Abstract
Cancer patients sometimes report positive life changes in addition to more harrowing ones. Theoretically, several cognitive processes are thought to contribute to posttraumatic growth, but few studies have examined these relationships empirically among cancer patients. Moreover, most research has been conducted in western developed countries. This preliminary study offered a novel examination of posttraumatic growth and its cognitive correlates among cancer patients in western India. As hypothesized, in bivariate analyses perceived growth was significantly associated with greater meaning-focused coping (sense-making, benefit-finding), and with reappraisal of worldviews. Growth was not related to subjective appraisals regarding illness threat or stressfulness. In multivariate analyses, reappraisal of worldviews was the strongest concurrent predictor of posttraumatic growth. Results suggest that deliberative cognitive processes merit further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Research among patients with cancer and other life-threatening illnesses suggest that debilitating physical and functional changes are sometimes accompanied by unexpected positive sequelae as well. Some individuals perceive growth as well as hardship. Posttraumatic growth (Tedeschi and Calhoun 2004) is one of several related constructs (e.g., stress-related growth, Park et al. 1996; thriving, O’Leary and Ickovics 1995) used by health investigators to highlight adaptive changes in the aftermath of difficult or traumatic events. In a separate line of inquiry, health communication scholars have used the term perspective transformation to depict similar processes (Mohammed and Thombre 2005). A growing research base has documented perceived growth among cancer patients at varying phases of care, from early treatment (Manne et al. 2004) through long-term survivorship (Tomich and Helgeson 2002). These findings have contributed to a more complex understanding of adjustment to serious illness.
Mechanisms of posttraumatic growth
Although research in this area is increasing rapidly, the fundamental processes that contribute to perceived growth are not yet well understood. Theoretical models have posited a number of factors thought to influence growth (Park et al. 1996; Tedeschi and Calhoun 2004), but the empirical database is rather limited. Within the oncology setting, most studies have focused on selected demographic or medical correlates, with inconsistent results (e.g., Bellizzi and Blank 2006; Harrington et al. 2008; Kinsinger et al. 2006; Lechner et al. 2003; Tomich and Helgeson 2004; Widows et al. 2005). Other investigations have begun to explore psychosocial factors that might influence perceived growth among cancer patients. A few studies examined associations with intrusive ideation, which is often construed as an indicator of automatic (as opposed to deliberative) cognitive processing. Most studies reported null findings (Carboon et al. 2005; Cordova et al. 2001; Manne et al. 2004; for exceptions see Jaarsma et al. 2006; Sears et al. 2003). Other investigations evaluated relationships between active coping strategies and growth (e.g., Bellizzi and Blank 2006; Harrington et al. 2008; Kinsinger et al. 2006; Widows et al. 2005). Overall however, there have been few theoretically-driven studies (e.g., Park et al. 2008; Sears et al. 2003; Widows et al. 2005).
One of the important factors that may influence posttraumatic growth involves illness appraisals. In Tedeschi and Calhoun’s model (2004), crises that are sufficiently severe to challenge core assumptions about the world are thought to be more conducive to growth, relative to less disruptive events. Among cancer patients, findings regarding relationships between posttraumatic growth and objective indicators of disease severity have been mixed (e.g., Harrington et al. 2008; Lechner et al. 2003; Thorton and Pererz 2006; Tomich and Helgeson 2004; Widows et al. 2005). Subjective appraisals of illness threat or stressfulness have been somewhat more consistently associated with perceived growth (Bellizzi and Blank 2006; Cordova et al. 2001; Sears et al. 2003). Not all studies have verified these relationships, however (Weiss 2004; Widows et al. 2005), and further research clearly is warranted.
Posttraumatic growth is also hypothesized to be influenced in important ways by coping processes. Recently there has been particular interest in the use of meaning-focused coping strategies (Park 2004; Park and Folkman 1997) in response to life-threatening illness. Two distinct approaches to deriving meaning in adversity were described by Davis et al. (1998): (1) making sense of the experience and (2) finding benefit in it. Sense-making concerns attempts to comprehend the event, to make it coherent or understandable. Benefit finding involves discovering positive implications or possibilities. These distinctions seem consistent with the work of other investigators within the fields of psychology and health communications, including the categories of “meaning as comprehensibility” and “meaning as significance” proposed by Janoff-Bulman and Frantz (1997), and the stages of “exploration/experimentation” and “consolidation of new meaning” described by Mohammed and Thombre (2005). Different approaches to meaning-focused coping appear to have distinct relationships with distress (Davis et al. 1998; Neimeyer et al. 2006), but their associations with posttraumatic growth are unclear. In particular, few investigations have examined the role of sense-making in contributing to growth among cancer patients (Manne et al. 2004); both sense-making and benefit-finding merit further study.
An additional process that is thought to play a central role in posttraumatic growth concerns a reevaluation of worldviews. A life crisis may challenge core cognitive schemas, rupturing tacit assumptions about the world or disrupting important goals (Janoff-Bulman 1992). Theoretically, the process of revising one’s worldviews in a way that can better accommodate the traumatic event is viewed as an important pathway to growth (Tedeschi and Calhoun 2004). Nevertheless, some investigators have questioned the degree to which posttraumatic growth is driven by this process of schema disruption and repair (McMillen 2004; Park 2004; Wortman 2004). Among the very few studies that examined these relationships, there was little evidence that posttraumatic growth was tied to major alterations in core schemas or worldviews (Carboon et al. 2005; Park 2004; Park and Fenster 2004). Notably however, these investigations focused on the content of core beliefs (e.g., perceptions of benevolence or justice), rather than the extent to which these beliefs had been violated and reevaluated in response to stressful events. Recent studies are beginning to examine more explicitly this process of schema rupture and reappraisal (Cann et al. 2009; Park 2008). Among leukemia patients, for example, higher levels of posttraumatic growth were associated with greater perceived disruption and reconsideration of core beliefs (Cann et al. 2009). Further research is needed to explore the importance of reevaluating goals and worldviews as a determinant of growth. Thus, the current study sought to examine some of the theoretically-salient cognitive processes that might contribute to perceived growth, including illness appraisals, meaning-focused coping, and reevaluation of worldviews.
Posttraumatic growth among Indian cancer patients
There has been limited research on posttraumatic growth among cancer patients outside of western industrialized nations (Ho et al. 2004; Schroevers and Teo 2008). In particular, we are aware of no studies that have focused on perceived growth among Indian oncology patients. The experience of severe illness would be expected to be influenced in important ways by the healthcare system and broader cultural-religious context in which patients are embedded. Notwithstanding rapid advances, the Indian healthcare system presents significant challenges for many cancer patients. Most individuals are diagnosed with advanced disease, though screening efforts are growing (Dinshaw et al. 2005). Access to specialized oncology care is more limited than access to general medical services, and there are notable geographic and socioeconomic disparities in treatment (Chopra 2001; Kurian 2007; Okonkwo et al. 2008). Psychosocial support services are uncommon.
At the same time, posttraumatic growth might be facilitated by distinct aspects of Indian culture. Strong kinship bonds are often an invaluable source of support for patients (Mehrotra and Sukumar 2007). Religious beliefs may offer an additional resource. The dominant tradition in India (which is home to many faiths) is Hinduism. In a previous qualitative study, we examined cognitive and cultural-religious processes associated with perceived growth among recently-diagnosed patients (Thombre and Sherman 2009a). For many, efforts to find meaning were related to a cyclical understanding of life as a continuum of birth, death, and rebirth (a tenet implicit in the Hindu tradition). Moreover, sense-making was often colored by culturally-embedded perceptions of dharma (the duties that characterize one’s particular phase of the lifecycle) and karma (the consequences of one’s previous good and bad actions). There is a need for additional research regarding perceived growth in distinctive cultural contexts (Abraido-Lanza et al. 1998; Ho et al. 2004; Taku et al. 2008), such as India.
Current study
The current study examined posttraumatic growth and theoretically-important cognitive processes among cancer patients in western India. We evaluated patients at a similar phase of care—those who had recently started treatment for non-metastatic disease. Drawing on the conceptual models of Tedeschi and Calhoun (2004), Park and Folkman (1997), and Davis et al. (1998) we hypothesized that higher levels of posttraumatic growth (or “perspective transformation”) would be associated with (1) more threatening illness appraisals (i.e., stressfulness and fear of recurrence), (2) increased meaning-focused coping (i.e., sense-making and benefit-finding), and (3) reappraisal of worldviews (i.e., reconsideration of important global beliefs). This preliminary international project was intended to establish a foundation for a subsequent longitudinal investigation.
Method
Participants
Participants were 61 patients with nonmetastatic disease who were receiving treatment at the Ruby Hall Clinic Cancer Center in Pune, India. Inclusion criteria required that participants were within 6 months of starting active treatment for non-metastatic (i.e., stages I–III) breast, lung, or head and neck cancer. These diseases were selected due to their high prevalence in India and reasonable survival rates over the near-term (Dinshaw et al. 2005). There were no restrictions on type of treatment regimen. Exclusion criteria included cognitive impairment, illiteracy, severe psychiatric disturbance, age < 20 years, or severely impaired performance status. Three patients (5%) declined participation. Two additional patients were excluded from the analyses because the diagnosis was not among the eligible disease sites. The study was approved by the ethics review boards of the cancer center and the investigator’s university.
Sample characteristics are summarized in Table 1. Most participants were of Maharashtrian or Gujarati ethnicity, consistent with the demographic profile of the Pune region. Most had non-recurrent disease and were currently receiving chemotherapy or radiotherapy. The sample was diverse with respect to education, income, and gender.
Procedure
Participants were recruited from consecutive patients receiving services at the cancer center clinics; after being screened for eligibility by research nurses, they were informed about the project, signed a written consent statement, and completed questionnaires.
Measures
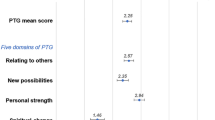
Posttraumatic growth
A modified version of the Posttraumatic Growth Inventory (PTGI, Tedeschi and Calhoun 1996) was used to assess perceived positive changes in response to the illness. The PTGI provides a total score as well as subscale scores in 5 domains. This instrument has demonstrated evidence of good internal consistency and construct validity in several studies with cancer patients (e.g., Cordova et al. 2001; Weiss 2004). Pilot-testing was undertaken to examine the feasibility and acceptability of the measure among Indian cancer patients; results indicated that participants had difficulty understanding the original 6-point Likert scale (“did not experience this change” to “experienced this change to a very great degree”). Consequently, the response format was simplified to a 3-point scale (“did not experience this change,” “not sure,” “did experience this change”), which was more comprehensible and acceptable to participants. The total score was used in the current study. Coefficient alpha for the revised instrument was .75. Moreover, patient scores were significantly correlated with family caregiver’s proxy ratings on the same measure (r = .28, P < .05), as well as a modified version of the Benefit-Finding scale (Antoni et al. 2001) (r = .50, P < .0001), supporting the convergent validity of the revised PTGI in this population (Thombre and Sherman 2009b).
Illness appraisals
Subjective appraisals of illness were assessed by a composite of two single-item measures drawn from Vinokur et al. (1990): (1) how stressful is the illness for you at the present time, and (2) how much does your illness make you feel uncertain about the future. Participants responded on a 5-point Likert scale (“not at all” to “a great deal”); coefficient alpha was .62. The Fear of Recurrence Scale was used as an additional measure of illness appraisals. This scale includes 3 items (e.g., “how often do you think about the possibility of your illness getting worse or coming back?”), which patients rate on a 5-point scale (“not at all” to “extremely”); this measure was developed by David Cella and has been used in prior studies with cancer patients (Bishop et al. 2007). In the current study, coefficient alpha was .74.
Meaning-focused coping
Meaning-based coping was assessed by two items drawn from Davis et al. (1998): (1) sense-making (“do you feel that you’ve been able to make sense of the illness”) and (2) benefit-finding (“have you found anything positive in this experience”). Participants responded to these items on a 4-point Likert scale (“not at all” to “a great deal”). In the Davis et al. study, these items were framed as open-ended questions and the coded responses demonstrated good predictive validity. We used a Likert scale format for these items in previous research with hematological cancer patients, which supported the construct validity of this approach (Sherman et al. 2009). Similar single-tem measures have been used in other investigations (e.g., Neimeyer et al. 2006; Thompson 1991; Tomich and Helgeson 2002). In the current study, the correlation between the sense-making and benefit-finding items was moderate (r = .56), suggesting that they tap overlapping but distinct dimensions of meaning.
Worldviews
Reevaluation of worldviews in response to the illness was assessed by the Core Beliefs Inventory (Cann et al. 2009). The instrument includes a series of core beliefs that might be disrupted by stressful events. Respondents were asked to consider each of these items, using the stem “how much has your illness led you to seriously examine your assumptions about …. (e.g., “the meaning of your life;” “your sense of your abilities, strengths, and weaknesses”). This measure has demonstrated good internal consistency, test–retest reliability, and construct validity (Cann et al. 2009). In pilot testing with Indian cancer patients, the instrument was modified by simplifying the response format from a 6-point scale to a 3-point scale (“no,” “not sure,” and “yes”), and by deleting 2 items which participants found less relevant and rarely endorsed. Coefficient alpha for the revised 7-item scale was .76.
Demographic and clinical variables
Participants completed a demographic form, and clinical variables were drawn from medical records and history forms completed by the patients.
Statistical analysis
Descriptive statistics were used to summarize responses to the PTGI. Preliminary analyses examined associations between PTGI scores and background demographic and medical variables, using Pearson correlations, t-tests, or analyses of variance, as appropriate. Bivariate associations between the PTGI and the predictor variables (i.e., illness appraisals, meaning-focused coping, and reappraisal of worldviews) were assessed using Pearson correlations. Variables that were significantly related to the PTGI scores were then modeled in multiple regression analyses, which controlled for any demographic or clinical variables that were significant in preliminary analyses. Distributions were checked for normality, and 3 outliers were removed from analyses regarding the PTGI. P-values less than .05 were considered significant; at this initial phase of research no adjustments were made for multiple comparisons. Power was adequate (.78–.89) to detect moderate correlations (r = .35–.40).
Results
Descriptive data and preliminary analyses
Descriptive statistics for the study variables are listed in Table 2. On average, participants scored near the midpoint on illness appraisal items, denoting moderate levels of stress/uncertainty and fear of recurrence, as might be expected at this phase of treatment. They reported relatively high levels of disrupted worldviews as a result of the illness. Average levels of posttraumatic growth were modest (below the midpoint). Bivariate analyses indicated that PTGI scores were not significantly associated with any of the demographic variables assessed (i.e., age, education, income, gender, religious affiliation, ethnicity; all P’s ≥ .12). Patients with a history of disease recurrence reported higher levels of posttraumatic growth than those with non-recurrent disease (P < .05). None of the other clinical characteristics were significantly related to PTGI scores (i.e., disease site, time since initial diagnosis, chemotherapy, radiotherapy; surgery, all P’s ≥ .06). Therefore, recurrence status was included as a covariate in the multivariate analyses.
Associations between perceived growth and cognitive predictor variables
Contrary to expectations, PTGI scores were not significantly related to either of the illness appraisal measures (i.e., stress/uncertainty, fear of recurrence) in bivariate analyses (see Table 3). Consistent with study hypotheses, PTGI scores were significantly associated with the two indices of meaning-focused coping: sense-making and benefit-finding (Table 3). Finally, as predicted, the PTGI was significantly associated with reevaluation of worldviews.
These relationships were further examined in multiple regression analyses, which examined the relative strength of the cognitive variables in predicting posttraumatic growth, controlling for recurrence status. Reevaluation of worldviews emerged as the only significant predictor of PTGI scores (see Table 4).Footnote 1
Discussion
As far as we are aware, this study is among the first to evaluate posttraumatic growth (or “perspective transformation”) in an Indian cancer population. We sought to address gaps in the literature by examining theoretically important cognitive processes that have received limited empirical attention, within a cultural setting that has rarely been studied. Our prior qualitative study suggested that perceptions of growth were not uncommon among the patients we interviewed, and appeared to be related to reevaluation of worldviews, meaning-focused coping, and illness appraisals (Thombre and Sherman 2009a). The current study used quantitative methodology to assess these processes among patients drawn from a different cancer center.
Reevaluation of worldviews
The extent to which an alteration in worldviews is intrinsic to the process of posttraumatic growth remains an area of uncertainty and debate (McMillen 2004; Park 2004; Wortman 2004). In the current study, patients reported the degree to which they had been seriously reevaluating or reconsidering their worldviews— this process of reflection was significantly associated with increased growth, consistent with the model of Tedeschi and Calhoun (2004). In multivariate analyses, this was the strongest predictor of perceived growth. These findings are consonant with those of a recent study of leukemia patients (Cann et al. 2009). In contrast, posttraumatic growth was not associated with longitudinal changes in worldviews in a study of hematological cancer patients (Carboon et al. 2005). However, that investigation examined the content of core beliefs, rather than perceived violations and active reconsideration of those beliefs in response to illness. It appears that the process of deliberative reflection (“cognitive work”) is the more salient element in propelling posttraumatic growth, at least for some individuals (Cann et al. 2009; Taku et al. 2008; Tedeschi and Calhoun 2004). The importance of active cognitive processing was also evident in a previous qualitative study of Indian cancer patients, who portrayed growth as a decidedly effortful and deliberative process rather than an automatic or reflexive one (Thombre and Sherman 2009a). Ultimately of course, a more rigorous demonstration of the role of reappraising worldviews in promoting posttraumatic growth will require additional longitudinal research.
The particular worldviews that might be challenged by serious illness would be expected to vary across cultural settings (Pals and McAdams 2004). In the current study, participants did not report strong violations in their expectations about the fairness or personal controllability of life (these items had to be eliminated during pilot testing due to limited relevance). In contrast, reappraisals regarding social roles and relationships, religious convictions, and the meaning of life were endorsed much more frequently—findings which seem consistent with the collectivist and spiritual values of Indian culture (Markus and Kitayama 1991; Miller et al. 1990). In future studies, investigators who seek to assess disrupted worldviews may wish to expand existing instruments (Cann et al. 2009; Park 2008) to encompass more culturally diverse goals and beliefs (e.g., social duties and obligations) (Markus and Kitayama 1991).
Sense-making and benefit-finding
Finding meaning in the illness, by making sense of the experience or discerning benefits in it, were both tied to increased posttraumatic growth in bivariate analyses. In Davis et al.’s (1998) conceptual model, coping strategies geared toward achieving a more complete understanding of the traumatic event (i.e., sense-making) are among the factors thought to contribute to favorable adjustment. Few investigations have examined associations between sense-making and growth. In a study of American breast cancer patients, contemplating reasons for the illness (i.e., a type sense-making) was prospectively associated with increased posttraumatic growth (Manne et al. 2004). Outside of the oncology literature, some studies have examined a broader construct—deliberative cognitive processing (i.e., purposeful reflection about the event and its implications), which similarly was associated with increased growth in some cases (e.g., Nolen-Hoeksema and Davis 2004; Taku et al. 2008). There is a need for more fine-grained analyses that focus specifically on sense-making, using more differentiated assessments (e.g., information-seeking, casual attributions for illness, reliance on religious explanatory systems, downward and upward social comparisons, reaffirmation of unrelated worldviews) (Heine et al. 2006; Park and Folkman 1997).
Finding benefits is another dimension of meaning-focused coping that is expected to contribute to perceived growth (Davis et al. 1998; Park and Folkman 1997; Sumalla et al. 2009). In the current study, individuals who found positive implications in their illness reported higher levels of posttraumatic growth in bivariate analyses. It would be helpful for future investigations to examine more specific components of benefit-finding (e.g., identification of relational, personal, or existential benefits) at particular phases of care—these efforts might have a more distinctly interpersonal focus in Asian, relative to white North American, cultural settings.
Notably, our measures of sense-making and benefit-finding captured only part of the process of meaning-focused coping. Recent theoretical models have distinguished between seeking meaning versus found meaning in stressful circumstances (Park et al. 2008; Steger et al. 2008; Thompson and Janigian 1988). Seeking and found meaning appear to have different relationships with psychosocial outcomes (e.g., Tomich and Helgeson 2002). In the current study, our indices of sense-making (i.e., achieving greater understanding) and benefit-finding (i.e., identifying positive consequences) focused predominantly on found meaning. That is, they reflect coping outcomes more than coping efforts. Found meaning in illness represents a complex and understudied target of inquiry (Park et al. 2008; Thompson 1991), which is conceptually distinct from a global sense of meaning in life. At the same time, there is also a need for further research regarding seeking (vs. attained) meaning in illness, and future studies should assess each of these dimensions.
Illness appraisals
Contrary to expectations, subjective appraisals of illness threat were not associated with posttraumatic growth in the current investigation. Tedeschi and Calhoun’s (2004) model posits that severely disruptive events may be more likely to rupture implicit assumptions and drive the process of growth (see also Janoff-Bulman 1992). We did not find significant links between PTGI scores and perceived stressfulness/uncertainty or fear of recurrence. On the other hand, patients with a history of recurrent disease reported greater growth than those with non-recurrent disease, which is consistent with the model. Previous findings have been mixed regarding connections between growth and objective indices of disease severity (Harrington et al. 2008; Lechner et al. 2003; Thorton and Pererz 2006; Tomich and Helgeson 2004; Widows et al. 2005), though most of these studies focused on tumor stage or prognosis rather than recurrence. Further work is required to explore the impact of subjective and objective threat on perceived growth, and the factors that might modify these relationships (e.g., optimism, social support, socioeconomic status, cultural context).
This preliminary study sheds light on correlates of perceived growth among Indian oncology patients undergoing active treatment. Strengths of this project included the novel population, the theoretical foundation of the inquiry, and the assessment of patients at a similar phase of care. This initial investigation has important limitations however. There is uncertainty as to how best to interpret reports of perceived growth on standardized measures such as the PTGI. Accounts of growth are subject to recall biases and self-enhancement processes (e.g., McFarland and Alvaro 2000; Widows et al. 2005), making it difficult to differentiate genuine life changes from illusory perceptions. In the current project, patient self-reports were modestly but significantly correlated with proxy ratings from family members, which provide some support for their validity. Nonetheless, future research would benefit by including prospective assessment of positive outcomes (Tennen and Affleck 2009). Additionally, it was necessary to adapt some of our assessment instruments (i.e., PTGI, core beliefs inventory) for use in this population, by simplifying the response formats. Although the modified measures demonstrated acceptable internal consistency and were related to other constructs in the expected manner, the truncated response format may have restricted variability in these measures, and thus our results may provide conservative estimates of the magnitude of these relationships.
The cross-sectional design of the current study precludes causal or temporal inferences regarding relationships between perceived growth and its cognitive correlates. Longitudinal studies would be important at the next phase of research, to provide more rigorous tests of these relationships. It is unlikely that active, deliberative cognitive processes are the only pathway to growth; some individuals report positive changes that seem to emerge automatically, without reflection or effort (McMillen 2004; Tedeschi and Calhoun 2004). Continued research is needed to explore myriad other personal and contextual factors that may contribute to these outcomes among patients with severe illness (e.g., social support, communication within the family, emotional processing, and cultural/religious narratives regarding illness).
Another limitation is that the current study included patients with varying disease sites and treatment regimens. We did not find differences in posttraumatic growth among these subgroups in our modest sample; moreover, results were unchanged when we excluded the small number with recurrent disease. Clearly, however, future studies should focus on larger, more medically homogenous samples. Finally, we evaluated patients early in the course of treatment; a number of previous studies have found indications of perceived growth at early phases of care (e.g., Affleck et al. 1987; Manne et al. 2004; Thombre and Sherman 2009a). However, one would anticipate that perceptions of growth, and their associations with cognitive processes, would vary at different phases of treatment. For example, sense-making may be more strongly tied to outcomes early in the recovery process, while benefit-finding may play a more prominent role at later phases (Davis et al. 1998; Janoff-Bulman and Frantz 1997). Similarly, in the current study, average levels of growth seemed relatively modest, while reappraisal of worldviews seemed more pronounced; higher levels of growth might be evident at a later point in recovery, perhaps in part due to the process of reevaluating core beliefs that patients had pursued initially. Additional work is needed to explore determinants of growth across the full trajectory of treatment and long-term survivorship.
In sum, the current study found partial support for associations between perceived growth (or “perspective transformation”) and theoretically important cognitive processes among cancer patients in western India. Active cognitive strategies, including reevaluation of worldviews and meaning-making coping (i.e., sense-making and benefit-finding), warrant careful attention in future research.
Notes
Regression analyses were repeated after excluding the few patients with recurrent disease, in order to evaluate effects in a more homogenous sample; findings were unchanged. Analyses were also repeated controlling for radiotherapy, which had been marginally associated with PTGI scores in bivariate analyses; again, results were the same.
References
Abraido-Lanza, A. F., Guier, C., & Colon, R. M. (1998). Psychological thriving among Latinas with chronic illness. Journal of Social Issues, 54, 405–424.
Affleck, G., Tennen, H., Croog, S., & Levine, S. (1987). Casual attribution, perceived benefits, and morbidity following a heart attack. Journal of Consulting and Clinical Psychology, 55, 29–35.
Antoni, M. H., Lehman, J. M., Kibourn, K. M., Boyers, A. E., Culver, J. L., Alferi, S. M., et al. (2001). Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology, 20, 20–32.
Bellizzi, K. M., & Blank, T. O. (2006). Predicting posttraumatic growth in breast cancer survivors. Health Psychology, 25, 47–56.
Bishop, M. M., Beaumont, J. L., Han, E. A., Cella, D., Andrykowski, M. A., Brady, M. J., et al. (2007). Late effects of cancer and hematopoietic stem-cell transplantation on spouses or partners compared with survivors and survivor-matched controls. Journal of Clinical Oncology, 25, 1402–1411.
Cann, A., Calhoun, L. G., Tedeschi, R. G., Kilmer, R. P., Gil-Rivas, V., Vishnevsky, T., & Danhauer, S. C. (2009). The core beliefs inventory: A brief measure of disruption in the assumptive world. Anxiety, Stress, & Coping, 1477–2205.
Carboon, I., Anderson, V. A., Pollard, A., Szer, J., & Seymour, J. F. (2005). Posttraumatic growth following a cancer diagnosis: Do world assumptions contribute? Traumatology, 11, 269–283.
Chopra, R. (2001). The Indian scene. Journal of Clinical Oncology, 19(Suppl), 106s–111s.
Cordova, M. J., Cunningham, L. L. C., Carlson, C. R., & Andrykowski, M. A. (2001). Posttraumatic growth following breast cancer. A controlled comparison study. Health Psychology, 20, 176–185.
Davis, C. G., Nolen-Hoeksema, S., & Larson, J. (1998). Making sense of loss and benefiting from the experience: Two construals of meaning. Journal of Personality and Social Psychology, 75, 561–574.
Dinshaw, K. A., Shastri, S. S., & Patil, S. S. (2005). Cancer control programme in India: Challenges for the new millennium. Health Administrator, 17, 10–13.
Harrington, S., McGurk, M., & Llewellyn, C. D. (2008). Positive consequences of head and neck cancer: Key correlates of finding benefit. Journal of Psychosocial Oncology, 26, 43–62.
Heine, S. J., Proulx, T., & Vohs, K. D. (2006). The meaning maintenance model: On the coherence of social motivation. Personality and Social Psychological Review, 10, 88–111.
Ho, S. M. Y., Chan, C. L. W., & Ho, R. T. H. (2004). Posttraumatic growth in Chinese cancer survivors. Psycho-Oncology, 13, 377–389.
Jaarsma, T. A., Pool, G., Sanderman, R., & Ranchor, A. V. (2006). Psychometric properties of the Dutch version of the posttraumatic growth inventory among cancer patients. Psycho-Oncology, 15, 911–920.
Janoff-Bulman, R. (1992). Shattered assumptions: Toward a new psychology of trauma. New York: Free Press.
Janoff-Bulman, R., & Frantz, C. M. (1997). The impact of trauma on meaning: From meaningless world to meaningful life. In M. Power & C. R. Brewin (Eds.), The transformation of meaning in psychological therapies (pp. 91–106). New York: Wiley.
Kinsinger, D. P., Penedo, F. J., Antoni, M. H., Darin, J. R., Lechner, S., & Schneiderman, N. (2006). Psychosocial and sociodemographic correlates of benefit-finding in men treated for localized prostate cancer. Psycho-Oncology, 15, 954–961.
Kurian, N. J. (2007). Widening economic and social disparities: Implications for India. Indian Journal of Medical Research, 126, 374–380.
Lechner, S. C., Zakowski, S. G., Antoni, M. H., Greenhawt, M., Block, K., & Block, P. (2003). Do socioeconomic and disease-related variables influence benefit finding in cancer patients? Psycho-Oncology, 12, 491–499.
Manne, S., Ostroff, J., Winkel, G., Goldstein, L., Fox, K., & Grana, G. (2004). Posttraumatic growth after breast cancer: Patient, partner, and couple perspectives. Psychosomatic Medicine, 66, 442–454.
Markus, H. R., & Kitayama, S. (1991). Culture and the self: Implications for cognition, emotion, and motivation. Psychological Review, 98, 224–253.
McFarland, C., & Alvaro, C. (2000). The impact of motivation on temporal comparisons: Coping with traumatic events by perceiving personal growth. Journal of Personality and Social Psychology, 79, 327–343.
McMillen, J. C. (2004). Posttraumatic growth: What’s it all about? Psychological Inquiry, 15, 48–52.
Mehrotra, S., & Sukumar, P. (2007). Sources of strength perceived by females caring for relatives diagnosed with cancer: An exploratory study from India. Supportive Care in Cancer, 15, 1357–1366.
Miller, J. G., Bersoff, D. M., & Harwood, R. L. (1990). Perceptions of social responsibilities in India and in the United States: Moral imperatives or personal decisions? Journal of Personality and Social Psychology, 58, 33–47.
Mohammed, S. N., & Thombre, A. (2005). HIV/AIDS stories on the World Wide Web and transformative perspective. Journal of Health Communication, 10, 347–360.
Neimeyer, R. A., Baldwin, S. A., & Gillies, J. (2006). Continuing bonds and reconstructing meaning: Mitigating complications in bereavement. Death Studies, 30, 715–738.
Nolen-Hoeksema, S., & Davis, C. G. (2004). Theoretical and methodological issues in the assessment and interpretation of posttraumatic growth. Psychological Inquiry, 15, 60–64.
O’Leary, V. E., & Ickovics, J. R. (1995). Resilience and thriving in response to challenge: An opportunity for a paradigm shift in women’s health. Women’s Health: Research on Gender, Behavior, and Policy, 1, 121–142.
Okonkwo, Q. L., Draisma, G., der Kinderen, A., Brown, M. L., & de Koning, H. J. (2008). Breast cancer screening policies in developing countries: A cost-effectiveness analysis for India. Journal of the National Cancer Institute, 100, 1290–1300.
Pals, J. L., & McAdams, D. P. (2004). The transformed self: A narrative understanding of posttraumatic growth. Psychological Inquiry, 15, 65–68.
Park, C. L. (2004). The notion of growth following stressful life experiences: Problems and prospects. Psychological Inquiry, 15, 69–76.
Park, C. L. (2008). Testing the meaning making model of coping with loss. Journal of Social and Clinical Psychology, 27, 970–994.
Park, C. L., Cohen, L., & Murch, R. (1996). Assessment and prediction of stress-related growth. Journal of Personality, 64, 71–105.
Park, C. L., Edmondson, D., Fenster, J. R., & Blank, T. O. (2008). Meaning making and psychological adjustment following cancer: The mediating roles of growth, life meaning, and restored just-world beliefs. Journal of Consulting and Clinical Psychology, 76, 863–875.
Park, C. L., & Fenster, J. R. (2004). Stress-related growth: Predictors of occurrence and correlates with psychological adjustment. Journal of Social and Clinical Psychology, 23, 195–215.
Park, C. L., & Folkman, S. (1997). Meaning in the context of stress and coping. Review of General Psychology, 2, 115–144.
Schroevers, M. J. & Teo, I. (2008). The report of posttraumatic growth in Malaysian cancer patients: Relationships with psychological distress and coping strategies. Psycho-Oncology, 17, 1239–1246.
Sears, S. R., Stanton, A. L., & Danoff-Burg, S. (2003). The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping, and posttraumatic growth in women with early-stage breast cancer. Health Psychology, 22, 487–497.
Sherman, A. C., Simonton, S., Latif, U., Plante, T. G., & Anaissie, E. J. (2009). Predicting health outcomes from global meaning and illness-specific meaning among stem cell transplant patients. [abstract] Annals of Behavioral Medicine, 37(Suppl), s192.
Steger, M. F., Kashdan, T. B., Sullivan, B. A., & Lorentz, D. (2008). Understanding the search for meaning in life: Personality, cognitive style, and the dynamic between seeking and experiencing meaning. Journal of Personality, 76, 199–228.
Sumalla, E. C., Ochoa, C., & Blanco, I. (2009). Posttraumatic growth in cancer: Reality or illusion? Clinical Psychology Review, 29, 24–33.
Taku, K., Calhoun, L. G., Cann, A., & Tedeschi, R. G. (2008). The role of rumination in the coexistennce of distress and posttraumatic growth among bereaved Japanese university students. Death Studies, 32, 428–444.
Tedeschi, R. G., & Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9, 455–471.
Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18.
Tennen, H., & Affleck, G. (2009). Assessing positive life change: In search of meticulous methods. In C. L. Park, S. C. Lechner, M. H. Antoni, & A. L. Stanton (Eds.), Medical illness and positive life change (pp. 31–49). Washington, DC: American Psychological Association.
Thombre, A., & Sherman, A. C. (2009a). Understanding perspective transformation among recently diagnosed cancer patients in western India (in review).
Thombre, A., & Sherman, A. C. (2009b). Assessing posttraumatic growth among cancer patients in India. [abstract] Annals of Behavioral Medicine, 37(Suppl), s193.
Thompson, S. C. (1991). The search for meaning following a stroke. Basic and Applied Social Psychology, 12, 81–96.
Thompson, S. C., & Janigian, A. S. (1988). Life schemes: A framework for understanding the search for meaning. Journal of Social and Clinical Psychology, 7, 260–2880.
Thorton, A. A., & Pererz, M. A. (2006). Posttraumatic growth in prostate cancer survivors and their partners. Psycho-Oncology, 15, 285–296.
Tomich, P. L., & Helgeson, V. (2002). Five years later: A cross-sectional comparison of breast cancer survivors with healthy women. Psycho-Oncology, 11, 154–169.
Tomich, P. L., & Helgeson, V. S. (2004). Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychology, 23, 16–22.
Vinokur, A. D., Threatt, B. A., Vinokur-Kaplan, D., & Satariano, W. A. (1990). The process of recovery from breast cancer for younger and older patients: Changes during the first year. Cancer, 65, 1142–1154.
Weiss, T. (2004). Correlates of posttraumatic growth in married breast cancer patients. Journal of Social and Clinical Psychology, 23, 733–746.
Widows, M. R., Jacobsen, P. B., Booth-Jones, M., & Fields, K. K. (2005). Predictors of posttraumatic growth following bone marrow transplantation for cancer. Health Psychology, 24, 266–273.
Wortman, C. M. (2004). Posttraumatic growth: Progress and problems. Psychological Inquiry, 15, 81–90.
Acknowledgments
This study was supported in part by the College of Professional Studies Summer Research Fellow Grant at the University of Arkansas at Little Rock.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thombre, A., Sherman, A.C. & Simonton, S. Posttraumatic growth among cancer patients in India. J Behav Med 33, 15–23 (2010). https://doi.org/10.1007/s10865-009-9229-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-009-9229-0