Abstract
Synthetic patch materials currently in use have major limitations, such as high susceptibility to infections and lack of contractility. Biological grafts are a novel approach to overcome these limitations, but do not always offer sufficient mechanical durability in early stages after implantation. Therefore, a stabilising structure based on resorbable magnesium alloys could support the biological graft until its physiologic remodelling. To prevent early breakage in vivo due to stress of non-determined forming, these scaffolds should be preformed according to the geometry of the targeted myocardial region. Thus, the left ventricular geometry of 28 patients was assessed via standard cardiac magnetic resonance imaging (MRI). The resulting data served as a basis for a finite element simulation (FEM). Calculated stresses and strains of flat and preformed scaffolds were evaluated. Afterwards, the structures were manufactured by abrasive waterjet cutting and preformed according to the MRI data. Finally, the mechanical durability of the preformed and flat structures was compared in an in vitro test rig. The FEM predicted higher durability of the preformed scaffolds, which was proven in the in vitro test. In conclusion, preformed scaffolds provide extended durability and will facilitate more widespread use of regenerative biological grafts for surgical left ventricular reconstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Cardiac ejection is a function of the ventricular geometry. Amphibians, for instance, have a low systemic blood pressure and a spherical geometry of the heart, whereas the human heart has an almost ellipsoid form and maintains a systolic blood pressure of about 140 mmHg in healthy individuals. Giraffes require a systolic pressure of up to 300 mmHg and their cardiac geometry is almost cylindrical [1]. Ischemic incidents or secondary remodelling processes often alter the human heart’s ellipsoid shape. This, in addition to the loss of functional tissue, severely impairs the cardiac pump function. Athanasuleas et al. [2] found that the ellipsoid geometry of the heart was diminished in cases of chronic cardiac insufficiencies. Finally, the ventricle’s geometry is correlated to the severity of clinical manifestations of chronic cardiac insufficiency [3]. Thus, the aim of surgical therapy since the 1980s has been the reconstruction of the physiological geometry of the damaged ventricle [4, 5]. Current surgical techniques are able to restore the physiological ventricle volume, but not the ellipsoid geometry [6]. Therefore, innovative surgical approaches that target both the physiological volume and shape are needed.
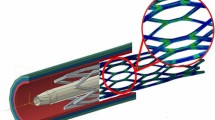
To this end, substitution of lesioned ventricular myocardium with different regenerative biological grafts, such as decellularised urinary bladder [7], skeletal muscle [8], small intestine mucosa [9], bowel [10] and others [11] has been tested in vitro and in vivo. The feasibility of these innovative approaches has been shown for treatment of the right ventricle and the atria, with average blood pressures of about 40–60 mmHg. However, use on a lesioned left ventricle, which can have a blood pressure of up to 240 mmHg, cannot be recommended so far; the mechanical strength of many biological grafts may not be sufficient, especially in the early stage after implantation. Nevertheless, there is evidence of in vivo remodelling processes which increase the strength of the graft [9]. A stabilizing structure based on degradable magnesium alloys can be fixed to the graft to provide support until sufficient mechanical strength has been achieved through the remodelling process [12].
It is hypothesised that non-geometric adaption of the scaffold to the heart leads to high stresses and plastic deformations of the magnesium structures. Preforming of the scaffolds could reduce those stresses and increase scaffold durability. Moreover, preforming of stabilising structures according to the heart’s natural curvature would allow for reconstruction of an optimal ellipsoid cardiac shape.
This hypothesis was investigated via the finite element method (FEM) by comparing the stresses within flat scaffolds and scaffolds preformed according to the geometry of the targeted myocardial area. Afterwards, the number of load cycles before breakage of manufactured flat and preformed structures was compared in a custom testing rig.
This standardised method would allow for rapid and cost efficient development and testing of new structure designs. In addition, the concept of geometric adaption (preforming) is introduced to enhance durability of the magnesium alloy scaffolds. The experiments presented at hand are the first part of developing and testing novel preformed stabilizing structures. The applicability of the resulting structure geometries in vivo and their specific long-term in vivo degradation process will be assessed in subsequent parts of this study.
2 Materials and methods
First of all, the average geometry of the left ventricle was assessed by MRI and a FEM simulation of flat and preformed scaffolds was performed. Then, the scaffolds were manufactured by abrasive waterjet cutting out of extruded sheets of magnesium alloy. Those scaffolds were preformed according to the left ventricular geometry. Finally, mechanical durability and number of load cycles until breakage of the non-preformed and preformed scaffolds were compared in a custom testing rig.
2.1 Measurement of the heart curvature
We obtained retrospective anonymized data of 28 patients (15 men, 13 women, average age of 57.6 ± 15.4 years, average weight of 71.3 ± 17.3 kg, and average height of 1.64 ± 0.16 m) who underwent cardiac magnetic resonance imaging (MRI) for some clinical reasons. Hence, involvement of the ethics committee was not required, since analysis of this data took place in terms of a non-interventional study. The patients were scanned with a standard cardiac MRI by standard midventricular vertical long axis steady-state free precession (SSFP) gradient echo sequence (TrueFISP), and a standard short axis cine SSFP stack. MRI was performed on a 1.5 tesla scanner (MagnetomAvanto, Siemens, Erlangen, Germany). The imaging parameters were: TR 43 ms, TE 1.2 ms, flip angle 56 degree, acquisition matrix 256 × 224, slice thickness 8 mm.
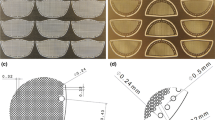
The curvature of the heart near the targeted position of the patch was analysed in end-systolic and end-diastolic images of the vertical long axis and the short axis view. These images were imported into graphic software and analysed by fitting a circle segment to the contours. The radii of the circle segments for both the diastolic and systolic phases were recorded in both views. Afterwards, arithmetic mean values of the radii were calculated in both views.
2.2 FEM-analysis
A stabilising structure was designed according to Bach et al. [12] with a thickness of 1 mm using the CAD software SolidWorks (Dassault Systèmes SolidWorks Corp., MA, USA). Simulations were performed within the commercial finite element package Abaqus (Dassault Systèmes Simulia Corp., RI, USA).
Two different approaches were simulated. Firstly, it was assumed that a flat stabilising structure would be deformed manually by a surgeon into a ‘preformed’ state. Therefore, a simulation of the surgeon’s thumbs was performed by bending the stabilising structure onto a plate using four pressure points. The structure was deformed into the shape of the mean values between the measured systolic and diastolic heart curvature, denoted as ‘preformed’ shape (Fig. 1a, b). Alternatively, it was assumed that a flat stabilising structure would be preformed in a forging die and heat-treated afterwards. This was simulated by bending the stabilising structure into the preformed shape. The resulting mesh was exported as an orphan-mesh. An orphan mesh contains no history variables and is therefore without strain (Fig. 1c, d). Both approaches led to a model shown in Fig. 1e, which depicts the stabilizing structure together with the myocardium and sutures. Sutures were modelled as half cylinders. They were constrained to be equidistant and perpendicular to the myocardium. Deforming the myocardium into diastolic and systolic shapes simulated the heart movement, whereby the stabilising structure was bent.
Material properties of the magnesium alloy LA63 were determined from tensile tests, which produced a Young’s modulus of 46 MPa, Poisson’s ratio of 0.28, and plastic stress–strain values (Table 1). Isotropic hardening was assumed. Myocardium and sutures were simulated with elastic material behaviour. Based on Hoffmeister et al. [13], the Young’s modulus of the myocardium was given to be 66 MPa. For suture material, a Young’s modulus of 1.300 MPa was assumed.
Surface-to-surface contact pairs were defined between the stabilising structure and the myocardium, as well as between the stabilising structure and the sutures (thumbs). Contact was assumed to be frictionless.
Linear hexahedral elements with incompatible mode (C3D8I) were used to generate the meshes. The stabilising structure was meshed with an element size of 0.2 mm and six elements in thickness, resulting in a total of about 130,000 elements. Sutures and thumbs were meshed with 0.2 mm and the myocardium with 1 mm element size, respectively.
2.3 Abrasive water jet cutting of stabilising structures
LA63 alloy is known to provide good elastic properties (Table 1) [14] and was proven to be of good biocompatibility in cardiovascular applications [15]. Since LA63 alloy is commercially not available, the scaffolds were manufactured from extruded sheets of magnesium alloy LA63 (6 vol% Li, 3 vol% Al) with a thickness of 1 mm fabricated in-house [Institut für Werkstoffkunde (Materials Science), Garbsen, Germany]. The scaffolds were shaped by abrasive waterjet cutting using a previously described cutting strategy [14].
In the first step, bores were drilled into the material. Secondly, one half of the structure was cut. Preliminary tests showed bending of the structure in axial direction when cutting the whole structure at once. For this reason, the structure could not be cut at once without damaging the small bars. After step two, a thin steel sheet of 0.2 mm of thickness was placed below the material to reinforce the structure while cutting its second half. In a fourth step, the structure was separated from the material sheet.
A high pressure pump (Manufacturer: Flow, Type 20 XW Waternife) with a maximal operating pressure of 400 MPa and a maximum water flow rate of 7.8 l/m was used for abrasive waterjet cutting of twelve scaffolds. The cutting table consisted of a catcher and a controlled X/Y axis in combination with a manual Z axis. A water orifice diameter of 0.17 mm and a focusing tube diameter of 0.6 mm were used. Garnet Mesh 120 was employed as abrasive particles at a flow rate of 150 g/min.
2.4 Preforming process
Based on the simulation results, a casting die was produced. 6 of 12 structures were preformed in the die and heat treated for 16 h at a temperature of 205 °C in order to remove internal stress caused by the forming process. The remaining six structures were not preformed, but tested in vitro as flat structures.
2.5 In-vitro test of the structures
The in vitro tests were performed in a custom made testing rig (Figs. 2, 3) based on a circular membrane. A second membrane, which the scaffolds were mounted on with surgical sutures, was placed over the circular membrane. The membrane was deflected pneumatically to mimic cardiac like movement dimensions as assessed by MRI data and deflection range was controlled by a laser distance sensor (LDS 60, Micro-Epsilon Eltrotec GmbH, Germany). The membrane of the test bay oscillated at a frequency of 1 Hz (60 oscillations per second) and had a distension corresponding to the curves of the heart in both sections obtained by MRI.
The structures were rinsed by (TRIS-) buffered physiological saline (pH = 7.5) during the whole experiment. This fluid is known to cause accelerated corrosion of the magnesium structures, as compared to in vivo corrosion.
A picture of the corrosion process of the magnesium scaffold was taken every 500 cycles, which equals 500 s (Camera C905, Logitech Europe S.A., Switzerland). This setup allowed for detection of time and location of the material’s failure. The failure was defined as the endpoint of this trial and was identified as complete disjunction of magnesium fragments.
3 Results
3.1 Measurement of the heart curvature
The average radius of the heart’s curvature was measured 49.7 ± 3.03 mm (end diastolic) and 45.8 ± 3.56 mm (end systolic) in the vertical long axis view. In the short axis plane, a curvature of 25.1 ± 1.54 mm (end diastolic) and 21.3 ± 1.69 mm (end systolic) of the heart was measured.
3.2 FEM-analysis
Von Mises stresses of the flat and the preformed stabilising structures can be seen in Fig. 4. The flat stabilising structures were initially stressed due to the manual preforming, while the preformed stabilising structures were without stress. Stresses in the preformed as well as the flat scaffolds were lower during the simulated diastolic stage in comparison to the systolic stage. The stress distributions in the preformed and flat scaffolds appeared similar during the systolic stage, but the stress magnitudes differed significantly between the groups. Maximal stresses within the preformed stabilising structures were about 99 MPa, while the yield point for LA63 is 137 MPa. Therefore, it can be said that the preformed stabilising structures were loaded in the elastic range. In contrast, some areas of the flat stabilising structures were stressed above the yield point, indicating plastic deformations. Further, some areas of the scaffolds, especially at the small radii, were stressed above the ultimate tensile strength of 197 MPa with maximal values of up to 249 MPa. Stresses above the ultimate tensile strength indicate a material overload, which can result in fatigue. These findings are demonstrated in detail by plotting the equivalent plastic strains (PEEQ) (Fig. 5). The maximal value of the scale was set to 2.6 %, since higher strains caused a fracture of the scaffolds in tensile tests. This limit was exceeded in some areas (Fig. 5, grey plots). Critical weakening of the material is suspected in these areas.
3.3 In-vitro test of the structures
The in vitro tests confirmed the results of the FEM-analysis: All flat scaffolds broke earlier than the preformed ones.
Flat structures bore 91,777 ± 22,901 load cycles in average until failure. In contrast, the preformed scaffolds showed an average life-time of 139,974 ± 44,635 cycles, which is a gain of 53 % (Fig. 6).
After breakage, the scaffolds were removed from the testing rig and the break positions were documented. Figure 7 shows the main locations of failure. The break positions of the flat scaffolds are marked 1–6, whereas the break positions of the preformed scaffolds are numbered 7–12. These positions correlate to highly stressed and strained locations as determined in the finite element calculations (Figs. 4, 5).
4 Discussion
Since the 1980s, surgical reconstruction of the left ventricle has been performed according to Dor et al. [4, 5] with various modern modifications [2, 16]. As the left ventricular ejection fraction is dependent on both the ventricle’s volume and on the myocardial shape, surgical therapy has been increasingly focused on physiological reconstruction of both aspects [2]. Therefore, surgeons utilise Dacron patches after resection of the lesioned muscle in most cases. However, Dacron is a synthetic material, which is not actively contractile. Thus, large-scale Dacron substitution of the myocardium results in reduced muscular performance of the heart. Moreover, secondary non-physiological muscle fibre remodelling in neighbouring and, so far, non-lesioned areas of the myocardium may occur, which would further decrease the already low cardiac output. Hence, regenerative biological grafts with remodelling potential promise to be more ideal myocardial prostheses. It has been shown that autologous tissue, utilised in heterotopic position for myocardial repair, has the potential to remodel into actively contracting tissue [7]. Infiltration of cardiomyocytes has even been demonstrated in biological grafts [9]. Several biological graft materials have been tested to serve as cardiac muscle substitutes in animal models and even in clinical applications [11]. However, most biological tissues cannot withstand the high blood pressure of the left ventricle, which severely limits the use of these novel therapeutic approaches. Therefore, stabilisation of the initially fragile biological graft with epicardially applied scaffolds could minimise the risk of aneurysm or even rupture of the biological graft.
Because of the limited stability and stiffness of various polymers, especially of very low thicknesses [17], scaffolds of magnesium alloy (LA63) have been tested in this study. Early breakage of the inflexible flat scaffolds was expected due to plastic deformation, first during the adaption of the scaffold’s shape to the specific curvature of the heart during implantation by the surgeon, and second, because of the ventricle’s strong strain during the heart’s movement. Hence, geometrical adaption of biodegradable magnesium alloy scaffolds to the specific heart’s curvature was introduced in this study.
To determine an average heart’s curvature, MRI scans of 28 patients were evaluated. Based on these data, scaffolds were designed by CAD and used in a stress test simulation by finite element analyses. Modelling of magnesium based cardiovascular implants is, so far, mainly limited to simulate properties and behaviour of coronary stents [18, 19]. In this study, for the first time, simulation of epicardially applied magnesium scaffolds is introduced.
The finite element method is an established engineering tool. It can be used to reduce costly and time-consuming in vitro and in vivo testing. Finite element models can simulate the deformation of the heart’s geometry due to contraction and twisting during systole and diastole [20, 21]. Even muscle fibre orientations for patient-specific heart geometries and blood flow dynamics can be considered with modern algorithms [22, 23]. These complex models are helpful to understand the cardiac biomechanics and even some heart diseases [21], as well as to facilitate development of specific cardiac implants. However, detailed knowledge of loading conditions is required for the development of magnesium scaffolds, and this was gained by the preceding evaluation of MRI scans in this study. Thereby, contraction and relaxation of the heart could successfully be mimicked in our model. Moreover, the geometric adaption of the scaffold to the heart’s specific curvature during systole and diastole could be simulated. Lower Mises stresses were calculated within the preformed structures than in the flat ones. High plastic strains at the small radii of the flat scaffolds were noted, indicating possible material failure.
A major limitation of this methodology is the restricted availability of physiological influence parameters and thus, a constrained validity of the model. However, since the simulation parameters are equal for testing both the preformed and the flat structures, the results at least indicate likely properties, in vitro, and in vivo behaviour.
The results of the simulation were validated by an in vitro test series in this study. 12 magnesium alloy structures were manufactured, six of which were preformed and heat treated. Subsequently, the six flat and the six preformed structures were tested in an in vitro testing rig. The preformed scaffolds, on average, bore 53 % more load cycles before a structural break, as compared to the flat scaffolds. These findings correlate with the FEM-analysis and confirm the validity of the simulation model, although the in vitro test’s own limitations must be taken into account: First, the custom made testing rig simulates the heart’s contraction and dilation, but not it’s twisting motion, which could further increase the applied stress on the scaffold under in vivo conditions. Second, the intraventricular blood pressure could be transduced to the magnesium scaffold via a marginally resistant biological graft in a possible clinical application. This strain by the blood pressure was also not accounted for in the in vitro tests. Third, even if buffered [24], saline solution is known to cause more rapid magnesium alloy corrosion than blood [25]. Witte et al. [26] concluded that results of in vitro corrosion tests of magnesium alloys do not validly predict their in vivo corrosion kinetics. Therefore alone, it is mandatory to test the specific in vivo behaviour of the novel structures prior to clinical application.
Fourth, the alloy composition (6 vol% Li, 3 vol% Al) determines the material properties of the scaffold. Thus, changing the alloy ingredients could cause different reactions to strain and stress in finite element simulations as well as in in vitro tests. Therefore, using different alloys in the future would require replicating the tests.
5 Conclusions
The introduced testing sequence allows for standardised assessment of novel shapes and alloy compositions of scaffolds to temporary stabilise biological myocardial grafts. Moreover, individual geometric adaption of stabilising scaffolds to the specific cardiac curvature of each patient after measurement of the specific geometry via MRI is a highly personalised therapeutic option. An optimal ellipsoid shape of a lesioned myocardium could be surgically restored. Finally, preformed scaffolds evidently provide extended durability and thereby facilitate a broader usage of regenerative biological grafts for surgical left ventricular reconstruction. A large animal trial is currently being prepared to confirm these in vitro results in an in vivo setting and show beneficial effects of the precise adaption of stabilizing scaffolds to the targeted myocardial shape.
References
Adhyapak SM, Parachuri VR. Architecture of the left ventricle: insights for optimal surgical ventricular restoration. Heart Fail Rev. 2010;15(1):73–83.
Athanasuleas CL, Stanley AW, Buckberg GD, Dor V, Di DM, Siler W. Surgical anterior ventricular endocardial restoration (SAVER) for dilated ischemic cardiomyopathy. Semin Thorac Cardiovasc Surg. 2001;13(4):448–58.
Buckberg GD. Form versus disease: optimizing geometry during ventricular restoration. Eur J Cardiothorac Surg. 2006;29(Suppl 1):S238–44.
Dor V, Saab M, Coste P, Kornaszewska M, Montiglio F. Left ventricular aneurysm: a new surgical approach. Thorac Cardiovasc Surg. 1989;37(1):11–9.
Dor V. Surgery for left ventricular aneurysm. Curr Opin Cardiol. 1990;5(6):773–80.
Calafiore AM, Iaco AL, Abukoudair W, Penco M, Di MM. Left ventricular surgical remodeling after the STICH trial. Thorac Cardiovasc Surg. 2011;59(4):195–200.
Badylak SF, Kochupura PV, Cohen IS, Doronin SV, Saltman AE, Gilbert TW, Kelly DJ, Ignotz RA, Gaudette GR. The use of extracellular matrix as an inductive scaffold for the partial replacement of functional myocardium. Cell Transplant. 2006;15:S29–40.
Taheri SA, Ashraf H, Merhige M, Miletich RS, Satchidanand S, Malik C, Naughton J, Zhao Q. Myoangiogenesis after cell patch cardiomyoplasty and omentopexy in a patient with ischemic cardiomyopathy. Tex Hear Inst J. 2005;32(4):598–601.
Tudorache I, Kostin S, Meyer T, Teebken O, Bara C, Hilfiker A, Haverich A, Cebotari S. Viable vascularized autologous patch for transmural myocardial reconstruction. Eur J Cardiothorac Surg. 2009;36(2):306–11.
Ruel MA, Sellke FW, Bianchi C, Khan TA, Faro R, Zhang JP, Cohn WE. Endogenous myocardial angiogenesis and revascularization using a gastric submucosal patch. Ann Thorac Surg. 2003;75(5):1443–9.
Schilling T, Cebotari S, Tudorache I, Haverich A. Tissue engineering of vascularized myocardial prosthetic tissue. Biological and solid matrices. Chirurg. 2011;82(4):319–24.
Bach F, Haverich A, Cebotari S, Biskup C, Schuster B. Supporting element for tissue implants. Patent WO 2011/101142 A1; 2011.
Hoffmeister BK, Handley SM, Wickline SA, Miller JG. Ultrasonic determination of the anisotropy of Young’s modulus of fixed tendon and fixed myocardium. J Acoust Soc Am. 1996;100(6):3933–40.
Biskup C, Hepke M, Grittner N, Plorin T, Hassel T, Bormann D, Bach F-W, Schilling T, Hilfiker A, Cebotari S, Tudorache I, Meyer T, Haverich A AWIJ cutting of structures made of magnesium alloys for the cardiovascular surgery. American WJTA Conference and Expo; 2009.
Schilling T, Brandes G, Tudorache I, Cebotari S, Hilfiker A, Meyer T, Biskup C, Bauer M, Waldmann KH, Bach FW, Haverich A, Hassel T. In vivo degradation of magnesium alloy LA63 scaffolds for temporary stabilization of biological myocardial grafts in a swine model. Biomed Tech (Berl). 2013;58:407–516.
Menicanti L, Castelvecchio S, Ranucci M, Frigiola A, Santambrogio C, de Vincentiis C, Brankovic J, Di DM. Surgical therapy for ischemic heart failure: single-center experience with surgical anterior ventricular restoration. J Thorac Cardiovasc Surg. 2007;134(2):433–41.
Daniels AU, Chang MK, Andriano KP. Mechanical properties of biodegradable polymers and composites proposed for internal fixation of bone. J Appl Biomater. 1990;1(1):57–78.
Wu W, Gastaldi D, Yang K, Tan L, Petrini L, Migliavacca F. Finite element analyses for design evaluation of biodegradable magnesium alloy stents in arterial vessels. Mat Sci Eng B. 2011;176:1733–40.
Grogan J, Leen S, McHugh P. Comparing coronary stent material performance on a common geometric platform through simulated bench testing. J Mech Behav Biomed Mater. 2012;12:129–38.
Feng B, Veress A, Sitek A, Gullberg G, Roy D. Estimation of mechanical properties from gated SPECT and cine MRI data using a finite-element mechanical model of the left ventricle. IEEE Trans Nucl Sci. 2001;48:725–33.
Feng L, Weixue L, Ling X, Guohua W. The construction of three-dimensional composite finite element mechanical model of human left ventricle. JSME Int J Ser C. 2001;44:125–33.
Watanabe H, Sugiura S, Kafuku H, Hisada T. Multiphysics simulation of left ventricular filling dynamics using fluid-structure interaction finite element method. Biophys J. 2004;87:2074–85.
Wong J, Kuhl E. Generating fibre orientation maps in human heart models using Poisson interpolation. Comput Methods Biomech Biomed Eng 2012;1–10.
Kirkland NT, Waterman J, Birbilis N, Dias G, Woodfield TB, Hartshorn RM, Staiger MP. Buffer-regulated biocorrosion of pure magnesium. J Mater Sci Mater Med. 2012;23(2):283–91.
Kirkland NT, Birbilis N, Staiger MP. Assessing the corrosion of biodegradable magnesium implants: a critical review of current methodologies and their limitations. Acta Biomater. 2012;8(3):925–36.
Witte F, Fischer J, Nellesen J, Crostack HA, Kaese V, Pisch A, Beckmann F, Windhagen H. In vitro and in vivo corrosion measurements of magnesium alloys. Biomaterials. 2006;27(7):1013–8.
Acknowledgments
The study was conducted within the framework of the collaborative research centre 599 financed by the German Research Foundation (DFG). The authors are very grateful to the DFG for financial support.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Bauer and T. Schilling have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Bauer, M., Schilling, T., Weidling, M. et al. Geometric adaption of biodegradable magnesium alloy scaffolds to stabilise biological myocardial grafts. Part I. J Mater Sci: Mater Med 25, 909–916 (2014). https://doi.org/10.1007/s10856-013-5100-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-013-5100-5