We examined the effects of two physical activity modes on depressive symptoms over a 5-year period among older adults and change in physical self-esteem as a mediator of changes in depressive symptoms. Formerly sedentary, older adults (N = 174) were randomly assigned into 6-month conditions of either walking or low-intensity resistance/flexibility training. Depressive symptoms and physical self-esteem were measured before and after the 6-month intervention, and 12 and 60 months after intervention initiation. Depressive symptoms scores were decreased immediately after the intervention, followed by a sustained reduction for 12 and 60 months after intervention initiation; there was no differential pattern of change between the physical activity modes. Change in physical self-esteem predicted change in depressive symptoms. This study supports the effectiveness of an exercise intervention for the sustained reduction of depressive symptoms among sedentary older adults and physical self-esteem as a potential mediator of this effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Individuals over 65 years of age represent one of the fastest growing age groups in the U.S. (National Institute of Aging, 2002) and depression has been identified as a significant but preventable cause and consequence of disability among older adults (Penninx et al., 1998). Physical activity might be one of the most important behavioral interventions for preventing depression among older adults. Indeed, evidence from population-based epidemiological studies using either cross-sectional or prospective research designs supports an association between physical activity participation and a reduction in depression among older adults. For example, physical activity was protective for both prevalent depression and incident depression in a large sample of community-dwelling adults (N = 1,947) aged 50–94 years from the Alameda County Study (Strawbridge et al., 2002).
Additional evidence for the antidepressant effect of physical activity among older adults has been provided from a number of experimental studies (Blumenthal et al., 1999; Mather et al., 2002; McNeil et al., 1992; Penninx et al., 2002; Singh et al., 1997, 2001). For example, the effects of 16 weeks of aerobic exercise, antidepressant medication, or combined exercise and medication on depression were examined among a large sample of older adults (N = 156) diagnosed with major depressive disorder (Blumenthal et al., 1999). All three conditions resulted in similar reductions in depression scores and similar rates of remittance (i.e., those who no longer met diagnostic criteria for major depressive disorder) immediately after the intervention (Blumenthal et al., 1999). However, the remitted subjects in the exercise only group had lower rates of relapse six months after the treatment than did subjects in the other two groups (Babyak et al., 2000).
Although previous findings are encouraging, we note three primary limitations of experimental studies that have examined the antidepressant effects of physical activity among older adults. First, relatively few studies have included a long-term follow-up measurement of depression after the intervention period (Dunn et al., 2001; O'Connor et al., 1993). One recent study reported a sustained reduction in depression for 26 months after a 20-week intervention that involved resistance training among depressed older adults (Singh et al., 2001). Another study reported a sustained reduction in depression for 6 months after a 10-week intervention that involved weight-bearing exercise performed with music among older adults with mood disorders (Mather et al., 2002). Hence, there is limited evidence that supports the effectiveness of an exercise training intervention for the sustained reduction of depressive symptoms after the intervention period, particularly among non-depressed older adults.
Second, previous research has failed to examine factors that mediate changes in depression brought about by physical activity in older adults (O'Connor et al., 1993). Neurobiological mechanisms, such as changes in brain monoamines, are frequently cited as underlying the antidepressant effects of physical activity (Broose et al., 2002; Dishman, 1997). There is a growing recognition, however, that cognitive factors such as self-esteem may play a role in the relationship between exercise and depression (Broose et al., 2002; Fox, 2000; O'Neal et al., 2000). In this regard, self-esteem, an individual's cognitive evaluation or judgment of self-worth (Rosenberg et al., 1995), is considered to be a fundamental component of mental health (Baumeister, 1993; Diener, 1984; Sonstroem, 1997). Individuals with high self-esteem are (a) substantially happier than other people and (b) less likely to be depressed in general or in response to stressful, traumatic events (Baumeister et al., 2003). Physical self-esteem, however, is more likely to mediate any antidepressant effects of physical activity than global self-esteem (Fox, 2000). This position is based upon evidence that the physical self has been associated with mood, depression, and reported physical and mental health, after statistically controlling for global self-esteem and socially desirable responding (Sonstroem and Potts, 1996). This position is further supported by the observation that physical activity interventions have increased physical self-esteem (Li et al., 2002; McAuley et al., 2000) in the manner hypothesized by the Exercise and Self-esteem Model (Sonstroem and Morgan, 1989; Sonstroem, 1997).
Third, few studies have directly compared the effects of different modes of physical activity on depression among older adults (Broose et al., 2002; Dunn et al., 2001). Indeed, most studies have used only aerobic conditioning forms of physical activity (e.g., walking and jogging), leading to the conclusion that aerobic activity has beneficial effects on depression. To date, there is limited information about the effects of lower intensity, non-aerobic forms of activity on depression, although there have been antidepressant effects associated with high intensity, progressive resistance training among older adults (Singh et al., 1997, 2001). Such research is necessary because it has obvious implications for older adults who may be unable to engage in more intense types of activity due to limited mobility or chronic illness. Moreover, the comparison of aerobic and non-aerobic forms of activity for reducing depression would provide further evidence that vigorous physical activity might not be necessary for the accrual of psychological benefits.
Herein, we examined (a) the effects of a six-month intervention that consisted of two different modes of physical activity (walking or low-intensity resistance/flexibility training) on depressive symptoms over a 5-year period among non-depressed older adults and (b) change in physical self-esteem as a factor mediating changes in depressive symptoms. We hypothesized that the physical activity interventions would result in a curvilinear pattern of growth across time with a significant reduction in depressive symptoms immediately post-intervention, and a possible maintenance of this reduction over a prolonged follow-up period. No hypothesis was generated for a differential pattern of change in depression across the two modes of physical activity, but we did expect that change in physical self-esteem would be related to the hypothesized reduction in depressive symptoms.
METHOD
Participants
Sedentary, older (M age = 65.5 years) adults were recruited to participate in a 6-month randomized exercise trial. Inclusion criteria for participation in the program were: (a) age 60 to 75 years, (b) sedentary, as defined by a lack of regular involvement in exercise during the previous six months verified by exercise history and assessment of aerobic capacity by maximal graded exercise testing, (c) healthy to the degree that participation in exercise testing and an exercise program would not exacerbate any existing symptomology, (d) personal physician's clearance for participation, (e) adequate mental status (i.e., <3 incorrect answers), as assessed by the Pfeiffer Mental Status Questionnaire (Pfeiffer, 1975), and (f) willingness to be randomly assigned to a treatment condition. Intervention procedures and outcomes have been published elsewhere (Boileau et al., 1999; Kramer et al., 1999; McAuley et al., 1999).
Recruitment and Group Assignment
The CONSORT diagram in Fig. 1 illustrates the flow of participants through each stage of this randomized trial. Participants were recruited through local media sources (e.g., newspaper advertisements, radio and television announcements). Initially, 596 individuals indicated interest in participation and were contacted for preliminary screening. After the screening, 363 individuals were declared ineligible or declined participation. Subsequent withdrawal and medical exclusion yielded a sample of 174 participants (49 males, 125 females) who entered the exercise trial. Those individuals were randomly assigned to one of two treatment conditions (walking or low-intensity resistance/flexibility). Random assignment was based on a modification of the baseline adaptive randomization scheme (Begg and Iglewicz, 1980).
Treatment Conditions
Walking Group
This group was led by experienced exercise specialists and met in a local shopping mall. The focus of this program was on the provision of an organized walking program as an aerobic stimulus designed to influence cardiorespiratory endurance. The exercise sessions were conducted three times per week for six months, and followed basic ACSM guidelines including adequate warm-up and cool down periods and progressive increments in exercise intensity and duration. The intensity level began at light levels (50–55% VO2peak) and gradually increased to more moderate levels (65% VO2peak) by the midpoint of the program. The level of exercise intensity was based on physiological responses during graded exercise testing and was monitored based on heart rate (Karvonen method) and ratings of perceived exertion (Borg, 1998). Exercise duration began at 10–15 minutes and progressively increased by one minute per session until participants were exercising between 40 and 45 minutes per session. Each walking session included 10 minutes of warm up and cool-down activities.
Resistance and Flexibility Group
This group of individuals was led by an experienced exercise specialist and met in a large gymnasium on the same frequency and duration as the aerobic group. The focus of this program was on the provision of an organized program of stretching and low intensity strengthening exercises for the whole body designed for older individuals. The program included (a) low-intensity resistance exercises consisting of one set of 8–12 repetition per major muscle group using elastic bands to provide resistance and (b) flexibility exercises for all large muscle groups with stretches held to the point of slight discomfort for approximately 20–30 s and repeated 5–10 times (Larsson et al., 1979). Consistent with the walking condition, exercise duration began at 10–15 minutes and progressively increased by one minute per session until participants were exercising between 40 and 45 minutes per session. Each resistance/flexibility session included 10 minutes of warm up and cool-down activities.
Measures
Demographics, Health History, and Physical Activity History
Participant completed an inventory that provided detailed demographic and medical, health, lifestyle, and exercise history information.
Depressive Symptoms
Depressive symptoms were measured using the 30-item Geriatric Depression Scale (GDS; Yesavage et al., 1982). The GDS was specifically developed for measuring depressive symptoms among geriatric populations and, consistent with recommendations (O'Connor et al., 1993), has been used in previous exercise interventions with older adults (McMurdo and Burnett, 1992; Singh et al., 1997). Sample items from the GDS are “Do you feel your life is empty” and “Do you feel that your situation is hopeless.” Each of the 30 items was rated regarding whether it was currently pertinent to the participant's life using No or Yes response options. Positively worded items were reverse scored, and scores from the 30 items were summed to provide a single composite score. The composite score ranged from 0 to 30 with higher scores reflecting greater depressive symptomology. Evidence supports the validity and reliability of GDS scores as a measure of depressive symptoms among older adults (Hyer and Blount, 1984; Yesavage et al., 1982). The internal consistencies of the GDS at baseline and 60 months in this study were .85 and .88, respectively.
Physical Self-Esteem
The Physical Self-Perception Profile (PSPP) is a 30-item instrument used to assess self-esteem relative to several domains of physical functioning in a hierarchical, multidimensional fashion (Fox, 1990). The instrument contains a general 6-item physical self-worth scale (PSW), which was of primary interest in this study as a measure of physical self-esteem, as well as four sub-domain scales specific to perceived sport competence, physical condition, attractive body, and strength, with six items per scale. Sample items tapping the domain of physical self-worth were “I am extremely proud of who I am and what I can do physically” and “I always have a really positive feeling about the physical side of myself.” Participants rated the degree to which each item was characteristic or true of them using a 4-point scale with anchors of Not at all true and Completely true. Evidence supports the reliability and factorial, construct, and predictive validity of PSPP scores (Fox, 1990). The internal consistencies of the PSW subscale at baseline and 60 months in this study were .89 and .84, respectively.
Procedures
The procedures were approved by an Institutional Review Board, and all participants provided written informed consent. Baseline assessments of depressive symptoms and physical self-esteem were completed upon entry into the trial, but before random assignment of participants to treatment conditions. The participants embarked on a 6-month exercise training program that involved either walking or low-intensity resistance/flexibility. The measures of depressive symptoms and physical self-esteem were completed immediately after the 6-month intervention, and then again 12 and 60 months after intervention initiation. The measures were mailed to the participants, and participants completed the self-report measures in their home.
Latent Growth Modeling
We used latent growth curve modeling (LGM) to examine (a) the pattern of change in depressive symptoms across time and (b) the effect of the two modes of physical activity on changes in depressive symptoms (Lance et al., 2000; Meredith and Tisak, 1990; Willett and Sayer, 1994). LGM is a two-stage process that invokes a confirmatory factor analytic framework on variables measured longitudinally (Lance et al., 2000; Meredith and Tisak, 1990; Willett and Sayer, 1994). In the first stage, individual-level growth trajectories are fit to represent change on measures of the same construct obtained on multiple measurement occasions. This within-individual stage models aspects of intra-individual change including the sample mean change trajectory and within sample variability in the mean change trajectory. The second stage, or the between-individual stage, involves an examination of additional variables as determinants or outcomes of longitudinal growth trajectories. For example, the effect of the two treatment groups on change in depressive symptoms was examined in the second stage of LGM.
LGM has a number of advantages over other more commonly adopted approaches used to study change among continuous variables (e.g., repeated measures ANOVA) including the ability to (a) model change at the individual as well as the group level of analysis; (b) model individual differences in change trajectories (initial status and change functions); and (c) model various functional forms of change (e.g., linear, quadratic, optimal; Duncan et al., 1999; Lance et al., 2000; Meredith and Tisak, 1990; Willett and Sayer, 1994). LGM has an additional advantage of increased power for detecting group differences in change across time compared with a factorial repeated measures ANOVA (Duncan et al., 1999).
Panel Analysis
We used panel analysis for examining the direct effects of physical self-esteem on changes in depressive symptoms across time. The panel model that was tested with covariance modeling is presented in Fig. 2. This model included (a) paths between the same variables measured across time (i.e., stability coefficients) and (b) paths linking physical self-esteem with depressive symptoms at baseline and at the 6-, 12-, and 60-month assessments.
Model tested with panel analysis that included direct effects of physical self-esteem on depressive symptoms across four time points. Path coefficients are completely standardized. M0 = baseline; M6 = 6 months; M12 = 12 months; and M60 =60 months. PSW = Physical Self-Worth; and GDS = Geriatric Depression Scale.
Model Estimation
The LGM and panel analyses were performed using LISREL 8.50 with full-information maximum likelihood (FIML) estimation because there were missing data (Jöreskog and Sörbom, 1996). Missing values were present for 8.0, 10.9, and 29.9% of depressive symptoms data and 6.9, 13.2, and 28.2% of physical self-esteem data for the 6-, 12-, and 60-month measurements, respectively. FIML estimation is an optimal method for the treatment of missing data in covariance modeling (Arbuckle, 1996; Enders, 2002; Enders and Bandalos, 2001), particularly in applications of longitudinal modeling (Wothke, 2000). This estimator provides an intent-to-treat analysis whereby all of the available data are used in the estimation procedure. That is, cases with complete and incomplete data are utilized, unlike traditional maximum likelihood estimation in covariance modeling which requires listwise or pairwise deletion of cases with incomplete data. The FIML estimator has yielded accurate parameter estimates and fit indices with simulated missing data (Arbuckle, 1996; Enders, 2002; Enders and Bandalos, 2001; Wothke, 2000). Other missing data techniques, particularly pairwise and listwise deletion of cases, have yielded biased parameter estimates and fit indices and fail to make maximal use of all available data (Arbuckle, 1996; Enders, 2002; Enders and Bandalos, 2001; Wothke, 2000).
Model Fit
The chi-square statistic, root mean square error of approximation (RMSEA), non-normed fit index (NNFI), and comparative fit index (CFI) were used to evaluate the model-data fit. The chi-square statistic assesses absolute fit of the model to the data (Bollen, 1989). The RMSEA represents closeness of fit of the model to the data, with values approximating or less than 0.05 demonstrating a good fit (Browne and Cudeck, 1993). The 90% confidence interval (CI) around the RMSEA should contain 0.05 to indicate the possibility of close model-data fit (Browne and Cudeck, 1993). The NNFI and CFI are incremental fit indices and test the proportionate improvement in fit by comparing the target model to a baseline model with no correlations among observed variables (Bentler, 1990; Bentler and Bonett, 1980). NNFI and CFI values approximating 0.95 are indicative of good model-data fit (Hu and Bentler, 1999).
RESULTS
The demographic characteristics of the sample at baseline are provided in Table I. The majority of sample participants were female and Caucasian. Of the initial 174 participants, 153 individuals completed the 6-month trial, yielding an 88% overall adherence rate. Attendance rates did not differ significantly between treatment conditions (t = 0.88, p > 0.30). The program consisted of a total of 70 activity days. The mean number of days attended for the overall sample was 56.7 (SD = 14.1). The mean number of days attended by exercise condition was 55.7 (SD = 14.8) for the walking group and 57.6 (SD = 13.5) for the resistance/flexibility group. We previously reported that the walking group exhibited a 5.1% increase in relative VO2peak, whereas the resistance/flexibility condition exhibited a 2.8% reduction in relative VO2peak (Boileau et al., 1999). This supports that the two modes of physical activity had different influences on cardiorespiratory fitness. Table II contains the mean scores and standard errors for the depressive symptoms and physical self-esteem measures.
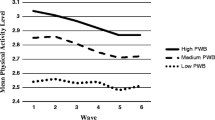
Estimating Growth in Depressive Symptoms
Growth in depressive symptom scores was best described by an optimal growth function with a heteroscedastic residual structure. This model provided an excellent fit for the depressive symptoms data (χ2 = 5.14, df = 3, p = .16, RMSEA [90% CI] = 0.06 [0.00–0.16], NNFI = 0.99, CFI = 0.99). Subsequent tests of the model with treatment group assignment as an exogenous predictor of initial status and change factors for depressive symptoms provided an excellent fit (χ2 = 8.74, df = 5, p = .12, RMSEA [90% CI] = 0.07 [0.00–0.14], NNFI = 0.98, CFI = 0.99). However, the effects for treatment group on the depressive symptoms initial status and change function endogenous variables were nonsignificant. Hence, the two conditions did not have a differential effect on depressive symptoms scores across time. The mean scores provided in Table II illustrated a curvilinear pattern of change in depressive symptom scores across time. There was an initial decrease of depressive symptom scores immediately after the intervention, followed by a sustained reduction of depressive symptom scores for the 12- and 60-month follow-up measurements. The effect sizes (Cohen's d) for the reduction in depression at the 6-, 12-, and 60-month time points relative to baseline were −0.26, −0.18, and −0.29, respectively. The correlation between initial status and change function endogenous variables was not statistically significant (ψ 21 = 0.04), and thus initial status did not impact the magnitude of change in depression scores across time.
Effects of Physical Self-Esteem on Changes in Depressive Symptoms
The previous analysis provided a representation of the growth function for depressive symptoms across time. The panel analysis examined the direct effect of physical self-esteem on changes in depressive symptoms across the baseline and 6-, 12-, and 60-month time points. This model is illustrated in Fig. 2, and it provided a good fit for the data (χ2 = 28.85, df = 12, p = .004, RMSEA [90% CI] = 0.09 [0.05–0.13], NNFI = 0.94, CFI = 0.98). Inspection of the path coefficients in Fig. 2 indicated that there were statistically significant direct effects of physical self-esteem on depressive symptoms at baseline (β = −.32), 6 months (β = −.13), 12 months (β = −.10), and 60 months (β = −.10). Hence, physical self-esteem was most strongly related with depressive symptoms at baseline (i.e., cross-sectional association), and less strongly related with depression symptoms at 6, 12, and 60 months after the initiation of the intervention (i.e., longitudinal association), which is expected, given the relatively small change in depressive symptoms after the exercise intervention.
Figure 2 provides further information about the stability of the measures across time. Overall, the stability coefficients were very strong for depressive symptoms and physical self-esteem for the first and second and second and third assessments, which was expected, given the relatively short period of time between assessments (i.e., 6 months). The stability coefficients were weaker for the two measures for the third and fourth assessments, as would be expected, given that the assessments occurred across a longer time period (i.e., 48 months).
DISCUSSION
The primary novel finding of this study involved the long-term maintenance effects of an exercise training intervention on reductions in depressive symptoms among older adults who were not clinically depressed. Latent growth curve modeling demonstrated that depressive symptoms scores were reduced immediately after the six-month exercise intervention, and this reduction was maintained at 12 and 60 months post-program initiation. This pattern of growth demonstrates that exercise training does not simply have a transient effect on depressive symptoms that vanishes immediately after the completion of an exercise intervention. Rather, exercise training may provide a long-lasting antidepressant effect, albeit in non-depressed older adults. Similar evidence of a sustained reduction in depression was observed 26 months after a 20-week exercise intervention among depressed older adults (Singh et al., 2001). Therefore, emerging evidence supports the effectiveness of exercise training for the sustained reduction of depressive symptoms after the intervention period among depressed and non-depressed older adults.
Another important finding of this study was that physical self-esteem predicted change in depressive symptoms. Although various neurobiological mechanisms have frequently been hypothesized as underlying the antidepressant effects of physical activity (Dishman, 1997), the role played in this relationship by cognitive factors has received increasing attention (Broose et al., 2002; Fox, 2000; O'Neal et al., 2000). Indeed, our results support such a position in that physical self-esteem is a cognitive factor that had direct, albeit modest, effects on changes in depressive symptoms. Subsequent physical activity intervention research might be designed to specifically target valued aspects of the physical self (i.e., strength, physical condition, physical appearance, etc.) in an effort to have a more pronounced effect on physical self-esteem and, in turn, depressive symptoms and other indicators of mental status. Previous research (Li et al., 2002; McAuley et al., 2000) and theory (Sonstroem and Morgan, 1989; Sonstroem, 1997) suggest that improving cardiorespiratory fitness, self-efficacy, and body composition through increased physical activity can lead to these desired improvements in physical self-esteem.
Interestingly, changes in depressive symptoms did not differ based on the mode of physical activity. There was no effect of treatment group on initial status or change in depressive symptoms scores. Such findings are consistent with previous research reporting that aerobic exercise training yields a reduction in depression (Dunn et al., 2001), but we are unaware of studies that have examined the effect of low-intensity resistance/flexibility exercise on depressive symptoms. However, Li and colleagues have reported that participation in Tai Chi results in improvements in anxiety, depression, self-esteem, and general well-being in older adults (Li et al., 2001, 2002). Tai Chi is a traditional exercise originating from Chinese culture that incorporates elements of balance, postural alignment, and concentration, and thus is a low-intensity form of exercise. Indeed, there is a growing body of literature supporting the position that vigorous physical activity is not necessary for health benefits (Blair and Connelly, 1996). Although there is increasing evidence to suggest that changes in aerobic fitness are implicated in improvements in cognitive function among older adults (see McAuley et al., 2004 for a review), fitness change may not be necessary for other mental health benefits.
We note that the sustained antidepressant effects of exercise reported in this study were observed in older adults who were not diagnosed as clinically depressed. Given the status of individuals over 65 years of age as one of the fastest growing age groups in the U.S. (National Institute of Aging, 2000) and the relationship between depression and disability among aging older adults (Penninx et al., 1998), such findings have important implications for identifying strategies for both prevention and treatment of depression in this age group. Although previous research has provided a basis for exercise as a treatment for depression among older adults, there is little experimental evidence to support physical activity as a possible means of preventing depression among non-depressed older adults (Dunn et al., 2001). The results of the present study demonstrate the effectiveness of an exercise training intervention for the long-term reduction of depressive symptoms across a five-year period, which, in combination with the results of population-based epidemiological studies (Strawbridge et al., 2002), supports exercise for the prevention of depressive symptoms in non-depressed older adults.
The present study, similar to others (Blumenthal et al., 1999), did not include a true control condition, and observed changes in depressive symptoms scores might have been caused by passage of time effects associated with regression to the mean. However, this does not appear to be the case in the present study. The initial mean depressive symptoms score in the present study was 5.6, while the mean value reported in the original validation study of the GDS with community-dwelling elderly persons was 5.8 (Yesavage et al., 1982). Accordingly, the participants in this study reported an initial depressive symptoms score that was below the value reported in the original validation research (Yesavage et al., 1982), and reported further reductions in depressive symptoms scores across time. Hence, we do not believe the changes in depressive symptoms scores are explained by regression to the mean. Moreover, we did not observe a relationship between initial level of depression and the magnitude of change in depression over the course of the intervention, which has been observed in previous research (Blumenthal et al., 1999). The low initial level of depression observed in this study likely accounts for the lack of a relationship between initial level of depression and the magnitude of change in depression over the course of the intervention.
Although this study had a number of strengths, it is necessary to acknowledge several limitations to our findings. Our sample was predominantly Caucasian and female, in spite of efforts to recruit participants from African-American and Latino communities. The distribution of sex in our sample is more reflective of the population at this age than an equal ratio of females and males, but the predominance of Caucasians is not as reflective of the population. Subsequent research might target such understudied populations to determine whether these long-term effects of physical activity on depressive symptoms and the roles played in this relationship by changes in physical self-esteem can be replicated. Additionally, we contrasted only a low-intensity resistance and flexibility exercise condition with a traditional aerobic walking condition. Whether other exercise modalities such as yoga and more intense resistance training programs have differential effects on depressive symptoms remains to be determined. Although we consider our sample to be relatively large for an exercise intervention, it will be necessary to cross-validate the findings in a larger independent sample. Finally, as has been acknowledged throughout this manuscript, participants in our sample were not, to our knowledge, clinically depressed but, rather, exhibited relatively low levels of depressive symptoms. Nonetheless, our effects were fairly robust and approximated a 1/4 standard deviation reduction in depressive symptoms. It will be important to determine whether the effects reported herein are amplified in samples with elevated or clinical depression levels. One might reasonably expect an intervention effect in the short-term, but determination of whether these effects can be maintained over time is warranted.
In summary, we provide novel evidence that supports (a) the effectiveness of an exercise training intervention for the sustained reduction of depressive symptoms among non-depressed older adults and (b) physical self-esteem as an important factor that underlies changes in depressive symptoms after an exercise training intervention among older adults.
REFERENCES
Arbuckle, J. L. (1996). Full information estimation in the presence of incomplete data. In Marcoulides, G. A., and Schumacker, R. E. (Eds.), Advanced Structural Equation Modeling: Issues and Techniques, Lawrence Erlbaum, Mahwah, NJ, pp. 243–277.
Babyak, M., Blumenthal, J. A., Herman, S., Khatri, P., Doraiswamy, M., Moore, K., Craighead, W. E., Baldewicz, T. T., and Krishnan, K. R. (2000). Exercise treatment for major depression: Maintenance of therapeutic benefit at 10 months. Psychosom. Med. 62: 633–638.
Baumeister, R. F. (1993). Understanding the inner nature of self-esteem. In Baumeister, R. F. (Ed.), Self-Esteem: The Puzzle of Low Self-Regard, Plenum, New York, pp. 201–218.
Baumeister, R. F., Campbell, J. D., Krueger, J. I., and Vohs, K. D. (2003). Does high self-esteem cause better performance, interpersonal success, happiness, or healthier lifestyles? Psychol. Sci. Pub. Inter. 4:1–44.
Begg, C. B., and Iglewicz, B. (1980). A treatment allocation procedure for sequential clinical trials. Biometrics 36: 81–90.
Bentler, P. M. (1990). Comparative fit indices in structural models. Psychol. Bull. 107: 238–246.
Bentler, P. M., and Bonett, D. G. (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 88: 588–606.
Blair, S. N., and Connelly, J. C. (1996). How much physical activity should we do? The case for moderate amounts and intensities of physical activity. Res. Q. Sport. Exerc. 67: 193–205.
Blumenthal, J. A., Babyak, M. A., Moore, K. E., Craighead, Plenum, W. A., Herman, S., Khatri, P., Waugh, R., Napolitano, M. A., Forman, L. M., Appelbaum, M., Doraiswamy, P. M., and Krishnan, K. R. (1999). Effects of exercise training on older adults with major depression. Arch. Intern. Med. 159: 2349–2356.
Boileau, R., McAuley, E., Demetriou, D., Devabhaktuni, N. K., Dykstra, G. L., Katula, J., Nelson, J., Pascale, A., Pena, M., and Talbot, H. (1999). Aerobic exercise training and cardiorespiratory fitness in older adults: A randomized controlled trial. J. Aging Physical Activity 7: 374–385.
Bollen, K. A. (1989). Structural Equations with Latent Variables, Wiley, New York, NY.
Borg, G. (1998). Borg's Perceived Exertion and Pain Scales, Human Kinetics, Champaign, IL.
Broose, A. L., Sheets, E. S., Lett, H. S., and Blumenthal, J. A. (2002). Exercise and the treatment of clinical depression in adults: Recent findings and future directions. Sports. Med. 32: 741–760.
Browne, M. W., and Cudeck, R. (1993). Alternative ways of assessing model fit. In Bollen, K. A., and Long, J. S. (Eds.), Testing Structural Equation Models, Sage, Newbury Park, CA, pp. 136–162.
Cutrona, C. E., and Russell, D. W. (1987). The provisions of social relationships and adaptations to stress. In Jones, W. H., and Perleman, D. (Eds.), Advances in Personal Relationships, JAI Press, Greenwich, pp. 37–67.
Diener, E. (1984). Subjective well-being. Psychol. Bull. 95: 542–575.
Dishman, R. K. (1997). Brain monoamines, exercise, and behavioral stress: Animal models. Med. Sci. Sports Exerc. 29: 63–74.
Duncan, T. E., Duncan, S. C., Strycker, L. A., Li, F., and Alpert, A. (1999). An Introduction to Latent Variable Growth Curve Modeling, Lawrence Erlbaum, Nahwah, NJ.
Dunn, A. L., Trivedi, M. H., and O'Neal, H. A. (2001). Physical activity dose-response effects on outcomes of depression and anxiety. Med. Sci. Sports Exerc. 33: S587–S597.
Enders, C. K. (2002). A primer of maximum likelihood algorithms available for use with missing data. Struct. Equat. Model. 8: 128–141.
Enders, C. K., and Bandalos, D. L. (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct. Equat. Model. 8: 430–457.
Fox, K. R. (1990). The Physical Self-Perception Manual, Office of Health Promotion, Northern Illinois University, Dekalb, IL.
Fox, K. R. (2000). Self-esteem, self-perceptions and exercise. Int. J. Sport Psychol. 31: 228–240.
Hu, L., and Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equat. Model. 6: 1–55.
Hyer, L., and Blount, J. (1984). Concurrent and discriminant validities of the Geriatric Depression Scale with older psychiatric inpatients. Psychol. Rep. 54: 611–616.
Jöreskog, K. G., and Sörbom, D. (1996). LISREL 8: User's reference guide, Scientific Software International, Chicago, IL.
Lance, C. E., Vandenberg, R. J., and Self, R. M. (2000). Latent growth models of individual change: The case of newcomer adjustment. Organ. Behav. Human Decis. Process. 83: 107–140.
Larsson, L., Grimby, G., and Karlsson, J. (1979). Muscle strength and speed of movement in relation to age and muscle morphology. J. Appl. Physiol. 46: 451–456.
Li, F., Duncan, T., Duncan, S., McAuley, E., et al. (2001). Enhancing psychological well-being of elderly individuals through tai-chi exercise. Struct. Equat. Model. 8: 53–83.
Li, F., Harmer, P., Chaumeton, N. R., Duncan, T. E., et al. (2002). Tai Chi as a means to enhance self-esteem: A randomized controlled trial. J. Appl. Gerontol. 21: 70–89.
Mather, A. S., Rodriguez, C., Guthrie, M. F., McHarg, A. M., M., Reid, I. C., and McMurdo, M. E. (2002). Effects of exercise on depressive symptoms in older adults with poorly responsive depressive disorder. Brit. J. Psychiatry 180: 411–415.
McAuley, E., Kramer, A. F., and Colcombe, S. J. (2004). Cardiovascular fitness and neurocognitive function in older adults: A brief review. Brain, Behav. Immun. 18: 214–220.
McAuley, E., Katula, J., Mihalko, S. L., Blissmer, B., et al. (1999). Mode of physical activity and self-efficacy in older adults: A latent growth curve analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 54: P283–P292.
McMurdo, M. E. T., and Burnett, L. (1992). Randomized controlled trial of exercise in the elderly. Gerontology 38: 292–298.
McNeil, J. K., LeBlanc, E. M., and Joyner, M. (1992). The effect of exercise on depressive symptoms in the moderately depressed elderly. Psychol. Aging 6: 487–488.
Meredith, W., and Tisak, J. (1990). Latent curve analysis. Psychometrika 55: 107–122.
National Institute of Aging (2002). Older Americans 2000: Key Indicators of Well-Being. (Federal Interagency Forum on Aging-Related Statistics), US Government Printing Office, Washington, DC.
O'Connor, P. J., Aenchbacher, L. E., and Dishman, R. K. (1993). Physical activity and depression in the elderly. J. Aging Physical Activity 1: 34–58.
O'Neal, H. A., Dunn, A. L., and Martinsen, E. W. (2000). Depression and exercise. Int. J. Sport Psychol. 31: 110–135.
Penninx, B. W., Guralnik, J. M., Ferrucci, L., Simonsick, E. M., Deeg, D. J., and Wallace, R. B. (1998). Depressive symptoms and physical decline in community-dwelling older persons. JAMA 279: 1720–1726.
Penninx, B. W., Rejeski, W. J., Pandya, J., Miller, M. E., et al. (2002). Exercise and depressive symptoms: A comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. J. Gerontol. B Psychol. Sci. Soc. Sci. 57: P124–P132.
Pfeiffer, E. (1975). A Short Portable Mental Status Questionnaire for the assessment of organic brain deficit in elderly patients. J. Am. Geriatr. Soc. 23: 433–441.
Rosenberg, M., Schooler, C., Schoenbach, C., and Rosenberg, F. (1995). Global self-esteem and specific self-esteem: Different concepts, different outcomes. Am. Sociol. Rev. 60: 141–156.
Singh, N. A., Clements, K. M., and Fiatarone, M. A. (1997). A randomized controlled trial of progressive resistance training in depressed elders. J. Gerontol. A Med. Sci. 52: M27–M35.
Singh, N. A., Clements, K. M., and Singh, M. A. F. (2001). The efficacy of exercise as a long-term antidepressant in elderly subjects: A randomized controlled trial. J. Gerontol. A Med. Sci. 56: M497–M504.
Sonstroem, R. J. (1997). Physical activity and self-esteem. In Morgan, W. P. (Ed.), Physical Activity and Mental Health, Taylor and Francis, Washington, DC, pp. 128–143.
Sonstroem, R. J., and Morgan, W. P. (1989). Exercise and self-esteem: Rationale and model. Med. Sci. Sports Exerc. 21: 329–337.
Sonstroem, R. J., and Potts, S. A. (1996). Life adjustment correlates of physical self-concepts. Med. Sci. Sports Exerc. 28: 619–625.
Strawbridge, W. J., Deleger, S., Roberts, R. E., and Kaplan, G. A. (2002). Physical activity reduces the risk of subsequent depression for older adults. Am. J. Epidemiol. 156: 328–334.
Willett, J. B., and Sayer, A. G. (1994). Using covariance structure analysis to detect correlates and predictors of individual change over time. Psychol. Bull. 116: 363–381.
Wothke, W. (2000). Longitudinal and multigroup modeling with missing data. In Little, T. D., Schnabel, K. U., and Baumert, J. (Eds.), Modeling Longitudinal and Multilevel Data: Practical Issues, Applied Approaches, and Specific Examples, Lawrence Erlbaum, Mahwah, NJ, pp. 219–240.
Yesavage, J. A., Brink, T. L., Rose, T. L., Lum, O., Huang, V., Adey, M., and Leirer, V.O. (1982). Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatric Res. 17: 37–49.
ACKNOWLEDGMENT
Funding for this study was provided by the National Institute on Aging (Grant 2RO1 AG 12113).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Motl, R.W., Konopack, J.F., McAuley, E. et al. Depressive Symptoms Among Older Adults: Long-Term Reduction After a Physical Activity Intervention. J Behav Med 28, 385–394 (2005). https://doi.org/10.1007/s10865-005-9005-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-005-9005-5