Abstract
Three dimensional tissue engineered scaffolds for the treatment of critical defect have been usually fabricated by salt leaching or gas forming technique. However, it is not easy for cells to penetrate the scaffolds due to the poor interconnectivity of pores. To overcome these current limitations we utilized a rapid prototyping (RP) technique for fabricating tissue engineered scaffolds to treat critical defects. The RP technique resulted in the uniform distribution and systematic connection of pores, which enabled cells to penetrate the scaffold. Two kinds of materials were used. They were poly(ε-caprolactone) (PCL) and poly(d, l-lactic-glycolic acid) (PLGA), where PCL is known to have longer degradation time than PLGA. In vitro tests supported the biocompatibility of the scaffolds. A 12-week animal study involving various examinations of rabbit tibias such as micro-CT and staining showed that both PCL and PLGA resulted in successful bone regeneration. As expected, PLGA degraded faster than PCL, and consequently the tissues generated in the PLGA group were less dense than those in the PCL group. We concluded that slower degradation is preferable in bone tissue engineering, especially when treating critical defects, as mechanical support is needed until full regeneration has occurred.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Tissue engineering can provide a way to regenerate damaged tissue [1]. A successful outcome requires the interactions of three major elements: a scaffold, cells, and the environment. It may be necessary to culture cells or stems cells on the scaffold before it is transplanted into the desired position for in vitro tests [2, 3]. However, as culturing cells before transplantation can have unexpected risks, the procedures should be minimal for clinical application. Therefore, insertion of the scaffolds without cells expecting recruitment of cells from neighborhood can be more close to clinical application. Biodegradation of the scaffold in vivo must also be considered [4, 5]. A polymer-based biocompatible material that eventually degrades when new tissue is generated is optimal [6]. Treatment of critical defects requires the regeneration of a three-dimensional (3D) structure. This study examined the use of a 3D scaffold as a bone substitute for treating critical defects without prior in vitro cell culture and tested the degradability of two polymers.
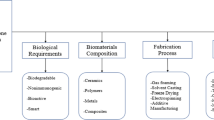
Several techniques for manufacturing polymer-based scaffolds have been introduced [7]. Preferably, a 3D scaffold should provide internal spaces for cells growth in order to generate a matrix. Popular techniques for accomplishing this include salt leaching [8] and gas foaming [9, 10]. These techniques can utilize most polymer types and make it relatively easy to control pore size and porosity. In addition, using various polymerization methods, the strength of the scaffold can be controlled within a certain range. However, poor pore inter-connectivity can prevent cells from penetrating the innermost part of the scaffold, even though the cells adapt on the surface [11, 12].
To overcome these limitations, the rapid prototype (RP) manufacturing technique was recently introduced for fabricating 3D scaffolds. Utilizing computer-aided design (CAD) software the RP technique was invented at MIT in 1993 (US Patent 5,204,055) as bioplotter or Fused Deposition Modeling (FDM). Based on this technique fully interconnected scaffolds with various bio-polymer have been able to be fabricated by feeding 3-dimensional data to the CAM (Computer-Aided-Manufacturing) system and tested. The pore size and overall shape can be controlled, and pore inter-connectivity can be enhanced. The strength of a scaffold can also be controlled within a certain range, depending on how the strands are fabricated. Specifically PCL has been widely used in fabricating 3D scaffolds with or without various nanoparticles [12–15].
The biodegradability of scaffold material must meet the demands at the site of the critical defect, and the speed of degradation should match the speed of regeneration. The most popular polymers used in tissue engineering are polylactic acid (PLA), polyglycolic acid (PGA), and poly (ε-caprolactone) (PCL). A combination of PLA and PGA (PLGA) is used widely because of its proven biocompatibility and biodegradability, and the degradation rate can be adjusted by varying the amount of each monomer type [6]. PCL degrades relatively slowly owing to its hydrophobic nature, but it displays relatively higher ductility [16, 17].
Recently PLGA made by RP technique for bone tissue regeneration was reported [18]. However, they made 3D scaffolds in different structural morphology then used the scaffolds in animal study. No animal study which adopted PCL and PLGA to compare their outcomes has been reported.
Therefore, the evaluation of RP technique based scaffolds made of different material types through in vitro and animal study for bone tissue engineering is worth to be studied. For this the present work examined 3D scaffolds made of two different materials, PLGA and PCL. The RP technique was used to control pore size and inter-connectivity in order enhance osteoconduction into the depths of the scaffold. The scaffolds were evaluated in vitro and in a 12-week animal study.
2 Materials and methods
2.1 Preparation and in vitro testing of scaffolds
2.1.1 PCL and PLGA scaffold preparation
Biodegradable PCL (molecular weight, 43,000–50,000; Polysciences, Warrington, PA, USA) and PLGA (PLGA 50:50 molecular weight, 83,000; Lakeshore, Birmingham, AL, USA) were used. A 3D RP system (M4T, Korea) was used to fabricate the scaffold designed using a CAD system (Fig. 1a). The polymer beads inside the heating cylinder (dotted circle in Fig. 1a) were heated electrically to 110 °C, and the hot polymer solution was extruded through a 350 μm-diameter nozzle under a pressure of 670 kPa. The fabrication was performed at room temperature while the cylinder temperature was kept 110 °C. The detailed morphology of each scaffold was observed using field emission scanning electron microscopy (FE-SEM; Hitachi, Tokyo, Japan) (Fig. 1b, c).
2.1.2 Mechanical testing of scaffolds
The mechanical strength of PLGA and PCL scaffolds measuring 10 × 10 × 5 mm3, which is larger than the scaffolds used in the animal study, was measured with a compression test (RB Model 302 ML; R&B, Daejeon, Korea). Using customized jigs, five specimens of each scaffold type were tested at a displacement rate of 0.5 mm/min. The average and standard deviation of were calculated for statistical analysis.
2.1.3 Toxicity testing of scaffolds
Toxicity tests were performed following the ISO 10993-5 guidelines. Five grams of each material (PLGA and PCL) were treated with ultraviolet (UV) light and immersed in 50 ml of RPMI 1640 (25 mM HEPES, 25 mM NaHCO3, 300 mg/L l-glutamine) with 10 % fetal bovine serum (FBS) at 37 °C. L-929 cells were seeded onto 24-well plates at 2.4 × 104 cells/300 μL with elution medium. For the control, L-929 cells were cultured in pure RPMI 1,640 at the same cell density. After 48 h of culturing, the cells were washed three times with Dulbecco’s phosphate-buffered saline (DPBS), and live/dead cell staining (Live/Dead® Viability/Cytotoxicity Kit; Molecular Probes, Eugene, OR, USA) and the MTT assay were performed. For live/dead cell staining, 100 μL of reagent were added, and images were acquired using a laser confocal microscope (LSM 510 META, Zeiss, Oberkochen, Germany) at 494/517 nm excitation and 528/617 nm emission to measure calcein/EthD-1, respectively. For the MTT assay, the cells were incubated with MTT reagent for 4 h at 37 °C, and the absorbance at 595 nm was measured.
2.2 Animal study
2.2.1 Scaffold implantation
The animal study was carried out with approval from the Institutional Animal Care and Use Committee of Chonnam University, Korea. Six New Zealand white rabbits (~1.2 kg) were assigned to each of two groups for implantation of PCL or PLGA scaffolds. The rabbits were anesthetized with an abdominal injection of ketamine and xylazine, a 1.5 cm defect was made in the right tibia, and the scaffold was implanted. A customized bone plate was used to prevent fracture [12] (Fig. 3a).
2.2.2 Micro-computed tomography (micro-CT) examination
X-ray images were acquired at 0, 4, 8, and 12 weeks after implantation. Three micro-CT (SkyScan1172; SkyScan, Kontich, Belgium) examinations were performed after dissecting the scaffold from the rabbit tibia. The scanner was set to a voltage of 81 kV and a current of 122 μA to allow sufficient energy. The samples were scanned at 80 μm voxel (3D pixel) resolution with an integration time of 120 ms, to produce reconstructed 3D images. The major pathological parameters were measured three times during the experiment.
2.2.3 Histological evaluation with hematoxylin and eosin staining
At weeks 4, 8, and 12 after implantation, histological evaluations were performed after hematoxylin and eosin (H&E) staining. The transplanted scaffolds were removed, fixed in 4 % paraformaldehyde, decalcified in Calci-Clear Rapid (National Diagnostics, Atlanta, GA), embedded in paraffin, and sectioned on a microtome (HM430; Microm International, Walldorf, Germany) at a thickness of 10 μm. The sections were floated in a water bath at 40 °C, positioned on poly-l-lysine-coated microscope slides, baked overnight at 37 °C, stained with H&E, and covered with Permount. Images were acquired at 10× magnification with a video microscope system (Stemi 2000; Carl Zeiss, Germany).
2.3 Statistical analysis
All data were analyzed using SPSS (ver. 11.0 K; SPSS Inc., Chicago, IL, USA) with one-way ANOVA. Fisher’s least significant difference (LSD) method was adopted for multiple comparisons. The significance level was set at P < 0.05.
3 Results
The general shape of each scaffold type and corresponding SEM images are shown in Fig. 1b, c. The pore size was uniform (~770 and 600 μm for PCL and PLGA scaffolds, respectively), and the pores were closely interconnected, which should enable cells to penetrate the depths of the scaffold. The layers showed uniform arrangement.
Live/dead staining of L-929 cells at day 2 (Fig. 2a, b) confirmed that neither scaffold material was toxic to the cells, suggesting that neither would cause side-effects in vivo. The MTT assay results (Fig. 2c) showed normal cell proliferation in the presence of the scaffold materials.
The apparent compressive modulus was 1.65 ± 0.52 and 2.55 ± 0.11 MPa for the PCL scaffolds and the PLGA scaffolds, respectively. They were significantly different (P < 0.05).
The hematological parameters measured during the experiment (Table 1) were all within normal ranges, indicating that the implanted scaffolds did not cause major hematological problems or side-effects.
Radiological observations for up to week 12 are presented in Fig. 3b. Immediately after surgery, the scaffold images were vague because of their radiological characteristics. At week 4, new bone had started to form in both scaffold types. The PLGA scaffolds showed some loss, while the PCL scaffolds were still intact. From week 8 to 12, continuous bone tissue formation was observed in both scaffold types. However, the density of the bone generated in the PLGA group did not appear to be uniform. The structure of the PCL scaffold remained distinct, whereas that of the PLGA did not.
Images illustrating the surgical technique for implanting scaffolds and radiological image. a A custom-designed bone plate was used to prevent fracture. b Radiological observations of the (top panels) PCL at 0, 4, 8, and 12 weeks after implantation. c Radiological observations of the (bottom panels) PLGA at 0, 4, 8, and 12 weeks after implantation
Radiological findings were supported by the micro-CT images (Fig. 4). At week 4, the PCL scaffold was intact, whereas the PLGA scaffold had started to degrade. At week 8, new bone tissue regeneration had started throughout the PCL scaffold, but new bone was not seen in the PLGA scaffold, as it continued to degenerate. Further bone regeneration was seen in both cases at week 12. Most parts of the scaffold were displaced by regenerated tissue in the PLGA group, while the PCL scaffold was still observed. Nevertheless, tissue regeneration occurred inside the PCL scaffold.
Microscopic observations of H&E stained preparations revealed the new bone tissue formation in more detail (Fig. 5). At week 4, new bone formation was seen throughout the scaffold structure in the PCL group. Although new bone formation was evident in the PLGA group, the scaffold structure itself was difficult to see; in addition, the density of the newly formed tissue was not uniform. Continuous new bone formation was observed in the PCL group. Even at week 12, the PCL structure remained, and it appeared to guide tissue formation. By contrast, it was difficult to find any remaining PLGA structure after week 8. Overall, new structural compact bone tissue formation was not found in the PLGA group compared with the PCL group.
4 Discussion
We adopted RP technique to fabricate 3D scaffolds for bone tissue regeneration by focusing on (1) enhanced inter-connectivity between pores, (2) controlled pore size, and (3) an optimal degradation rate in vivo. Two types of polymers were used. They were PCL and PLGA, which have different degradation rates [6]. In this study, we did not culture cells on the scaffolds before inserting the scaffolds into relatively large defects in rabbit tibias, in order to simplify the tissue engineering procedure and eliminate the additional effects of cell culture.
Scaffolds were successfully fabricated from two different materials by the RP technique. The pore sizes were uniform and satisfactory, about 770 and 600 μm in the PCL and PLGA scaffolds, respectively, and the layers were regular throughout the thickness of the scaffold (Fig. 1b, c). The apparent compressive modulus of PLGA was found significantly higher than that of PCL, which is supported by a previous report [19]. In addition we used thicker strands and made smaller pores in the PLGA scaffolds because we expected PLGA to degrade sooner than PCL. Regarding to the pore size various researches suggest that the desirable pore size for cell residence and growth is 200 ~ 300 μm [20, 21]. However, we chose larger pores than recommended because we implanted the scaffolds without cells [7, 22]. Although the scaffolds tested were cubes, any shape can be designed with the aid of CAD [12].
The in vitro toxicity tests, following the ISO 10993-5 guidelines, confirmed that both types of scaffolds were safe. In addition, cells proliferated on both materials.
Gradual new bone formation was detected on X-ray images of both scaffolds (Fig. 3b). The scaffolds in the PCL group, but not in the PLGA group, remained visible at week 4 and thereafter. Scaffold degradation in the PLGA group was confirmed on micro-CT images (Fig. 4), which also showed that the PCL scaffolds were intact. With H&E staining (Fig. 5), dense bone tissue was seen inside the PCL scaffolds. Bone tissue had been generated in the PLGA scaffolds, although no scaffold structure remained. Moreover, the tissue generated in the PLGA group did fill the defect uniformly. Thus, in contrast to the PLGA scaffold, the PCL scaffold structure remained intact, bone tissue was generated throughout the PCL structure, and the new bone was denser in the PCL group.
As mentioned above, our scaffolds were designed for treating relatively large defects, in which structural or bone-like material is needed to promote the formation of uniform, dense bone tissue. Ultimately, the implanted material should be degraded, meaning that the rate of degradation should match the rate of new tissue formation.
Given that PCL takes 2 ~ 3 years to degrade and could serve as a structural guide until tissue regeneration is completed [6, 23], PCL appears to be preferable to PLGA for scaffold formation. However, additional material characteristics such as brittleness and ductility should be considered in selecting scaffold materials. The mechanical stiffness of PCL was about 1.0 MPa lower than that of PLGA, which has stiffness lower than that of bone [24–26]. The more brittle and less ductile nature of PLGA in addition to its faster degradation rate make it less desirable than PCL for regeneration of large defects.
5 Conclusions
We also concluded that the RP technique is a promising tool for manufacturing 3D scaffolds whose structural characteristics better enable cells to penetrate to the center of the scaffold, making these scaffolds more desirable for bone tissue regeneration, especially for larger defects [27]. While most previous researches on 3D scaffolds made by RP technique used PCL or PLGA alone. Even most tests were based on in vitro experiments. However, we went further to animal tests for up to 12 weeks, where two promising materials were adopted. Also we inserted the scaffolds into the defect areas without cells, expecting recruitment of neighboring cells. Hematological and in vitro measurements suggest that both PLGA and PCL are safe scaffold materials, although PCL is preferable. PCL scaffold fabricated using the RP technique for larger defect is promising for bone tissue regeneration even without carrying cells before insertion.
References
Persidis A. Tissue engineering. Nat Biotechnol. 1999;17:508–10.
Sachlos E, Czernuszka JT. Making tissue engineering scaffolds work review on the application of solid freeform fabrication technology to the production of tissue engineering scaffolds. Eur Cells Mater. 2009;5:29–40.
Chen G, Ushida T, Tateishi T. Scaffold design for tissue engineering. Macromol Biosci. 2002;2:67–77.
Pathiraja AG, Raju A. Biodegradable synthetic polymers for tissue engineering. Eur Cells Mater. 2003;5:1–16.
Sabir MI, Xu X, Li L. A review on biodegradable polymeric materials for bone tissue engineering applications. J Mater Sci. 2009;44:5713–24.
Nair LS, Laurencin CT. Biodegradable polymers as biomaterials. Prog Polym Sci. 2007;32:762–98.
Hutmacher DW. Scaffolds in tissue engineering bone and cartilage. Biomaterials. 2000;21:2529–43.
Barbanti SH, Carvalho Zavaglia CA, de Rezende Duek EA. Effect of salt leaching on PCL and PLGA(50/50) resorbable scaffolds. Mater Res. 2008;11:75–80.
Mooney DJ, Baldwin DF, Suh NP, Vacanti JP, Langer R. Novel approach to fabricate porous sponges of poly(d,l lactic-co-glycolic acid) without the use of organic solvents. Biomaterials. 1996;17:1417–22.
Harris LD, Kim BS, Mooney DJ. Open pore biodegradable matrices formed with gas foaming. J Biomed Mater Res. 1998;42:396–402.
Yun H, Kim S, Hyun Y, Heo S, Shin J. Three-dimensional mesoporous-giantporous inorganic/organic composite scaffolds for tissue engineering. Chem Mater. 2007;19:6363–6.
Heo S, Kim S, Wei J, Kim DH, Hyun Y, Yun H, Kim HK, Yoon TR, Kim S, Park S, Shin JW, Shin J. In vitro and animal study of novel nano-hydroxyapatite/poly(ε-caprolactone) composite scaffolds fabricated by layer manufacturing process. Tissue Eng Part A. 2009;15:977–89.
De Santis R, Gloria A, Russo T, D’Amora U, Zeppetelli S, Dionigi C, Sytcheva A, Herrmannsdörfer T, Dediu V, Ambrosio L. A basic approach toward the development of nanocomposite magnetic scaffolds for advanced bone tissue engineering. J Appl Polym Sci. 2010;122:3599–605.
Kim GH, Son JG. 3D polycarprolactone (PCL) scaffold with hierarchical structure fabricated by a piezoelectric transducer (PZT)-assisted bioplotter. Appl Phys A. 2009;94:781–5.
Seyednejad H, Gawlitta D, Kuiper RV, Bruin A, Nostrum CF, Vermonden T, Dhert W, Hennink WE. In vivo biocompatibility and biodegradation of 3D-printed porous scaffolds based on a hydroxyl-functionalized poly(ε-caprolactone). Biomaterials. 2012;33:4309–18.
Jia YT, Zhu XY, Liu QQ. In vitro degradation of electrospun fiber membranes of PCL/PVP blends. AMR. 2011;332–334:1330–4.
Sun H, Mei L, Song C, Cui X, Wang P. The in vivo degradation, absorption and excretion of PCL-based implant. Biomaterials. 2006;27:1735–40.
Kim J, McBride S, Tellis B, Alvarez-Urena P, Song YH, Dean DD, Sylvia VL, Elgendy H, Ong J, Hollinger JO. Rapid-prototyped PLGA/β-TCP/hydroxyapatite nanocomposite scaffolds in a rabbit femoral defect model. Biofabrication. 2012;4:1–11.
Baker SC, Rohman G, Southgate J, Cameron NR. The relationship between the mechanical properties and cell behaviour on PLGA and PCL scaffolds for bladder tissue engineering. Biomaterials. 2009;30:1321–8.
Hulbert SF, Morrison SJ, Klawitter JJ. Tissue reaction to three ceramics of porous and non-porous structures. J Biomed Mater Res. 1972;6:347–74.
Flatley TJ, Lynch KL, Benson M. Tissue response to implants of calcium phosphate ceramics in rabbit spine. Clin Orthop. 1983;179:246–52.
Slagada AJ, Coutinho OP, Reis RL. Bone tissue engineering: state of they are and future trends. Macromol Biosci. 2004;4:743–65.
Yao J, Tao SL, Young MJ. Synthetic polymer scaffolds for stem cell transplantation in retinal tissue engineering. Polymers. 2011;3:899–914.
Hoffmeister BK, Smith SR, Handley SM, Rho JY. Anisotropy of Young’s modulus of human tibial cortical bone. Med Biol Eng Comput. 2000;38:333–8.
Rho JY, Ashman RB, Turner CH. Young’s modulus of trabecular and cortical bone material: ultrasonic and microtensile measurements. J Biomech. 1993;26:111–9.
Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials. 2005;26:5474–91.
Schieker M, Seitz H, Drosse I, Seitz S, Mutschler W. Biomaterials as scaffold for bone tissue engineering. Eur J Trauma. 2006;2:114–24.
Acknowledgments
This work was supported by the grants of Technology Innovation Program (10038667, Ministry of Knowledge Economy, ROK) and Priority Research Centers Program (2010-0020224, the Ministry of Education, Science and Technology).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Park, S.H., Park, D.S., Shin, J.W. et al. Scaffolds for bone tissue engineering fabricated from two different materials by the rapid prototyping technique: PCL versus PLGA. J Mater Sci: Mater Med 23, 2671–2678 (2012). https://doi.org/10.1007/s10856-012-4738-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-012-4738-8