Abstract
In regenerative dentistry, stem cell-based therapy often requires a scaffold to deliver cells and/or growth factors to the injured site. Graphene oxide (GO) and silk fibroin (SF) are promising biomaterials for tissue engineering as they are both non toxic and promote cell proliferation. On the other hand, periodontal ligament stem cells (PDLSCs) are mesenchymal stem cells readily accessible with a promising use in cell therapy. The purpose of this study was to investigate the effects of composite films of GO, SF and GO combined with fibroin in the mesenchymal phenotype, viability, adhesion and proliferation rate of PDLSCs. PDLSCs obtained from healthy extracted teeth were cultured on GO, SF or combination of GO and SF films up to 10 days. Adhesion level of PDSCs on the different biomaterials were evaluated after 12 h of culture, whereas proliferation rate of cells was assessed using the MTT assay. Level of apoptosis was determined using Annexin-V and 7-AAD and mesenchymal markers expression of PDLSCs were analyzed by flow cytometry. At day 7 of culture, MTT experiments showed a high rate of proliferation of PDLSCs growing on GO films compared to the other tested biomaterials, although it was slightly lower than in plastic (control). However PDLSCs growing in fibroin or GO plus fibroin films showed a discrete proliferation. Importantly, at day 10 of culture it was observed a significant increase in PDLSCs proliferation rate in GO films compared to plastic (P < 0.05), as well as in GO plus fibroin compared to fibroin alone (P < 0.001). Flow cytometry analysis showed that culture of PDLSCs in fibroin, GO or GO plus fibroin films did not significantly alter the level of expression of the mesenchymal markers CD73, CD90 or CD105 up to 168 h, being the cell viability in GO even better than obtained in plastic. Our findings suggest that the combination of human dental stem cells/fibroin/GO based-bioengineered constructs have strong potential for their therapeutic use in regenerative dentistry.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Graphene is a recent addition to the family of carbon-based materials such as graphite, fullerenes, nanotubes, nanowires and nanoribbons. It is a sheet of two-dimensional single layer sp2 hybridized carbon atoms in a honeycomb lattice configuration [1]. Because of the singularity of its molecular configuration, graphene shows outstanding properties. It has a high electric and thermal conductivities, and high mechanical strength, as well as excellent optical properties. Thus, graphene is being developed in a considerable diversity of applications in fields as diverse as energy conversion [2] biosensing [3], imaging [4] and the fabrication of all kind of electronic, optical and energy storage devices [1, 5].
This versatility is also related to the fact that graphene is not a single chemical species but rather a diverse family of nanomaterials with different fabrication techniques. Graphene can be produced as a monolayer on a copper foil by carbon vapour deposition (CVD) that after etching of the metal can be transferred to different types of bidimensional substrates. Alternatively, graphene can be exfoliated from graphite, under very oxidative chemical treatment that yields graphene oxide (GO), which takes the form of nanoflakes of variable number of layers and with many carboxilate and epoxy groups. This reactivity allows the formation of stable GO colloidal aqueous solutions that can be reduced again to graphene, with a variety of reductants, recovering in this way part of its original properties [1, 5, 6].
The graphene family of nanomaterials also shows interesting biological properties. Although the issue of graphene biocompatibility is still object of some study and debate, it is generally considered as a biocompatible and implantable material when formulated in the adequate amount [7]. Moreover, its considerable chemical reactivity opens a wide field of uses on gene and drug delivery and other applications in the biomedical field [8, 9]. Interestingly, graphene surfaces have a good affinity with cells. Numerous reports have noted the optimal adhesion and proliferation of diverse type of cells in plastic or glass plates coated with graphene or GO [10, 11]. But a remarkable aspect is that the chemical nature of the graphene seems to act on the differentiation of stem cells, raising the possibility of favoring this process by modifying the chemical configuration of this material [12–15]. These evidences give to the material a considerable potential as a component in tissue engineering (TE) scaffolds [16].
However, some work has to be done in order to fabricate graphene in the suitable configurations for covering the many requirements of stem cells scaffolds. Most of the experiments made to date to illustrate the behavior of cells on graphene surfaces have been made in glass or plastic surfaces covered by graphene monolayers, or papers made by GO flakes recovered by filtration of an aqueous solution. But these constructs are scarcely implantable, reducing their applicability in a biological context. As a consequence, the need arise to develop composite materials where graphene could provide their excellent properties, while a polymeric filler could give tridimensionality and mechanical strength to the construct.
Many different types of composites exist and are being developed based on graphene [17], but most of the fillers used are not apt for their use in a cellular environment. In search of a biocompatible graphene composite, a natural candidate could be a film made by silk fibroin (SF) and GO. SF is widely described and used as a biocompatible material in the fabrication of cellular scaffolds for TE.
A composite of the two materials has already been proposed. A film fabricated with spin-coated alternate layers resulted in a construct of an unusually high mechanical strength [18]. In a later evolution, the same group made a composite film by the simple procedure of mixing an aqueous solution of fibroin with other of GO, followed by casting and drying [19]. This fact opens a set of applications of the new SF/GO composite in several fields, but its performance as a substrate for cell growing has not been addressed yet. This evaluation could be relevant, as scaffolds with a film configuration have a wide scope of applications in TE.
A field that could be improved by the availability of an effective film scaffold would be the reparation of periodontal tissues. The periodontium, which is composed of four dental tissues (i.e., gingiva, alveolar bone, cementum, and periodontal ligament [PDL]), is constantly maintained by periodontal ligament stem cells (PDLSCs) owing to their great capacity of differentiation into cementoblasts, odontoblasts, and fibroblasts. PDL plays a key role in the attachment of teeth to the jaw; in the most drastic cases of periodontitis, which is associated with a chronic inflammation process, PDL destruction could lead to the loss of the tooth [20]. With the aim of expanding TE therapy to as many patients as possible, acellular biomaterials may be employed as a novel approach to heal periodontal site by the active recruitment of autologous cells into the PDL scaffold, thus providing an in situ regeneration in cases of periodontitis. So, in order to make the evaluation of the mentioned SF/GO composite film as scaffold, human dental stem cells were chosen as cellular model in this work. These cells are generally applied in cellular therapies for tissue and organ regeneration [20]. To date, several types of adult stem cells have been isolated from teeth, including dental pulp stem cells (DPSCs) [21], stem cells from human exfoliated deciduous teeth (SHEDs) [22], PDLSCs [23], dental follicle progenitor stem cells (DFPCs) [24], and stem cells from apical papilla (SCAPs) [25].
PDLSCs are multipotent cells that proliferate extensively (maintained for at least 25 passages), can be safely cryopreserved, possess immunosuppressive properties, and express mesenchymal stem cell markers. These adherent cells are morphologically identical to the mesenchymal stem cells obtained from other sources such as the bone marrow (BMMSCs) [21]. Also PDLSCs can differentiate in vitro into cells of the three germinal layers, including ectoderm (neural cells), mesoderm (myocytes, osteoblasts, chondrocytes, adipocytes, and cardiomyocytes), and endoderm (hepatic cells) [26].
The goal of this study was to analyze the performance of a composite film made of SF and GO in cell adhesion and proliferation, viability and mesenchymal phenotype expression of PDLSCs and compare these effects with obtained using these two biomaterials individually. If effective, the SF/GO composite could be a viable therapeutic tool to develop a scaffold with enhanced inductive properties for supporting the growth of PDL in a clinical approach.
2 Materials and methods
2.1 Films preparation
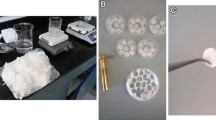
Cocoons of Bombyx mori were obtained from silkworms reared in the sericulture facilities of the IMIDA (Murcia, Spain) and GO water dispersion (4 mg/mL) was provided by GRAPHENEA (San Sebastian, Spain). Forty eight-well tissue culture plates (Nunclon™) were used to prepare different films composed of GO, SF and SF plus GO. After handling, all tissue culture plates were sterilized by immersion in 70 % ethanol.
To make GO films a GO water dispersion (250 µL/well) at 4 mg/mL was evaporated at r/t into 48-well tissue culture plates, leading to the formation of brown films composed of 1 mg of GO, covering the bottom of each well.
For SF films, cocoons of silkworms were chopped in 4 or 5 pieces and boiled in 0.02 M Na2CO3 for 30 min to remove the glue-like sericin proteins. Then raw SF was rinsed thoroughly with water and dried at r/t for 3 days. The extracted SF was dissolved in 9.3 M LiBr (Acros Organics) for 3 h at 60 °C to generate a 20 % w/v solution that was dialyzed against distilled water for 3 days (Snakeskin Dialysis Tubing 3.5 kDa MWCO, Thermo Scientific) with 8 total water changes. The resultant 6 % w/v SF dissolution was recovered, filtered and stored at 4 °C for no longer than 30 days. SF films were obtained by casting 100 µL of 3 % w/v SF aqueous dissolution per well (3 mg/well), once dried at room temperature, these films were annealed within a water filled desiccator in vacuum conditions for 24 h to produce water insoluble films.
To manufacture the composite films of SF and GO, a mixture of 250 µL of GO water dispersion (4 mg/mL) and 100 µL of SF water dissolution (3 % w/v) was evaporated at r/t inside each well of the tissue culture plates, then these materials were water annealed as it was previously described. The resultant films were opaque and light brown.
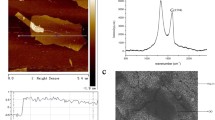
2.2 Scanning electron microscopy (SEM)
Scanning electron microscopy (SEM) was used to characterize the surface of the materials in order to understand possible implications of their topography on cell adhesion and proliferation.
Films were dryed and gold coated and then visualized using a Jeol T-6100 scanning electron microscope at 15 kV. Several pictures of the films were taken (surfaces and edges).
2.3 Isolation and culture of PDLSCs
Human periodontal ligaments (hPDL) were obtained from impacted third molars from 14 healthy subjects. Donors gave written an informed consent according to the guidelines of the Ethics Committee of our Institution. hPDLs was scraped from the middle third region of the root surface. After extraction hPDLs was washed with Ca2+/Mg2+-free Hank’s balance salt solution (HBSS) (Gibco, Gaithersburg, MD, USA), and immersed in a solution containing 3 mg/mL collagenase type I (Sigma-Aldrich, St. Louis, MO, USA) for 1 h at 37 °C. Cells obtained after this treatment were seeded into two 25 cm2 plastic tissue culture flasks (BD Biosciences, San Diego, CA, USA) in DMEM supplemented with penicillin/streptomycin (PAA Laboratories, Pasching, Austria), l-glutamine (PAA Laboratories) and 10 % fetal bovine serum (FBS) (Gibco Invitrogen, Paisley, Scotland) (complete medium) and incubated at 37 °C in a humid atmosphere containing 7.5 % CO2 for 3 days. After 3 days of initial seeding, red blood cells and other non-adherent cells were removed and fresh medium was added to allow further growth. The adherent cells were grown to 80 % of confluence and were defined as passage zero (P0). For passaging, cells were washed with Ca2+/Mg2+-free phosphate-buffered saline (PBS) (Gibco Invitrogen) and detached by incubating with 0.25 % trypsin–EDTA solution (Gibco Invitrogen) for 2-5 min at 37 °C. Culture medium was added in order to inactivate the trypsin activity. Then, cells were centrifuged at 200×g for 10 min and plated in 75 cm2 flasks at a density of 6 × 103 cells/cm2.
2.4 Analysis of cell morphology on graphene and fibroin-based biomaterials
PDLSCs were resuspended in complete medium at a density of 3.0 × 104 cells/cm2, seeded in 48-wells plates coated with the different biomaterials and incubated for 48, 72, 96 and 168 h at 37 °C. After, cells were fixed with 4 % paraformaldehyde in PBS and permeabilized with 0.25 % Triton-X. For staining of F-actin and nucleus, cells were incubated with CruzFluor594-conjugated Phalloidin (Santa Cruz Biotechnology, Dallas, TX, USA) and 4′,6-diamidino-2-phenylindole dihydrochloride (DAPI) (Sigma Aldrich), respectively. Images were acquired using an epifluorescence microscope (Nikon, Tokyo, Japan).
2.5 Adhesion and proliferation assays
For analyze the initial adhesion level of PDLSCs on the different biomaterials, cells were resuspended in complete medium, added to wells at a density of 3.0 × 104 cells/cm2 and allowed to adhere for 12 h at 37 °C. After, nonbound cells were removed by washing with PBS, whereas adherent cells were detached using a 0.25 % w/v trypsin–EDTA solution and counted using an automatic cell counter (BioRad, Hercules, CA, USA).
The increase in the cell number growing on the different biomaterials was evaluated using the MTT assay (MTT Cell Growth Kit, Chemicon, Rosemont, IL, USA). This assay is based on the ability of the mitochondrial dehydrogenase enzymes to convert the yellow water-soluble tetrazolium salt 3-(4,5-dimethyl-thiazol)-2,5-diphenyl-tetrazolium bromide into coloured compounds of formazan, whose absorbance is proportional to the amount of living cells. The proliferation of PDLSCs was analyzed at 48, 72, 96, 168 h and at day 10. Suspensions of the isolated cells from hPDL were prepared in complete medium at a density of 3.0 × 104 cells/cm2 and seeded into 48-well cell culture plates previously coated with fibroin, graphene or fibroin plus graphene films, in a total volume of 100 μL/well. Other PDLSCs were seeded in plastic in order to be used as a quality control of the cells seeded into the composites. Wells were washed twice with PBS and 50 µL of MTT solution (1 mg/mL) was added to the culture and incubated for 4 h. Thereafter, each well was washed with 300 μL of PBS 1X, and 100 µL of Dimethyl sulfoxide (DMSO) was added to extract and solubilize the formazan. The optical density at 570 nm (OD570) was measured by using an automatic microplate reader (ELx800; Bio-Tek Instruments, Winooski, VT, USA) using OD690 as reference wavelength. Each condition of the assay was analyzed in quintuplicate. Data worksheets were imported to Excel software (Office 2007; Microsoft Corporation, Redmond, WA, USA) and subjected to statistical analysis.
2.6 Analysis of expression of mesenchymal stem cell surface markers by flow cytometry
To analyze possible phenotypic changes in the expression of mesenchymal markers, PDLSCs were seeded at a density of 3.0 × 104 cells/cm2 in 48-well plates previously coated with fibroin, graphene or fibroin plus graphene films and cultured in complete medium for 24, 48, 72, 96 or 168 h at 37 °C. After, cells were detached using a 0.25 % w/v trypsin–EDTA solution, washed with PBS and incubated in the dark at 4 °C for 30 min with fluorescence-conjugated monoclonal antibodies for CD73, CD90, CD105, CD14, CD20, CD34 and CD45 (Miltenyi Biotec, Bergisch Gladbach, Germany). The determination of these markers are recommended by the International Society of Cellular Therapy (ISCT) as essential to confirm the mesenchymal phenotype of the cells [27, 28]. After labelling and washing, cells were acquired using a Beckman Coulter Navios flow cytometer (Fullerton, CA, USA) and analyzed with Kaluza analysis software. Non-specific fluorescence was measured using specific isotype monoclonal antibodies.
2.7 Determination of cellular viability (Annexin V/7-AAD staining)
To study the viability of the cells growing on the different biomaterials up to 168 h, Annexin-V and 7-AAD (BD Biosciences) were used according to the manufacturer’s instructions. Briefly, cells were cultured, detached and washed as described above and incubated with PE-conjugated Annexin-V and 7-AAD in Annexin-V-binding buffer at r/t for 15 min. Annexin-V single positive cells and Annexin-V/7-AAD double positive cells were considered as early or late apoptotic respectively. The percentage of live (Annexin-V−/7-AAD−), early apoptotic (Annexin+/7-AAD−) or late apoptotic and necrotic cells (Annexin-V+/7-AAD+) were analyzed in a Beckman Coulter Navios flow cytometer. Subsequently, percentages of each population were calculated. All determinations were performed in triplicate.
2.8 Statistical analysis
Statistical analysis was performed using SPSS version 15.0 statistical software (SPSS, Inc., Chicago, IL, USA) and group comparisons were conducted using a Student’s t test. All values are presented as the mean ± standard deviation (SD). P < 0.05 was considered as statistically significant difference.
3 Results
3.1 Characterization of surface topography by SEM
Pictures obtained by SEM were used in order to visualize the surface of the different films (Fig. 1). Films composed of fibroin showed a flat surface with some dispersed nanometric structures. The same appearance was observed also on GO films, but in this case a lot of fissures were detected, this fact explained the high brittleness of these materials. On the other hand, the edges of GO materials exhibited a multilayered aspect, denoting the sedimentation pattern of GO flakes during the formation of those films.
Films composed of SF/GO mixtures showed a higher roughness when compared with the other two materials. These films have a wrinkled surface topography that can be easily observed at low magnification. A cross-sectional multilayered appearance was detected on the edges of the materials.
3.2 Morphology of PDLSCs on graphene and fibroin-based biomaterials
All PDLSCs displayed plastic adherent characteristics when maintained in standard culture conditions using tissue culture flasks. From a morphologic point of view, PDLSCs were quite heterogeneous, fibroblast-like or spindle shaped and displaying many cytoplasmic lamellipodia (Fig. 2a). In addition, to evaluate the morphology of PDLSCs on the different biomaterials, cells were allowed to grow for the indicated times in plastic (control), fibroin, GO or GO plus fibroin films and stained with phalloidin (red fluorescence) and DAPI (blue fluorescence) to visualize actin cytoskeleton and nucleus, respectively (Fig. 2b). When using plastic, PDLSCs showed a gradual increase of growth over time, an extended morphology and a high content of F-actin, reaching confluence at 168 h of culture. On the other hand, PDLSCs cultured on the GO surface showed an initial slight growth delay compared to plastic, which was recovered from 96 h of culture. However, when cultured on fibroin, PDLSCs displayed a lower growth rate and cellular spreading, showing decreased levels of F-actin. Importantly, when using the composite film of GO and fibroin, PDLSCs displayed an increased growth rate and F-actin content at 168 h compared to cells cultured on fibroin alone.
Morphology of PDLSCs cultured on graphene and fibroin-based biomaterials. a Microscopic images showing the plastic adherence properties and spindle shape morphology with extended cytoplasmatic cellular structures typical of PDLSCs. b PDLSCs were cultured for the indicated times on plastic, fibroin, GO or GO plus fibroin biomaterials. After fixation and permeabilization, cells were incubated with CruzFluor594-Phalloidin (red fluorescence) and DAPI (blue fluorescence). Representative fluorescence images of each condition are shown. Scale bar 100 μm (Color figure online)
3.3 Effect of GO and fibroin on PDLSCs adhesion and proliferation
For analyzing the initial adhesion of PDLSCs on the different surfaces, cells were allowed to adhere for 12 h at 37 °C, and after removing nonbound cells, attached cells were quantified. When using plastic, extent of adhesion of PDLSCs was 40 %, whereas on fibroin, GO and GO plus fibroin the level of adhesion were significantly lower compared to plastic (P < 0.01, according to Student’s t test) (Fig. 3a). However, initial adhesion showed by PDLSCs on GO and GO plus fibroin were slightly higher than on fibroin, although significant (P < 0.05).
Effect of GO and fibroin-based biomaterials on PDLSCs adhesion and proliferation. a PDLSCs were added to wells coated with fibroin, GO or the composite film of GO and fibroin. After 12 h at 37 °C, adherent cells were quantified using an automatic cell counter. Percentage of adhesion was significantly decreased, ** P < 0.01, compared to plastic (control), or significantly augmented, δ P < 0.05, compared to fibroin alone, according to Student’s t test (B) Cell proliferation rates of PDSCs cultured in the different composite films for the indicated times was determined using the MTT assay. Cell proliferation was significantly decreased, ** P < 0.01, *** P < 0.001, or significantly augmented, Δ P < 0.05, compared to plastic (control), respectively, Also, cell proliferation was significantly increased, δ P < 0.05, δδ P < 0.01, δδδ P < 0.001 compared to that achieved when using fibroin films, according to Student’s t test
In addition, we measured the proliferation rate of PDLSCs growing in GO, SF or a combination of GO and SF films and were compared with the proliferation shown by PDLSCs cultured in plastic (control) after periods of 48, 72, 96, 168, 196 and 240 h. MTT cell proliferation assay confirmed the visual observations and the absorbance data obtained in each experimental condition were analyzed using the Student’s t test. After 48 h of culture, the proliferation rate of PDLSCs growing on GO, fibroin or GO plus fibroin films were comparable, although it were slightly higher and statistically significant in GO and GO plus fibroin compared to fibroin alone (P < 0.001, according to Student’s t test). Also proliferation was significantly lower in all tested biomaterials compared to plastic (Fig. 3b). At day 7, PDLSCs showed a high cell proliferation rate in GO, although it was slightly lower than in plastic. At this time point fibroin or GO/fibroin biomaterials supported a discrete proliferation, although was significantly higher in GO/fibroin than in fibroin alone (P < 0.05). However, at day 10 of culture it was observed a higher and statistically significant cell proliferation in GO compared to plastic (P < 0.05), as well as in the composite film of GO and fibroin compared to fibroin alone (4,4-fold increase) (P < 0.001).
3.4 Analysis of mesenchymal phenotype and viability of PDLSCs cultured in GO and fibroin-based biomaterials
To evaluate the possible cellular cytotoxic effect of the different biomaterials employed as well as changes on the expression of mesenchymal surface markers, we cultured PDLSCs on plastic (control), fibroin, GO or GO plus fibroin films for different times up to 1 week (168 h). After, cells were detached, washed and analyzed by flow cytometry as described in Sect. 2. More than 95 % of the PDLSCs analyzed were positive for the mesenchymal markers CD73, CD90 and CD105 and negative for the hematopoietic markers CD14, CD20, CD34 and CD45 (Fig. 4 and not shown, respectively). Culture of PDLSCs on fibroin, GO or GO plus fibroin did not significantly alter the level of expression of CD73, CD90 or CD105 after 24, 48, 72, 96 or 168 h compared to expression levels displayed by PDLSCs cultured on plastic (Fig. 4). On the other hand, to assess cell viability we measured the binding of Annexin-V and 7-AAD, two colour flow cytometry analysis usually employed to analyze the apoptosis stage of cells. This method allows to detect three populations: live (left lower quadrant), early apoptotic (right lower quadrant) and both late and necrotic cells (right and left upper quadrants). PDLSCs cultured on plastic maintained their viability (Annexin-V−/7-AAD−) at all times of study tested, being the live population always higher than 88 % (Fig. 5, left column). When PDLSCs were cultured on fibroin films, there was a slight decrease on live cell percentage from 48 h up to 72 h, although later cells recovered a level of viability comparable to that achieved on plastic (Fig. 5, middle-left column). On the other hand, PDLSCs cultured on GO films underwent same initial small reduction in viability, although their recovery was faster than using fibroin (from 24 h), reaching at 168 h percentages of live cells even higher than those obtained using a plastic surface of culture (Fig. 5, middle-right column). However, when using a composite film of GO and fibroin the viability of PDLSCs was more compromised, mainly up to 48 h of culture. From 72 h of culture there was a partial recovery of cellular viability, although percentages of live cells were always slightly lower than in plastic (Fig. 5, right column).
Mesenchymal immunophenotype analysis of PDLSCs after culture in GO and fibroin-based biomaterials by flow cytometry. PDLSCs were cultured at 37 °C in plastic (control) or in composite films of fibroin, GO or GO plus fibroin for the indicated times. After, PDLSCs were labelled with fluorescence-conjugated specific antibodies for the mesenchymal markers CD73, CD90 and CD105 and hematopoietic markers CD14, CD20, CD34 and CD45 (not shown). Figure shows representative flow cytometry histograms obtained after three independent experiments
Effect of GO and fibroin-based biomaterials in PDLSCs viability. PDLSCs were cultured at 37 °C on plastic (control) or in composite films of fibroin, GO or GO plus fibroin for the indicated times, labelled with Annexin-V and 7-AAD and analyzed by flow cytometry. Insert numbers represent percentages of live (Annexin-V−/7-AAD−), early apoptotic (Annexin-V+/7-AAD−) or late apoptotic and necrotic cells (Annexin-V+/7-AAD+). Figure shows representative flow cytometry plots obtained after three independent experiments
4 Discussion
TE strategies combine living cells and scaffold materials to develop biological substitutes that can restore tissue functions. Both natural and synthetic materials have been fabricated for transplantation of stem cells and their specific differentiation into muscles, bones and dental tissues. One of the key objectives of the periodontal regeneration therapy to be successful is to direct stem cells to proliferate and accelerate their differentiation in a controlled manner through the use of growth factors and cementogenic inducers [20]. The present study evaluated the effects of the novel biomaterials GO and SF on mesenchymal stem cell phenotype, adhesion, proliferation rate and viability of PDLSCs. Biocompatibility of scaffolds is a prerequisite for generating cell-biomaterial constructs and for their successful clinical application. GO and fibroin-based biomaterials have been previously studied for several TE based-therapies [29–31], but they have never been tested in conjunction with mesenchymal stem cells isolated from PDL. Thus, due to the easy accessibility of this type of cells and their great ability to differentiate into other types of dental cells present in dentin and cementum such as odontoblasts and cementoblasts, we chose PDLSCs as source for mesenchymal stem cells [20, 32]. Recents studies reported the use of graphene for cell proliferation and osteogenic differentiaton with optimal results [13, 33, 34]. Aryaei et al. [35] showed that graphene did not have toxic effects on osteoblasts and demonstrated that graphene-coated substrates greatly improved the attachment of these cells. Regarding SF, some studies evidenced the capacity of this biomaterial in combination with bone marrow mesenchymal stem cells to favor cardiac repair in vivo [36]. Also, Riccio et al. [37] demonstrated the strong potential of stem cells/fibroin bioengineered constructs for correcting large cranial defects in an animal model. In this work we have studied the morphology of PDLSCs cultured for different times on GO and fibroin-coated surfaces by staining of actin cytoskeleton (Fig. 2b). Cells cultured on plastic showed a high content of F-actin and an adequate cell spreading and growth rate. However, PDLSCs cultured on fibroin displayed lower amounts of F-actin, lower spreading and delayed growth. Despite SF has been previously described as a biomaterial that allows an optimal adhesion of mesenchymal stem cells from other sources, PDLSCs showed a limited attachment to these biomaterial, discarding the possibility of use of fibroin alone in conjunction with these type of cells. By contrast, GO or GO plus fibroin-coated surfaces significantly improved F-actin content, cell spreading and growth rate from 96 h of culture when compared to fibroin alone. Moreover, it has been measured the initial cell adhesion of PDLSCs on the different biomaterials after a short period of 12 h (Fig. 3a). Adhesion level to fibroin, GO or GO plus fibroin was significantly lower than on plastic. These differences could be explained partially by a possible different distribution of deposited serum proteins due to the specific topographic characteristics of each biomaterial. Importantly, GO or GO plus fibroin-coated surfaces significantly improved this initial adhesion when compared to fibroin alone. Furthermore, it has been also studied the proliferation rate of PDLSCs on GO and fibroin-based biomaterials by MTT assays, a method normally used to evaluate the cell proliferation or induced cytotoxic effects. The advantages of the MTT procedure are the simplicity, accuracy, reliability, and time saving. After 7 days of culture, PDLSCs showed a high cell proliferation rate in presence of GO, although it was slightly lower than on plastic, whereas fibroin or GO/fibroin biomaterials supported a discrete proliferation (Fig. 3b). However, after 10 days of culture we observed a higher and significant cell proliferation on GO compared to plastic (P < 0.05), as well as on GO/fibroin combined biomaterial compared to fibroin (P < 0.001). Behavior shown by the fibroin film is not unexpected, being as it has been previously reported. Although fibroin usually improves adhesion and proliferation in the configuration of electrospun mats or 3D sponge, it is not as effective when fabricated as a film. Proliferation of human corneal keratocytes was significantly lesser on fibroin film as compared to TCP plastic [38]. In other work, a line of human corneal endothelial cells proliferated worse on fibroin film than on plastic, which was only improved with the coating with collagen or other extracellular matrix proteins [39]. However, data of Fig. 3b showed that the combination with GO significantly improved the performance of the fibroin film, as an alternative to the coating with collagen. In addition, to evaluate the possible cellular cytotoxic effect of the different biomaterials employed as well as changes on the expression of mesenchymal surface markers we characterized their surface molecule expression pattern by flow cytometry (Fig. 4). The International Society for Cellular Therapy states that multipotent mesenchymal stromal cells must express CD105, CD73, and CD90 and should be devoid of the expression of hematopoietic markers such as CD45, CD34, CD14, or CD11b [27, 28]. Culture of PDLSCs on fibroin, GO or GO plus fibroin did not significantly alter the level of expression of CD73, CD90 or CD105 after 24, 48, 72, 96 or 168 h compared to expression levels displayed by PDLSCs cultured on plastic. Thus, the biomaterials employed in this study were able to maintain the mesenchymal phenotype of PDLSCs. Rodríguez-Lozano et al. [40] previously demonstrated the persistence of mesenchymal markers expression in dental stem cells cultured on other biomaterials, so PDLSCs is a good candidate as mesenchymal stem cell. In addition, in the present work it was measured if GO, fibroin or GO plus fibroin could affect the viability of PDLSCs cultured in vitro on these biomaterials (Fig. 5). For this assay, the method of the double-staining of cells with Annexin-V and 7-AAD was chosen. Annexin-V staining precedes the loss of membrane integrity which accompanies the latest stages of cell death, resulting from either apoptotic or necrotic processes. Therefore, Annexin-V staining is typically used in combination with a vital dye such as 7-AAD to allow to identify the apoptosis in its different stages. It was found that PDLSCs cultured on plastic maintained their viability up to 168 h, being the live population always higher than 88 %. On the other hand, using GO, fibroin or GO/fibroin biomaterials there was an initial small reduction in viability compared to plastic, being GO plus fibroin the biomaterial with the higher reduction of this viability, mainly up to 48 h of culture. We could hypothesize that this initial effect could be due to a light delay in the cell attachment or limited initial adhesion on these biomaterials, as we shown in Figs. 2b, 3a. From 72 to 96 h of culture there was a partial recovery of cellular viability when using fibroin or GO plus fibroin biomaterials, reaching comparable percentages of live cells in fibroin to that achieved using plastic at 168 h, and somewhat lower than with GO plus fibroin. However, using a GO film we observed a rapid attachment and spreading of PDLSCs (Fig. 2b), that could allow a faster recovery of cellular viability compared to fibroin or GO plus fibroin biomaterials. At the final time point of the study (168 h) viability of PDLSCs cultured on the GO film was even higher than using plastic, highlighting the great cytocompatibility of this biomaterial. The SEM pictures are not resolutive enough to visualize the GO nanoflakes, that would require atomic force microscopy techniques that are usual in the literature on graphene. But they showed something of a lamellar structure, with layers that could be originated by the interaction between fibroin and GO flakes. A configuration of this type was described in previous papers on the fabrication of fibroin/graphene composites [18]. Their authors stated that the layered molecular structures of fibroin beta sheet and graphene flakes reinforce each other resulting in a very robust construction [18]. As a consequence, the present work shows that the composite film presents an interesting combination of biocompatibility, induction of proliferation and mechanical resistance, very apt to work in cellular environments where mechanical resistance is required. Akhavan et al. suggested that due to the high potential applications of graphene in TE (as delivery vehicles and scaffolds), graphene sheets with lower cytotoxicity seem to be a better selection with higher biomedical safety [41]. In concordance with our results, they did not observed any substantial morphological change of human mesenchymal stem cells in presence of graphene nor cellular apoptosis in their experiments. On the other hand, different studies suggested that SF film could be an excellent biomaterial with an optimal cytocompatibility, providing a framework for tissue reparation after trauma in clinical applications [36, 42]. Two previous papers reported by Tsukruk and co-authors [18, 19] have shown that fibroin is an excellent polymer to give structure and mechanical resistance to graphene materials. They also showed that the layered configuration of the two materials interacts in some way to produce films of unusually high robustness [18]. The resulting composite makes easier the use of graphene in diverse applications in the field of electrochemistry. In the present work, it is shown that this composite is also biocompatible and favors the proliferation of PDLSCs. This fact opens a big group of applications where interactions of physical devices and living tissues are required, such as biosensors, conductive scaffolds and so on. And in addition to that, the composite can be made with a very simple technique. As a consequence, this is a step in the way to take advantage of the many favorable properties of graphene in a biological environment. Also further additional studies using both fibroin and GO alternative configurations are required in order to improve their synergic properties, representing a promising field of extensive research in TE.
References
Allen MJ, Tung VC, Kaner RB. Honeycomb carbon: a review of graphene. Chem Rev. 2010;110(1):132–45.
Sahoo NG, Pan Y, Li L, Chan SH. Graphene-based materials for energy conversion. Adv Mater. 2012;24(30):4203–10.
Pumera M, Ambrosi A, Bonanni A, Chng ELK, Poh HL. Graphene for electrochemical sensing and biosensing. TrAC Trends Anal Chem. 2010;29(9):954–65.
Yao J, Sun Y, Yang M, Duan Y. Chemistry, physics and biology of graphene-based nanomaterials: new horizons for sensing, imaging and medicine. J Mater Chem. 2012;22:14313–29.
Geim AK. Graphene: status and prospects. Science. 2009;324(5934):1530–4.
Fernández-Merino MJ, Guardia L, Paredes JI, Villar-Rodil S, Solís-Fernández P, et al. Vitamin C is an ideal substitute for hydrazine in the reduction of graphene oxide suspensions. J Phys Chem C. 2010;114:6426–32.
Yang K, Li Y, Tan X, Peng R, Liu Z. Behavior and toxicity of graphene and its functionalized derivatives in biological systems. Small. 2013;9(9–10):1492–503.
Chung C, Kim YK, Shin D, Ryoo SR, Hong BH, Min DH. Biomedical applications of graphene and graphene oxide. Acc Chem Res. 2013;46(10):2211–24.
Shen H, Zhang L, Liu M, Zhang Z. Biomedical applications of graphene. Theranostics. 2012;2(3):283–94.
Kalbacova M, Broz A, Kong J, Kalbac M. Graphene substrates promote adherence of human osteoblasts and mesenchymal stromal cells. Carbon. 2010;48(15):4323–9.
Li N, Zhang X, Song Q, Su R, Zhang Q, Kong T, et al. The promotion of neurite sprouting and outgrowth of mouse hippocampal cells in culture by graphene substrates. Biomaterials. 2011;32(35):9374–82.
Akhavan O, Ghaderi E, Abouei E, Hatamie S, Ghasemi E. Accelerated differentiation of neural stem cells into neurons on ginseng-reduced graphene oxide sheets. Carbon. 2014;66:395–406.
Nayak TR, Andersen H, Makam VS, Khaw C, Bae S, Xu X, et al. Graphene for controlled and accelerated osteogenic differentiation of human mesenchymal stem cells. ACS Nano. 2011;5(6):4670–8.
Park SY, Park J, Sim SH, Sung MG, Kim KS, Hong BH, et al. Enhanced differentiation of human neural stem cells into neurons on graphene. Adv Mater. 2011;23(36):H263–7.
Chen GY, Pang DW, Hwang SM, Tuan HY, Hu YC. A graphene-based platform for induced pluripotent stem cells culture and differentiation. Biomaterials. 2012;33(2):418–27.
Goenka S, Sant V, Sant S. Graphene-based nanomaterials for drug delivery and tissue engineering. J Control Release. 2014;173:75–88.
Verdejo R, Bernal MM, Romasanta LJ, Lopez-Manchado MA. Graphene filled polymer nanocomposites. J Mater Chem. 2011;21:3301–10.
Hu K, Gupta MK, Kulkarni DD, Tsukruk VV. Ultra-robust graphene oxide-silk fibroin nanocomposite membranes. Adv Mater. 2013;25(16):2301–7.
Hu K, Tolentino LS, Kulkarni DD, Ye C, Kumar S, Tsukruk VV. Written-in conductive patterns on robust graphene oxide biopaper by electrochemical microstamping. Angew Chem Int Ed Engl. 2013;52(51):13784–8.
Rodríguez-Lozano FJ, Insausti CL, Iniesta F, Blanquer M, Ramírez MD, Meseguer L, et al. Mesenchymal dental stem cells in regenerative dentistry. Med Oral Patol Oral Cir Bucal. 2012;17(6):e1062–7.
Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci USA. 2000;97:13625–30.
Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, et al. SHED: stem cells from human exfoliated deciduous teeth. Proc Natl Acad Sci USA. 2003;100:5807–12.
Seo BM, Miura M, Gronthos S, Bartold PM, Batouli S, Brahim J, et al. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet. 2004;364:149–55.
Morsczeck C, Götz W, Schierholz J, Zeilhofer F, Kühn U, Möhl C, et al. Isolation of precursor cells (PCs) from human dental follicle of wisdom teeth. Matrix Biol. 2005;24:155–65.
Sonoyama W, Liu Y, Fang D, Yamaza T, Seo BM, Zhang C, et al. Mesenchymal stem cell-mediated functional tooth regeneration in swine. PLoS One. 2006;1:e79.
Rodríguez-Lozano FJ, Bueno C, Insausti CL, Meseguer L, Ramírez MC, Blanquer M, et al. Mesenchymal stem cells derived from dental tissues. Int Endod J. 2011;44:800–6.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–7.
Horwitz EM, Le Blanc K, Dominici M, Mueller I, Slaper-Cortenbach I, Marini FC, et al. Clarification of the nomenclature for MSC: the International Society for Cellular Therapy position statement. Cytotherapy. 2005;7:393–5.
Etienne O, Schneider A, Kluge JA, Bellemin-Laponnaz C, Polidori C, Leisk GG, et al. Soft tissue augmentation using silk gels: an in vitro and in vivo study. J Periodontol. 2009;80(11):1852–8.
Park J, Park S, Ryu S, Bhang SH, Kim J, Yoon JK, et al. Graphene-regulated cardiomyogenic differentiation process of mesenchymal stem cells by enhancing the expression of extracellular matrix proteins and cell signaling molecules. Adv Healthc Mater. 2014;3(2):176–81.
Kim TH, Lee KB, Choi JW. 3D graphene oxide-encapsulated gold nanoparticles to detect neural stem cell differentiation. Biomaterials. 2013;34(34):8660–70.
Bueno C, Ramirez C, Rodríguez-Lozano FJ, Tabarés-Seisdedos R, Rodenas M, Moraleda JM, et al. Human adult periodontal ligament-derived cells integrate and differentiate after implantation into the adult mammalian brain. Cell Transpl. 2013;22(11):2017–28.
Crowder SW, Prasai D, Rath R, Balikov DA, Bae H, Bolotin KI, et al. Three-dimensional graphene foams promote osteogenic differentiation of human mesenchymal stem cells. Nanoscale. 2013;5(10):4171–6.
Li X, Liu H, Niu X, Yu B, Fan Y, Feng Q, et al. The use of carbon nanotubes to induce osteogenic differentiation of human adipose-derived MSCs in vitro and ectopic bone formation in vivo. Biomaterials. 2012;33(19):4818–27.
Aryaei A, Jayatissa AH, Jayasuriya AC. The effect of graphene substrate on osteoblast cell adhesion and proliferation. J. Biomed Mater Res A. 2013. doi:10.1002/jbm.a.34993.
Chi NH, Yang MC, Chung TW, Chen JY, Chou NK, Wang SS. Cardiac repair achieved by bone marrow mesenchymal stem cells/silk fibroin/hyaluronic acid patches in a rat of myocardial infarction model. Biomaterials. 2012;33(22):5541–51.
Riccio M, Maraldi T, Pisciotta A, La Sala GB, Ferrari A, Bruzzesi G. Fibroin scaffold repairs critical-size bone defects in vivo supported by human amniotic fluid and dental pulp stem cells. Tissue Eng Part A. 2012;18(9–10):1006–13.
Lawrence BD, Marchant JK, Pindrus MA, Omenetto FG, Kaplan DL. Silk film biomaterials for cornea tissue engineering. Biomaterials. 2009;30(7):1299–308.
Madden PW, Lai JN, George KA, Giovenco T, Harkin DG, Chirila TV. Human corneal endothelial cell growth on a silk fibroin membrane. Biomaterials. 2011;32(17):4076–84.
Rodríguez-Lozano FJ, Serrano-Belmonte I, Pérez Calvo JC, Coronado-Parra MT, Bernabeu-Esclapez A, Moraleda JM. Effects of two low-shrinkage composites on dental stem cells (viability, cell damaged or apoptosis and mesenchymal markers expression). J Mater Sci Mater Med. 2013;24(4):979–88.
Akhavan O, Ghaderi E, Akhavan A. Size-dependent genotoxicity of graphene nanoplatelets in human stem cells. Biomaterials. 2012;33(32):8017–25.
Liu TL, Miao JC, Sheng WH, Xie YF, Huang Q, Shan YB, et al. Cytocompatibility of regenerated silk fibroin film: a medical biomaterial applicable to wound healing. J Zhejiang Univ Sci B. 2010;11(1):10–6.
Acknowledgments
We thank the teeth donors for their generosity. This work was supported by FIS EC07/90762 Grant and the Spanish Net of Cell Therapy (TerCel) provided by Carlos III Institute of Health (ISCiii) (RETICS RD07/0010/2012 and RD12/0019/0001) together with the Junction Program for Biomedical Research in Advanced Therapies and Regenerative Medicine from ISCiii and FFIS, and by the Fundación Seneca (Grant 08859/PI/08). Experiments made at the IMIDA were supported by funds from UE FEDER Operative Program Region of Murcia 2007–2013.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rodríguez-Lozano, F.J., García-Bernal, D., Aznar-Cervantes, S. et al. Effects of composite films of silk fibroin and graphene oxide on the proliferation, cell viability and mesenchymal phenotype of periodontal ligament stem cells. J Mater Sci: Mater Med 25, 2731–2741 (2014). https://doi.org/10.1007/s10856-014-5293-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-014-5293-2