired Immune Deficiency Syndromes, 50, 100–108.
Mugavero, M. J., Lin, H. Y., Willig, J. H., Westfall, A. O., Ulett, K. B., Routman, J. S., et al. (2009b). Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clinical Infectious Diseases, 48, 248–256.
Neal, R. D., Lawlor, D. A., Allgar, V., Colledge, M., Ali, S., Hassey, A., et al. (2001). Missed appointments in general practice: Retrospective data analysis from four practices. British Journal of General Practice, 51, 830–832.
Palacio, H., Shiboski, C. H., Yelin, E. H., Hessol, N. A., & Greenblatt, R. M. (1999). Access to and utilization of primary care services among HIV-infected women. Journal of Acquired Immune Deficiency Syndromes, 21, 293–300.
Park, W. B., Choe, P. G., Kim, S. H., Jo, J. H., Bang, J. H., Kim, H. B., et al. (2007). One-year adherence to clinic visits after highly active antiretroviral therapy: A predictor of clinical progress in HIV patients. Journal of Internal Medicine, 261, 268–275.
Rastegar, D. A., Fingerhood, M. I., & Jasinski, D. R. (2003). Highly active antiretroviral therapy outcomes in a primary care clinic. AIDS Care, 15, 231–237.
Rosenbaum, A. H., Schatzberg, A. F., Jost, F. A., 3rd, Cross, P. D., Wells, L. A., Jiang, N. S., et al. (1983). Urinary free cortisol levels in anxiety. Psychosomatics, 24, 835–837.
Safren, S. A., O’cleirigh, C., Tan, J. Y., Raminani, S. R., Reilly, L. C., Otto, M. W., et al. (2009). A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychology, 28, 1–10.
Sohler, N. L., Wong, M. D., Cunningham, W. E., Cabral, H., Drainoni, M. L., & Cunningham, C. O. (2007). Type and pattern of illicit drug use and access to health care services for HIV-infected people. AIDS Patient Care and STDS, 21, S68–S76.
Sol, B. G., van der Graaf, Y., van Petersen, R., & Visseren, F. L. (2011). The effect of self-efficacy on cardiovascular lifestyle. European Journal of Cardiovascular Nursing, 10, 180–186.
Spitzer, R. L., Korenke, K., & Williams, J. B. W. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Journal of the American Medical Association, 282, 1737–1744.
Stutterheim, S. E., Bos, A. E., Shiripinda, I., de Bruin, M., Pryor, J. B., & Schaalma, H. P. (2011). HIV-related stigma in African and Afro-Caribbean communities in the Netherlands: Manifestations, consequences and coping. Psychology & Health, 1, 1–17.
Swendeman, D., Ingram, B. L., & Rotheram-Borus, M. J. (2009). Common elements in self-management of HIV and other chronic illnesses: An integrative framework. AIDS Care, 21, 1321–1334.
Torian, L. V., & Wiewel, E. W. (2011). Continuity of HIV-related medical care, New York City, 2005–2009: Do patients who initiate care stay in care? AIDS Patient Care and STDs, 25, 79–88.
Trenouth, M. J., & Hough, A. (1991). Reasons for broken and canceled appointments in a British orthodontic clinic. Journal of Clinical Orthodontics, 25, 115–120.
Tsao, J. C., Dobalian, A., Moreau, C., & Dobalian, K. (2004). Stability of anxiety and depression in a national sample of adults with human immunodeficiency virus. Journal of Nervous and Mental Disease, 192, 111–118.
van Ameringen, M., Mancini, C., & Oakman, J. M. (1998). The relationship of behavioral inhibition and shyness to anxiety disorder. Journal of Nervous and Mental Disease, 186, 425–431.
Van der Meer, G., & Loock, J. W. (2008). Why patients miss follow-up appointments: A prospective control-matched study. East African Journal of Public Health, 5, 154–156.
Ware, J. E., Jr, & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Medical Care, 30, 473–483.
Weinger, K., McMurrich, S. J., Yi, J. P., Lin, S., & Rodriguez, M. (2005). Psychological characteristics of frequent short-notice cancellers of diabetes medical and education appointments. Diabetes Care, 28, 1791–1793.
Weiser, S. D., Riley, E. D., Ragland, K., Hammer, G., Clark, R., & Bangsberg, D. R. (2006). Brief report: Factors associated with depression among homeless and marginally housed HIV-infected men in San Francisco. Journal of General Internal Medicine, 21, 61–64.
Acknowledgment
General funding for this project including data collection was from grant 5R01MH068746-05 and HRSA grant H97HA01293 to Drs. Steven A. Safren and Kenneth H. Mayer. Grant K24MH094214-01 to Dr. Steven A. Safren provided additional support for some investigator time.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Traeger, L., O’Cleirigh, C., Skeer, M.R. et al. Risk factors for missed HIV primary care visits among men who have sex with men. J Behav Med 35, 548–556 (2012). https://doi.org/10.1007/s10865-011-9383-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-011-9383-z