Abstract
Calcium phosphate cements have the potential to be successful in minimally invasive surgical techniques, like that of vertebroplasty, due to their ability to be injected into a specific bone cavity. These bone cements set to produce a material similar to that of the natural mineral component in bone. Due to the ceramic nature of these materials they are highly brittle and it has been found that they are difficult to inject. This study was carried out to determine the factors that have the greatest effect on the mechanical and handling properties of an apatitic calcium phosphate cement with the use of a Design of Experiments (DoE) approach. The properties of the cement were predominantly influenced by the liquid:powder ratio and weight percent of di-sodium hydrogen phosphate within the liquid phase. An optimum cement composition was hypothesised and tested. The mechanical properties of the optimised cement were within the clinical range for vertebroplasty, however, the handling properties still require improvement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The first successful calcium phosphate cement (CPC) was created by Brown and Chow in 1983 [1]. It consisted of powder and liquid components which, when mixed produced an injectable paste that could be moulded to a specific bone cavity. This cement subsequently hardened in situ to produce a porous material. Since this development there have been many different formulations of CPCs with various compositions proposed. There are two basic forms available, apatite and brushite, depending on the material used and cement produced [2]. Apatitic cements typically include alpha-tricalcium phosphate (α-TCP) as its powder component which sets according to the Eq. 1 [3, 4]:
Brushite cements are produced as a result of an acid–base reaction (Eq. 2), often using beta-tricalcium phosphate (β-TCP) as the starting material [3, 4]:
A significant focus in this field of research has been on the use of α-TCP based cements produced through a dissolution-precipitation reaction [5]. This involves the α-TCP dissolving within the chosen solution, after which an interlocked network of crystals, that is calcium deficient hydroxyapatite (CDHA, Ca9(HPO4)(PO4)5(OH)), is produced providing a state of mechanical stability [6]. Even though these cements are widely used in maxillofacial and craniofacial surgery, they still do not have the capability for the treatment of traumatic vertebral burst fractures using vertebroplasty due to the CPC’s not having sufficient mechanical stability [7, 8]. Vertebroplasty is a minimally invasive surgical technique that aims to stabilise fractured vertebrae. If a CPC was to be successful in this anatomical region it is thought that it must at least match the properties of the healthy intact bone. Certain clinical requirements have therefore been proposed to provide direction in this area of research, which are that the final setting should be no more than 15 min, a minimum compressive strength of 30 MPa should be achieved and the material must be easily injected into the collapsed vertebra without leakage or material wastage [9, 10].
In an attempt to achieve the aforementioned clinical requirements, attention has been paid to cement optimisation by altering the initial powder and/or liquid phase. It is widely accepted that the injectability can be controlled by the liquid to powder ratio (LPR), whereby increasing the LPR will improve the injection capabilities [11]. However, if the cement has too low a viscosity washout can become an issue, which is when the cement washes out into the surrounding area upon contact with blood and body fluids [12]. The liquid phase has been studied by a number of research groups. Ginebra et al. [13] considered the use of a sodium phosphate solution compared to distilled water. This study concluded that di-sodium hydrogen phosphate solution (Na2HPO4) could be used to reduce the setting time, however, this solution reduced the compressive strength from 40 to 7 MPa. Barone et al. [14] verified these results with a commercially available CPC (BoneSource™) and demonstrated that using a sodium phosphate solution reduced the final setting time from 99 to 43 min. Within the powder phase particular attention has been paid to the idea of using a seed which is a material that acts as a nucleator for the precipitation reaction, which may reduce the extent of the setting reaction [4]. A typical nucleation agent used is hydroxyapatite (HA, Ca5(PO4)3OH)). Brown et al. [15] found that adding 43 weight percent (wt%) HA to the powder phase reduced the setting time from 22 to 8 min. Lui et al. [16] used 5 wt% HA and observed that the final setting time was reduced from 150 to 7 min. Previous work has concentrated on using HA in the micro form, however, it has been postulated theoretically that nanosized HA could have a profound effect on both the setting and injection capability of CPC, though this hypothesis has not been validated [17]. One issue that often arises with the introduction of nanosized materials is the occurrence of agglomerations, due to smaller particles having an increased attraction in the form of van der Waals forces [3, 18].
Notwithstanding the significant amount of research being conducted in the area of CPC systems, it is still unclear as to what is the optimum liquid and powder composition and if there are any interactions taking place between the changeable factors (for example, LPR, wt% sodium phosphate solution, size of HA particles). The objective of this study was to investigate the changeable factors that had the greatest effect on the mechanical performance and handling properties of a CPC system using a Design of Experiments (DoE) approach. The information collated was then used to design an optimum CPC system for the clinical application of vertebroplasty. The DoE methodology was also used to determine the major factors and interactions that affect the initial and final cement properties.
2 Materials and methods
2.1 Production of CPC
The main powder component used was α-TCP which was produced following the method described by Jack et al. [2]. This involved mixing calcium phosphate (CaHPO4) and calcium carbonate (CaCO3) powders at a molar mixture of 2:1, which was turbo-blended and heat treated in a furnace (Elite BRF15/5, Elite Thermal Systems Ltd., UK) for 6 h at a temperature of 1400°C. The sintered specimens were then removed and placed into a stainless steel bowl and rapidly cooled using compressed air, thereby reducing the possible transformation of α-TCP to β-TCP. The cooled powder was subsequently ground using a planetary mill (Pulverisette 6, Frisch, Germany) for 5 min periods for a total of 30 min at 600 ± 5 RPM which produced an average D10 particle size of 1.07 ± 0.1 μm, D50 of 3.81 ± 0.5 μm and D90 of 11.03 ± 0.7 μm as measured by laser diffraction. The cement liquid used was an aqueous solution of Na2HPO4 in various weight percentages (BDH Laboratories Supplies, UK). The powder and liquid components were mixed for 1 min to produce a cement paste for a particular LPR, and a time of 4 min was designated for manual delivery into an appropriate mould.
2.2 Design of experiments
The DoE involved a two level factorial design using a ½ fractional factorial (Design-Expert V5 Software, Stat-Ease Inc, USA). The design included five factors: (Factor A) the wt% Na2HPO4; (Factor B) LPR; (Factor C) micro or nanosized HA; (Factor D) wt% HA and (Factor E) duration in Ringer’s solution prior to mechanical testing (Table 1). The DoE created a fractional factorial that produced 20 random experiments. The cement properties that were analysed are as follows: compressive strength, injection capabilities, setting times and the percentage content of CDHA. Each run was repeated three times for accuracy. The DoE method allows for statistical analysis using the Analysis of Variance method (ANOVA) whereby a P value < 0.05 is deemed a significant result.
2.3 Characterisation techniques
Compressive properties were measured in accordance with ISO 5833:2002. The cement paste was delivered into a PTFE mould, which formed 15 cylinders (height of 12 mm, Ø 6 mm). The mould was then placed in an oven (37°C) for 20 min and then immersed in Ringer’s solution (37°C) for either 3 or 7 days. The Ringer’s solution contained 6 g sodium chloride (NaCl), 0.33 g calcium chloride (CaCl) and 0.3 g potassium chloride (KCl) per litre of distilled water [2]. Compressive properties were determined using a EZ50 universal materials test system (Lloyds Instruments, UK) with a 5kN load cell at a rate of displacement of 1 mm min−1. All specimens were tested to failure to determine the compressive strength.
Post failure, the cement specimens were quenched in acetone to arrest further transformation to CDHA and crushed into powder form for analysis using a X-Pert Pro X-ray diffraction (XRD) system with an X’Celerator X-ray detector (Panalytical Ltd., UK). X’Pert High Score V 2.2b software (Panalytical Ltd., UK) was used to identify the phases present in the CDHA powder and their respective quantity.
The degree of injectability was measured using a 4 g batch of powder with the appropriate amount of the liquid phase. The cement paste was delivered into a proprietary syringe (Summit Medical Ltd., UK) and extruded after 1 min by applying a piston extrusion rate of 10 mm min−1 and a volumetric flow rate of 1,377 mm3 min−1 using an EZ50 universal testing machine (Lloyd Instrument Ltd., UK) until a maximum load of 100 N was achieved. The degree of injectability (I%) was then quantified (Eq. 3).
Initial (t i) and final (t f) setting times were determined in accordance with ASTM C266-99 using the Gillmore needle apparatus. The apparatus consisted of a weighted needle of 113.4 ± 0.5 g for measuring t i, and a weighted needle of 453.6 ± 0.5 g for testing t f. The powder batch (4 g) was delivered into three chambers (height of 12 mm, Ø6 mm) of a PTFE mould, which was stored at 37°C to represent the clinical environment. The t i and t f values were denoted as the time when the cement could bear the weight of the lighter and heavier needles without any appreciable indentation to the cement surface.
Laser diffraction (LD) was used to determine particle size and distribution of the different powder components. The powder was dispersed in ethanol and measurement was performed using a Sympatec HELOS/BF particle sizer (Sympatec GmbH Ltd., Germany). Each test required a reference scan of the liquid phase alone before the measurements stage could begin. Values of D10, D50 and D90 were recorded, which corresponded to the cumulative distribution at 10, 50 and 90% of the total powder distribution of particle sizes.
Scanning electron microscopy (SEM) (JEOL 6500 FEG SEM, Advanced MicroBeam Inc., USA) was used as a qualitative technique to determine the morphological and particle size of the HA powders. An acceleration voltage of 5 kV was used. All powders were mounted on aluminium discs and sputter coated with gold under vacuum to induce conductively.
3 Results and discussion
The DoE indicated that percentage content of CDHA as measured by XRD was not greatly influenced by any of the factors assessed in this study and, therefore, the effects graphs could not be determined. Analysis highlighted that all cements within the design matrix had a content of CDHA between 90 and 92%, indicating that all CPC’s had fully transformed from α-TCP to CDHA. The remaining phases mainly consisted of β-TCP (5–7%) which is to be expected from the processing technique used in this study to prepare α-TCP. The effects of the remaining factors that were found to be significant (as indicated by a contribution of greater than 10%) are shown in Figs. 1, 2, 3 and the overall contribution of said effects are indicated in Table 2. Results indicated that there were no strong interactions between the different factors which can affect the individual properties. All interactions had an overall contribution less then 10% and were deemed not to be significant.
The experimental results highlighted that the compressive strength was affected the greatest by the LPR, which contributed to 82% of the overall property contribution. Figure 1 shows how this factor affected compressive strength at the low and high levels (i.e. 0.35 and 0.5 mL/g). This result can be explained by the fact that the level of water within the cement has a direct effect on the level of porosity in the final set cement. A larger amount of water resulted in an increase in the porosity content of the cement and consequently, a material demonstrating poorer mechanical properties. Khairoun et al. [19] reported similar findings, they considered a LPR ranging from 0.30 to 0.40 mL/g using a comparable cement formulation. The present study also highlighted that Na2HPO4 exhibited no significant effect on the compressive strength. This finding is contrary to data documented by Ginebra et al. [13], who reported that 4 wt% Na2HPO4 significantly reduced the compressive strength from 59 to 34 MPa. The mechanism for the interaction of Na2HPO4 on the mechanical properties is an area of research that has not been greatly reported and requires further investigation.
With respect to injectability, the DoE results showed that LPR and wt% of Na2HPO4 had the greatest influence on how the CPC was injected. An increase in LPR resulted in the CPC exhibiting a lower viscosity (that is a higher injectability) and conversely a higher wt% Na2HPO4 led to the CPC being more difficult to inject from the syringe (Fig. 2). The overall contributions of the LPR and wt% of Na2HPO4 were 14 and 65%, respectively. It has been well reported that the ease of injection can be improved by modifying the LPR and this study confirmed this fact [11]. A knock-on effect of increasing the LPR is that the mechanical properties of the final CPC are compromised; therefore LPR is a factor that must be chosen with caution. In addition to this, the effect of Na2HPO4 on the injection capabilities was studied. The results demonstrated that increasing the loading of Na2HPO4 can reduce injectability of the CPC paste. This is not a surprising finding as the function of the Na2HPO4 is to act as an accelerant to the setting reaction of the CPC and, therefore, reduce the handling properties of the CPC within a set period. Such an effect was also highlighted by Khairoun et al. [19] where Na2HPO4 was used in concentrations of 2, 3 and 4% within the liquid phase of a CPC system. Injectability was measured as a function of the time and the results showed that maximum extrusion of cement occurred at lower time points for increasing amounts of Na2HPO4 and hence caused a reduction in the amount of cement extruded.
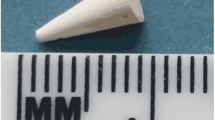
The LPR and wt% of Na2HPO4 had the greatest influence on the initial and final setting times (Table 2). Figure 3 shows the relationship between the LPR and wt% of Na2HPO4 and the final setting times, similar trends were also observed for the initial setting times. Increasing the LPR resulted in an increase in the setting times and conversely an increase in wt% Na2HPO4 showed an increase in the setting reaction of the CPC. The setting times currently being achieved for CPCs are too long for the application in minimally invasive surgery. Therefore, there has been a large drive towards finding techniques to reduce the setting reaction of CPC systems. A number of techniques have been proposed: for example the inclusion of a seed material [15, 16] and addition of an accelerator or reducing the LPR [11, 13, 14]. The addition of a seed alters the setting reaction by introducing crystals that will act as nucleating agents, thereby accelerating the initial stages of precipitation of CDHA crystal growth and hence decreasing the setting duration. In this study HA was used, which has been reported to function as a nucleating agent [15]. The results from the DoE demonstrate that incorporating HA to the CPC did not have a significant effect on the setting reaction. However, this result could be due to the low levels of HA, that is 0–3 wt%. Brown et al. [15] showed that incorporating 43 wt% HA reduced the final setting time from 22 to 8 min. In contrast, Ginebra et al. [20] found that using as low as 2 wt% HA reduced the setting time of an apatitic CPC from 54 to 13.5 min. Thus, there may be other factors governing how HA influences the setting reaction of the CPC, for example particle size, particle distribution, homogenous dispersion of the HA, etc. To address some of these questions, laser diffraction was carried out to determine the particle size of the microsized and nanosized HA powders. The micro HA powder exhibited a D10 1.35 ± 0.06 μm, D50 4.82 ± 0.23 μm and D90 8.98 ± 0.36 μm. The particle size range for the nanosized HA recorded the following values, D10 1.55 ± 0.07 μm, D50 6.56 ± 0.59 μm and D90 32.96 ± 0.42 μm, which did not correspond to the data sheets supplied by the manufacturer. The particle size distribution (Fig. 4) showed that both powders demonstrated a tri-modal profile. SEM analysis concurred with the laser diffraction data, showing that the nanosized HA had a greater propensity to agglomerate (Fig. 5). Particle agglomeration is due to a number of factors that include molecular, electrostatic and/or magnetic forces. Reducing the incidence of particle agglomeration is currently being investigated by many biomaterials research groups. For example, using appropriate techniques (ultrasonic disintegration) to homogenously disperse the particles within the solution [21] or by coating the nanoparticles with an emulsifying agent (for example, sodium dodecyl sulphate), thereby reducing the attraction forces between the particles [22]. With respect to how the LPR and NA2HPO4 influenced the setting properties of the CPC, similar observations were reported by Barone et al. and Ginebra et al. [14, 20].
The experimental data indicated that compressive strength was not affected significantly by the duration that the CPC was immersed in Ringer’s solution prior to testing. It is postulated that this finding could be because of the high (7 days) and low (3 days) time points chosen for the study. It has been reported that apatitic based CPC typically completes its reaction to CDHA within 24 h after mixing the powder and liquid components together [13]. Therefore, a future study needs to be conducted to evaluate the compression properties of the CPC when immersed in Ringer’s solution for time points up to 3 days to get a better understanding of the evolution from α-TCP to CDHA and the role HA plays in the setting reaction.
On completion and analysis of the DoE experiments cement composition and storage parameters were hypothesised that would facilitate a CPC demonstrating optimal compressive strength, injectability and setting characteristics (Table 3). It is important to state that there are certain requirements this cement was aiming to achieve, being: a final setting time no greater than 15 min, compressive strength no less than 30 MPa and injectability as close to 100% as possible [9, 10]. The optimal levels predicted by DoE were used to prepare the optimal CPC and subsequently validated (Table 4). The predicted values proposed by the DoE software and the actual values determined by experiments were different, for example the measured value for compressive strength was 31.5 ± 7.1 MPa and the DoE predicted value was 26 MPa. The DoE makes these predictions based on the main factor(s) affecting each property. Using the DoE approach a small deviation between the measured and the predicted results is expected as the results proposed by DoE do not take into consideration all the factors that individually are insignificant, but combined can result in a variation. The issue with attempting to produce optimal CPC is that the material properties are interrelated, therefore improving the compressive strength of the cement has a negative effect on the handling properties and vice versa. Even though this study provided a method to produce cement which may not yet derive an optimum injectable cement, this approach could be used for clinical techniques whereby the surgeon manually packs the cement into a bone cavity.
4 Conclusions
This investigation was conducted to obtain a better understanding of the factors that have the greatest effect on the mechanical and handling properties of apatitic CPC, thereby proposing a formulation of an optimal CPC that could be considered for vertebroplasty. The DoE methodology showed that LPR and the wt% Na2HPO4 had a significant influence on the properties of the CPC system whereas the addition of HA at ≤3 wt% did not. The optimal CPC proposed by the DoE methodology demonstrated a compressive strength within the clinical range acceptable for vertebroplasty; however, the initial and final setting time and injection capabilities did not meet these requirements. Therefore, further strategies need to be developed in order to improve the setting and handling properties of CPC before the cement can be considered as a suitable candidate for minimal invasive vertebroplasty.
References
Brown WE, Chow LC. A new calcium phosphate setting cement. J Dent Res. 1983;62:672.
Jack V, Buchanan FJ, Dunne NJ. Particle attrition of a-tricalcium phosphate: effect on mechanical, handling, and injectability properties of calcium phosphate cements. Proc Inst Mech Eng H. 2008;222(1):19–28.
Bohner M. Reactivity of calcium phosphate cements. J Mater Chem. 2007;17:3980–6.
Ginebra MP. Calcium phosphate bone cements. In: Deb S, editor. Orthopaedic bone cements. Cambridge: Woodhead Publishing Ltd; 2008. p. 206–230. ISBN 978-1-84569-376-3.
Bohner M. Calcium orthophosphates in medicine: from ceramics to calcium phosphate cements Calcium. Injury 2000;31(4):S-D37–47.
Friberg J, Fernández E, Sarda S, Nilsson M, Ginebra MP, Martínez S, et al. An experimental approach to the study of the rheology behaviour of synthetic bone calcium phosphate cements. Key Eng Mater. 2001;192–195:777–80.
Ambard AJ, Mueninghoff L. Calcium phosphate cement: review of mechanical and biological properties. J Prosthodont. 2006;15(5):321–8.
Verlann JJ, Cumhur Oner F, Dhert WJA. Anterior spinal column augmentation with injectable bone cements. Biomaterials. 2006;27(3):290–301.
Jansen J, Ooms E, Verdonschot N, Wolke J. Injectable calcium phosphate cement for bone repair and implant fixation. Orthop Clin N Am. 2005;36(1):89–95.
Lewis G. Injectable bone cements for use in vertebroplasty and kyphoplasty: state-of-the-art review. J Biomed Mater Res B. 2005;76B(2):456–68.
Bohner M, Baroud G. Injectability of calcium phosphate pastes. Biomaterials. 2005;26(13):1553–63.
Xu HHK, Simon CG. Fast setting calcium phosphate–chitosan scaffold: mechanical properties and biocompatibility. Biomaterials. 2005;26(12):1337–48.
Ginebra MP, Fernández E, Boltong MG, Planell JA, Bermúdez O, Driessens FCM. Compliance of a calcium phosphate cement with some short-term clinical requirements. Bioceramics. 1994;7:273–8.
Barone CM, Jimenez DF, Boschert MT, Beckert BW. BoneSource solidification: a comparison between water and sodium phosphate as the solvent. J Craniofac Surg. 2000;11(5):495–7.
Brown WE, Chow LC. Cements research progress. Westerville: American Ceramic Society; 1986. p. 351.
Lui C, Shen W. Effect of crystal seeding on the hydration of calcium phosphate cement. J Mater Sci. 1997;8(12):803–7.
Dorozhkin SV. Calcium orthophosphate cements and concretes. Materials. 2009;2(1):221–91.
Ginebra MP, Driessens FCM, Planell JA. Effect of the particle size on the micro and nanostructural features of a calcium phosphate cement: a kinetic analysis. Biomaterials. 2004;25(17):3453–62.
Khairoun I, Boltong MG, Driessens FCM, Planell JA. Some factors controlling the injectability of calcium phosphate bone cements. J Mater Sci. 1998;9(8):425–8.
Ginebra MP, Fernández E, Boltong MG, Bermúdez O, Planell JA, Driessens FCM. Compliance of an apatitic calcium phosphate cement with the short-term clinical requirements in bone surgery, orthopaedic and dentistry. Clin Mater. 1995;17:99–104.
Sato K, Li JG, Kamiya H, Ishigaki T. Ultrasonic dispersion of TiO2 nanoparticles in aqueous suspension. J Am Ceram Soc. 2008;91(8):2481–7.
Xiao F, Ye J, Wang Y, Rao P. Deagglomeration of HA during the precipitation synthesis. J Mater Sci. 2005;40(20):5442–93.
Acknowledgements
The authors would like to acknowledge the financial support provided by Engineering and Physical Sciences Research Council (EP/E022863/1).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Hara, R.M., Dunne, N.J., Orr, J.F. et al. Optimisation of the mechanical and handling properties of an injectable calcium phosphate cement. J Mater Sci: Mater Med 21, 2299–2305 (2010). https://doi.org/10.1007/s10856-009-3977-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-009-3977-9