Abstract
Biofabrication is currently able to provide reliable models for studying the development of cells and tissues into multiple environments. As the complexity of biofabricated constructs is becoming increasingly higher their ability to closely mimic native tissues and organs is also increasing. Various biofabrication technologies currently allow to precisely build cell/tissue constructs at multiple dimension ranges with great accuracy. Such technologies are also able to assemble together multiple types of cells and/or materials and generate constructs closely mimicking various types of tissues. Furthermore, the high degree of automation involved in these technologies enables the study of large arrays of testing conditions within increasingly smaller and automated devices both in vitro and in vivo. Despite not yet being able to generate constructs similar to complex tissues and organs, biofabrication is rapidly evolving in that direction. One major hurdle to be overcome in order for such level of complex detail to be achieved is the ability to generate complex vascular structures within biofabricated constructs. This review describes several of the most relevant technologies and methodologies currently utilized within biofabrication and provides as well a brief overview of their current and future potential applications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The establishment of more reliable and versatile human tissue models is becoming an increasing need in order to properly understand human cells and tissues as well as their mode of interaction with a wide variety of external factors ranging from drugs to nanoparticle-based products.
On one hand, as drugs and medical treatments are becoming increasingly specific and personalized, the currently utilized in vitro human cell culture models and in vivo animal models are becoming obsolete since they are not able to closely mimic the environment and the properties of cells in human tissues and organs. On the other hand, man-made materials and products are also becoming increasingly complex, making the task of evaluating their biosafety through current methodologies extremely difficult if not impossible. As an example, the number of products containing manufactured nanoparticles (MNPs) is in constant increase with at least 200 new products entering the consumer markets every year [1] yet, increasing evidence shows that some of those nanoparticles may exert toxic effects both toward humans and environmental endpoints [2, 3].
Tissue engineering has emerged as a field aiming to generate living substitutes for damaged human tissues. Over the last two decades, various types of relatively simple tissue substitutes such as bone [4], cartilage [5] and skin [6], have been successfully generated in vitro, although not fully translated to clinical application due to their labour-intensive and costly production processes [7].
Automated technologies such as biofabrication are seen as the missing link for this transition to happen since they enable mass production of complex constructs in a timely and cost-effective manner [8]. Despite having as its long term goal to generate fully functional complex tissues and organs, biofabrication already shows the potential to radically change important industries such as the pharmaceutical and consumer product industries, simply by being able to generate constructs which more closely mimic native human tissues. Such improvement will greatly increase the reliability of the screening, testing and validation of products for human use.
In this short review we intend to demonstrate how tissue engineering-based biofabrication technologies may become a versatile tool for the rapid and reliable study of human cells and tissues and their interactions with external factors.
2 Single cell models
The concept of biofabrication is very broad and can be implemented by using a wide range of technologies at various size scales. As stated by Mironov et al. in 2009 [9], biofabrication can be generally defined as the production of complex living and non-living biological products from raw materials such as living cells, molecules, extracellular matrices, and biomaterials. In a more recent definition and in the scope of tissue engineering and regenerative medicine, biofabrication was further described as being capable of constructing or patterning materials, with a high degree of control, by finely tuning and defining material geometries, localization of biomolecular cues, and/or mechanical properties in order to resemble endogenous tissues [10].
The ability to manipulate single cells as building blocks within the context of biofabrication is of great importance not only for building larger complex and organized constructs from single cells but also for enabling the detailed study of tissues at the single cell level when exposed to external factors. An important advantage of biofabrication is that it enables to perform such characterization by means of high throughput screening (HTS) which consists of simultaneously characterizing extensive numbers of samples under automated and highly controlled conditions. HTS is widely utilised in pharmaceutical research for drug discovery purposes [11] given the large amount of compounds being constantly tested for many targets.
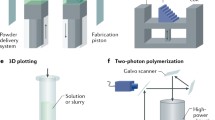
The technology underlying single cell printing can mainly be of two types, namely microfluidics-based or laser-based. In both cases, precisely positioned cells can be deposited into large organized arrays for testing (Fig. 1a). The microfluidics-based approach resorts to a concept very similar to the well-established fluorescence activated cell sorting (FACS). However, unlike FACS which requires cells to be fluorescently labelled in order to be manipulated [12, 13], microfluidics-based cell printing can instead resort to a label-free detection system which allows to accurately detect single cells as they are being dispensed onto substrates [14]. Microfluidics-based single cell printing can also be achieved to a certain extent by utilizing common inkjet printers, however inkjet printers do not possess any particle/cell detection systems integrated into their printing cartridges. For this reason the efficiency of single cell deposition in inkjet printers is highly based on probability resulting from the concentration and efficiency of dispersion of cells in the solution ejected from the print cartridge in the form of small droplets. The laser-based approach for printing single cells involves the selective transfer of cells from one substrate to another in order to generate defined patterns [15]. It consists of a multi-step procedure where cells are first spread over a transparent surface (target substrate) which is then turned upside down, and onto which a laser is then focused resulting in a droplet of cell solution being propelled through air toward a second surface (receiving substrate). The patterning of the transferred cells results from the relative alignment of the laser source, the target surface and the receiving substrate during transfer. The volume of transferred cell solution is a function of the laser energy, laser spot size, solution composition and thickness.
Scheme representing biofabricated cell/tissue models which can be of varying sizes and complexities depending on the technology utilized. a 2D array of single cell models which can be biofabricated through microfluidics-based or laser-based technologies, b biofabricated 3D cellular aggregate models, c bioprinted 3D model composed of vascular cells organized in a vessel-like structure surrounded by a second tissue composed of another cellular type, d biofabricated 3D scaffold seeded with cells
3 Cellular aggregate models
In the same way as single cells, cellular aggregates can also be biofabricated into organized arrays in order to serve as HTS study models (Fig. 1b). The utilized cells can be originated from either single or multiple sources allowing also to closely study the interactions taking place between multiple cells/cell types [16]. Cell printing has also been recently employed in reproducibly generating large arrays of human mesenchymal stem cells (hMSCs) spheroid pellets with incrementally increasing sizes which can be used for various applications [17]. Such strategy consisted of depositing incrementally increasing concentrations of cells directly into round bottom well plates which were then turned upside down in order to generate spheroids through the hanging-drop methodology [18]. Another main advantage of 3D cellular aggregates (such as spheroid pellets) is that they resemble more closely the three-dimensional organization of tissues since traditional two dimensional models are increasingly known for not being able to closely mimic the events taking place in native 3D tissue environments [19–22].
4 Bioprinted models
Bioprinting can be seen as the natural step forward from single cell printing and aggregate printing since it basically utilizes either cells or cellular aggregates to generate 3D cellular constructs possessing complex architectures (Fig. 1c). Bioprinting consists of the coordinated extrusion of cellular aggregates or gel-based cell suspensions onto a surface through a nozzle mounted in a 3D positioning system. This process is usually performed at room or physiological temperature preventing any damage to the extruded cells and gels. The process of bioprinting cellular aggregates starts with the patterned deposition of a gel filament which forms a thin layer possessing grooves [23]. A second layer consisting of cellular aggregates is then laid on top of these grooves resulting in the entrapment of the cellular aggregates into exact pre-determined positions. This process is repeated layer over layer generating a three-dimensional shape composed of cellular aggregates which further maturate and fuse together generating a continuous mass of cells with the pre-determined shape. Aggregate-based bioprinting has been largely employed in the generation of vascular constructs given that this process is able to simultaneously print various cellular types into complex shapes [23]. The special attention given to the printing of vascular structures relates to their unique role in delivering nutrients and oxygen and in removing metabolic residues from all of the organ systems in the body which becomes critical in the generation of larger and more complex tissues, organs and organisms [24]. In this context, gel-based cell suspension bioprinting has also been employed into generating vascular constructs with similar end results [25]. Better still, gel-based cell suspension bioprinting has shown to be a more straightforward process than cellular aggregate bioprinting since it does not require the laborious stage of preparing cellular aggregates by means of processes such as the hanging drop strategy. Through this simplified method, cells can be grown in standard culture flasks, quickly suspended in a gel and bioprinted right away. Furthermore, gels can also be easily combined with extra components such as i.e. drugs [26] or hydroxyapatite particles [27] in order to promote the formation of specific tissues as well as improve the mechanical properties of bioprinted constructs.
More recently, gels have also been employed in a different and somewhat original bioprinting strategy for generating vascular structures contained within two other bioprinted tissue types. In a study by Kolesly et al. [28], two different gel-based cellular suspensions and one sacrificial (fugitive) gel were first sequentially printed on top of each other within a casting chamber which was then filled with a GelMA gel. After crosslinking of the GelMA by ultraviolet exposure, the environmental temperature was reduced resulting in the liquification of the fugitive gel which could then be removed by aspiration. The resulting channels which were left engraved within the complex gel structure were then perfused with human umbilical vein endothelial cells (HUVEC) which attached to the channel’s walls resulting in the vascularization of the complex bioprinted construct. This process of generating perfusable channels within tissue engineered constructs by utilizing 3D printed sacrificial materials was also employed before in a study by Miller et al. [29] where a gel containing suspended cells was casted over a 3D printed carbohydrate glass structure. After crosslinking of the casted gel, the carbohydrate structure was dissolved leaving behind a channel network which could be further perfused with HUVEC which attached to the channel walls.
5 Biofabricated constructs combining cells and materials
The printing of constructs combining cells and materials is the most common type of biofabrication in the field of tissue engineering and regenerative medicine (Fig. 1d). This tendency is mainly inherited from the typically employed tissue engineering strategy of utilizing scaffold structures onto which cells are seeded and cultured until generating a tissue construct [30]. Along with many other processing techniques, additive manufacturing is able to produce such tissue engineering scaffolds but with the added advantage of being able to closely replicate the anatomical structures of tissues to be repaired to a high degree of complexity [31]. Given that in this strategy additive manufacturing is solely utilized for fabricating scaffolds composed of polymeric or composite materials it becomes therefore possible to generate structures with much better mechanical properties which can be applied to the regeneration of load-bearing tissues such as bone [32]. The main technologies employed in this strategy are fused deposition modelling (FDM) and selective laser sintering (SLS). Both of these technologies rely on the fusion of thermoplastic polymers or blends which are deposited in a layer-over-layer process either in the form of filaments extruded from a heated nozzle in the case of FDM [33] or in the form of powder which is selectively fused together by means of directed laser radiation in the case of SLS [34]. Another technology worth mentioning is melt electrospinning which operates in a similar way to FDM but which is able to generate filaments with smaller diameters due to the action of a strong electrical field which stretches the fused polymer filament as it is being extruded from the heated nozzle and deposited onto the deposition surface [35]. Melt electrospinning has been shown to enable the generation of highly organized three-dimensional structures according to pre-determined architectures by depositing the fused polymer onto a numerically controlled XY-moving stage under closely controlled conditions [36, 37]. Furthermore, melt electrospun structures can also be combined with other structures produced through methodologies such as FDM in order to generate complex scaffolds which are able to accommodate various types of cells/tissues in separate compartments of one single scaffold [38].
Combinations of multiple materials possessing various types of three-dimensional architectures can themselves also be screened in a high throughput manner for their ability to interact with cells and support their development into tissue substitutes [39–45]. Additive manufacturing can also be further employed to manufacture not only the scaffolds but as well the culture chambers where the cell/scaffold constructs are cultured [46]. By moving the design of both scaffold and culture chamber to a digital dimension and afterwards having the scaffold/chamber device manufactured by a single highly automated, standardized and precise machine (in this case a 3D printer) it becomes possible to achieve a higher level of reproducibility since the various manufacturing and culturing steps prone to generate variability in typical tissue engineering processes are simply eliminated. The superior mechanical properties of materials printed through technologies such as FDM and SLS also allow to generate structures with sufficient dimensional stability to withstand in vivo implantation. An additively manufactured device developed by Higuera et al. is currently utilized for screening combinations of cells and biomaterials for their tissue regeneration potential in a high throughput manner while implanted in vivo [47]. Up to 36 different conditions have been tested simultaneously in this small device while implanted subcutaneously in one single mouse model. Finally, material-based biofabrication has also recently been performed directly into defects of living animals establishing a precedent for the adoption of computer-assisted biofabrication-based medical interventions. In a very innovative work by Keriquel et al. [48] a laser-based 3D printing device was employed into the in situ fabrication of a 3D scaffold within a critical size calvarial defect of an anesthetized mouse. It was shown that the utilized laser printing procedure did not provoke any harmful effects on the mice’s brain and that the in vivo-printed scaffold composed of hydroxyapatite was well integrated into the defect site enabling the formation of new bone tissue. A future alternative to the utilization of laser printing in such an in situ strategy could be extrusion-based 3D printing of known osteoinductive in situ-setting cements such as calcium phosphate [49, 50]. Another alternative methodology for in situ fabrication of scaffolds recently suggested by Liebschner et al. [51] has been the fabrication of Lego-like building blocks possessing optimal biological and mechanical functionality which can be rapidly assembled in the operating room using robotic technology.
6 Future perspectives
The utilization of biofabricated constructs is already a reality mainly in generating simplified tissue/organ models. However, novel biofabrication technologies and methodologies are expected in the future to enable the generation of fully functional organs which apart from being the perfect models will also enable the replacement of damaged native organs. Currently existing biofabrication technologies are already equipped with advanced components able to three-dimensionally move and position cells and materials with extremely high levels of accuracy and precision. The next step for achieving an even greater degree of accuracy and precision in building tissue engineered constructs is now mostly related with the properties of bioinks (composed of cells and/or materials) which need to be optimized in order to be more accurately and precisely handled by biofabrication technologies. A major hurdle preventing the biofabrication of complex fully functional tissues/organs is still mainly related with the ability to combine multiple types of cells into complex architectures within large tissue/organ constructs. In particular, the generation of full vascular structures within biofabricated tissues and organs will be crucial to maintaining such constructs alive and to allowing their full integration into the host. In the same way, by integrating these organ-like constructs into advanced artificial life support systems (bioreactors) it will become possible to closely study and resolve medical conditions and diseases before they even take place in patients. In case of an already existing medical condition or disease taking place, a high level of optimization and personalization of the treatment will become possible by manufacturing multiple copies of the afflicted tissues/organs for pre-testing. The future potential of bioprinting is immense and will allow to significantly improve the quality of life and life expectancy of humans.
7 Conclusions
This review provided a brief outlook onto the utilization of biofabricated constructs as models for studying tissues and organs. Even though the greatly expected biofabrication of whole organs has not yet been achieved, biofabrication is already changing the way how tissues and organs are studied by providing reliable constructs with increasing complexity and resemblance to native tissues and organs. The biofabrication processes which allow to generate such constructs are reaching higher levels of reproducibility due to the increasingly higher levels of automation employed. Such automation has also been crucial into making high throughput screening processes simpler, easier, faster and less expensive, both in vitro and in vivo. By doing so, the interaction of cells and tissues with elements such as novel materials is becoming better understood, which in turn also further advances biofabrication technologies by enabling the discovery of novel material/cell bioinks. Lastly, biofabrication has been as well enabling the integration of multiple laborious and repetitive processes into small and automated devices which permit allocating valuable research and development human resources to more intellectually demanding tasks.
References
Project on Emerging Nanotechnologies. Consumer Products Inventory. Retrieved October 2013, from http://www.nanotechproject.org/cpi.
Levard C, Hotze EM, Lowry GV, Brown GE Jr. Environmental transformations of silver nanoparticles: impact on stability and toxicity. Environ Sci Technol. 2012;46(13):6900–14. doi:10.1021/es2037405.
Reidy B, Haase A, Luch A, Dawson K, Lynch I. Mechanisms of silver nanoparticle release, transformation and toxicity: a critical review of current knowledge and recommendations for future studies and applications. Materials. 2013;6(6):2295–350.
Quarto R, Mastrogiacomo M, Cancedda R, Kutepov SM, Mukhachev V, Lavroukov A, et al. Repair of large bone defects with the use of autologous bone marrow stromal cells. N Engl J Med. 2001;344(5):385–6. doi:10.1056/NEJM200102013440516.
Brun P, Dickinson SC, Zavan B, Cortivo R, Hollander AP, Abatangelo G. Characteristics of repair tissue in second-look and third-look biopsies from patients treated with engineered cartilage: relationship to symptomatology and time after implantation. Arthritis Res Ther. 2008;10(6):R132. doi:10.1186/ar2549.
Eaglstein WH, Falanga V. Tissue engineering and the development of Apligraf, a human skin equivalent. Clin Ther. 1997;19(5):894–905.
Mason C. Automated tissue engineering: a major paradigm shift in health care. Med Device Technol. 2003;14(1):16–8.
Costa PF, Martins A, Neves NM, Gomes ME, Reis RL. Automating the processing steps for obtaining bone tissue-engineered substitutes: from imaging tools to bioreactors. Tissue Eng B. 2014;. doi:10.1089/ten.TEB.2013.0751.
Mironov V, Trusk T, Kasyanov V, Little S, Swaja R, Markwald R. Biofabrication: a 21st century manufacturing paradigm. Biofabrication. 2009;1(2):022001. doi:10.1088/1758-5082/1/2/022001.
Bajaj P, Schweller RM, Khademhosseini A, West JL, Bashir R. 3D biofabrication strategies for tissue engineering and regenerative medicine. Annu Rev Biomed Eng. 2014;16:247–76. doi:10.1146/annurev-bioeng-071813-105155.
Pereira DA, Williams JA. Origin and evolution of high throughput screening. Br J Pharmacol. 2007;152(1):53–61. doi:10.1038/sj.bjp.0707373.
Fu AY, Spence C, Scherer A, Arnold FH, Quake SR. A microfabricated fluorescence-activated cell sorter. Nat Biotechnol. 1999;17(11):1109–11. doi:10.1038/15095.
Segerink LI, Koster MJ, Sprenkels AJ, van den Berg A. A low-cost 2D fluorescence detection system for mum sized beads on-chip. Lab Chip. 2012;12(10):1780–3. doi:10.1039/c2lc21187d.
Yusof A, Keegan H, Spillane CD, Sheils OM, Martin CM, O’Leary JJ, et al. Inkjet-like printing of single-cells. Lab Chip. 2011;11(14):2447–54. doi:10.1039/c1lc20176j.
Barron JA, Krizman DB, Ringeisen BR. Laser printing of single cells: statistical analysis, cell viability, and stress. Ann Biomed Eng. 2005;33(2):121–30.
Barron JA, Wu P, Ladouceur HD, Ringeisen BR. Biological laser printing: a novel technique for creating heterogeneous 3-dimensional cell patterns. Biomed Microdevices. 2004;6(2):139–47.
Faulkner-Jones A, Greenhough S, King JA, Gardner J, Courtney A, Shu W. Development of a valve-based cell printer for the formation of human embryonic stem cell spheroid aggregates. Biofabrication. 2013;5(1):015013. doi:10.1088/1758-5082/5/1/015013.
Kurosawa H, Imamura T, Koike M, Sasaki K, Amano Y. A simple method for forming embryoid body from mouse embryonic stem cells. J Biosci Bioeng. 2003;96(4):409–11. doi:10.1016/S1389-1723(03)90148-4.
Cukierman E, Pankov R, Stevens DR, Yamada KM. Taking cell-matrix adhesions to the third dimension. Science. 2001;294(5547):1708–12. doi:10.1126/science.1064829.
Sun T, Jackson S, Haycock JW, MacNeil S. Culture of skin cells in 3D rather than 2D improves their ability to survive exposure to cytotoxic agents. J Biotechnol. 2006;122(3):372–81. doi:10.1016/j.jbiotec.2006.12.021.
Birgersdotter A, Sandberg R, Ernberg I. Gene expression perturbation in vitro—a growing case for three-dimensional (3D) culture systems. Semin Cancer Biol. 2005;15(5):405–12. doi:10.1016/j.semcancer.2005.06.009.
Hutmacher DW. Biomaterials offer cancer research the third dimension. Nat Mater. 2010;9(2):90–3. doi:10.1038/Nmat2619.
Norotte C, Marga FS, Niklason LE, Forgacs G. Scaffold-free vascular tissue engineering using bioprinting. Biomaterials. 2009;30(30):5910–7. doi:10.1016/j.biomaterials.2009.06.034.
Schmidt-Nielsen K. Scaling in biology: the consequences of size. J Exp Zool. 1975;194(1):287–307. doi:10.1002/jez.1401940120.
Skardal A, Zhang J, Prestwich GD. Bioprinting vessel-like constructs using hyaluronan hydrogels crosslinked with tetrahedral polyethylene glycol tetracrylates. Biomaterials. 2010;31(24):6173–81. doi:10.1016/j.biomaterials.2010.04.045.
Kaigler D, Silva EA, Mooney DJ. Guided bone regeneration using injectable vascular endothelial growth factor delivery gel. J Periodontol. 2012;84(2):230–8. doi:10.1902/jop.2012.110684.
Wust S, Godla ME, Muller R, Hofmann S. Tunable hydrogel composite with two-step processing in combination with innovative hardware upgrade for cell-based three-dimensional bioprinting. Acta Biomater. 2014;10(2):630–40. doi:10.1016/j.actbio.2013.10.016.
Kolesky DB, Truby RL, Gladman AS, Busbee TA, Homan KA, Lewis JA. 3D bioprinting of vascularized, heterogeneous cell-laden tissue constructs. Adv Mater. 2014;26(19):3124–30. doi:10.1002/adma.201305506.
Miller JS, Stevens KR, Yang MT, Baker BM, Nguyen DH, Cohen DM, et al. Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues. Nat Mater. 2012;11(9):768–74. doi:10.1038/nmat3357.
Langer R, Vacanti JP. Tissue engineering. Science. 1993;260(5110):920–6.
Hollister SJ. Porous scaffold design for tissue engineering. Nat Mater. 2005;4(7):518–24. doi:10.1038/nmat1421.
Williams JM, Adewunmi A, Schek RM, Flanagan CL, Krebsbach PH, Feinberg SE, et al. Bone tissue engineering using polycaprolactone scaffolds fabricated via selective laser sintering. Biomaterials. 2005;26(23):4817–27. doi:10.1016/j.biomaterials.2004.11.057.
Zein I, Hutmacher DW, Tan KC, Teoh SH. Fused deposition modeling of novel scaffold architectures for tissue engineering applications. Biomaterials. 2002;23(4):1169–85. doi:10.1016/S0142-9612(01)00232-0.
Eosoly S, Brabazon D, Lohfeld S, Looney L. Selective laser sintering of hydroxyapatite/poly-epsilon-caprolactone scaffolds. Acta Biomater. 2010;6(7):2511–7. doi:10.1016/j.actbio.2009.07.018.
Dalton PD, Lleixa Calvet J, Mourran A, Klee D, Moller M. Melt electrospinning of poly-(ethylene glycol-block-epsilon-caprolactone). Biotechnol J. 2006;1(9):998–1006. doi:10.1002/biot.200600064.
Brown TD, Dalton PD, Hutmacher DW. Direct writing by way of melt electrospinning. Adv Mater. 2011;23(47):5651–7. doi:10.1002/adma.201103482.
Farrugia BL, Brown TD, Upton Z, Hutmacher DW, Dalton PD, Dargaville TR. Dermal fibroblast infiltration of poly(epsilon-caprolactone) scaffolds fabricated by melt electrospinning in a direct writing mode. Biofabrication. 2013;5(2):025001. doi:10.1088/1758-5082/5/2/025001.
Costa PF, Vaquette C, Zhang Q, Reis RL, Ivanovski S, Hutmacher DW. Advanced tissue engineering scaffold design for regeneration of the complex hierarchical periodontal structure. J Clin Periodontol. 2014;41(3):283–94. doi:10.1111/jcpe.12214.
Simon CG Jr, Stephens JS, Dorsey SM, Becker ML. Fabrication of combinatorial polymer scaffold libraries. Rev Sci Instrum. 2007;78(7):072207. doi:10.1063/1.2755761.
Zapata P, Su J, Garcia AJ, Meredith JC. Quantitative high-throughput screening of osteoblast attachment, spreading, and proliferation on demixed polymer blend micropatterns. Biomacromolecules. 2007;8(6):1907–17. doi:10.1021/Bm061134t.
Nakajima M, Ishimuro T, Kato K, Ko IK, Hirata I, Arima Y, et al. Combinatorial protein display for the cell-based screening of biomaterials that direct neural stem cell differentiation. Biomaterials. 2007;28(6):1048–60. doi:10.1016/j.biomaterials.2006.10.004.
Albrecht DR, Tsang VL, Sah RL, Bhatia SN. Photo- and electropatterning of hydrogel-encapsulated living cell arrays. Lab Chip. 2005;5(1):111–8. doi:10.1039/B406953f.
Simon CG Jr, Eidelman N, Kennedy SB, Sehgal A, Khatri CA, Washburn NR. Combinatorial screening of cell proliferation on poly(L-lactic acid)/poly(D, L-lactic acid) blends. Biomaterials. 2005;26(34):6906–15. doi:10.1016/j.biomaterials.2005.04.050.
Kohn J. New approaches to biomaterials design. Nat Mater. 2004;3(11):745–7. doi:10.1038/Nmat1249.
Anderson DG, Levenberg S, Langer R. Nanoliter-scale synthesis of arrayed biomaterials and application to human embryonic stem cells. Nat Biotechnol. 2004;22(7):863–6. doi:10.1038/nbt981.
Costa PF, Vaquette C, Baldwin J, Chhaya M, Gomes ME, Reis RL, et al. Biofabrication of customized bone grafts by combination of additive manufacturing and bioreactor knowhow. Biofabrication. 2014;6(3):035006. doi:10.1088/1758-5082/6/3/035006.
Higuera GA, Hendriks JA, van Dalum J, Wu L, Schotel R, Moreira-Teixeira L, et al. In vivo screening of extracellular matrix components produced under multiple experimental conditions implanted in one animal. Integr Biol. 2013;5(6):889–98. doi:10.1039/c3ib40023a.
Keriquel V, Guillemot F, Arnault I, Guillotin B, Miraux S, Amedee J, et al. In vivo bioprinting for computer- and robotic-assisted medical intervention: preliminary study in mice. Biofabrication. 2010;2(1):014101. doi:10.1088/1758-5082/2/1/014101.
Xu HH, Burguera EF, Carey LE. Strong, macroporous, and in situ-setting calcium phosphate cement-layered structures. Biomaterials. 2007;28(26):3786–96. doi:10.1016/j.biomaterials.2007.05.015.
Song G, Habibovic P, Bao C, Hu J, van Blitterswijk CA, Yuan H, et al. The homing of bone marrow MSCs to non-osseous sites for ectopic bone formation induced by osteoinductive calcium phosphate. Biomaterials. 2013;34(9):2167–76. doi:10.1016/j.biomaterials.2012.12.010.
Liebschner MAK, Chun K, Behni B. Intra-Operative Patient Specific Functional Scaffold Fabrication. Orthopaedic Research Society Annual Meeting; February; San Francisco (USA); 2012.
Acknowledgments
Pedro F. Costa would like to thank the TUM University Foundation for his current Postdoctoral fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costa, P.F. Biofabricated constructs as tissue models: a short review. J Mater Sci: Mater Med 26, 156 (2015). https://doi.org/10.1007/s10856-015-5502-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-015-5502-7