Abstract
Currently, in bone tissue engineering research, the development of appropriate biomaterials for the regeneration of bony tissues is a major concern. Bone tissue is composed of a structural protein, collagen type I, on which calcium phosphate crystals are enclosed. For tissue engineering, one of the most applied strategies consists on the development and application of three dimensional porous scaffolds with similar composition to the bone. In this way, they can provide a physical support for cell attachment, proliferation, nutrient transport and new bone tissue infiltration. Hydroxyapatite is a calcium phosphate with a similar composition of bone and widely applied in several medical/dentistry fields. Therefore, in this study, hydroxyapatite three dimensional porous scaffolds were produced using the polymer replication method. Next, the porous scaffolds were homogeneously coated with a film of collagen type I by applying vacuum force. Yet, due to collagen degradability properties, it was necessary to perform an adequate crosslinking method. As a result, N-(3-dimethylaminopropyl)-N′-ethylcarbodiimide hydrochloride (EDC) and N-hydroxysuccinimide (NHS) was employed as an efficient and non-toxic crosslinking method in this research. The composites were characterized by means of SEM, DSC and TNBS. Furthermore, heparin was incorporated in order to accomplish sustained delivery of a growth factor of interest namely, bone morphogenetic proteins (BMP-2). BMP-2 binding and release of non-heparinized and heparinized scaffolds was evaluated at specific time points. The incorporation of heparin leads to a reduced initial burst phase when compared to the non heparinized materials. The results show a beneficial effect with the incorporation of heparin and its potential as a localized drug delivery system for the sustained release of growth factors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The current strategies capable of repairing and/or substituting damaged or lost bone tissue consist of using autografts and allografts.
However, these options bring some disadvantages, namely, tissue availability, transmission of diseases and donor morbidity [1]. Consequently, different approaches are required, including the development of alternative therapies for the repair/substitution of damaged bone tissue. Bone tissue engineering is a promising area that aims at developing implants specifically through the use of scaffolds that are combined with the appropriate cells.
To be used as a scaffold, a 3D structure must meet some criteria. First, the scaffold must have an adequate macroporosity to allow cell migration. Second, the scaffold should present microporosity thereby creating locations for cell attachment. Another requirement is the presence of interconnected porosity, providing conditions for nutrient transport, tissue infiltration and vascularization. Several materials may be used as scaffolds namely, polymers, glasses and calcium phosphates, being the latter a very interesting choice. On the other hand, since these materials will be in contact with cells, it is important to choose a scaffold material that facilitates cell adhesion, differentiation and assist the formation of new bone tissue. In order to provide these conditions to cells, the scaffold material is preferably similar to the natural bone’s composition. Given that the mineral phase of bone is mainly constituted by calcium phosphate crystals, hydroxyapatite is then one of the most employed ceramics for maxilo-facial, dentistry and orthopaedic applications [1]. Hydroxyapatite is biocompatible, osteoconductive and can be easily combined with other materials. The most common examples are hydroxyapatite associated with synthetic polymers (PLLA, PGLA, etc.) [2–6], or even nanohydroxyapatite combined with natural polymers (chitosan, collagen) [7–10].
Collagen is the most important structural protein present in bone. Collagen as a biomaterial is widely used in the form of gels, powders or films. However, due to its degradation rate, crosslinking must be applied to overcome its fast resorption in vivo. In order to do that, several crosslinking agents can be applied, being glutaraldehyde one of the most common. Although glutaraldehyde is considered to be a toxic crosslinking agent, it is still one of the most widely applied. Recently the use of N-(3-dimethylaminopropyl)-N′-ethylcarbodiimide hydrochloride (EDC) and N-hydroxysuccinimide (NHS) has proven an effective non-toxic collagen crosslinker [11–13] and was used in the production of collagen scaffolds [11, 12, 14–17]. In addition, collagen based systems can also be used as carriers for the delivery of molecules of interest such as bone morphogenetic proteins (BMP’s), vascular endothelial factors (VEGF’s), etc [18, 19].
Heparin is well known for its affinity to bind to certain proteins, namely collagen and growth factors. Coating heparin onto a surface of a biomaterial can result in the development of a localized drug delivery system, capable to perform a sustained release of growth factors, or other important molecules [14, 20–23].
One important aspect in the development of bioengineered tissue is vascularization [14]. The use of growth factors such as bone morphogenetic proteins (BMP’s) have a great influence in promoting newly formed bony tissue. On the other hand, heparin has great binding affinity to these factors and can promote its sustained release [12, 14, 16, 18, 19].
Nevertheless, when designing a scaffold for bone tissue engineering, collagen/heparin systems are not the best proposition due to their low mechanical strength [12, 14, 16].
In this work, highly macroporous hydroxyapatite scaffolds were produced and a homogeneous collagen type I film was deposited on the scaffold surface. The EDC/NHS crosslinking method was then applied to stabilize the collagen coating. Additionally, heparin was successfully conjugated to the collagen, and BMP-2 binding and release of non-heparinized and heparinized scaffolds was also evaluated, showing the potential of this composite to be used not only as a bone regenerating tissue scaffold, but as a localized drug delivery system for the sustained release of growth factors.
2 Materials and methods
2.1 Sample preparation
The scaffolds were prepared using polyurethane sponges kindly provided by Recticel (Belgium). These polyurethane sponges were impregnated with ceramic slurry as reported previously [24]. Briefly, a ceramic slurry was prepared using a mixture of hydroxyapatite (Plasma Biotal, P120), water and surfactant (LM-3, NeoDisher), in a ratio of 6 to 4 to 0.2 (w/w).
The polyurethane sponge was squeezed to remove the excess slurry and submitted to the following sintering cycle: heating from 20 to 600°C at 1°C/min followed by 1 h at 600°C; heating from 600 to 1300°C at 4°C/min followed by 1 h at 1350°C. Then the samples were slowly cooled inside the oven. Afterwards, the sponges were cut into 5 mm edge cubes.
Bovine Achilles tendon collagen type I from Sigma-Aldrich was swollen in hydrochloric acid (0.01 M) overnight at 4°C. The slurry was shredded for 10 min at 9500 rpm using an Ultra-Turrax T25. The temperature was kept below 4°C. The resulting mixture was filtered using a 74 μm filter (Bellco Glass Inc.) to give a homogeneous collagen dispersion.
Collagen films were prepared by casting the collagen dispersion onto a PTFE surface using a casting knife. After drying at room temperature, a collagen film with a thickness of approximately 50 μm was obtained.
The hydroxyapatite scaffolds were impregnated with the collagen dispersion by applying vacuum (1 bar pressure) as a driving force.
2.2 Collagen crosslinking
The collagen in the scaffolds was either crosslinked with glutaraldehyde (Aga) or with a mixture of N-(3-dimethylaminopropyl)-N′-ethylcarbodiimide hydrochloride (EDC, Fluka) and N-hydroxysuccinimide (NHS, Fluka) as described previously [15–17].
For collagen dispersions and films, the crosslinking procedure applied was the same. Due to the fact that collagen assays (denaturation temperature and free amino group content) could not be performed on the collagen coating present in the scaffolds, they were performed on collagen films and dispersions prepared from the same collagen starting material.
For glutaraldehyde crosslinking, 5 ml of a freshly prepared collagen dispersion was added to a mixture of 190 ml of PBS (phosphate buffered saline buffer, pH 7.4, Sigma) and 5 ml of glutaraldehyde (10% v/v) solution and the resulting mixture was gently shaken for 2 h at room temperature. Afterwards, the crosslinking solution was removed and the samples were rinsed with tap water (15 min), 4 M NaCl (30 min) and demineralized Millipore water (2 times for 30 min), respectively. After the washing, the samples were frozen with liquid nitrogen and freeze dried.
Crosslinking of collagen present in the scaffolds by the activation method using EDC and NHS was performed by first equilibrating the samples in a buffer of 2-morpholinoethane sulfonic acid (MES buffer, 0.05 M, pH = 5.40, Sigma) for 30 min.
To a solution of 3.766 g of heparin in 188.3 ml of MES buffer were added 0.433 g of EDC and 0.157 g of NHS. The films were then incubated in this preactivated solution for 2 h to afford both crosslinking and heparin immobilization. Afterwards, the samples were removed and placed in a PBS solution for 2 h to stop the immobilization reaction. The samples were then washed with 2 M NaCl (6 times for 4 h), 4 M NaCl (4 times for 6 h), and distilled water (3 times for 8 h), respectively. Samples were then frozen with liquid nitrogen and freeze dried for 48 h.
2.3 Scanning electron microscopy (SEM)
The samples were partially immersed in resin and gold sputtered. Scanning electron microscopy was carried out using a JEOL JSM 6301F microscope.
2.4 Differential scanning calorimetry (DSC)
The denaturation temperature of non crosslinked and crosslinked collagen was measured using a Perkin Elmer DSC7 DSC apparatus. The samples (with a dry weight between 3 and 5 mg) were incubated overnight in 50 μl of phosphate buffered saline solution (PBS) before measurement. The samples were heated from 20 to 90°C at a rate of 5°C per minute. A sample containing 50 μl of PBS was used as a reference. The maximum of the endothermic peak was taken as being the denaturation temperature.
2.5 Determination of free amino groups (TNBS)
The free amino groups content of native and cross-linked samples was determined using the 2,4,6-trinitrobenzenesulfonic acid (TNBS, Fluka) assay [15–17].
Samples of freeze dried collagen fibrils or films of 3–5 mg were incubated for 30 min in 1 ml of a 4 wt% solution of NaHCO3. To this mixture, 1 ml of a freshly prepared solution of TNBS (0.5 wt%) in 4 wt% NaHCO3 was added. The resulting mixture was incubated for 2 h at 40°C. After the addition of HCl (3 ml, 6 M), the temperature was raised to 60°C. Solubilization of collagen was achieved within 90 min. The resulting solution was diluted with 5 ml Millipore water and cooled to room temperature. The absorbance at 420 nm was measured using a Varian Cary 300 Bio spectrophotometer.
A blank was prepared applying the same procedure, except that HCl was added before the addition of TNBS. The absorbance was correlated to the concentration of free amino groups using a calibration curve obtained with glycine. The free amino group content was expressed as the number of free amino groups per 1000 amino acids (n/1000).
2.6 Alcian blue staining
Alcian blue belongs to a group of polyvalent basic dyes that are water soluble. This stain solution was used to visualize the immobilized heparin in the crosslinked collagen samples. Samples were incubated in an acetic acid solution (3% v/v, pH 2.5) for 3 min, being subsequently transferred to the Alcian Blue staining solution (Sigma), where they remained for 30 min. Samples were then washed with Millipore water four times for 15 min.
2.7 Toluidine blue
The heparin content of the collagen films was determined using a colorimetric method based on binding of toluidine blue. Samples were incubated in a toluidine blue solution (0.15 mg/ml, Fluka) and the decrease in absorption of the toluidine solution was measured at 630 nm. To quantify the immobilized heparin content on the collagen films, 1 mg of sample was incubated in 0.5 ml of water and 0.5 ml of toluidine blue solution (0.15 mg/ml) for 24 h.
Next, 1 ml of cyclohexane was added and the mixture was thoroughly vortexed. The mixture was left to rest, in order to allow the phases to separate. The upper layer was then removed and 0.3 ml of the lower phase were re-suspended with 3 ml of water and the absorbance was measured at 630 nm. A calibration curve was prepared with known concentrations of heparin and its absorbance was measured.
2.8 BMP-2 binding
BMP-2 (BioSource, 5 μg in 100 μl of 1% bovine serum albumin/phosphate buffered saline (BSA/PBS)) was loaded onto the surface of all porous scaffolds: hydroxyapatite (HA), hydroxyapatite with collagen (HA XL) and hydroxyapatite with collagen and heparin (HA XL Hep) using vacuum as a driving force. The samples were kept at 4°C overnight before incubation with 1 ml of release medium (1% bovine serum albumin/phosphate buffered saline (BSA/PBS). The release medium was collected and replaced with fresh one at specific time points: 1, 6, 12, 24, 48, 72, 96, 120 and 168 h.
All collected solutions were stored at −20°C until their concentration was analysed by means of enzyme linked immunoabsorvent assay (ELISA). The ELISA procedure was adapted from Human BMP-2 Quantikine ELISA kit (DBP200, R&D Systems) for human BMP-2. A monoclonal antibody specific for BMP-2 was used as capture antibody and a substrate solution was used as detection antibody. The samples were then read in a ELISA plate reader (ELX 808, Biotek Intrusments, Inc.) at 450 nm with a wavelength correction set to 540 nm.
3 Results
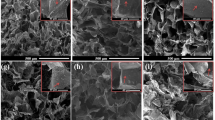
In Fig. 1, SEM images of a hydroxyapatite scaffold obtained by the replication method are presented. In the replication method, polyurethane sponges were impregnated with ceramic slurry. The excess slurry was removed and the polyurethane/hydroxyapatite composite was submitted to a sintering cycle to remove the polyurethane, resulting in a highly porous hydroxyapatite scaffold.
The scaffold surface suggests the presence of appropriate sites for cell attachment (Fig. 1b) due to the existence of micropores, macropores (with diameters ranging 300 μm), which are completely interconnected throughout the scaffold, leading to a high interconnectivity (Fig. 1a). From this analysis and previous performed μ-CT measurements [25], it may be concluded that the scaffold meets the required criteria for bone tissue engineering applications in terms of porosity. After producing hydroxyapatite porous scaffolds, the collagen was later integrated to complete the hydroxyaptite/collagen composite.
Collagen type I solution was prepared and incorporated onto the structure (by means of vacuum) of the porous hydroxyapatite scaffolds. Because the effects of crosslinking on the properties of collagen coating were difficult to determine when coated on the scaffold, thin films were prepared of the same material and subsequently analyzed. Using DSC, the denaturation temperature of collagen non-crosslinked and collagen crosslinked with either glutaraldehyde or EDC/NHS method was determined and the results are shown in Table 1.
These results are commonly observed in collagen crosslinking using these methods. Despite this, the shrinkage temperature measurements show that there is only a slight difference between glutaraldehyde and EDC/NHS values, indicating that EDC/NHS is a viable alternative as a non-toxic crosslinker, as reported in the literature [15–19].
DSC measurements were also performed (Table 1) showing that, the incorporation of heparin did not interfere with the shrinkage temperature of the developed system.
The collagen coating present in the porous hydroxyapatite scaffold before and after crosslinking was visualised by SEM and representative images are presented in Figs. 2 and 3.
The incorporation of collagen (native and crosslinked) in the structure of the porous hydroxyapatite scaffold does not alter significantly the scaffold porous inner structure.
Heparin was incorporated in the composite to improve biocompatibility and also to study the possibility of carrying other heparin-binding molecules to be used for controlled and sustained release.
In order to carry out a qualitative and quantitative analysis of the heparin present in the composite, Alcian Blue Staining and the Toluidine Blue assays were performed on films prepared from collagen-heparin conjugates.
Since the composites were coated with a thin film of collagen and some assays require critical collagen content, the assays were performed on collagen-heparin films.
In Table 1, it can be seen that the amount of heparin retained is higher than the one present in the non-crosslinked collagen system. Furthermore, the distribution of heparin throughout the collagen film is more homogeneous in the crosslinked system than in the non-crosslinked system, being the latter characterized by a heterogeneous distribution (Fig. 4).
BMP-2 (5 μg in 100 μl of release medium) was loaded in hydroxyapatite scaffolds, with collagen and heparin and its cumulative release profile evaluated (Fig. 5).
BMP 2 cumulative release profiles of all the tested samples: hydroxyapatite scaffold (♦), hydroxyapatite scaffold coated with collagen (■) and hydroxyapatite scaffold coated with collagen/ heparin conjugate (▲). Figure 6 Concentration of BMP 2 retained in all the tested samples: hydroxyapatite scaffold (HA), hydroxyapatite scaffold coated with collagen (HA XL COL) and hydroxyapatite scaffold coated with collagen/ heparin conjugate (HA COL HEP)
The samples were collected at specific time points and their concentration measured by means of ELISA.
For all tested samples, it can be seen from Fig. 5 that the cumulative release profile consists of two phases: an initial burst release occurring during the first 24 h and then a linear and progressive release phase for the rest of the time course (48 h until 168 h).
The cumulative release profiles show that the collagen and collagen heparin conjugates gave a reduced initial burst and subsequent slow release of the growth. The hydroxyapatite samples gave a high growth factor release in the first hour. In order to estimate the amount of non released BMP-2, the remaining BMP-2 present in the scaffolds was also determined.
The scaffolds were kept after the experiment, crushed and their supernatant removed and the concentration was determined by means of ELISA (Fig. 6).
By analysing Fig. 6, it can be seen that a higher amount of BMP-2 was retained by the collagen/heparin coated samples than by the non-modified material.
This fact also supports the cumulative release profile obtained, that showed a slower release of the growth factor at all time points evaluated (1 h until 168 h) in the case of heparin containing samples.
4 Discussion
In this study, hydroxyapatite macroporous scaffolds were produced, biofunctionalized and their potential to serve as carriers of BMP-2 was investigated.
By using the polymer replication method, macroporous interconnected scaffolds were prepared. Polyurethane sponges were soaked with a ceramic slurry composed of hydroxyapatite, water and tensioactive and later, after the excess solution was removed, the sponges were sintered. To improve cell adhesion, a collagen type I coating was added to the scaffold surface. This was done by incubating the scaffolds in a suspension of collagen fibrils and applying vacuum to ensure that all surface would be exposed to collagen. These fibrils were either non-crosslinked or crosslinked prior to the incubation step using different crosslinking techniques. Non-crosslinked collagen and glutaraldehyde crosslinked collagen samples were used as references. In order to characterize the shrinkage temperature and the crosslinking density, differential scanning calorimetry and free amine groups quantification methods were used, respectively. DSC results showed that the collagen crosslinking with EDC/NHS is very efficient and proved to be almost as effective as glutaraldehyde, as reported in literature [15, 18]. The free amino group content (lysine, hydroxylysine residues) of the collagen materials decreased upon crosslinking. For glutaraldehyde treatment the values are somewhat lower than found upon crosslinking using EDC/NHS activation. With the deposition of collagen in the pores surface, it was possible to have a coating that did not affect the scaffold porosity during the following crosslinking step with EDC/NHS. Moreover, the pore size was not significantly altered after crosslinking and round pores were observed in both cases, by SEM.
The presence of heparin and its content were evaluated by qualitative and quantitative methods, namely the Alcian Blue staining and the Toluidine Blue assay. In the crosslinked and heparinized films, heparin was homogeneously distributed along the surface, whereas in the non-crosslinked films the heparin was dispersed in small clusters along the film surface as expected [15–17]. This fact indicated that the crosslinking step plays a critical role since it influences the distribution of the heparin along the film. Furthermore, results pointed out that higher amounts of heparin are retained in the crosslinked system than in the non-crosslinked system, as expected (and also confirmed by the alcian blue staining).
The ability of these scaffolds to adsorb, carry and deliver in a sustainable manner BMP-2 with the aid of heparin was the next step on this study. The results showed that coating hydroxyapatite scaffolds with collagen and conjugate heparin into the system, led to a higher quantity of retained BMP-2 compared with non-modified collagen and hydroxyapatite alone. This could be due to stronger binding of BMP-2 to heparin compared with collagen, as it is known that BMP-2 contains a binding site for heparin [25].
The retarded release of BMP-2 from heparinized collagen scaffolds was characterized by a reduced initial burst release phase followed by a controlled and prolonged release of the growth factor when compared to the other samples. Interestingly, the release of BMP-2 from a collagen coating shows a similar profile with a slightly higher burst release compared to the collagen/heparin conjugate coating. Furthermore, higher concentration of BMP-2 was retained on the hydroxyapatite/collagen/heparin samples when compared with other the other conditions. As previously stated, heparin affinity to BMP-2 allows the later to act as a reservoir for the molecule, hindering its release form the overall system, hence acting as an advantage on the controlled release.
In bone tissue engineering, scaffold materials are the current strategy to repair bony tissue and to locally deliver growth factors of interest, namely BMP-2. During this process, it is important to maintain a constant and sustained release of the growth factors from the scaffold [27]. Compared with other scaffold materials, HA XL Hep possess adequate mechanical properties [28] and superior bioactivity when used in bone tissue engineering applications [26] as previously reported by our findings. Moreover, the composites investigated in this study exhibited good absorption and sustained release of BMP-2 over a 7-day period in vitro. These findings suggest that HA XL Hep scaffolds have the potential to serve as a controlled-release carrier of BMP-2 which would be potentially useful as a bone regenerative material.
5 Conclusion
In order to investigate the possibility of using macroporous hydroxyapatite/collagen scaffolds as a controlled-release carrier of BMP-2, this work examined the absorption of BMP-2 and the release kinetics of BMP-2 from hydroxyapatite/collagen scaffolds in vitro. To ensure a controlled and sustained delivery of BMP-2, heparin was included onto the system. It was observed that the presence of heparin severely reduces the characteristic initial burst release phase, hence, the release profile of BMP-2 could be sustained for 7 days in vitro and in a controlled manner. Moreover, our results suggest that these materials have the potential to function as a carriers for drug delivery systems and to be applicable as a scaffold material in bone tissue as previously reported in our findings.
References
Rose FR, Cyster LA, Grant DM, Scotchford CA, Howdle SM, Shakesheff KM. In vitro assessment of cell penetration into porous hydroxyapatite scaffolds with a central aligned channel. Biomaterials. 2004;25(24):5507–14.
Hong Z, Zhang P, He C, Qiu X, Liu A, Chen L, et al. Nano-composite of poly(l-lactide) and surface grafted hydroxyapatite: mechanical properties and biocompatibility. Biomaterials. 2005;26(32):6296–304.
Ignjatovic N, Tomic S, Dakic M, Miljkovic M, Plavsic M, Uskokovic D. Synthesis and properties of hydroxyapatite/poly-l-lactide composite biomaterials. Biomaterials. 1999;20(9):809–16.
Kothapalli CR, Shaw MT, Wei M. Biodegradable HA-PLA 3-D porous scaffolds: effect of nano-sized filler content on scaffold properties. Acta Biomater. 2005;1(6):653–62.
Liao S, Wang W, Uo M, Ohkawa S, Akasaka T, Tamura K, et al. A three-layered nano-carbonated hydroxyapatite/collagen/PLGA composite membrane for guided tissue regeneration. Biomaterials. 2005;26(36):7564–71.
Maeda H, Kasuga T, Hench LL. Preparation of poly(l-lactic acid)-polysiloxane-calcium carbonate hybrid membranes for guided bone regeneration. Biomaterials. 2006;27(8):1216–22.
Kong L, Gao Y, Cao W, Gong Y, Zhao N, Zhang X. Preparation and characterization of nano-hydroxyapatite/chitosan composite scaffolds. J Biomed Mater Res. 2005;75(2):275–82.
Li XM, Feng QL, Cui FZ. In vitro degradation of porous nano-hydroxyapatite/collagen/PLLA scaffold reinforced by chitin fibres. Mater Sci Eng C-Biomim Supramol Syst. 2006;26(4):716–20.
Sachlos E, Gotora D, Czernuszka JT. Collagen scaffolds reinforced with biomimetic composite nano-sized carbonate-substituted hydroxyapatite crystals and shaped by rapid prototyping to contain internal microchannels. Tissue Eng. 2006;12(9):2479–87.
Zhu X, Eibl O, Scheideler L, Geis-Gerstorfer J. Characterization of nano hydroxyapatite/collagen surfaces and cellular behaviors. J Biomed Mater Res. 2006;79(1):114–27.
Pieper JS, Hafmans T, Veerkamp JH, van Kuppevelt TH. Development of tailor-made collagen-glycosaminoglycan matrices: EDC/NHS crosslinking, and ultrastructural aspects. Biomaterials. 2000;21(6):581–93.
Pieper JS, Oosterhof A, Dijkstra PJ, Veerkamp JH, van Kuppevelt TH. Preparation and characterization of porous crosslinked collagenous matrices containing bioavailable chondroitin sulphate. Biomaterials. 1999;20(9):847–58.
Pieper JS, van Wachem PB, van Luyn MJA, Brouwer LA, Hafmans T, Veerkamp JH, et al. Attachment of glycosaminoglycans to collagenous matrices modulates the tissue response in rats. Biomaterials. 2000;21(16):1689–99.
Pieper JS, Hafmans T, van Wachem PB, van Luyn MJA, Brouwer LA, Veerkamp JH, et al. Loading of collagen-heparan sulfate matrices with bFGF promotes angiogenesis and tissue generation in rats. J Biomed Mater Res. 2002;62(2):185–94.
Wissink MJB, Beernink R, Pieper JS, Poot AA, Engbers GHM, Beugeling T, et al. Immobilization of heparin to EDC/NHS-crosslinked collagen. Characterization and in vitro evaluation. Biomaterials. 2001;22(2):151–63.
Wissink MJB, Beernink R, Poot AA, Engbers GHM, Beugeling T, van Aken WG, et al. Improved endothelialization of vascular grafts by local release of growth factor from heparinized collagen matrices. J Control Release. 2000;64(1–3):103–14.
Wissink MJB, Beernink R, Scharenborg NM, Poot AA, Engbers GHM, Beugeling T, et al. Endothelial cell seeding of (heparinized) collagen matrices: effects of bFGF pre-loading on proliferation (after low density seeding) and pro-coagulant factors. J Control Release. 2000;67(2–3):141–55.
Steffens GCM, Yao C, Prevel P, Markowicz M, Schenck P, Noah EM, et al. Modulation of angiogenic potential of collagen matrices by covalent incorporation of heparin and loading with vascular endothelial growth factor.Tissue Eng. 2004:1502–9.
Yao C, Markowicz M, Pallua N, Magnus Noah E, Steffens G. The effect of cross-linking of collagen matrices on their angiogenic capability. Biomaterials. 2008;29(1):66–74.
Jiao YY, Ubrich N, Hoffart V, Marchand-Arvier M, Vigneron C, Hoffman M, et al. Preparation and characterization of heparin-loaded polymeric microparticles. Drug Dev Ind Pharm. 2002;28(8):1033–41.
Jiao YY, Ubrich N, Marchand-Arvier M, Vigneron C, Hoffman M, Lecompte T, et al. In vitro and in vivo evaluation of oral heparin-loaded polymeric nanoparticles in rabbits. Circulation. 2002;105(2):230–5.
Lee KW, Yoon JJ, Lee JH, Kim SY, Jung HJ, Kim SJ, et al. Sustained release of vascular endothelial growth factor from calcium-induced alginate hydrogels reinforced by heparin and chitosan. Transpl Proc. 2004;36(8):2464–5.
SchroederTefft JA, Bentz H, Estridge TD. Collagen and heparin matrices for growth factor delivery. J Control Release. 1997;48(1):29–33.
Teixeira S, Ferraz MP, Monteiro FJ. Biocompatibility of highly macroporous ceramic scaffolds: cell adhesion and morphology studies. J Mater Sci. 2008;19(2):855–9.
Edlund U, Dånmark S, Albertsson AC. A strategy for the covalent functionalization of resorbable polymers with heparin and osteoinductive growth factor. Biomacromolecules. 2008;9(3):901–5.
Teixeira S, Oliveira S, Ferraz M, Monteiro FJ. Three dimensional macroporous calcium phosphates scaffolds for bone tissue engineering. Key Eng Mater Trans Tech. 2008:947–50.
Yamamoto M, Tabata Y, Hong L, Miyamoto S, Hashimoto N, Ikada Y. Bone regeneration by transforming growth factor beta1 released from a biodegradable hydrogel. J Control Release. 2000;64:133–42.
Teixeira S, Rodriguez MA, Pena P, De Aza AH, De Aza S, Ferraz MP, Monteiro FJ. Physical characterization of hydroxyapatite porous scaffolds for tissue engineering. Mater Sci Eng C. 2009;29(5):1510–4.
Acknowledgments
This work was supported by the Portuguese Foundation for Science and Technology (FCT) PhD grant SFRH/BD/17139/2004 and project FCT - POCTI/SAU - BMA/56061/2004. The authors would also like to thank Jun Liu for the assistance in the release experiments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teixeira, S., Yang, L., Dijkstra, P.J. et al. Heparinized hydroxyapatite/collagen three-dimensional scaffolds for tissue engineering. J Mater Sci: Mater Med 21, 2385–2392 (2010). https://doi.org/10.1007/s10856-010-4097-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-010-4097-2