Abstract
This study replicates and extends studies of the Massachusetts Youth Screening Instrument, Version 2 (MAYSI-2) in a sample of 479 urban, rural, and suburban 12–16 year old youths (68% boys; 41% African American, 23% Latino) consecutively admitted to juvenile detention centers. Six principal components replicated the MAYSI-2 factor-analytically-derived subscales except for Depression/Anxiety, and suggested modifications of specific items in each sub-scale. Findings supported the internal consistency and validity of the modified MAYSI-2 sub-scales. Few gender differences emerged, except that girls reported higher levels of hopelessness and trauma than boys. Five sub-groups were identified based on component profiles: (1) non-clinical, (2) addiction, somatic problems, and suicidality, (3) anger problems, (4) thought disturbance, and (5) addiction and traumatic stress. The findings support the validity of the MAYSI-2 for juvenile justice mental health screening while highlighting possible refinements in scoring in order to identify delinquent youths with distinctive psychosocial risks and needs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An estimated 2.4 million children and adolescents are involved in the justice system as a result of arrests each year (Snyder 2004). Teplin et al. (2002) studied a representative sample of youth detainees in a large city, and found that approximately two in three boys (66%) and three in four girls (74%) met diagnostic criteria for one or more psychiatric disorders. Half of the boys and almost half of the girls met criteria for a substance use disorder. Abram et al. (2003) reported that 46% of these boys and 57% of these girls had two or more psychiatric disorders, while 20% of boys and 17% of girls met criteria for one disorder. Garland et al. (2001) found that 52% of a sample of youths with prior juvenile justice involvement met criteria for a psychiatric diagnosis, compared to 54% of a sample of abused or neglected children in the child welfare system. Thus, juvenile justice-involved youth typically have one, and often several, psychiatric disorders.
Although juveniles in detention centers are entitled to receive necessary mental health services (Grisso and Underwood 2004), most youths in juvenile justice systems are not screened or assessed for potential mental health concerns (MacKinnon-Lewis et al. 2002). In most juvenile justice settings, screening and assessment procedures and tests are not standardized (Hoge 2002; Soler 2002). The mental health services that exist for these youths are fragmented and geared primarily to managing risk and controlling behavior by treating the most severe pathology (Cocozza and Skowyra 2000). Wasserman et al. (2003) argue for reform by creating best practices in mental health screening and assessment. Such changes hinge on the development and application of psychometrically reliable and valid measures to assess internalizing as well as externalizing problems, and psychosocial strengths as well as deficits, in order to identify and individualize services for both currently impaired and high risk youths.
Recently, a mental health and substance abuse screen was developed specifically for youths involved in the justice system, the 52-item Massachusetts Youth Screening Instrument, Version 2 (MAYSI-2; Grisso and Barnum 2006). The MAYSI was designed to screen detained youth in order to identify those in need of immediate care (e.g., for suicidality). MAYSI-2 subscales were factor analytically derived from a sample of 1,279 boys and girls. Factors were selected using the minimum average partial method (Velicer 1976) in analyses separately for boys, girls, and the total sample. An eight-Component solution provided the most interpretable factors, and on the basis of items that loaded 0.35 or higher the boys’ and girls’ eight-factor solutions produced five factors with similar item structures for both genders. The sixth factor (pertaining to traumatic experiences) appeared for both genders, with one unique boys item and one for girls. A seventh factor (Thought Disturbance) appeared for boys but was not interpretable for girls. An eighth factor was not interpretable and was dropped. In a replication study (Grisso et al. 2001), item loadings were generally similar to those from the first sample, except that four of the nine initially high-loading items loaded only marginally for the second sample on the Depressed-Anxious factor. The MAYSI-2 has seven subscales for boys and six for girls, with good internal consistency, retest reliability, and concurrent validity (Grisso and Barnum 2006; Grisso and Quinlan 2005). Replication studies have supported the MAYSI-2’s criterion validity (Cauffman 2004; Goldstein et al. 2003) and predictive validity (in identifying immediate risk of self-harm or harm to others, or need for intensive mental health assessment; Cruise et al. 2003; Wasserman et al. 2004).
The present study was designed to empirically replicate the factor structure of the MAYSI-2 in a representative sample derived from a mixture of primarily urban, but also suburban, and rural milieus, upon entry to detention facilities. It extended past studies’ findings by testing the reliability and convergent, predictive, and discriminant validity of empirically derived factor scores in relation to independent measures of serious but preventable risk factors that are prevalent among detained youths: suicidality, violence, alcohol and drug use problems (Sanislow et al. 2003; Hayes 2004; McClelland et al. 2004). Although other MAYSI-2 sub-scales assess clinically relevant constructs, the three risk foci were selected because they reflect safety and behavior management problems that are more prevalent (i.e., vs. thought disorder) or immediately dangerous (i.e., vs. somatic complaints, depression/anxiety, traumatic experiences, or anger) than the constructs represented by the other MAYSI-2 sub-scales. The goal of the study was to determine if the domains represented by the factor analytically derived MAYSI-2 subscales are replicable, and to test their relationships to several specific brief risk screening instruments.
Materials and Methods
Participants
Study participants were 479 youths (68% boys) admitted within the prior 24–72 h to State of Connecticut pretrial juvenile detention centers, derived from a sample of 757 youths screened by detention facility staff between January–December 2003. Eight youths who were younger than 12 years old and one who was 17 years old were excluded in order to produce a sample ranging in age from at least 12 (the lower age level for MAYSI-2 norms) to no more than 16 years old. The highest age generally admitted in Connecticut juvenile detention facilities is 15 years, although older youths with outstanding juvenile cases may sometimes be detained. Missing data on the MAYSI-2 occurred randomly, resulting in a loss of 269 subjects; no differences were found between participants included in analyses and those excluded due to missing data on demographics (i.e., age, gender, ethnocultural background), type or violence of offense, or available scores on all other measures.
Participants’ self-reported ethnicities also were comparable to those of census data for all detained youths, including: White, not Hispanic (35% of this sample, versus 36% in detention facilities overall), Black (African–American and Caribbean American, 42%, versus 39% statewide), Latino/ Hispanic (23% of sample, versus 25% statewide). The types of legal charges for participants also were representative, including nonviolent acts and technical violations (e.g., theft, breach of the peace, drug use, failure to adhere to probation requirements; 65% of this sample, versus 60% in detention facilities overall), violent crimes (e.g., assault without a weapon, 26%, versus 33% statewide), and serious felonies such as rape and murder (9% for this sample versus 7% statewide).
Procedure and Measures
As mandated by State statute, self-report screening occurs at the time of intake, within 24–72 h of admission to one of the three pretrial detention centers for youths in Connecticut. Staff ratings of youth violence risk were collected for all new admissions throughout the first week, on a schedule dictated by each facility’s logistics and policies. Data were abstracted on a redacted basis to ensure anonymity from secure institutional electronic databases by a co-author (JC), according to an exempt protocol for the management of archival data approved by the institutional review boards of the Court Support Services Division (IRRC) and University of Connecticut Health Center.
Massachusetts Youth Screening Instrument, Version 2 (MAYSI-2)
This 52-item self-report measure requires about 10 min to administer and is readable at the fifth grade level (Grisso et al. 2001). The computerized Voice CD Version 3 was used, with dichotomous “yes” or “no” items answered based on “the past few months” (Cauffman 2004). Face valid items suggested by adolescent mental health experts and juvenile detention staff were refined in the MAYSI-2 based on psychometric studies of seven factor analytically derived subscales: Alcohol/ Drug Use, Angry–Irritable, Depressed–Anxious, Somatic Complaints, Suicide Ideation, Thought Disturbance, and Traumatic Experiences. The MAYSI-2 shows evidence of internal consistency (median Cronbach’s α = 0.70; median item-total correlations = 0.35–0.62, with none below 0.20) and retest reliability (median intraclass correlation = 0.74), convergent validity with the Child Behavior Checklist Youth Self Report and Millon Adolescent Clinical Inventory (rs = 0.35–0.65); and criterion and predictive validity based on correctional records identifying youths with: (a) prior mental health treatment, (b) post-detention placement in secure facilities, and (c) a low likelihood of receiving post-detention mental health services (Grisso and Barnum 2006; Grisso and Quinlan 2005).
Structured Assessment of Violence Risk in Youth (SAVRY)
This 30-item rating scale reliably and validly assesses 24 risk factors in three domains (Historical, Social/ Contextual, and Individual) and six protective factors (Borum et al. 2005, 2006). SAVRY ratings were completed by Masters-level counselors based upon an intake interview they conducted prior to administering the self-report measures. The three risk domain scores were highly correlated (rs = 0.61–0.62, p < 0.001) and less well correlated with the protective factors score (rs = −0.42–0.60, p < 0.001), so a single risk score was calculated. The risk (α = 0.82) and protective factors (α = 0.73) scores had good internal consistency.
Suicidal Ideation Questionnaire (SIQ)
The 30-item SIQ was used with youths ages 14–16 years, and the 15-item SIQ-Jr. was used with 12–13 year olds (D’Eramo et al. 2004). The SIQ is a paper and pencil self-report questionnaire with demonstrated internal consistency and temporal reliability and concurrent and predictive validity in clinical (D’Eramo et al. 2004; Pinto et al. 1997) and non-clinical (Gutierrez et al. 2004) samples of adolescents ages 12–18 years old. SIQ items are answered on a 0–6 scale for the past month, ranging from “never had that thought” to “daily or almost every day.” In order to compare data from the SIQ (completed by 34% of the sample) and the SIQ-Jr. (completed by 66% of the sample), scores were converted to percentiles based upon normative data (Reynolds 1988). The current sample’s SIQ percentile score distribution (Range = 15–99; Median = 24) was skewed toward low scores compared to clinical samples with the SIQ (D’Eramo et al. 2004: Range = 41–99) or to normative samples with SIQ and SIQ-Jr for which, by definition, the Median = 50.
Drug Abuse Screening Test for Adolescents (DAST-A)
This 27-item self-report paper-and-pencil questionnaire was shown to be internally consistent (α = 0.91), temporally reliable (one week re-test r = 0.89), and to have criterion validity related to substance abuse/dependency diagnoses (Martino et al. 2000) and concurrent validity with the Millon Adolescent Clinical Inventory substance proneness scale (Pinto and Grilo 2004). These psychometric studies were conducted with youths ages 13–19 years old who were admitted to psychiatric facilities due to acute suicidality, behavioral dyscontrol, or dangerousness. A cut-point of 7 or higher was found to be predictive of a substance abuse/dependency diagnosis (Martino et al. 2000). The distribution of scores (Range = 0–24; M = 4.0, SD = 5.1) was comparable but somewhat lower on Mean scores than the Martino et al. (2000) sample (M = 5.9, SD = 5.9) and the Pinto and Grilo (2004) sample(M = 6.3, SD = 6.1), with a higher mean score than that reported by Martino et al. for patients with no substance use disorder diagnosis (M = 2.8) and a lower mean score than Martino et al. reported for patients with addictive disorder diagnoses (M = 7.2–13.6).
Alcohol Problems Risk: Adolescent Alcohol Involvement Scale (AAIS)
This 14 item paper-and-pencil self-report questionnaire assesses perceived interference of alcohol use with psychological, social, and family functioning with items scored on scales ranging from 0–4 to 0–7 and a total possible score of 79 (Mayer and Filstead 1979). One-week re-test reliability was strong for adolescents in addiction treatment (r = 0.91) and infrequent drinkers (r = 0.89) (Mayer and Filstead 1979). Criterion validity has been shown with substance abuse/dependency diagnosis (Martino et al. 2000) and addiction proneness (Pinto and Grilo 2004) in psychiatric samples. The score distribution (Range = 0–79; SD = 20.3) was comparable in range and variability to those from high risk (Mayer and Filstead 1979) or psychiatrically hospitalized (Martino et al. 2000; Pinto and Grilo 2004) adolescent samples, but with a lower Mean (M = 18.9 vs. M ∼ 32), consistent with the non-clinical nature of this sample.
Statistical Analyses
After initial review and cleaning of all data to eliminate extreme outliers and cases with invalid or missing data, SPSS (Version 12) was used to conduct a principal components analysis (PCA) with varimax orthogonal rotation, including all items from the MAYSI-2. After inspection of the scree plot, components with Eigen values >1.0 that met Velicer’s (1976) MAP criteria were retained. Items loading >0.40 on one component and <0.35 (i.e., <10% shared variance) on all other components were used to define the components. In order to test the stability of the solution for boys and girls, separate principal components analyses were conducted for each gender. Correlations between the component scores and the original MAYSI-2 subscale scores were calculated to test the replicability of MAYSI-2 subscales. Discriminant validity of the empirically derived components was tested by examining the correlations between each component score and all original MAYSI-2 subscale scores. Predictive validity of the empirically derived MAYSI-2 components, controlling for demographics, was tested in linear multivariate regressions with SAVRY risk and protective factor scores, and in logistic regressions with high/low risk groupings identified by a median-split of the SIQ, DAST and AAIS scores. Median splits rather than continuous scores were used because, due to the low-end skew of their distributions, use of continuous scores would have violated the requirement of normally distributed scores that is necessary for reliable results with linear multiple regression analyses. Finally, clinical utility was tested with a k-means cluster analysis, to determine if distinct sub-groups based on the MAYSI-2 component scores could be identified.
Results
A 6-Component PCA solution was identified as optimal overall as well as in separate analyses for each gender (Table 1). The derived components generally replicated the MAYSI-2 subscales (Table 2), except there was no component corresponding to the depression/anxiety sub-scale. Components with items reflecting (1) Hopelessness, (2) Anger, and (3) Addiction, accounted for one quarter of the total variance. Components with items reflecting (4) Somatic problems, (5) Psychosis, and (6) Trauma, accounted for 15–20% variance. The addiction component exactly replicated the corresponding MAYSI-2 sub-scale. The hopelessness component replicated the MAYSI-2 suicide ideation sub-scale, except that one item from the depression/anxiety sub-scale (#17, loneliness) and one item that was not in any MAYSI-2 sub-scale (#38, “can’t do anything right”) were added. The anger component replicated the MAYSI-2 sub-scale, except adding an item that was not in any MAYSI-2 sub-scale (#4, problems concentrating). The somatic component replicated the MAYSI-2 sub-scale except adding one item from the MAYSI-2 depression/anxiety sub-scale (#3, worry or nervousness impairs functioning). The trauma component replicated the MAYSI-2 subscale except adding an item from the MAYSI-2 depression/anxiety sub-scale (#21, bodily pain), excluding an item from the MAYSI-2 boys’ trauma sub-scale (#46, “people talk about me”), and including an item for both genders that the MAYSI-2 included only for girls (#50, rape).
The two MAYSI-2 sub-scales that were most altered in the present results were thought disturbance and depression/anxiety. Only two thought disturbance items (visual hallucinations, #9; auditory hallucinations, #20) had strong loadings on the psychosis component overall and for both boys and girls. One item from the MAYSI-2 anger/irritability sub-scale (#8, hyperarousal) loaded strongly overall and for girls (but not boys) on the psychosis component. Two of the five thought disturbance items approached but did not reach the 0.40 criterion on this component (#32, thought projection; #25, external control), as did an item that was not in any MAYSI-2 sub-scale (#12, excessive daydreams). A final original item did not load on any component (#26, dissociation).
As noted above, there was no component reflecting depression/anxiety. Three items from this sub-scale (#35, “feel angry a lot”; #47, feel hopeless; #51, intrusive memories) also are scored on other MAYSI-2 sub-scales, and the component solution eliminated this redundancy by assigning them to a single component. Other MAYSI-2 depression/anxiety sub-scale items also loaded on the components representing hopelessness (#17, lonely), somatic distress (#3, worry or nervousness impairs functioning), and traumatic stress (#21, bodily complaints). One depression/anxiety sub-scale item, #14 (nightmares), did not load on any component overall, but loaded on the somatic component for boys (.466) and the trauma component for girls (0.426). Two depression/anxiety sub-scale items did not load on any component (#34, social anhedonia; #41, emotional detachment).
Cronbach’s α for the original MAYSI-2 sub-scales confirmed adequate internal consistency for suicide ideation (0.88), angry/irritable (0.80), alcohol/drug use (0.84), depressed/anxious (0.74), and somatic complaints (0.73), but not for the thought disturbance (0.59) and traumatic experiences (0.58) subscales. Revisions based upon PCA loadings improved the traumatic experiences subscale α to 0.68: deleting item #46 (“people talk about me”), including #50 (rape) for both genders, and adding #21 (bodily pain). The low internal consistency of the thought disturbance sub-scale appeared to be related to low intercorrelations amongst the items: only the two items that loaded most strongly and consistently (#9, 20) were correlated > 0.30 (r = 0.54, p < 0.0001).
Gender differences were identified on the regression-derived scores for two components, hopelessness (t[457] = 5.5, p < 0.001; d = 0.51) and trauma (t[457] = 3.7, p < 0.001; d = 0.36), with effect sizes in the medium range (Cohen 1988). Girls scored higher than boys on both components. No differences were found in the items loading on the addiction component in the overall, girls’, and boys’ PCAs (Table 3), and minimal differences were found for: (a) hopelessness (i.e. one item, #17 [felt lonely] loaded marginally for girls), (b) anger (i.e., one item, #44 [intentional property damage] loaded marginally for girls), (c) somatic (i.e., one item, #3 [worried] loaded marginally for girls; sleep problems [#1] loaded marginally for boys and overall), and (d) trauma (i.e., fatigue/anhedonia, #15, loaded for girls, not overall or for boys). The psychosis component had four gender differences in loadings: strong loadings for girls (weak for boys) on hyperarousal (#8), thought projection (#32), and excessive daydreams (#12); strong loading for boys (weak for girls) on external control (#25).
The PCA components were uncorrelated by design (i.e., Varimax rotation) to maximize component independence. In correlational analyses (Table 3), all empirical components showed evidence of discriminant validity, correlating primarily only with the corresponding MAYSI-2 subscale. Depression/anxiety was the only MAYSI-2 subscale with which the component scores correlated consistently >0.30, correlating >0.40 with trauma, hopelessness, and anger components and >0.30 with the somatic component. These correlations may be due both to shared items and to the known conceptual and clinical overlap of depression and anxiety with trauma, hopelessness, and somatic problems. The only other MAYSI-2 sub-scale that correlated >0.20 with more than two component scores was Thought Disturbance (with addiction, hopelessness, and anger components). Thus, the depression/anxiety and thought disturbance MAYSI-2 sub-scales had the poorest evidence as well as the weakest validation evidence in the principal components analyses.
In multivariate linear regression analyses (Table 4), the anger component and African American ethnocultural background were consistent correlates of risk and protective factors on the SAVRY in opposite directions: anger correlated with risk, and (consistent with prior SAVRY findings related to race; Chapman et al. 2006) African American background was related to protective factors. Addiction component scores correlated with risk, and somatic component scores correlated with protective factors. Each multiple R was statistically significant (p < 0.001): R = 0.34, 0.28; R 2 = 0.13, 0.08, respectively, for risk and protective factors. Age, gender, assessor gender and race, and other component scores were unrelated to SAVRY risk or protective factors.
In multivariate logistic regression analyses (Table 5), above-median scores on the SIQ were associated with all of the component scores, and inversely related to Hispanic ethnicity. Above-median AAIS and DAST-A correlated with the addiction, anger, and hopelessness component scores and older age. The psychosis component score also was related to elevated DAST-A scores. Gender and ethnocultural background (of the youth or the detention staff person) were unrelated to scoring below or above the median on the DAST-A and AAIS.
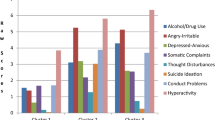
Five clinically-relevant sub-groups were identified via a k-Means cluster analysis, which converged in 16 iterations and for which all independent variables (empirically-derived MAYSI-2 component scores) were associated with membership in one or more clusters (Fs[4,482] = 5.0–229.1, p < 0.001; Table 6). Solutions with fewer or more clusters were tested, but rejected due to resulting in insufficient discrimination among the empirical components in solutions with fewer clusters, and clusters with weak cluster centers (<0.40) and small Ns (<25) in solutions with more clusters. The five clusters reflect, respectively: (1) no problems, (2) comorbid substance use/somatic problems and hopelessness, (3) anger problems, with substance abuse denied, (4) thought disturbance, and (5) comorbid substance use/traumatic stress problems, with hopelessness denied.
Substance abuse was denied (i.e., cluster center <−0.40) by youths in the anger problems cluster, as was hopelessness by youths in the addiction/trauma cluster. Girls (32% of the overall sample) were disproportionately likely (Chi Squared [X 2] = 17.9, df = 4, p < 0.001) to be members of the addiction/somatic problems and hopelessness cluster (58%). The gender distribution in the other clusters was proportionate to that of the overall sample. There was no statistically significant difference in ethnocultural composition between the clusters. Mean age of the clusters differed statistically significantly only between the thought disorder (M = 14.0 years) and addiction/trauma (M = 14.6) clusters (F[4,482] = 2.7, p = 0.005).
Analyses of variance followed by post hoc Scheffe tests showed that the cluster groups differed on SAVRY risk scores (F[4,482] = 8.9, p < 0.001). As expected, the “no problems” cluster members had significantly lower risk scores than members of the addiction/somatic problems and hopelessness cluster and the addiction/trauma clusters. Thought disorder cluster members also had significantly lower risk scores than the addiction/trauma cluster members. On protective factors, the only statistically significant difference was between the “no problems” cluster (higher mean score) and the addiction/somatic problems and hopelessness cluster (lower mean score). Chi Squared tests (df = 4) showed that the clusters differed on the likelihood of scoring above the median on the SIQ (X 2 = 55.4, p < 0.001), the DAST-A (X 2 = 59.2, p < 0.001), and the AAIS (X 2 = 35.2, p < 0.001). Almost all (94%) members of the cluster reporting high levels of hopelessness scored above the median on the SIQ. The two clusters with prominent addiction component scores had very high proportions (80–91%) of members scoring above the median on the DAST and AAIS. Fewer (half to two-thirds) of the members of the anger and thought disorder clusters had above-median scores on the SIQ, DAST, and AAIS. Between a third and half of the “no problems” cluster members had above median scores on these measures.
Discussion
The study findings support the use of the MAYSI-2 as a primary mental health intake screen in juvenile detention centers, while also suggesting possible refinements in the use of the MAYSI-2 and benefits of the inclusion of other more focal screening instruments. Replicating prior MAYSI-2 studies, there was evidence of internal consistency reliability for all but two subscales, one of which (traumatic experiences) approached acceptable reliability when altered using the study’s findings. There also was support for the factorial, concurrent, and discriminant validity for all sub-scales except depression/anxiety and thought disturbance, based upon correlational results with measures of risk and protective factors, suicide ideation, and substance use problems, as well as cluster analyses in which youths with distinct profiles on the MAYSI-2 component scores were identified.
The findings support the use of the MAYSI-2 alcohol/drug use sub-scale as a reliable, valid, and clinically useful screener. Screeners such as the DAST-A and AAIS provide more detailed information about substance use and abuse, but the briefer MAYSI-2 sub-scale appears sufficient to identify youths in juvenile detention who are willing to disclose substance use problems despite the general tendency for these youths to deny such problems for a variety of legal, psychological, and social reasons (McClelland et al. 2004). The cluster analysis findings also suggest that a combination of substance use problems with somatic distress and hopelessness, or with trauma (despite denying hopelessness), warrants special attention in order to identify particularly vulnerable youths.
A combination of substance abuse, somatic complaints, and hopelessness was associated with the most severe degree of risk, but was not associated with trauma experiences or symptoms. This finding is consistent with a growing body of research showing that children who experience early onset chronic traumas (e.g., physical, sexual, or emotional abuse or neglect; Teicher et al. 2006; Widom 1999) may develop severe affect and somatic dysregulation that is not identical to PTSD (Ford 2005). This result also is consistent with a prior study’s finding that dysphoria, decreased social connectedness, impulsivity and instability were correlates of suicidality and suicide attempts among juvenile justice-involved youths (Rhode et al. 1997). The 10% of detained youths who report this pattern of addiction, hopelessness, and somatic problems appear to warrant more detailed clinical evaluation of suicide risk (Bonner 2000), mood disorders (Ryan and Redding 2004), and trauma history and symptoms (Wolpaw et al. 2004) than is provided in the brief MAYSI-2 sub-scales.
The additional 15% of detained youths who reported trauma experiences or symptoms also often endorsed substance use problems and denied hopelessness. They may constitute what Terr (1991) describes as Type I trauma survivors, who have experienced fairly discrete traumas (e.g., severe accidents or assaults) and who are more likely to need help with anxiety and emotional numbing (hence their proneness to addiction; Ouimette and Brown 2003) than hopelessness or suicidality.
Girls were more likely than boys to report trauma experiences and symptoms, as well as to report fatigue and anhedonia if they endorsed trauma items. Girls in juvenile detention samples are at high risk for recurrent trauma (although not more likely than boys to have PTSD; Abram et al. 2004). Therefore, preventive and treatment services for traumatized girls are particularly needed in juvenile justice settings (Hennessey et al. 2004).
The MAYSI-2 depression/anxiety subscale may warrant re-examination based on growing evidence questioning its validity. In addition to the present study’s findings, the scale’s item content has not been well replicated in prior studies (Grisso et al. 2001), and in another study (Wasserman et al. 2004) it was not associated with diagnoses of mood or anxiety disorders and it better identified youths with a comorbid internalizing and other disorder than youths with only an internalizing disorder. Screening for clinical depression and anxiety clearly is needed in light of high prevalence levels among juvenile justice-involved youths-estimates range from17–19% in Mississippi (Robertson et al. 2004) to 20% in Texas (Pliszka et al. 2000), and 24% in South Carolina, (Atkins et al. 1999). However, screening, assessment, and treatment for depressive or anxiety symptoms in this population may be most accurate and efficient if more specific problems associated with both anxiety and depression (e.g., traumatic stress, hopelessness, anger, somatic complaints) are the focus.
Consistent with this view, recent evidence demonstrates that stressors and reduced caregiver support are independent risk factors for depression among juvenile justice involved youths, with stress contributing to the risk of depression, particularly for boys (McCarty et al. 2006). Rather than focusing primarily on depression as an approach to preventing suicide, juvenile justice programs might identify youths needing close observation and special treatment planning for self-harm (Lyons et al. 2003) by focusing on hopelessness in combination with physical complaints and problematic substance use. These conditions may exacerbate disinhibition and dysphoria, which can lead to suicidality (Hayes 2004).
The MAYSI-2 traumatic experiences sub-scale also warrants re-examination. Removing the interpersonal hypervigilance item, adding a bodily pain item, and using the rape item with boys as well as girls, was consistent with the principal components results and produced a more internally consistent traumatic experiences score. These modifications are consistent with findings that: (1) interpersonal sensitivity or suspiciousness may be more related to environmental adversity or temperamental oppositionality than to trauma; (Calvert 2002; Loeber and Farrington 2000); (2) bodily pain, while not a formal symptom of PTSD, is associated with both trauma exposure and PTSD (Schnurr and Green 2004), and (3) although more rarely reported by boys than girls, when sexual assault does occur to boys the impact is severe (Wolfe et al. 2006).
The empirically-derived clusters are consistent with prior juvenile justice research findings that identified three sub-groups of youths (Stewart and Trupin 2003)-asymptomatic, psychiatrically impaired, and dual diagnosis (addictive and psychiatric disorders)-and that showed that the latter two groups were more likely to receive longer, more restrictive punishments, and less likely to have access to minimum security and transitional placements and services. The cluster findings suggest that psychiatric and dual diagnosis sub-groups can be further sub-divided based on: (a) somatic distress and hopelessness, (b) trauma history and symptoms, (c) anger, and (d) thought disorder.
The sub-group endorsing high levels of anger constituted almost one third of the sample, and these youths tended to deny substance use problems (as well as hopelessness, thought disturbance, and trauma history or symptoms). Further assessment of anger may be useful in order to distinguish the majority whose anger is likely to be primarily situational from smaller but clinically significant sub-groups who: (a) are angry and hopeless, which the present findings suggest increases the risk of suicidality and substance abuse; (b) are angry and agitated (e.g., thought disorder), which increases the risk of suicidality and drug abuse; or (c) are angry and psychopathic. The former two sub-groups are consistent with a formulation of “reactive” aggression while the latter sub-group may represent a “proactive” antisocial form of aggression (Connor et al. 2004). Although anger problems correlated with problematic substance use, violence, and suicide ideation, the results of the cluster analyses suggest that anger per se does not distinguish youths at highest risk for addiction or suicide ideation. Anger is expectable for many adolescents in juvenile justice settings, due to the peer group, socioeconomic, and familial conflicts, deprivations, or adversities they face.
A smaller (7% of the sample) sub-group reported thought disorder problems, primarily on two items (visual and auditory hallucinations) that were associated with suicide ideation and drug use, but not violence risk or alcohol use problems. The two primary MAYSI-2 psychosis items may represent an efficient initial screen to identify youths in need of further clinical evaluation for psychosis.
Gender did not contribute to multivariate identification of risk status for violence, suicide ideation, or substance use problems. By contrast, prevalence studies with community or clinical (Costello et al. 2003) and juvenile justice (Wasserman et al. 2005) samples, have shown that girls are at higher risk than boys for affective or anxiety disorders and boys are at higher risk than girls for externalizing disorders. The present findings suggest that, although externalizing factors (especially anger problems) are most consistently associated with violence risk and substance use problems, and internalizing factors (e.g., thought disorder, hopelessness) are most reliably associated with suicide ideation, in juvenile detention populations both girls and boys may have either externalizing or internalizing problems.
The study has several limitations. The sample, while ethnically diverse, representing both genders, and drawing from rural, suburban, and urban populations, is limited to one northeastern state. The girls sub-sample was small, providing only a 3:1 ratio of participants to MAYSI-2 items (i.e., 154:52) which may not provide stable PCA results. Independent confirmation of self-reported problems on the SIQ, DAST, and AAIS was not possible (e.g., legal/institutional records of suicide attempts or violent behavior, medical records of health problems, child protective services or health care records of traumatic events). The traumatic experiences sub-scale items do not fully represent the nature or extent of youths’ trauma exposure or traumatic stress symptoms. Due to not having inter-rater checks in this study, the SAVRY data were of uncertain reliability.
In summary, the present study’s results support the MAYSI-2’s psychometric status while suggesting modifications in scoring and interpretation that may enhance its ability to provide the critical “alerting function” of identifying youths in need of immediate psychiatric evaluation or care (Grisso and Quinlan 2005). With continued empirically-based refinement, the MAYSI-2 is uniquely positioned to anchor mental health screening in the juvenile justice system (Wasserman et al. 2004).
References
Abram, K. M., Teplin, L., Charles, D., Longworth, S., McClelland, G., & Dulcan, M. (2004). Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of General Psychiatry, 61, 403–410.
Abram, K. M., Teplin, L., & McLelland, G. (2003). Comorbidity of severe psychiatric disorders and substance use disorders among women in jail. American Journal of Psychiatry, 160, 1007–1010.
Atkins, D. L., Pumariega, A. J., Rogers, K., Montgomery, L., Nybro, C., & Jeffers, G., et al. (1999). Mental health and incarcerated youth I:. Journal of Child and Family Studies, 8, 193–204.
Bonner, R. L. (2000). Correctional suicide prevention in the year 2000 and beyond. Suicide and Life Threatening Behavior, 30, 370–376.
Borum, R., Bartel, P., & Forth, A. (2005). Structured Assessment of Violence Risk in Youth (SAVRY). In T. Grisso, G. Vincent, & D. Seagrave (Eds.). Mental health screening and assessment in juvenile justice (pp. 311–323). New York: Guilford.
Borum, R. Bartel, P., & Forth, A. (2006). Manual for the structured assessment of violence risk in youth (SAVRY) professional manual: Lutz, FL: Psychological Assessment Resources, Inc.
Calvert, W. J. (2002). Neighborhood disorder, individual protective factors, and the risk of adolescent delinquency. ABNF Journal, 13, 127–135.
Cauffman, E. (2004). A statewide screening of mental health symptoms among juvenile offenders in detention. Journal of the American Academy of Child & Adolescent Psychiatry, 43, 430–439.
Chapman, J. F., Desai, R. A., Falzer, P. R., & Borum, R. (2006). Violence risk and race in a sample of youth in juvenile detention: The potential to reduce disproportionate minority confinement. Youth Violence and Juvenile Justice, 4, 170–184.
Cocozza, J. J., & Skowyra, K. R. (2000). Youth with mental health disorders: Issues and emerging responses. Journal of the Office of Juvenile Justice and Delinquency Prevention, 7, 3–13.
Cohen, J. (1988). Statistical methods for the social sciences (2nd Ed.). New York: Plenum.
Connor, D., Steingard, R., & Cunningham, J. (2004). Proactive and reactive aggression in referred children and adolescents. American Journal of Orthopsychiatry, 74, 129–136.
Costello, E. J., Mustillo, S., Erklani, A., Keeler, G., & Angold, A. (2003). Prevalence and develop-ment of psychiatric disorders in adolescence. Archives of General Psychiatry, 60, 837–844.
Cruise, K., Colwell, L., Lyons, P., & Baker, M. (2003). Prototypical analysis of adolescent psychopathy. Behavioral Sciences & the Law, 21, 829–846.
D’Eramo, K., Prinstein, M., Freeman, J., Grapentine, W., & Spirito, A. (2004). Psychiatric diagnoses and comorbidity in relation to suicidal behavior among psychiatrically hospitalized adolescents. Child Psychiatry and Human Development, 35, 21–35.
Ford, J. D. (2005). Treatment implications of altered affect regulation and information processing following child maltreatment. Psychiatric Annals, 35, 410–419.
Garland, A. F., Hough, R. L., McCabe, K. M., Yeh, M., Wood, P. A., & Aarons, G. A. (2001). Prevalence of psychiatric disorders in youths across five sectors of care. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 409–418.
Goldstein, N., Arnold, D., Weil, J., Mesiarik, C., Peuschold, D., & Grisso, T., et al. (2003). Comorbid symptom patterns in female juvenile offenders. International Journal of Law & Psychiatry, 26, 865–882.
Grisso, T., & Barnum, R. (2006). Massachusetts youth screening instrument version 2: User’s manual and technical report. Sarasota, FL: Professional Resource Press.
Grisso, T., Barnum, R., Fletcher, K., Cauffman, E., & Peuschold, D. (2001). Massachusetts youth screening instrument for mental health needs of juvenile justice youths. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 541–548.
Grisso, T., & Quinlan, J. (2005). Massachusetts youth screening instrument—Version 2. In T. Grisso, G. Vincent, & D. Seagrave (Eds.). Mental health screening and assessment in juvenile justice (pp. 99–111). NY: Guilford.
Grisso, T., & Underwood, L. (2004). Screening and assessing mental health and substance use disorders among youth in the juvenile justice system: A resource guide for practitioners (Document #204956). Washington, DC: Office of Juvenile Justice and Delinquency Prevention.
Gutierrez, P., Watkins, R., & Collura, D. (2004). Suicide risk screening in an urban high school. Suicide and Life-Threatening Behavior, 34, 421–428.
Hayes, L. (2004). Juvenile suicide in confinement: A national survey. Washington, DC: National Center on Institutions and Alternatives.
Hennessey, M., Ford, J. D., Mahoney, K., Ko, S., & Siegfried, C. (2004). Trauma among girls in the juvenile justice system. Los Angeles: National Child Traumatic Stress Network (www.NCTSNet.org).
Hoge, R. (2002). Standardized instruments for assessing risk and need in youthful offenders. Criminal Justice & Behavior, 29, 380–396.
Loeber, R., & Farrington, D. P. (2000). Young children who commit crime. Development and Psychopathology, 12, 737–762.
Lyons, J., Griffin, G., Quintenz, S., Jenuwine, M., & Shasha, M. (2003). Clinical and forensic outcomes from the Illinois mental health juvenile justice initiative. Psychiatric Services, 54, 1629–1634.
MacKinnon-Lewis, C., Kaufman, M. C., & Frabutt, J. M. (2002). Juvenile justice and mental health: Youth and families in the middle. Aggression and Violent Behavior, 7, 353–363.
Martino, S., Grilo, C. M., & Fehon, D. C. (2000). The development of the Drug Abuse Screening Test for adolescents (DAST-A). Addictive Behaviors, 25, 57–70.
Mayer, J., & Filstead, W. J. (1979). The adolescent alcohol involvement scale: An instrument for measuring adolescent’s use and misuse of alcohol. Journal of Studies on Alcohol, 40, 291–300.
McCarty, C. A., Vander Stoep, A., Kuo, E., & McCauley, E. (2006). Depressive symptoms among delinquent youth. Journal of Psychopathology and Behavioral Assessment, 26, 85–93.
McClelland, G., Elkington, K., & Teplin, L. A. (2004). Multiple substance use disorders in juvenile detainees. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 1215–1224.
Ouimette, P., & Brown, S. (Eds.) (2003). Trauma and substance abuse. Washington, DC: American Psychological Association.
Pinto, M., & Grilo, C. (2004). Reliability, diagnostic efficiency, and validity of the Millon Adolescent Clinical Inventory. Behaviour Research and Therapy, 42, 1505–1519.
Pinto, A., Whisman, C., & McCoy, K. (1997). Suicidal ideation in adolescents: Psychometric properties of the Suicidal Ideation Questionnaire in a clinical sample. Psychological Assessment, 9, 63–66.
Pliszka, S. R., Sherman, J. O., Barrow, M. V., & Irick, S. (2000). Affective disorder in juvenile offenders. American Journal of Psychiatry, 157, 130–132.
Reynolds, W. M. (1988). Suicidal ideation questionnaire: Professional manual. Odessa, FL: PAR.
Rhode, P., Seeley, J. R., & Mace, D. E. (1997). Correlates of suicidal behavior in a juvenile detention population. Suicide and Life Threatening Behavior, 27, 164–175.
Robertson, A. A., Dill, P. L., Husain, J., & Undesser, C. (2004). Prevalence of mental illness and substance abuse disorders among incarcerated juvenile offenders in Mississippi. Child Psychiatry and Human Development, 35, 55–74.
Ryan, E. P., & Redding, R. E. (2004). A review of mood disorders among juvenile offenders. Psychiatric Services, 55, 1397–1407.
Sanislow, C. A., Grilo, C. M., Fehon, D. C., Axelrod, S. R., & McGlashan, T. H. (2003). Correlates of suicide risk in juvenile detainees and adolescent inpatients. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 234–240.
Schnurr, P., & Green, B. (2004). Trauma and health. Washington: American Psychological Association.
Snyder, H. N. (2004). Juvenile arrests 2002. Washington, DC: Office of Juvenile Justice and Deliniquency Programs. (2004). http://www.ncjrs.org/html/ojjdp/204608/contents.html.
Soler, M. (2002). Health issues for adolescents in the justice system. Journal of Adolescent Health, 31, 321–333.
Stewart, D., & Trupin, E. (2003). Clinical utility and policy implications of a statewide mental health screening process for juvenile offenders. Psychiatric Services, 54, 377–382.
Teicher, M., Samson, J., Polcari, A., & McGreenery, C. (2006). Sticks, stones, and hurtful words: relative effects of various forms of childhood maltreatment. American Journal of Psychiatry, 163, 993–1000.
Teplin, L. A., Abram, K. M., McClelland, G. M., Dulcan, M., & Mericle, A. (2002). Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry, 59, 1133–1143.
Terr, L. (1991). Childhood traumas: an outline and overview. American Journal of Psychiatry, 148, 10–20.
Velicer, W. (1976). The relation between Component score estimates, image scores and principal component scores. Educational and Psychological Measurement, 36, 149–159.
Wasserman, G. A., Jensen, P. S., Ko, S. J., Cocozza, J., Trupin, E., & Angold, A., et al. (2003). Mental health assessments in juvenile justice: Report on the consensus conference. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 751–761.
Wasserman, G. A., McReynolds, L., Ko, S., Katz, L., & Carpenter, J. (2005). Gender differences in psychiatric disorders at juvenile probation intake. American Journal of Public Health, 95, 131–137.
Wasserman, G. A., McReynolds, L. S., Ko, S. J., Katz, L. M., Kauffman, E., & Haxton, W., et al. (2004). Screening for emergent risk and service needs among incarcerated youth. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 629–639.
Widom, C. S. (1999). Posttraumatic stress disorder in abused and neglected children grown up. American Journal of Psychiatry, 156, 1223–1229.
Wolfe, D., Francis, K., & Straatman, A. (2006). Child abuse in religiously-affiliated institutions: long-term impact on men’s mental health. Child Abuse and Neglect, 30, 205–212.
Wolpaw, J. M., Ford, J. D., Ko, S. J., & Siegfried, C. B. (2004). Trauma assessment for youth in the juvenile justice system. Los Angeles: National Child Traumatic Stress Network (www.nctsnet.org).
Acknowledgements
The study was supported in part by a contract from the Connecticut State Court Support Services Division (CSSD) to the University of Connecticut School of Medicine Department of Psychiatry, and by a grant from the National Institute of Mental Health (MH01889-01A1), Julian D. Ford, Principal Investigator. The authors are grateful to CSSD colleagues (Mr. William Carbone, Mr. Karl Alston, Mr. Leo Arnone, Ms. Cathy Foley-Geib) for their support of this project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ford, J.D., Chapman, J.F., Pearson, G. et al. Psychometric Status and Clinical Utility of the MAYSI-2 with Girls and Boys in Juvenile Detention. J Psychopathol Behav Assess 30, 87–99 (2008). https://doi.org/10.1007/s10862-007-9058-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10862-007-9058-9