Abstract
The onset of infections associated to bacterial proliferation and biofilm formation on indwelling medical devices represents the major risk of morbidity and mortality among patients. In order to contain the risk of infections in clinical practice, there is a growing interest nowadays in silver-based products due to the strong antimicrobial efficacy of silver against a broad spectrum of microorganisms. In this work, temporary catheters for haemodialysis were coated with silver nano-particles through the in situ photo-reduction of a silver salt in alcoholic solution. A homogeneous distribution of silver particles firmly bonded to the substrate was obtained through the adopted technique. An optimisation study was required to define the amount of silver, in order to obtain good efficacy against Gram-positive and Gram-negative bacteria and no cytotoxic effect. At this purpose, three concentrations of silver, 0.1, 0.25 and 0.5 wt%, have been deposited and tested with respect to bacterial reduction percentage and cellular response. Particularly, bacterial enumeration on Escherichia coli and Staphylococcus aureus, and BrdU incorporation, TUNEL assay and Actin staining on a selected primary cell population were performed on catheters treated with the different silver solutions. The silver percentages tested demonstrated strong antibacterial properties together with a good cellular response, thus indicating that the developed product could be proposed in clinical practice and that the lower percentage tested can be preferred with evident advantages in terms of costs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Vascular access catheters represent the major source of infectious complications in haemodialysis therapy. The incidence of infections due to Methicillin-resistant Staphylococcus aureus colonization in haemodialysis patients contributes to morbidity, mortality and healthcare costs [1].
Biofilm formation poses a serious problem for public health because of the increased resistance of biofilm-associated organisms to antimicrobial agents and the potential of these organisms to cause infections in patients with indwelling medical devices [2].
When an intravascular catheter becomes infected, frequently the only solution is its removal, thus causing additional health costs [3].
The colonization of the catheter occurs mainly through the extraluminal and the intraluminal routes. The colonization of short-term central vascular accesses occurs predominantly from the skin puncture site; the colonization of long-term central vascular accesses is usually related to intraluminal bacterial spread from a contaminated hub [4]. When bacteria make contact with the biomaterial, they begin the production of a sticky adhesion that attaches it to the surface [5]. After the attachment on the surface of the catheter, the microorganisms grow and later produce polymers, mostly polysaccharides, to form the matrix of the biofilm [6]. The bacterial colonization also increases by rising the endovascular indwelling time. Antimicrobial-coated catheter materials such as catheters impregnated with rifampin compounds, chlorhexidine and silver sulfadiazine, have been extensively investigated [7]. Both the chlorhexidine/silver sulfadiazine—and the minocycline/rifampin—impregnated catheters are approved by the Food and Drug Administration and are currently available for use in the United States [8].
The development of surfaces and coatings that can eradicate microorganisms in an active way is important to maintain an aseptic environment. A large number of methods have been developed in recent years. Current preventive measures to decrease the risk of serious infections include antimicrobial lock therapy [3]. New materials and processes that prevent biofilm formation and bacterial growth were tested. Recently, new materials that decrease the risk of skin-to-vein bacterial migration, such as new antiseptic dressings, were extensively tested. Antimicrobial-coated catheters can prevent catheter-related bloodstream infections but have a theoretical risk of selecting resistant bacteria. An antimicrobial or antiseptic lock may prevent bacterial migration from the hub to the bloodstream [9]. The use of polyurethane catheters with an antimicrobial system based on silver ions was assessed as a source against catheter-related infection and bacteremia. The risk of developing bacterial resistance was demonstrated much lower for silver than for antibiotics and the protection from microorganisms during the entire catheterization period was also assessed [10].
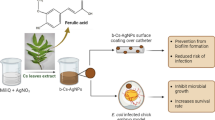
Many silver deposition technologies and surface functionalization with silver nanoparticles have been proposed as an alternative to common strategy to prevent bacterial colonization [11]. Silver coated catheters for haemodialysis were developed according to a technology based on the photochemical deposition of silver nanoparticles [12] in both the luminal and outer side of the device [13, 14]. The impressive efficacy in preventing the biofilm formation on the surface of the catheter for the whole working life of the device has been demonstrated on S. aureus in simulated working conditions [14]. Moreover, the technology was demonstrated to provide a strong adhesion and a homogeneous distribution of the silver particles to the polymeric surface in contact with biological fluids under flow conditions [14]. Aim of this work is the evaluation of the influence of the silver percentage deposited on the device in terms of both antibacterial capability and cytotoxicity. At this purpose, three concentrations of silver have been tested with respect to antibacterial tests on S. aureus and Escherichia coli and to the proliferation, apoptosis and morphology of a selected primary cell population.
2 Materials and methods
2.1 Silver deposition on polyurethane catheters
Polyurethane “Carbothane” catheters for haemodialysis were treated with silver particles according to a silver deposition technology extensively studied in previous works on different types of substrates [13–17]. The technology is based on the photo-reduction of a silver salt and provides the synthesis in situ of silver particles. Firstly, a silver solution containing silver nitrate dissolved in methanol or in a mixture methanol/water is prepared; secondly, the silver solution is used to treat the substrate through dip coating or spray coating; finally, the wet substrate is exposed to an ultraviolet source in order to induce the photo-reduction of the silver salt and the formation of silver particles. The photo-reduction is strictly related to the presence of methanol that is used as both solvent and reducing agent. The amount of silver is related to the expected antibacterial properties in function of the specific application. In this work a low, medium, and high percentages of silver have been tested for the treatment of catheters, respectively 0.1, 0.25, and 0.5 wt%. Catheters were silver-treated on the luminal and outer side by dip coating into the silver solutions and by exposing them to a UV lamp (λ = 365 nm; 50 W) for 30 min. The luminal side was treated adopting a syringe to force and expel the solution in and out of the device.
2.2 Preparation of samples
Two sets of samples for antibacterial tests on S. aureus and E. coli respectively were obtained by cutting each type of coated catheters (length 1 cm, average weight 90 mg) by means of a sharp scalpel. Samples for the cytotoxicity tests were obtained applying the deposition technology to flat pieces of catheters in order to promote their adhesion to the tissue culture plates. Such pieces were cut from the internal surface separating the lumina adopting a razor blade. Then, they were treated with the same silver solutions adopted for the other samples and UV sterilized for 1 h.
2.3 Microbiological analysis
After UV sterilization for 1 h, two sets of samples were incubated respectively in 4 ml of nutrient broth inoculated with a suspension of S. aureus (NCTC 10338, inoculating cell density 8.4 × 106 CFU/ml) and in 4 ml of Luria Broth inoculated with a suspension of E. coli (DH5(α), inoculating cell density 5.3 × 106 CFU/ml) at 37 °C overnight. After incubation, samples were removed from the broth and serial dilutions were performed in sterile saline. From each dilution 100 μl were extracted and plated on nutrient agar plates for S. aureus and on LB plates for E.coli. The inoculated plates were incubated at 37 °C overnight and then bacterial colonies were counted adopting a colony counter. Samples were tested in triplicate. The number of colonies grown on each plate was recorded and the average of bacterial number was calculated for each sample and compared with the untreated sample. The percentage of bacterial reduction was hence calculated.
2.4 Cell culture
Fibroblasts were isolated from swine Achilles tendons. Briefly, tendons were aseptically harvested from young pigs (10 kg) and washed in sterile phosphate buffered saline (PBS) (Celbio, Italy), supplemented with 50 μg/ml of gentamicin (Lonza, Italy), 0.5 μg/ml of amphotericin B (Lonza, Italy), 100 U/ml of Penicillin/Streptomycin solution (Lonza, Italy); after three washes, samples were finely minced and digested in DMEM High Glucose medium (Celbio, Italy) containing 0.1 % collagenase Type I (DBA-Italia Srl, Italy), 10 % fetal bovine serum (Celbio, Italy), 2 mM ultra-glutamine, 100 U/ml of Penicillin/Streptomycin solution, 50 μg/ml of gentamicin and 0.5 μg/ml of amphotericin B. The specimens were incubated overnight in an oscillating water bath at 37 °C. Undigested tissue and debris were removed by filtering the cell suspension using a 100 micron sterile strainer (BD Falcon, USA). The cell suspension obtained was centrifuged at 1,400 rpm for 10 min. The cell pellet was washed twice in PBS. Cells were seeded and cultured in DMEM High Glucose medium (Celbio, Italy) containing 20 % fetal bovine serum, 2 mM ultra-glutamine, 100 U/ml of Penicillin/Streptomycin solution, 50 μg/ml of gentamicin, 0.5 μg/ml of amphotericin B, 1 mM sodium pyruvate (GIBCO, Italy) and 10 mM HEPES (GIBCO, Italy). Cells were expanded and, at P2, seeded on 6-well plates at a density of 30,000 cells/cm2 for the BrdU and TUNEL assays. Before cell seeding, silver containing catheters (0, 0.1, 0.25 and 0.5 wt%) were stuck on the bottom of the wells by using a small drop of 1 % agarose.
2.5 BrdU incorporation
After 24 h of culture, fibroblasts were treated with 10 μg/ml of BrdU overnight. Catheters were then removed and fibroblasts were washed three times with PBS and fixed with pre-cooled methanol at −20 °C for 10 min. After three washes in PBS, cells were washed twice with PBS containing 1 % BSA (bovine serum albumin) (Sigma, Italy) and 0.2 % triton (Sigma, Italy); they were then treated with 2 M HCl for 45 min, followed by the treatment with 0.1 M Na2B4O7 for 10 min. Cells were washed twice with PBS and left in blocking solution for 30 min (PBS containing 10 % goat serum). Fibroblasts were then incubated with the anti-BrdU antibody (1:200) (BD, Italy) for 2 h, washed three times with PBS and finally incubated for 1 h with an anti-mouse IgG (H + L) antibody conjugated to fluorescein (Molecular Probes). Finally, nuclei were counterstained with 10 g/ml of Hoechst bisbenzimide (Sigma, Italy). The immunofluorescent stainings were observed using an Olympus BX51 light microscope equipped with an Amplified Fluorescence by Transmitted Excitation of Radiation (AFTER) Light Emitting Diodes (LED) Fluorescence Microscope kit (Lab Vision), thus providing an easy adaptation of a light microscope to a fluorescence one as described by Deponti et al. [18]. In order to calculate the proliferation index, ten fields were considered for the analysis of each experimental sample, focusing on the cells just around the catheter; for each field, the number of total and BrdU-positive nuclei was registered in order to determine the percentage of BrdU-positive nuclei.
2.6 TUNEL assay
The TUNEL assay was performed with the ApopTag Fluorescein In Situ Apoptosis Detection Kit (Millipore, Italy), according to the manufacturer’s protocol. After 24 h of culture with the different silver coated catheters, fibroblasts were fixed in 1 % paraformaldehyde pH 7.4 for 10 min and washed twice with PBS; then, they were post-fixed with pre-cooled ethanol:acetic acid (2:1) for 5 min at −20 °C. After three washes with PBS, cells were incubated with the equilibration buffer for 5 min and then with the TdT enzyme solution for 1 h at 37 °C. Fibroblasts were then treated with the stop/wash buffer for 10 min and washed three times with PBS; finally, cells were incubated with anti-digoxigenin conjugated for 30 min at room temperature. Nuclei were counterstained with 10 g/ml of Hoechst bisbenzimide. The immunofluorescent stainings were observed as described above. In order to calculate the apoptotic index, ten fields were considered for the analysis of each experimental sample, focusing on the cells just around the catheter; for each field, the number of total and apoptotic nuclei was registered in order to determine the percentage of apoptotic nuclei.
2.7 ACTIN staining
In order to evaluate fibroblasts morphology in response to the different silver coated catheters, after 24 h of culture they were fixed in pre-cooled methanol for 10 min at −20 °C and then washed three times with PBS. Cells were then incubated first with a blocking solution (PBS with 10 % goat serum) for 30 min and then with the anti-actin antibody (1:200) (SIGMA, Italy) for 2 h. After three washes, cells were incubated with an anti-rabbit antibody conjugated with rhodamine (Molecular Probes) for 1 h. The obtained staining was observed at the microscope as described above.
3 Results
3.1 Silver deposition on polyurethane catheters
The catheters treated with silver by adopting the described technology are characterized by an evident change in colour from white to brown. In Fig. 1, images of the samples produced for the cellular study with different amounts of silver are reported. The effect of darkening increased by increasing the percentage of silver adopted for the preparation of the silver solutions. However, in any case a homogeneous coating was obtained and no zone of discoloration could be observed. Samples were washed with deionized water before characterization. No detachment of coating was observed in any sample even after several washings. The morphology of the silver coating obtained by the adopted technology, together with dimensions and distribution of the silver particles on the surface of catheters have been extensively analysed and described in a previous work [13] where SEM and TEM analyses are reported. The analyses demonstrated a homogeneous distribution of the silver particles across the surface, as well as the durability of the treatment due to the strong adhesion of the particles to the substrate [13, 14].
Pictures of catheters treated with different silver solutions: a untreated; b 0.1 wt% Ag; c 0.25 wt% Ag; d 0.5 wt% Ag. The effect of darkening induced on the surface of the catheter by the presence of the silver coating rises by increasing the percentage of silver used for the preparation of the silver solution
3.2 Microbiological analysis
The results of the microbiological analysis on S. aureus and E. coli are collected in the graph in Fig. 2. The average percentages of the bacterial reduction induced by samples treated with different amounts of silver are reported. The samples exhibited different antibacterial capabilities, according to the concentrations of silver adopted for the treatment (Fig. 2). As expected, no bacterial reduction was associated to the untreated sample, while 72 and 75 % of bacteria reduction were demonstrated by the sample treated with 0.5 wt% Ag on S. aureus and E. coli, respectively. 60 and 58 %, 66 and 64 % were the percentages of bacterial reductions obtained on each bacterial strain, respectively, for the sample treated with 0.1 wt% Ag and 0.25 wt% Ag.
3.3 Proliferation
Fibroblasts proliferation was evaluated by BrdU incorporation. Cells were grown for 24 h in presence of different silver coated catheters (0, 0.1, 0.25, and 0.5 wt%) and then BrdU was added to the culture medium in order to evaluate the percentage of proliferating cells in response to the different silver concentrations. Proliferation resulted to be significantly reduced only in the samples treated with 0.5 % silver; no differences were observed in the other experimental samples (Fig. 3).
BrdU incorporation: a–d Fibroblasts nuclei were stained for BrdU incorporation (green) and then counterstained with Hoechst (blue). Representative images are shown for each experimental conditions: 0 % wt silver (a), 0.1 % wt silver (b), 0.25 % wt silver (c), 0.5 % wt silver (d). e The graph shows the percentage of BrdU positive nuclei in response to the different silver coated catheters (Color figure online)
3.4 Apoptosis
Fibroblasts apoptosis was evaluated by TUNEL assay after 24 h of culture. None of the different silver coated catheters showed significant increase of the apoptotic index of the cell population (Fig. 4).
TUNEL assay: a–d Fibroblasts apoptotic nuclei were stained according to the TUNEL assay protocol (green) and then counterstained with Hoechst (blue). Representative images are shown for each experimental conditions: 0 % wt silver (a), 0.1 % wt silver (b), 0.25 % wt silver (c), 0.5 % wt silver (d). Arrows indicate the few apoptotic nuclei for each field (green). e The graph shows the percentage of TUNEL positive nuclei in response to the different silver coated catheters (Color figure online)
3.5 Cell morphology
Fibroblasts morphology was evaluated by actin staining after 24 h of culture. Fibroblasts showed no cell shrinkage or cell shape abnormalities when cultured in presence of 0, 0.1 and 0.25 wt% silver coated catheters, indicating a maintenance of the normal cytoskeletal architecture (Fig. 5). On the other hand, the highest silver concentration (0.5 wt%) induced a slight contraction of the cytoskeleton, demonstrating a preliminary cell response to a toxic condition.
Fibroblasts morphology. a–d Fibroblasts were stained with anti-actin antibody in order to determine the effect of silver coated catheters on the cell shape. Representative images are shown for each experimental conditions: 0 % wt silver (a), 0.1 % wt silver (b), 0.25 % wt silver (c), 0.5 % wt silver (d)
4 Discussion
Vascular access catheters represent the major source of infectious complications in haemodialysis therapy [1, 19]. S. aureus was recognized as the most common pathogen in haemodialysis patients [20]. Current preventive measures to decrease the risk of serious infections include antimicrobial lock therapy and antimicrobial agent impregnated catheters [21].
Anti-infective lock solutions were demonstrated efficient in killing organisms embedded in the biofilm and in preventing intraluminal contamination in catheters that are not used continuously, such as haemodialysis catheters [22]. The use of 40 % ethanol as catheter lock solution for a short period rather than using high concentrations of antibiotics for extended periods has been proposed to eradicate biofilms and to prevent catheter related bloodstream infections. Gentamicin, ciprofloxacin and vancomycin were found to be unable to eradicate the biofilms even after 24 h [23]. An antimicrobial study of a multicomponent lock solution confirms its properties in the elimination of both planktonic and sessile microorganisms [24]. A correlation between S. aureus biofilm formation and sodium heparin, which is the most widely used catheter lock solution, was demonstrated [25]. Heparin alternatives, sodium citrate and sodium EDTA, can prevent the formation of S. aureus biofilms and, hence, the risk of biofilm-associated complications in indwelling catheters [26]. Catheters impregnated with chlorhexidine-silver sulfadiazine and catheters impregnated with minocycline and rifampin are commercially available [27].
The deposition of thin films, the ionically bonding and the entrapment of anti-infective agents into the polymer matrix are currently the most described technologies [28]. Compared to different techniques such as the ion beam assisted deposition (IBAD) process, the technology adopted in this work is extremely innovative in the field of the biomedical devices as it provides the superficial deposition of silver nanoparticles on both the luminal and the outer surface of the catheter, with great advantages in terms of prevention of the infections. In the IBAD process, the silver coating can be deposited only on the outside surface of the catheter because catheters are placed on mandrels and rotated along their longitudinal axis as the silver vapour and ions are incident perpendicularly to the axis of rotation. Manipulations of the catheter are also required to obtain a uniform coating deposited around its diameter [29].
The presented technology ensured the deposition of the silver coating on both the side of the device at the same time without any manipulation. Moreover, no expensive equipment was required for the process, thus reducing significantly the costs of production. A homogeneous coating was provided across the surface of the catheter with dimensions of the particles ranging between 20 and 100 nm where aggregated, as demonstrated through SEM analyses reported in a previous work [13]. Moreover, the excellent adhesion of the silver particles was demonstrated after 30 days even in flow conditions thorough SEM analysis and biological tests. The impressive efficacy in preventing bacterial adhesion and biofilm formation was assessed for the whole working life of the device [13, 14]. The release of silver ions from the silver coating was studied in simulated corporeal conditions in contact with biologic fluids and the results were largely below the limit of toxicity reported in literature, thus suggesting that no relevant implication in human health can be associated to the release of silver ions [14]. The results obtained from the previous works indicated that the developed product could be considered an interesting alternative to the antimicrobial device currently available on the market. The aim of this work was the evaluation of the influence of the silver amount on the biological properties of the final product in terms of antibacterial capability and cytotoxicity, in order to optimize the cost-effectiveness of the final product. At this purpose, three percentages of silver were tested on Gram positive and Gram negative bacteria and on a selected cellular line. As expected, the samples treated with the highest percentage of silver (0.5 wt%) provided the best result in terms of antibacterial capability by inducing 72 and 75 % of bacterial reduction on S. aureus and E. coli respectively, but also the other percentages provided good antimicrobial properties, thus suggesting that the lower amounts of silver can be preferred with evident advantages of production costs. Moreover, cell survival was not affected by any of the percentages of silver tested even if, at the highest percentage, cells showed reduced proliferation and a slight contraction of the cytoskeleton that may be interpreted as an initial step of the apoptotic cascade.
The difference in the percentage of the bacterial reduction between the samples treated with 0.1 and 0.25 wt% Ag could be considered not significant, indicating that 0.1 wt% Ag can be proposed as the optimised percentage for the treatment of catheters with the best cost-effectiveness ratio.
5 Conclusions
In this work an innovative technology to obtain antibacterial silver-coated catheters for haemodialysis was presented and discussed. The technology was based on the photochemical deposition of silver nanoparticles through the dipping of catheters into an alcoholic silver solution and the following exposure of the wet devices to a UV source. The process resulted in a homogeneous coating characterized by an excellent adhesion to the substrate. If compared with other widespread approaches based on silver treatments, the presented technology is extremely innovative and effective because it provided the treatments on both the luminal and external surface of the catheter without any manipulation of the device and any expensive equipment. Moreover, the efficacy of the obtained silver coating in inhibiting bacterial adhesion and biofilm formation was demonstrated even in flow conditions for the whole working life of the catheters. However, an optimisation study was required to determine the percentage of silver to be adopted for the treatment, in order to obtain good antibacterial capability without inducing cytotoxic effects. At this purpose, three percentages of silver, 0.1, 0.25 and 0.5 wt%, were deposited on catheters and tested on bacteria and fibroblasts respectively. The lower and medium percentages tested, 0.1 and 0.25 respectively, provided excellent results because they demonstrated at the same time good antibacterial capabilities on Gram positive and Gram negative bacteria and good cellular response in terms of viability, proliferation and morphology of fibroblasts. Also the highest percentage, i.e. 0.5 wt%, demonstrated good efficacy in reducing bacterial proliferation, but it slightly affected cellular proliferation and morphology. However, the similarity in the antibacterial properties exhibited by the different materials suggested that catheters treated with 0.1 wt% of silver can be proposed as the best compromise in terms of cost-effectiveness ratio. The ease of preparation of the silver treated devices, together with their long-term antibacterial effectiveness and the low costs of production, can be considered an interesting alternative to the common strategies adopted in the clinical practice to contain the risk of infections.
References
Parker MG, Doebbeling BN. The challenge of methicillin-resistant Staphylococcus aureus prevention in hemodialysis therapy. Semin Dial. 2012;25:42–9.
Donlan RM. Biofilm formation: a clinically relevant microbiological process. Clin Infect Dis. 2001;33:1387–92.
Sousa C, Henriques M, Oliveira R. Mini-review: antimicrobial central venous catheters—recent advances and strategies. Biofouling. 2011;27:609–20.
Mermel LA. What is the predominant source of intravascular catheter infections? Clin Infect Dis. 2011;52:211–2.
Beathard GA, Urbanes A. Infection associated with tunneled hemodialysis catheters. Semin Dial. 2008;21:528–38.
Maya ID. Antibiotic lock for treatment of tunneled hemodialysis catheter bacteremia. Semin Dial. 2008;21:539–41.
Dwyer A. Surface-treated catheters—a review. Semin Dial. 2008;21:542–6.
Trautner BW, Darouiche RO. Catheter-associated infections pathogenesis affects prevention. Arch Intern Med. 2004;164:842–50.
Timsit JF, et al. New materials and devices for preventing catheter-related infections. Ann Intensive Care. 2011;1:34.
Loertzer H, Soukup J, Hamza A, Wicht A, Rettkowski O, Koch E, Fornara P. Use of catheters with the AgION antimicrobial system in kidney transplant recipients to reduce infection risk. Transplant Proc. 2006;38:707–10.
Roe D, Karandikar B, Bonn-Savage N, Gibbins B, Roullet JB. Antimicrobial surface functionalization of plastic catheters by silver nanoparticles. J Antimicrob Chemother. 2008;61:869–76.
Pollini M, Sannino A, Maffezzoli A, Licciulli A. Antibacterial surface treatments based on silver clusters deposition. European Patent No. EP1986499, 2008.
Pollini M, Paladini F, Catalano M, Taurino A, Licciulli A, Maffezzoli A, Sannino A. Antibacterial coatings on haemodialysis catheters by photochemical deposition of silver nanoparticles. Mater Sci Mater Med. 2011;22:2005–12.
Paladini F, Pollini M, Talà A, Alifano P, Sannino A. Efficacy of silver treated catheters for haemodialysis in preventing bacterial adhesion. J Mater Sci Mater Med. 2012;23:1983–90.
Pollini M, Paladini F, Licciulli A, Maffezzoli A, Sannino A. Engineering nanostructured silver coatings for antimicrobial applications. In: Cioffi N, Rai M, editors. Nanoantimicrobials progress and prospects. New York: Springer; 2012. p. 313–336.
Pollini M, Paladini F, Licciulli A, Maffezzoli A, Nicolais L, Sannino A. Silver coated wool yarns with durable antibacterial properties. J Appl Polym Sci. 2012;125:2239–44.
Pollini M, Russo M, Licciulli A, Sannino A, Maffezzoli A. Characterization of antibacterial silver coated yarns. Mater Sci Mater Med. 2009;20:2361–6.
Deponti D, Di Giancamillo A, Mangiavini L, Pozzi A, Fraschini G, Sosio C, Domeneghini C, Peretti GM. Fibrin-based model for cartilage regeneration: tissue maturation from in vitro to in vivo. Tissue Eng Part A. 2012;18(11–12):1109–22.
Adal KA, Farr BM. Central venous catheter-related infections: a review. Nutrition. 1996;12:208–13.
Wang IK, et al. Bacteremia in hemodialysis and peritoneal dialysis patients. Intern Med. 2012;51:1015–21.
Shah CB, Mittelman MW, Costerton JW, Parenteau S, Pelak M, Arsenault R, Mermel LA. Antimicrobial activity of a novel catheter lock solution. Antimicrob Agents Chemother. 2002;46:1674–9.
Timsit JF. Diagnosis and prevention of catheter-related infections. Curr Opin Crit Care. 2007;13:563–71.
Chaudhury A, Rangineni J. Catheter lock technique: in vitro efficacy of ethanol for eradication of methicillin-resistant staphylococcal biofilm compared with other agents. FEMS Immunol Med Microbiol. 2012;65:305–8.
Steczko J, Ash SR, Nivens DE, Brewer L, Winger RK. Microbial inactivation properties of a new antimicrobial/antithrombotic catheter lock solution (citrate/methylene blue/parabens). Nephrol Dial Transpl. 2009;24:1937–45.
Shanks RM, et al. Heparin stimulates Staphylococcus aureus biofilm formation. Infect Immun. 2005;73:4596–606.
Shanks RM, Sargent JL, Martinez RM, Graber ML, O’Toole GA. Catheter lock solutions influence staphylococcal biofilm formation on abiotic surfaces. Nephrol Dial Transpl. 2006;21:2247–55.
Mermel LA. New technologies to prevent intravascular catheter-related bloodstream infections. Emerg Infect Dis. 2001;7:197–9.
Shintani H. Modification of medical device surface to attain anti-infection. Trends Biomater Artif Organs. 2004;18:1–8.
Tobin EJ, Bambauer R. Silver coating of dialysis catheters to reduce bacterial colonization and infection. Ther Apher Dial. 2003;7:504–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Paladini, F., Pollini, M., Deponti, D. et al. Effect of silver nanocoatings on catheters for haemodialysis in terms of cell viability, proliferation, morphology and antibacterial activity. J Mater Sci: Mater Med 24, 1105–1112 (2013). https://doi.org/10.1007/s10856-013-4870-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-013-4870-0