Abstract
This study was performed to microscopically observe and measure inflammatory cytokine production by human macrophages phagocytosing submicron titanium (Ti) particles. Observations with secondary electron microscopy (SEM), SEM/electron probe microanalysis (EPMA) and transmission electron microscopy (TEM) indicated that macrophages [phorbol-12-myristate-13-acetate (PMA)-differentiated THP-1 cells] at 24 h in culture actively phagocytosed and accumulated submicron Ti particles in intracellular phagosomes, in which refinement of Ti particles occurred. The macrophages were also cultured for 24 h in four media with and without submicron Ti particles and lipopolysaccharide (LPS; components of bacteria). Whilst neither stimulus reduced cell viability, submicron Ti particles and LPS activation independently and synergistically caused the macrophages to produce three inflammatory cytokines (TNF-α, IL-1β and IL-6) at high levels in the culture supernatants. The inflammatory and osteolysis conditions caused by macrophages phagocytosing submicron Ti particles would be worsened by challenge with LPS in patients wearing Ti prostheses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Bulk titanium (Ti) is widely used as a prosthetic material for dental and medical applications (e.g., dental implant and bone–plate–screw assemblies) due to its good mechanical strength, corrosion resistance and biocompatibility [1]. The drawback of Ti is its weak resistance to wear and fretting [2]. Phagocytosis of submicron Ti wear particles from prostheses, which are smaller than the cell, cause macrophages to produce inflammatory and pro-osteoclastogenic cytokines, including TNF-α, IL-1β and IL-6, leading to inflammation, osteolysis and loosening of implants [3]. Gram-negative bacteria are also always present in the oral environment, and multiply considerably if oral care is neglected. The cell walls of these bacteria contain lipopolysaccharide (LPS), and activate macrophages by recognition of LPS and a subsequent cell signalling cascade to secrete these three cytokines [4], which leads to pathological conditions (e.g., periodontitis and osteoclastogenesis in dental patients) [5]. Patients who require dental implants are often over 50 years old [6] and are highly susceptible to bacterial LPS attack due to periodontitis. However, few comparative studies have been performed on the production of these cytokines by macrophages when stimulated by submicron Ti particles and/or soluble LPS alone or in combination [3].
The intracellular morphological changes of macrophages phagocytosing submicron Ti particles have not been examined in detail [3, 7]. In addition, the changes in submicron Ti particles themselves due to phagocytosis by macrophages have not been examined in depth [3].
The present study was performed to morphologically observe phagocytosis of submicron Ti particles by human macrophages [phorbol 12-myristate 13-acetate (PMA)-differentiated THP-1 cells] by optical microscopy, scanning electron microscopy (SEM), SEM/electron probe X-ray microanalysis (EPMA) and transmission electron microscopy (TEM), and to evaluate the production of three cytokines in these cells stimulated by submicron Ti particles and by LPS alone and in combination.
2 Materials and methods
2.1 Preparation of sub-micron Ti particles
Raw fine pure Ti particles less than 2 μm in size in water (purity = 95% minimum; Soekawa Chemicals, Tokyo, Japan) were sonicated, followed by natural setting of larger particles and collection of small particles in water. These powders in water were sterilised by autoclaving prior to mixing with the culture medium. Portions were then dried naturally on double carbon tape on aluminium stubs, and observed by SEM (S-4700; Hitachi, Ibaraki, Japan). The particle size distribution was checked with a laser diffraction/scattering particle-size analyser (Microtrac UPA150; Nikkiso, Tokyo, Japan).
2.2 Observation of human macrophages phagocytosing submicron Ti particles by optical microscopy, SEM, SEM/EMPA and TEM
The human monocytic cell line THP-1 (RCB 1189; Riken Cell Bank, Tsukuba, Japan) was cultured in RPMI1640 medium (Invitrogen, Carlsbad, CA, USA) supplemented with 10 vol.% foetal bovine serum (Cat. No. 10099-141; Invitrogen) and antibiotics (penicillin–streptomycin–amphotericin, Cat. No. 15240-096; Invitrogen) in an incubator under an atmosphere of 5% CO2/95% air at 37°C.
THP-1 cells (1 × 106) were differentiated into macrophages by culturing for 48 h in medium supplemented with 200 nM PMA [8] (Sigma-Aldrich Japan, Tokyo, Japan) (1 ml) in two single-chamber slide glasses (5700-001; Iwaki, Tokyo, Japan). The media were then exchanged with fresh media [i.e., control medium without PMA (Control) and medium with suspended Ti particles (0.5 wt%, 0.94 vol.%) (SM-Ti)], and culture was continued for an additional 24 h. The cells in one chamber slide glass were then washed twice with phosphate-buffered saline (PBS) (−) solution, infiltrated with n-butyl alcohol, freeze-dried and coated with osmium, followed by SEM observation. The cells in the other chamber slide glass were also washed twice with 2.5% glutaraldehyde/0.1 M PBS (−) solution, fixed in 1% OsO4/0.1 M PBS (−) solution, dehydrated through a graded alcohol series, infiltrated and cured with epoxy resin and sliced horizontally parallel to the chamber slide using a diamond blade. Sections 1 μm thick were stained with toluidine blue, and observed under an optical microscope (CK-30; Nikon, Tokyo, Japan). They were also analysed chemically by SEM/EPMA (JXA-8900L; JEOL, Tokyo, Japan). Sections 70 nm thick were observed morphologically by TEM (H-7100; Hitachi).
2.3 Measurements of cell viability and production of three inflammatory cytokines by human macrophages with and without submicron Ti particles and LPS
Human macrophages (PMA-differentiated THP-1 cells) (1 × 106) were also cultured in four media (1 ml) (four replicates, respectively), that is., control medium without PMA (Control), medium with suspended submicron Ti particles (SM-Ti), medium with LPS [LPS (+)] and medium with both submicron Ti particles and LPS [LPS (+) SM-Ti], in 24-well microplates (3020-024; Iwaki) for 24 h. For LPS stimulation, a commercial LPS (Escherichia coli O26; Difco, Detroit, MI, USA) was added to the culture media at a final concentration of 1 μg/ml. Cell viability was measured with a Cell-counting Kit 8 (Doujin-Chemical, Kumamoto, Japan) and a microplate reader (Model 680; Bio-Rad, Hercules, CA, USA) to determine whether phagocytosis of submicron Ti particles and LPS stimulation were cytotoxic to the macrophages examined. The cells were collected using cell scrapers, dissolved and homogenised in 1 wt% Triton X-100 containing PBS (−) solution and centrifuged; DNA contents in the supernatants were examined with a double-strand DNA assay kit (Quant-iT PicoGreen; Invitrogen) and a fluorometer (FP-6300; JASCO, Tokyo, Japan). The concentrations of the three cytokines (TNF-α, IL-1β and IL-6) in the culture supernatants were measured using ELISA kits (RPN5967, RPN5971 and RPN5968, respectively, Amersham Biotrak Easy ELISA; GE Healthcare, Piscataway, NJ, USA) according to the standard protocols. All cell culture measurements were carried out in four replicates with two repetitions (total number n = 4 × 2 = 8). The secreted levels of three inflammatory cytokines were normalised to the amounts of DNA. Statistical analysis was performed using StatView-J 5 (SAS Institute, Cary, NC, USA) with the unpaired t-test.
3 Results
3.1 Characterisation of Ti particles employed
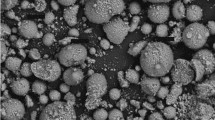
SEM micrographs (Fig. 1) indicated that the Ti particles added to the culture medium were irregular in shape and less than 1.0 μm in size. The laser particle size analyser confirmed that these particles had a mean size of 0.24 μm with standard deviation of 0.10 μm, whilst the minimum and maximum sizes were 0.04 μm and 1.64 μm, respectively (95% of particles <1.00 μm; 90% particles <0.50 μm) (Fig. 2). Therefore, the Ti particles used were judged to be in the submicron size range.
3.2 Observation of macrophages phagocytosing submicron Ti particles
Control macrophages tended to agglomerate and secrete extracellular matrix (ECM), as shown in the SEM image in Fig. 3a. In the presence of submicron Ti particles, macrophages showed marked changes in their morphological characteristics. The macrophages actively phagocytosed these particles by extending many projections outward with little production of extracellular matrix, as indicated in SEM micrographs (Fig. 3b). Whilst almost all of the Ti fine particles were eliminated around macrophages, leaving a zone labelled (−) SM-Ti in the figure, many Ti fine particles remained intact on the glass surface away from the macrophages, labelled as (+) SM-Ti (Fig. 3b). Optical microscopic observation of 1-μm sections of toluidine blue-stained macrophages phagocytosing submicron Ti particles indicated that particles accumulated and localised in some confined areas (Fig. 4). SEM/EPMA analysis of 1-μm sections of macrophages phagocytosing submicron Ti particles confirmed that these particles consisted of Ti (Fig. 5). In composite images, Ti particles appeared opaque white or black against the grey cell background (Fig. 5a). On EPMA, Ti appeared blue to red depending on the composition level according to the scale shown on the right-hand side of Fig. 5b.
TEM observations of 70-nm sections of macrophages indicated that phagocytosed submicron Ti particles were transferred to and collected within many intracellular phagosomes (Fig. 6a). The nuclei of the macrophages were free from inclusions of fine Ti particles (Fig. 6a). Considering the original size of the submicron Ti particles (Fig. 2), refinement of Ti particles down to <0.5 μm was universally observed (Fig. 6b) with phagocytosis by human macrophages in culture for 24 h. In two TEM images at the highest magnification (Fig. 7), the dense (residual) Ti particles (high contrast, black) was reduced to the order of 1–10 nm embedded in the larger grey ambiguous grain zones (low contrast). These zones were previously fully occupied by submicron Ti particles but became porous, indicating dissolution of submicron Ti particles in the phagosomes.
3.3 Cell viability
The cell viabilities of human macrophages cultured in four media [Control, SM-Ti, LPS (+) and LPS (+) SM-Ti] were essentially identical (Fig. 8) (P > 0.05), indicating that phagocytosis of submicron Ti particles and LPS stimulation were not cytotoxic to the macrophages examined.
Cell viabilities of human macrophages cultured for 24 h in four media: control medium (Control), medium with added submicron Ti particles (SM-Ti), medium stimulated with LPS [LPS (+)] and medium with submicron Ti particles and LPS [LPS (+) SM-Ti]. Data are expressed as mean values with standard deviation in parentheses of eight measurements (n = 8): Control, 1.17(0.04); SM-Ti, 1.14(0.10); LPS (+), 1.16(0.02); LPS (+) SM-Ti, 1.10(0.07). * Mean values of any two combinations were not significantly different at α = 0.05 level of significance (NS)
3.4 Inflammatory cytokine production
Control macrophages (Control) secreted the minimum amount of TNF-α (Fig. 9). The macrophages phagocytosing submicron Ti particles (SM-Ti) showed secretion of high levels of TNF-α (66-fold higher than the Control). The macrophages also produced high levels of TNF-α (48-fold higher than the Control) when stimulated by LPS [LPS (+)]. Dual stimulation with submicron Ti particles and LPS [LPS (+) SM-Ti] resulted in a further increase in the production of TNF-α (85-fold higher than the Control). Mean values of any two combinations were significantly different (P < 0.01).
TNF-α production by human macrophages cultured for 24 h in four media: control medium (Control), medium with added submicron Ti particles (SM-Ti), medium stimulated with LPS [LPS (+)] and medium with submicron Ti particles and LPS [LPS (+) SM-Ti]. Data are expressed as mean values with standard deviations in parentheses of eight measurements (n = 8): Control, 80.4(3.2); SM-Ti, 6215.5(404.7); LPS (+), 4966.3(666.0); LPS (+) SM-Ti, 8045.7(830.3) pg/DNA (μg). Mean values of any two combinations were significantly different (P < 0.01)
Control macrophages (Control) also showed the minimum amount of IL-1β (Fig. 10). The macrophages phagocytosing submicron Ti particles (SM-Ti) showed significantly enhanced production of IL-1β (47-fold higher than the Control). When stimulated with LPS, the amount of IL-1β produced by the macrophages [LPS (+)] was 5-fold greater than that of the Control. Dual stimulation with submicron Ti particles and LPS [LPS (+) SM-Ti] also resulted in a considerable increase in production of IL-1β to 101-fold higher than the Control. Mean values of any two combinations were significantly different (P < 0.01).
IL-1β production by human macrophages cultured for 24 h in four media: control medium (Control), medium with added submicron Ti particles (SM-Ti), medium stimulated with LPS [LPS (+)] and medium with submicron Ti particles and LPS [LPS (+) SM-Ti]. Data are expressed as mean values with standard deviations in parentheses of eight measurements (n = 8): Control, 16.8(4.8); SM-Ti, 918.0(64.9); LPS (+), 104.9(0.2); LPS (+) SM-Ti, 1996.7(208.3) pg/DNA (μg). Mean values of any two combinations were significantly different (P < 0.01)
Control macrophages (Control) did not produce IL-6 (Fig. 11). Macrophages phagocytosing submicron Ti particles (SM-Ti) showed moderate production of IL-6. When stimulated with LPS, the macrophages [LPS (+)] showed slightly higher levels of IL-6 production (19%) than SM-Ti. Dual stimulation with submicron Ti particles and LPS [LPS (+) SM-Ti] resulted in a significant increase in production of IL-6 to 2.8-fold greater than that of SM-Ti. Mean values of any two combinations were significantly different (P < 0.01).
IL-6 production by human macrophages cultured for 24 h in four media: control medium (Control), medium with added submicron Ti particles (SM-Ti), medium stimulated with LPS [LPS (+)] and medium with submicron Ti particles and LPS [LPS (+) SM-Ti]. Data are expressed as mean values with standard deviations in parentheses of eight measurements (n = 8): Control, 0(0); SM-Ti, 409.6(12.4); LPS (+), 487.9(23.2); LPS (+) SM-Ti, 1138.4(65.1) pg/DNA (μg). Mean values of any two combinations were significantly different (P < 0.01)
4 Discussion
The mechanism of transport of Ti particles into the macrophages from the surface into the interior with vigorous extension of the projections is not well understood (Fig. 3) [9]. The results in the present study indicated that submicron Ti particles were phagocytosed by macrophages and intracellularly localised in confined areas (i.e., phagosomes) as visualised by optical microscopy (Fig. 4), SEM/EPMA (Fig. 5) and TEM (Fig. 6). In addition, the sizes of most individual submicron Ti particles were refined to within the range of 1–10 nm after phagocytosis (Figs. 6, 7), although submicron Ti particles larger than 0.5 μm were present before phagocytosis (Figs. 1, 2). The refinement of submicron Ti particles in macrophages is not unexpected because Ti particles dissolve at acid pH, and the phagosome is a low-pH environment with the presence of active oxygen species (superoxide anion radicals) [10]. Ti particles were speculated as having been successively dissolved by H+ ions, superoxide and hydroxyl radicals, but were then instantaneously reconstituted to refined metallic Ti or titanium dioxides within and close to the phagosomes. Such refinement and chemical alteration may contribute to the exclusion of digested finer Ti particles from the body via the blood circulation through the liver, lung and spleen [11]. These findings, however, contradict those of a previous study by Xing et al. [12] suggesting that the shape and size of Ti particles remained unchanged in phagosomes whilst the surface chemistry was altered. The LPS-stimulated macrophages phagocytosed submicron Ti particles in a similar manner to the phagocytosis of LPS (−) macrophages reported here (SM-Ti) (data not shown).
PMA-differentiated THP-1 cells were utilised in this study as human macrophages because they are often used in the evaluation of particle-induced inflammation and osteolysis, especially in evaluations of failed artificial total hip joint replacements [7]. In orthopaedics, phagocytosis of wear debris is known to cause induction of inflammatory cytokine expression by macrophages (TNF-α, IL-1β and IL-6), provoking systematic symptoms, including osteolysis, around prostheses via osteoclastogenesis [3, 13]. The wear debris varies not only in composition (e.g., polyethylene, Ti, Ti–6Al–4V, Co–Cr alloy [14] and apatite) but also size (millimetre, submicron, nanometre [15]). Variations in the size and composition of wear debris may alter the phagocytosis activity of macrophages [16, 17]. Submicron Ti particles were evaluated in this study because Ti has been utilised in dentistry as a prosthetic metal in implants and oral surgery. In addition, the submicron size is less than half that of the macrophages, and the macrophages show very high phagocytotic activity against particles in this size range [18].
Recent Ti prostheses employ surface modification treatments, such as surface roughening [19], micropatterning [20] and rutile oxidisation [21]. All such treatments, however, appear to increase the frequency and amount of wear debris from Ti prostheses [22]. The adverse effects of submicron Ti particles on macrophages must therefore be clarified, considering the recent increase in usage of Ti prostheses. Retrieval analyses indicated transfer of Ti particles from dental Ti prostheses to the surrounding tissues [22, 23].
Our experimental results clearly indicated that submicron Ti particles themselves and LPS stimulation were not cytotoxic (Fig. 8), but that these two stimuli could independently increase the production levels of three inflammatory cytokines, whilst combined stimulation synergistically intensified the production of these cytokines (Figs. 9, 10, 11), leading to severe adverse tissue reactions such as inflammation and osteolysis [24]. The cell culture test is usually performed under clean conditions without LPS, but the actual oral environment contains many contaminants, including LPS. Therefore, considering the effects of bacterial contamination is important, especially because of the adverse effects of submicron Ti particles on the tissues surrounding both dental Ti implants and Ti bone–plate–screw assemblies set in the mandible and maxilla [23].
The macrophages were activated not only by LPS stimulation, but also by phagocytosis of submicron Ti particles. The former is derived from the cross talk between LPS and Toll-like receptor 4 (TLR4), resulting in production of three cytokines by activation of NF-κB, often defined as a Toll-like receptor signalling pathway [4, 25]. The latter appears to be due to oxidative stress (superoxide) occurring during phagocytosis of submicron Ti particles [26], followed by damage to the surface membrane lipid layers, activation of NF-κB [27] and production of three cytokines. However, the latter process has not been clarified in detail and should be evaluated in future studies. Although the two stimuli, phagocytosis of submicron Ti particles and LPS stimulation, have different entry points in their pathways, they share NF-κB, and are thereby capable of independently and synergistically increasing production of the three inflammatory cytokines. We confirmed the up-regulation of NF-κB genes by macrophages stimulated with submicron Ti particles and LPS by quantitative real-time PCR. QC (relative quantity) values for NF-κB genes of macrophages cultured for 6 h in control medium (Control), medium with submicron Ti particles (SM-Ti), medium with LPS [LPS (+)] and medium with both LPS and submicron Ti particles [LPS (+) SM-Ti] were 1.0, 2.0, 3.9 and 3.2, respectively [28], suggesting that both submicron Ti particles and LPS significantly up-regulated expression of NF-κB genes in the macrophages.
All three inflammatory cytokines, but especially IL-1β, are known to increase the number and accelerate the differentiation of osteoclasts [29], leading to periodontitis [5]. The reason why phagocytosis of submicron Ti particles produced higher levels of IL-1β than LPS stimulation is not clear, and further studies to address this question are needed. The production and release of IL-1β have been reported to be stimulated by either pathogen-associated molecular pattern molecules (PAMPs) or damage-associated molecular pattern molecules (DAMPs) [30]. LPS and phagocytosis of submicron Ti particles may be associated with PAMPs and DAMPs, respectively, and DAMPs may induce higher levels of IL-1β than PAMPs.
Further research into osteoclasts as well as macrophages exposed to submicron Ti particles are also required to both gain a better understanding and develop ways to avoid bone resorption around Ti prostheses. In clinical dentistry, studies have suggested that peri-implantitis may be caused by submicron Ti wear debris derived from Ti implants [22], and that the symptoms of periimplantitis would be worsened as a result of pathological reactions due to inflammatory cytokines produced by macrophages in cases with periodontitis. Therefore, the occlusal contact condition should be checked continuously in dental patients with Ti implants to minimise excessive contact and stress concentrations that cause and accelerate submicron Ti particle separation and to continuously check the oral hygiene conditions to minimise bacterial invasion with LPS around the implants. Similar risks have been reported in the use of endotoxin adherent/contaminated orthopaedic implants [31, 32]. Bone–plate–screw assemblies may also be susceptible to this endotoxin problem. Care should be taken to remove endotoxins when applying dental Ti implants and bone–plate–screw assemblies in clinical dentistry.
References
Fugazzotto PA, Vlassis J. Report of 1633 implants in 814 augmented sinus areas in function for up to 180 months. Implant Dent. 2007;16:369–78.
Cipriano CA, Issack PS, Beksac B, Della Valle AG, Sculco TP, Salvati EA. Metallosis after metal-on-polyethylene total hip arthroplasty. Am J Orthop. 2008;37:E18–25.
Vallés G, González-Melendi P, González-Carrasco JL, Saldaña L, Sánchez-Sabaté E, Munuera L, et al. Differential inflammatory macrophage response to rutile and titanium particles. Biomater. 2006;27:5199–211.
Zhou Q, Amar S. Identification of signaling pathways in macrophage exposed to Porphyromonas gingivalis or to its purified cell wall components. J Immunol. 2007;179:7777–90.
Rogers JE, Li F, Coatney DD, Rossa C, Bronson P, Krieder JM, et al. Actinobacillus actinomycetemcomitans lipopolysaccharide-mediated experimental bone loss model for aggressive periodontitis. J Periodontol. 2007;78:550–8.
Yerit KC, Posch M, Hainich S, Turhani D, Klug C, Wanschitz F, et al. Long-term implant survival in the grafted maxilla: results of a 12-year retrospective study. Clin Oral Implants Res. 2004;15:693–9.
Doorn PF, Campbell PA, Worrall J, Benya PD, McKellop HA, Amstutz HC. Metal wear particle characterization from metal on metal total hip replacements: transmission electron microscopy study of periprosthetic tissues and isolated particles. J Biomed Mater Res. 1998;42:103–11.
Baumann B, Seufert J, Jakob F, Nöth U, Rolf O, Eulert J, et al. Activation of NF-kappaB signalling and TNFalpha-expression in THP-1 macrophages by TiAlV- and polyethylene-wear particles. J Orthop Res. 2005;23:1241–8.
Tse SM, Furuya W, Gold E, Schreiber AD, Sandvig K, Inman RD, et al. Differential role of actin, clathrin, and dynamin in Fc gamma receptor-mediated endocytosis and phagocytosis. J Biol Chem. 2003;278:3331–8.
Amatore C, Arbault S, Bouton C, Coffi K, Drapier JC, Ghandour H, et al. Monitoring in real time with a microelectrode the release of reactive oxygen and nitrogen species by a single macrophage stimulated by its membrane mechanical depolarization. Chembiochem. 2006;7:653–61.
Olmedo D, Guglielmotti MB, Cabrini RL. An experimental study of the dissemination of titanium and zirconium in the body. J Mater Sci: Mater Med. 2002;13:793–6.
Xing Z, Schwab LP, Alley CF, Hasty KA, Smith RA. Titanium particles that have undergone phagocytosis by macrophages lose the ability to activate other macrophages. J Biomed Mater Res B Appl Biomater. 2008;85:37–41.
Tamaki Y, Sasaki K, Sasaki A, Takakubo Y, Hasegawa H, Ogino T, et al. Enhanced osteolytic potential of monocytes/macrophages derived from bone marrow after particle stimulation. J Biomed Mater Res B Appl Biomater. 2008;84:191–204.
Savarino L, Granchi D, Ciapetti G, Cenni E, Nardi Pantoli A, Rotini R, et al. Ion release in patients with metal-on-metal hip bearings in total joint replacement: a comparison with metal-on-polyethylene bearings. J Biomed Mater Res. 2002;63:467–74.
Tipper JL, Galvin AL, Williams S, McEwen HM, Stone MH, Ingham E, et al. Isolation and characterization of UHMWPE wear particles down to ten nanometers in size from in vitro hip and knee joint simulators. J Biomed Mater Res A. 2006;78:473–80.
Garrigues GE, Cho DR, Rubash HE, Goldring SR, Herndon JH, Shanbhag AS. Gene expression clustering using self-organizing maps: analysis of the macrophage response to particulate biomaterials. Biomater. 2005;26:2933–45.
Rakshit DS, Lim JT, Ly K, Ivashkiv LB, Nestor BJ, Sculco TP, et al. Involvement of complement receptor 3 (CR3) and scavenger receptor in macrophage responses to wear debris. J Orthop Res. 2006;24:2036–44.
Shanbhag AS, Jacobs JJ, Black J, Galante JO, Glant TT. Macrophage/particle interactions: effect of size, composition and surface area. J Biomed Mater Res. 1994;28:81–90.
Refai AK, Textor M, Brunette DM, Waterfield JD. Effect of titanium surface topography on macrophage activation and secretion of proinflammatory cytokines and chemokines. J Biomed Mater Res A. 2004;70:194–205.
Monsees TK, Barth K, Tippelt S, Heidel K, Gorbunov A, Pompe W, et al. Effects of different titanium alloys and nanosize surface patterning on adhesion, differentiation, and orientation of osteoblast-like cells. Cells Tissues Organs. 2005;180:81–95.
Rossi S, Tirri T, Paldan H, Kuntsi-Vaattovaara H, Tulamo R, Närhi T. Peri-implant tissue response to TiO2 surface modified implants. Clin Oral Implants Res. 2008;19:348–55.
Meyer U, Bühner M, Büchter A, Kruse-Lösler B, Stamm T, Wiesmann HP. Fast element mapping of titanium wear around implants of different surface structures. Clin Oral Implants Res. 2006;17:206–11.
Zaffe D, Bertoldi C, Consolo U. Element release from titanium devices used in oral and maxillofacial surgery. Biomater. 2003;24:1093–9.
Warashita H, Sakano S, Kitamura S, Yamauchi K, Yamaguchi J, Ishiguro N, et al. Biologocal reaction to alumina, zirconia, titanium and polyethelene particles implanted onto murine calvaria. Biomater. 2003;24:3655–61.
Lu YC, Yeh WC, Ohashi PS. LPS/TLR4 signal transduction pathway. Cytokine. 2008;42:145–51.
Soloviev A, Schwarz EM, Darowish M, O’Keefe RJ. Sphingomyelinase mediates macrophage activation by titanium particles independent of phagocytosis: a role for free radicals, NFkappaB, and TNFalpha. J Orthop Res. 2005;23:1258–65.
Akisue T, Bauer TW, Farver CF, Mochida Y. The effect of particle wear debris on NFkappaB activation and pro-inflammatory cytokine release in differentiated THP-1 cells. J Biomed Mater Res. 2002;59:507–15.
Taira M, Nezu T, Sasaki M, Kimura S, Kagiya T, Harada H, Narushima T, Araki Y. Gene expression analyses of human macrophage phagocytising sub-μ titanium particles by allergy DNA chip (GenopalTM). Bio-Med Mater Eng. 2009;19:63–70.
Kwan Tat S, Padrines M, Théoleyre S, Heymann D, Fortun Y. IL-6, RANKL, TNF-alpha/IL-1: interrelations in bone resorption pathophysiology. Cytokine Growth Factor Rev. 2004;15:49–60.
Eder C. Mechanisms of interleukin-1beta release. Immunobiology. 2009. doi:10.1016/j.imbio.2008.11.007.
Bi Y, Seabold JM, Kaar SG, Ragab AA, Goldberg VM, Anderson JM, et al. Adherent endotoxin on orthopedic wear particles stimulates cytokine production and osteoclast differentiation. J Bone Miner Res. 2001;16:2082–91.
Kim DH, Novak MT, Wilkins J, Kim M, Sawyer A, Reichert WM. Response of monocytes exposed to phagocytosable particles and discs of comparable surface roughness. Biomater. 2007;28:4231–9.
Acknowledgements
This study was supported in part by a Grant-in-Aid for the Open Research Project from 2007 to 2011, a Grant-in-Aid for the High-Tech Research Project from 2005 to 2009 from the Ministry of Education, Culture, Sports, Science and Technology, Japan, a Grant-in-Aid for Young Scientists (B) 21791830 and a Grant-in-Aid (B) 21390526 from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taira, M., Kagiya, T., Harada, H. et al. Microscopic observations and inflammatory cytokine productions of human macrophage phagocytising submicron titanium particles. J Mater Sci: Mater Med 21, 267–275 (2010). https://doi.org/10.1007/s10856-009-3834-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-009-3834-x