Abstract
In this study, a spray-coating method has been set up with the aim to control the coating of poly(2-hydroxy-ethyl-methacrylate) (pHEMA), an hydrophilic polymeric hydrogel, onto the complex surface of a 316L steel stent for percutaneous coronary intervention (PCI). By varying process parameters, tuneable thicknesses, from 5 to 20 μm, have been obtained with uniform and homogeneous surface without crack or bridges. Surface characteristics of pHEMA coating onto metal surface have been investigated through FTIR-ATR, contact angle measurement, SEM, EDS and AFM. Moreover, results from Single-Lap-Joint and Pull-Off adhesion tests as well as calorimetric analysis of glass transition temperature suggested that pHEMA deposition is firmly adhered on metallic surface. The pHEMA coating evaluation of roughness, wettability together with its morphological and chemical stability after three cycles of expansion-crimping along with preliminary results after 6 months demonstrates the suitability of the coating for surgical implantation of stent.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The adsorption of microbial related to infection and the crop up of thrombus are the two major complications affecting medical devices in contact with blood [1]. These responses to tissue damages, such as the healing event cascade, are always initiated by protein adsorption [2–4], platelet and leukocyte deposition at injury sites, followed by smooth muscle cell migration, proliferation, production of extra cellular matrix, and finally production of neointimal hyperplasia [5]. Therefore, it is important for the implant material to be inert, non-toxic and to possess low protein adsorption and cell adhesion properties [6]. To this end, hydrogels, thanks to their three-dimensional hydrophilic structures that are capable of absorbing a large amount of water [7, 8], may be excellent candidates for a tissue-implant intermediary. These swollen networks have been of considerable interest in biomaterials as well as drug delivery applications due to their mechanical behaviour similar to soft tissue and their special surface properties [9, 10].
Currently, synthetic polymeric hydrogels like poly(hydroxyethylmethacrylate) (pHEMA) and poly(hydroxyethylacrylate) (pHEA) are widely used as compliant materials particularly in the case of contact with blood or other biological fluids [11]. Moreover, pHEMA has been widely used in many biomedical applications [12], dating back to the work of Wichterle and Lim [13], because it is biologically inert, nonionic (suitable for blood contact), resistant to degradation, permeable to metabolites and non-absorbable [11–14].
The treatment of coronary artery disease, which remains the leading cause of mortality in the developed world, has undergone revolutionary changes in the past decade. This disease has been routinely treated with bare metal coronary artery stent implantation. However, stainless steel alloys are inherently thrombogenic which involve the possibility to incur in-stent restenosis and thus the need for repeated procedures limits the long-term benefit of coronary stents [15]. Intimal response to stents might be partially caused by allergic reaction to the metal ions, therefore many attempts to reduce neointimal proliferation following stenting procedure have focused on device coatings, with or without local drug delivery [16]. This has led to the development of drug-eluting stents (DESs), which have reduced the occurrence of major cardiac events from 16.4% with bare-metal stents to 7.8% with DESs [17]. Even though drug interdispersion within the coat of DESs has led to some clinical success, more recently thrombosis has emerged as a major clinical drawback consequence of a late endothelization [18]. In this frame, stent coating itself is an important factor for stent design, influencing both angiographic and clinical outcomes. Therefore, to efficiently engineer drug-eluting implants, an adherent, uniform, flexible coating is desirable; moreover, coating materials could be designed to increase the biocompatibility of the implant, to limit wall injury at the site of implant as well as to encapsulate drugs. However, in most cases polymers, non fully biocompatible, were selected as coating materials for stent strut [19]. Hydrophobic polymers were chosen principally because they firmly adhere to the stent surface and allow an homogeneous dispersion of the drug into the polymeric matrix [20, 21]; nevertheless, there is some concern that these polymers can contribute to an inflammatory response after drug release completion [22–24]. Moreover, the lack of coating surface uniformity may induce unpredictable healing patterns and thus affects procedural outcome.
To overcome limitation concerning hydrophobic polymers, hydrogel materials can be exploited because of their well established tissue compatibility [10]. Of particular interest for stent application are the results of previous studies, focused on hydrophilic polymer, highlighting that proteins preventing platelet deposition, as albumine, are absorbed on hydrophilic surface, resulting in a reduced occurrence of in-stent restenosis [25].
In this context, the use of a biocompatible polymeric hydrogel coat like pHEMA, capable to reduce injury to blood vessel at the site of stent implantation after swelling, might overcome the current issue affecting stent clinical outcome due essentially to tissue-device interface.
A critical issue arising in the clinical application is the high level of shear and tensile stresses that originates from stent deployment [26]. Despite their good flexibility in the swollen state, hydrogels usually lack of suitable mechanical properties [27] and this could greatly impair their use as coating materials for surgical procedure. Moreover, in case of inadequate adhesion between the hydrogel coating and the metal surfaces, a breakage at the coating-steel interfaces might occur [28].
The aim of this work was to fully investigate the ability of pHEMA coating to withstand surgical procedure in terms of interfacial adhesion to the steel substrate. An uniform, smooth and reproducible hydrogel layer with tuneable thickness was applied onto 316L stainless steel stents and the properties of the metal-polymer interface and the chemical stability were assessed.
2 Materials and methods
2.1 Materials
Poly(2-hydroxyethyl methacrylate) (pHEMA) having an average molecular weight (Mv) of 20,000 Da was supplied by Aldrich. Ethanol, used as polymer solvent, was purchased from Fluka. MULTI-LINK PIXEL 316L Stainless Steel (SS) stent, currently implemented in clinical applications, was kindly supplied by Guidant (California, USA). Plates of 316L SS characterized by 0.5-mm-thickness were obtained from L.f.g.m. Inox S.r.l. (Italy).
2.2 Preparation of hydrogel coating: spray-coating technique
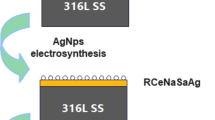
Thin hydrogel coating have been realized by an air sprayer on a stent mounted on a rotating system. The spray coating technique is based on the nebulisation of a coating polymer solution (Fig. 1). The air stream flows by means of an air compressor (A) through the nozzle (B) of a dual action, internal mix airbrush (Budger 100) (C) aspirating and entraining the polymer solution contained in the cup (D). An optimum flow rate of polymeric solution at the spray nozzle outflow (6 ml/min) and distance between stent and nozzle (~60 cm) were kept constant. The optimum has been obtained varying the flow rate and analysing the resulting coating. A flow rate lower than 6 ml/min results in a spotted coat whereas a higher one results in a layer too thin or, in the case of exaggerate flow rate, in a complete absence of pHEMA coating. Stent film deposition has been achieved by spraying a solution of pHEMA and ethanol (10% w/v) onto stent (F) rotating on its axis by means of a motorized stage system PC-controlled (ProScan, Prior) (E) keeping a constant velocity using a computerized software (Microsoft© HyperTerminal), and by following solvent evaporation under different controlled conditions (Fig. 1). To optimise the uniformity of coating thickness, process parameters as rotation speed, nebulisation time and solvent evaporation conditions were surveyed (Table 1).
Schematic layout of spray-coating technology system. pHEMA/ethanol solution (d) has been nebulised by means of an air compressor (a) through the nozzle (b) of an airbrush (c) onto a stent (f). A motorized stage system PC-controlled (e) keeps the stent rotate on its axis during polymeric nebulisation
Different rotation speed (3–12 rpm) and time of nebulisation (up to 40 s, at 6 rpm) were used to study the influence of process conditions on coating thickness. After nebulisation, samples have been kept at different controlled conditions to allow uniform solvent evaporation (Table 1). In particular, the stent, held by grips, has been dried in a clean room or in a laminar flow hood (Mars, Celbio).
3 Methods
3.1 Surface morphology and topography
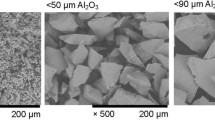
The surface morphology of spray-coated stent was examined by scanning electron microscope (SEM) (LEIKA S400) equipped for analysis in dispersion of energy (EDS) (EDAX, Oxford mod. INCA 200). In particular, the samples were mounted onto metal stubs using double sided adhesive tape and then coated with gold–palladium under an argon atmosphere.
Moreover, the topography of the coated surfaces was determined by atomic force microscopy (AFM) in order to compare roughness of pHEMA-coated and bare 316L steel surfaces. This technique involves moving a sensitive stylus over the stent’s surface and measuring the vertical height changes. The technique yielded parameters of R a , R q which equations are
where L is the evaluation length, and r(x) is the profile height function [29].
In particular, the R a value is the arithmetic average, while the R q value the geometric average, of the distances from the surface to a centre reference line. Samples were analyzed at room temperature and 40% of humidity in tapping mode using a Digital Instrument Nanoscope 3A by scanning a square window of 4 × 4 μm2 on each sample.
3.2 Surface wettability
The sessile method of contact angle measurement was performed by a Data Physics (model OCA 20) equipped with a video CCD-camera and SCA 20 software. Static contact angles were measured by placing a water droplet (3 μl) onto the coated and uncoated sample surface at a dispensing speed of 1 μl/min. The angle was measured within 4 s of water contact with the sample. A minimum of 10 samples were considered for any measurement.
3.3 Surface chemical characterization
The structural and molecular composition of the thin pHEMA coating was investigated by fourier transform infrared spectroscopy (FTIR). FTIR transmittance spectra were recorded in the 500–4000 cm−1 by a Nexus FT-IR spectrometer using a single reflection attenuated total reflectance (ATR) accessory with a resolution of 4 cm−1 and 20 scans. The tests were carried out on the coatings after solvent evaporation. Results are an average of at least five samples.
3.4 Adhesion tests
To investigate hydrogel–steel interface, 316L stainless steel sheets have been coated and tested according to the standard method of Single-Lap-Joint (S-L-J) and Pull Off (P-O) (ASTM: D 1002–05) using a microtest specimens (Fig. 2).
The tested 316L stainless sheet samples were cleaned ultrasonically with ethanol and acetone in sequence for 15 min. A 10 wt% solution of pHEMA was prepared by dissolving it in ethanol. Then the solution was used to cast, within a frame made up of silicon mould, thin polymer films onto 316L sheet samples, then hydrogel surface was attached to the other 316L SS sheet using cyano-acrylate glue. The 50 μm thickness coatings (measured by a micrometer Mitutoyo Digimatic Micrometer, Serie 293, Japan) ensure that glue does not penetrate into the coating up to the interface of interest.
Two different loading conditions were tested in both dry and swollen pHEMA state to fully determine the resistance of hydrogel–steel interface: condition (A) related to a shear stress while (B) is related to the tensile stress, both present during stent deployment.
A dynamometer (Instron 4204), to which the strip was attached by a grip, was used to calculate the failing load and displacement of the interfaces. For the swollen state, specimens have been kept in PBS solution prior to the test to allow the complete hydration of the coating. The tests were performed with a 1 kN load cell and a cross-bar speed of 1.3 mm/min. The load measured at the moment of detachment was divided by the adhesion overlap surface between metal and polymer film, related to specimens (A) and (B), in order to obtain respectively the shear and tensile stress value.
Furthermore, in both S-L-J and P-O tests, analysis in dispersion of energy (EDAX, Oxford mod. INCA 200) using scanner electron microscope (SEM, Leica 420) has been performed throughout the fractured surface in order to investigate the mechanism governing the breakage and in particular whether the failure occurred at one or both the interfaces present (pHEMA/steel and pHEMA/glue/steel) or within the pHEMA coating.
3.5 Calorimetric analysis
The effect of interfacial residual stress on the glass transition temperatures of pHEMA film was measured by TA Instrument DSC 2910. The polymer films were prepared by two different methods. pHEMA/ethanol solution was cast either onto 316L or on teflon sheet. Both pHEMA films were tested in crimped aluminium pans at a heating rate of 10°C/min under dry N2 gas over a temperature ranging from room temperature to 180°C. The glass transition temperature (Tg) was determined as the average of at least three separate measurements from the TA Universal analysis software.
3.6 In vitro stability of pHEMA/steel interface
Three cycles of expansion-crimping were performed after hydrogel deposition onto stent surface and following solvent evaporation to assess the stability of interface to solicitations comparable with those occurring during surgical procedures.
Afterwards, in order to study and verify the long-term stability of the coating we tested the device in wet environment. Briefly, after nebulisation and solvent evaporation, hydrogel-coated stents were immersed in 3 ml of PBS solution and kept at room temperature. Due to the small dimension of stent used in this study, the amount of PBS used was enough to ensure that test was conduct in sink condition. After 6-months PBS incubation the pHEMA/steel systems were extensively washed and investigated by analysis in dispersion of energy to check out the chemical compounds present on the surface.
4 Results
4.1 Surface morphology and topography
When drying was performed in the clean room, the pHEMA spray-coated stents were characterized by a very smooth and uniform surface, with no cracks observed between struts and an inner and outer homogeneous surface appearance (Fig. 3).
Measurements of the coating thickness were taken by the means of SEM after cracking the pHEMA surface. Analysis was performed at different locations all along the stent surface, carefully choosing point of interest situated in the internal, external and radial surface of the polymeric coating. For each measurement, the thickness has been calculated using the SEM software resulting in a constant value in all the investigated locations.
Solvent evaporation conditions strongly influenced the surface coating. Briefly, stent coated under laminar flow hood resulted in a non-uniform surface, with cracks along the stent length (data not shown). These differences in coating appearance are principally related to the velocity of solvent evaporation. In the laminar flow hood, the evaporation was faster with respect to that achieved in clean room. Moreover, the presence of the laminar flow strongly alters the condition of evaporation along the stent length. All these parameters are the cause of the crack formation on the coating.
Processing conditions strongly influenced the thickness of the coating. In particular, the coating thickness ranged from 5 to 20 μm depending on the process parameters chosen (i.e. rotation speed, time of nebulisation) (Fig. 4).
Coating thickness achieved allowing one complete rotation of the stent on its axis during polymeric nebulisation decreases with increasing rotation speed, ranging from 18 to 5 μm for 3 and 12 rpm (Fig. 4a). An opposite trend was observed as function of nebulisation time, at constant rotation speed of 6 rpm. Moving from 10 up to 40 s, coating thickness increases from 10 to 23 μm (Fig. 4b). These thickness values are expressed as a mean value of at least three different stents coated using the same parameters, assuring the high reproducibility of the proposed technique.
Tapping mode AFM images of the surface of pHEMA-coated stent showed (Fig. 5) that the surface was very smooth, with an average roughness, of R a and R q , of about 0.2 nm, if compared to uncoated samples (R a ~ 1 nm; R q ~ 1.3 nm).
4.2 Surface wettability
By coating the 316L steel with a thin hydrogel layer the contact angle was reduced from 73° (for uncoated sample) to 32° for pHEMA-coated samples (Fig. 6).
Reduction in contact angle data for pHEMA-coated stents, compared with uncoated stents, was representative of increased wettability of the device, highlighting the strong hydrophilic nature of pHEMA hydrogel.
4.3 Surface chemistry
The presence of pHEMA layer on surface samples has been investigated immediately after coating by FTIR-ATR spectra. The ATR spectra (Fig. 7) showed the characteristic alcoholic (O–H) peaks of the pHEMA at 3,445 cm−1 for the stretching O–H and 1,022 cm−1 for the bending O–H [30]. Furthermore, ester groups were identified by peaks at 1,728 cm−1 (C=O stretching) and at 1,275 cm−1 (C–O stretching).
4.4 Adhesion properties
Adhesion tests have been performed according to the Standard Method ASTM D 1002–05 for Single-Lap-Joint and Pull-Off in order to test polymer–metal interfaces by imposing both shear and tensile stresses. Both tests have been carried out using steel plates on which a thin layer of pHEMA was adhered, and the hydrogel have been tested in its dry as well as wet state.
4.4.1 Single-Lap-Joint test
The specimens withstood a displacement of 0.06 mm for dry sample and 0.09 mm for swollen hydrogel until fracture, resulting in a more plastic behaviour for the swollen hydrogel state as expected (Fig. 8a). The load at failure was very similar in both conditions, consequently the maximum shear stress obtained for dry and wet samples, 0.25 and 0.24 MPa respectively, was comparable.
4.4.2 Pull-Off test
No significant differences in displacement at failure were observed for dry and wet samples, (respectively 0.05 and 0.06 mm) (Fig. 8b). However, a great difference in the maximum load (0.4 kN for dry samples to 0.1 kN for swollen hydrogels) and in maximum strengths (0.9 MPa for dry and 0.4 MPa for wet samples) were observed.
Each fractured surface after adhesion tests was studied by electron microscopy in order to observe the locus of failure. Failures were predominantly interfacial, occurring primarily at the stainless steel–pHEMA interface, whereas few zones of cohesive failure within the polymer layer were observed (Fig. 9).
This was demonstrated by EDS analysis performed on both typical phases present after fracture. A number of 10 scansions have been performed on both side of the tested plates and a representative EDS spectrum is reported in Table 2. Moreover, no trace of glue penetrating up to the hydrogel–steel interface was detected.
EDS analysis was also preformed on cross section of the coating layer upon deposition of glue and without the imposition of the plate, at the level of pHEMA/glue interface. The glue penetration in depth at the cross section attained scarcely 500 nm (data not shown).
4.5 Calorimetric analysis
A study on the interfacial stress arising from solvent evaporation within the pHEMA has been carried out. It is well documented in the literature that glass transition temperature of polymers may be affected by the presence of residual stresses [31]. In particular, residual stresses include two contributions: interfacial residual and matrix residual stresses. In our case, matrix residual stresses are due to solvent evaporation during pHEMA deposition, whilst interfacial residual stresses arise from the adhesion between pHEMA and steel surfaces.
In order to evaluate the interfacial adhesion, two different kinds of samples were designed to obtain, after solvent evaporation, a layer with both interfacial and matrix residual stresses when adhered to steel surface (A) and one with matrix stresses alone when cast on Teflon substrate (B) (Teflon-pHEMA representing a “not adhesive” interface).
Characteristic Tg for pHEMA obtained from Sigma is around 83°C. Interestingly, we found a Tg of 79°C in the case of sample (B) and a further depression of Tg (64°C) in samples (A). The decrease Tg in the case of sample B is reasonably due to stress arising from solvent evaporation, while it is reasonable to assume that the additional effect of interfacial residual stresses (which are present in A and absent in B) are responsible for the further Tg depression. Such finding suggests that the solvent evaporation affects the internal stress of polymeric film, and, more importantly, the further decrease of Tg for samples A confirms the adhesive properties of pHEMA on 316L steel after solvent evaporation.
4.6 In vitro stability of pHEMA/steel interface
SEM of coated stent after solvent evaporation and after three cycles of expansion-crimping and 6-months immersion in PBS solution showed that the pHEMA layer was still present on the metallic surface (Fig. 10). EDS analysis, indeed, reported in Table 3, showed the presence of carbon (C) and oxygen (O) at the pHEMA stoichiometric ratio.
5 Discussion
The purpose of this work consisted in the design, realization and characterization of a novel stent coating made up of a hydrophilic material, such as a hydrogel. The material becomes softer after swelling due to a biological fluid uptake, thus preventing tissue injury during surgical procedure.
In particular, we realized a pHEMA layer on 316L stainless steel stent by a spray technique and then the adhesion and stability of pHEMA/steel interface were assessed for the obtained coating.
Indeed, we firstly focused on the set up of a reliable and easy to produce spray-coating technique to obtain a controlled homogeneous and uniform layer of polymeric hydrogel onto the complex metallic surfaces. Briefly, the technique consists in the atomization of a polymeric hydrogel solution on the stent, when rotating on its axis at controlled rotation speed. Process parameters have been optimised in order to obtain different thicknesses of the coating compatible with the proposed applications. Such advantage, together with the easy principle and the cheap raw materials utilized, make this technique low-cost, easy and versatile.
Recent advances in stent technology also suggest that stents can be successfully deployed in small diameter blood vessels of <3 mm [32]. Therefore, the control of coating thickness with the resolution of few microns becomes fundamental in modern coating technologies. By our approach, optimizing process parameters, such as rotation speed and time of solution atomization, it is possible to obtain tuneable coating thickness with control over a dimensional range, spanning from 5 to 20 μm. Moreover, since the technique enables stent struts to be surrounded by an uniform coating (Fig. 3), it is reasonable to assume that the device will help to reduce blood flow instability through the lumen and enhance the anchorage of the stent to the duct wall. Furthermore, since the polymer coating did not significantly increase the calibre of the stent, it did not necessitate a larger introducer. This fact guarantees, in addition to manageability, reasonable margins of safety and tolerability for the patient.
The homogeneous and uniform surfaces’ appearance can be attributed to the rotating motion of the stent on its axis allowing for the nebulised droplets to access the entire (inner, outer and lateral) surface of the struts. Furthermore the coating’s thickness can be finely tailored to better fit the needs of a specific application. As an example, for DES, a coating of about 5 μm would not allow to carry a high amount of the drug of interest, whereas a 20 μm coating should be capable to retain and deliver high dose of drug, compatible with the therapeutic approaches without obstructing stent mesh.
For coating stent applications, it is well known that either rupture or cracks could induce fast restenosis while uneven surface structures could represent a major cause of thrombogenic events. If the stent has webbings and bridges between the struts, the coating may break off from the stent when the stent is dilated by a balloon catheter during the deployment, and thrombus and vascular smooth muscle cells (VSMCs) proliferation can occur at the site where the coating breaks off [33].
In our case, hydrophilic pHEMA layer on metallic stent surface has been clearly visualized by SEM showing a very uniform and smooth surface with no cracks or webbings between struts. Furthermore, surface topography is considered to have a crucial influence on stent performance in fact, overcoming the natural roughness of bare metal stent was one of the first reasons to coat metal stents with polymers [34].
For cardiovascular application, indeed, a smooth surface coating of devices can significantly decrease injury to blood vessels. In addition, surface roughness is often correlated to cell adhesion and migration and in particular to human endothelial cells growth [35, 36]. Furthermore, a smooth stent surface is believed to reduce platelet activation and aggregation, consequently leading to less thrombus formation and neointimal proliferation [37]. The developed coating stent showed a reduced surface roughness when compared to bare metal stents, even in dry conditions, that could lead to less vascular injury at the moment of angioplasty procedures.
Severe stresses are imposed to stent device, and therefore to coating materials, during both surgical procedure and normal working conditions. High level of deformation in devices made up of different materials, as in the case of coated stent (coating layer and stent bulk), could cause the breakage of the system at the interface between the different materials. Therefore, since cardiovascular devices are constantly in direct contact with blood working in pulsatile shear stress conditions, adhesion between the metal backbone and the polymeric coating is very demanding, thus being a crucial feature for a coating to be successful in such application. If the adhesion is not sufficiently strong, the coating might be unable to withstand clinical procedure leading to cracks at the bottom of as well as within the coating or, even worst, degradation products of polymer coating could detach from the metallic substrate to enter the bloodstream.
Mechanical interlocking and chemical bonding occurring at interface between pHEMA and steel have been investigated by considering standard adhesion tests (ASTM D 1002-05) on steel plates and by evaluating physical properties, such as Tg, after coating.
pHEMA coating demonstrated good adhesion on metal plates when tested both in shear and tensile conditions. Data of shear stress were found comparable with those obtained for polycarbonate urethane and polyether urethane coated on steel stent (Gianturco-Rosch stent) [38] widely used in clinical practice, with even higher tensile stress at failure.
There are several reasons why the pHEMA deposited onto 316L steel shows such interface adhesion properties. Since the adhered layer of pHEMA represents a soft material when compared to steel and steel roughness is quite low (R a about 1 nm) the good mechanical stability of interface results mainly from the strong chemical bonds established between pHEMA and metal substrate enabling any adhesion mechanism across this interface to act more effectively. These considerations could explain the high value of stress at failure as high as 0.40 and 0.24 MPa, respectively, in tensile and shear conditions in adhesion tests. Evaluated strengths thus represent the stress values that pHEMA–metal interface could withstand in different conditions before interfacial fracture. The good interfacial adhesion is also confirmed by Tg depression reported for pHEMA coated on stainless steel (sample A). It is worthy to notice that other procedures reported in literature evaluate the coating adhesion in comparative manner or determining adhesion values, like Ga in the case of blister test, unable to be used in differing operative conditions [39]. The proposed procedure allow to calculate adhesion strength both in tensile and in shear stress conditions that can be also used for mathematical modelling or different loading conditions (vessel recoil, shear stress at wall or different stent shape).
Moreover, the proposed polymeric coating has been investigated in order to study its stability on steel stent after three cycles of expansion-crimping and following contact with biological solutions. SEM images confirm that the proposed pHEMA coating is capable to withstand mechanical solicitations arisen from surgical implantation. Moreover, as highlighted by EDS analysis, oxygen and carbon are still present at the stoichiometric ratio of pHEMA onto the steel surface after 6-month incubation in PBS solution.
To conclude, such a device with a stable smooth hydrophilic shell could be designed, in term of thickness, according to a desired application. Moreover, pHEMA coating can be further modified with insertion of selected peptides on its surface able to elicit adhesion of selected cells [40] and then to promote the endothelialisation of struts exposed to blood stream.
6 Conclusions
A new technique to obtain a pHEMA coating was set-up by spraying in a controlled fashion, pHEMA solutions on complex shaped solid surfaces. The proposed reproducible and easy to perform technique allows to fabricate uniform in roughness (with a value of R a of about 0.2 nm), and controlled in thickness (with thickness ranging from 5 to 20 μm) coating on the overall 316L steel stent surface without cracks or bridges.
As a result, pHEMA coating showed a good and stable interfacial adhesion with the ability to withstand high shear and tensile stresses (respectively S-L-J and P-O) as demonstrated by mechanical tests in both dry and wet conditions. The interfacial adhesion was further confirmed by suppression of glass transition temperature of pHEMA after solvent evaporation, when deposited on steel surface. Moreover, the morphological and chemical stability of the pHEMA–steel interface was verified after simulation of working conditions occurring during the surgical procedure of stent implantation and after 6-months incubation in PBS.
References
M.C. Martins, D. Wang, J. Ji, L. Feng, M.A. Barbosa, Albumin and fibrinogen adsorption on PU–PHEMA surfaces. Biomaterials 24, 2067–2076 (2003). doi:10.1016/S0142-9612(03)00002-4
B.D. Ratner, A.S. Hoffman, F.J. Schoen, J.L. Lemons, Biomaterials science—An introduction to materials in medicine (Academic Press, CA, USA, San Diego, 1996), pp. 84–94
R.S. Greco, Implantation biology, the host response and biomedical devices. Ann Arbour (CRC Press, USA, 1994), pp. 68–80
S. Sapatnekar, J.M. Anderson, Hemocompatibility: effects on humoral elements. In: von Recum AF, editor. Handbook of biomaterials evaluation, Scientific technical and clinical testing of implant materials (Taylor & Francis, Philadelphia, PA, USA, 1999), pp. 353–365
F.G. Welt, C. Rogers, Inflammation and restenosis in the stent era. Arterioscler. Thromb. Vasc. Biol. 22, 1769–1776 (2002). doi:10.1161/01.ATV.0000037100.44766.5B
D.J. Mooney, R.S. Langer, Engineering biomaterials for tissue engineering: the 10–100 micron size scale, in The biomedical engineering handbook, ed. by J.D. Bronzino (CRC Press, Boca Raton, FL, 1995), pp. 1609–1618
D.H. Kim, M. Abidian, D.C. Martin, Conducting polymers grown in hydrogel scaffolds coated on neural prosthetic devices. J. Biomed. Mater. Res. 71A, 577–585 (2004). doi:10.1002/jbm.a.30124
K.S. Anseth, A.T. Metters, S.J. Bryant, P.J. Martens, J.H. Elisseeff, C.N. Bowman, In situ forming degradable networks and their application in tissue engineering and drug delivery. J. Control. Release 78, 199–209 (2002). doi:10.1016/S0168-3659(01)00500-4
T.D. Dziubla, M.C. Torjman, J.I. Joseph, M. Murphy-Tatum, A.M. Lowman, Evaluation of porous networks of poly(2-hydroxyethyl methacrylate) as interfacial drug delivery devices. Biomaterials 22, 2893–2899 (2001). doi:10.1016/S0142-9612(01)00035-7
B. Baroli, Photopolymerization of biomaterials: issues and potentialities in drug delivery, tissue engineering, and cell encapsulation applications. J. Chem. Technol. Biotechnol. 81, 491–499 (2006). doi:10.1002/jctb.1468
A.J. Cadotte, T.B. DeMarse, Poly-HEMA as a drug delivery device for in vitro neural networks on micro-electrode arrays. J. Neural Eng. 2, 114–122 (2005). doi:10.1088/1741-2560/2/4/007
J.P. Montheard, M. Chatzopoulos, D. Chappard, 2-Hydroxyethylmethacrylate (HEMA): chemical properties and applications in biomedical fields. JMS-Rev. Macromol. Chem. Phys. C32, 1–34 (1992)
O. Wichterle, D. Lim, Hydrophilic gels in biologic use. Nature 185, 117–118 (1960)
A.S. Hoffman, Hydrogels for biomedical applications. Adv. Drug Deliv. Rev. 43, 3–12 (2002). doi:10.1016/S0169-409X(01)00239-3
A. Abizaid, M.A. Costa, M. Centemero et al., Clinical and economic impact of diabetesmellitus on percutaneous and surgical treatment ofmultivessel coronary disease patients: insights from the arterial revascularization therapy study (ARTS) trial. Circulation 104, 533–538 (2001). doi:10.1161/hc3101.093700
A. Schuesseler, et al. Manufacturing of stents: optimize the stent with new manufacturing technologies, In: New technologies in vascular biomaterials: fundamentals about stent II, ed. by N. Chakfè, B. Durand, J-G Kretz (EUROPROT, Strasbourg, France, 2007), pp. 93–106
M.N. Babapulle, L. Joseph, P. Belisle, J.M. Brophy, M.J. Eisenberg, A hierarchical bayesian meta-analysis of randomised clinical trials of drug-eluting stents. Lancet 364, 583–591 (2004). doi:10.1016/S0140-6736(04)16850-5
G. Sandhu, B. Doyle, R. Singh, M. Bell, J. Bresnahan, V. Mathew, D. Holmes, A. Lerman, C. Rihal, Frequency, etiology, treatment, and outcomes of drug-eluting stent thrombosis during one year of follow-up. Am. J. Cardiol. 99(4), 465–469 (2007). doi:10.1016/j.amjcard.2006.08.058
Y. Nakayama, T. Masuda, Development of a polymeric matrix metalloproteinase inhibitor as a bioactive stent coating material for prevention of restenosis. J. Biomed. Mater. Res. B Appl. Biomater. 80B, 260–267 (2007). doi:10.1002/jbm.b.30592
C.D. Rogers, Optimal stent design for drug delivery. Rev. Cardiovasc. Med. 5(Suppl 2), S9–S15 (2004). doi:10.1016/j.carrad.2004.04.002
S.V. Ranade, K.M. Miller, R.E. Richard, A.K. Chan, M.J. Allen, M.N. Helmus, Physical characterization of controlled release of paclitaxel from the TAXUS Express2 drug-eluting stent. J. Biomed. Mater. Res. A 71, 625–634 (2004). doi:10.1002/jbm.a.30188
R. Virmani, A. Farb, G. Guagliumi, F.D. Kolodgie, Drug-eluting stents: caution and concerns for long-term outcome. Coron. Artery Dis. 15, 313–318 (2004). doi:10.1097/00019501-200409000-00003
N. Kipshidze, M.B. Leon, M. Tsapenko, R. Falotico, G.A. Kopia, J. Moses, Update on sirolimus drug-eluting stents. Curr. Pharm. Des. 10, 337–348 (2004). doi:10.2174/1381612043453315
L. Buellesfeld. Second generation drug-eluting stents. Clinical experience with new drugs and designs, In: New technologies in vascular biomaterials: fundamentals about stent II, ed. by N. Chakfè, B. Durand, J-G Kretz (EUROPROT, Strasbourg, France, 2007), pp. 161–168
J.L. West, J.A. Hubbell, Separation of the arterial wall from blood contact using hydrogel barriers reduces intimal thickening after balloon injury in the rat: the role of medial and luminal factors in arterial healing. Proc. Natl Acad. Sci. USA 93, 13188–13193 (1996). doi:10.1073/pnas.93.23.13188
C. Dumoulin, B. Cochelin, Mechanical behaviour modelling of balloon-expandable stents. J. Biomech. 33, 1461–1470 (2000). doi:10.1016/S0021-9290(00)00098-1
D. Darwis et al., Characterization of poly(vinyl alcohol) hydrogel for prosthetic intervertebral disc nucleus. Radiat. Phys. Chem. 63, 539–542 (2002). doi:10.1016/S0969-806X(01)00636-3
J.S. Belkas, C.A. Munro, M.S. Shoichet, M. Johnston, R. Midha, Long-term in vivo biomechanical properties and biocompatibility of poly(2-hydroxyethyl methacrylate–co-methyl methacrylate) nerve conduits. Biomaterials 26, 1741–1749 (2005). doi:10.1016/j.biomaterials.2004.05.031
D.L. Whitehouse, Handbook of surface metrology. (Institute of Physics Publishing, Bristol, 1994), ISBN 0-7503-0039-6
Roman. Jantas, Synthesis and characterization of poly(2-hydroxyethylmethacrylate)-1-naphthylacetic acid adduct. Polym. Bull. 58, 513–520 (2007). doi:10.1007/s00289-006-0696-y
H. Wang, K. Siow, Measurement of Tg in epoxy resins by DSC-effects of residual stress, polym. Eng. Sci. 39(3), 422–429 (1999)
A. Roguin, E. Grenadier, Stent-based percutaneous coronary interventions in small coronary arteries. Acute Card. Care 8(2), 70–74 (2006)
S.V. Ranade et al., Physical characterization of controlled release of paclitaxel from TAXUS express drug eluting stent. J. Biomed. Mater. Res. A 71A, 625–634 (2004). doi:10.1002/jbm.a.30188
P.P. de Jaegere, P.J. de Feyter, W.J. van der Giessen, P.W. Serruys, Endovascular stent: preliminary clinical results and future developrments. Clin. Cardiol. 16(5), 369–378 (1993)
T.W. Chung, D.Z. Liu, S.Y. Wang, S.S. Wang, Enhancement of the growth of human endothelial cells by surface roughness at nanometer scale. Biomaterials 24, 4655–4661 (2003). doi:10.1016/S0142-9612(03)00361-2
M. Lampin, R. Warocquier-Clerout, C. Legris, M. Degrange, M.F. Sigot-Luizard, Correlation between substratum roughness and wet ability, cell adhesion and cell migration. J. Biomed. Mater. Res. 36, 99–108 (1997). doi:10.1002/(SICI)1097-4636(199707)36:1<99::AID-JBM12>3.0.CO;2-E
A. Dibra et al., Influence of stent surface topography on the outcomes of patients undergoing coronary stenting: a randomized double-blind controlled trial. Catheter. Cardiovasc. Interv. 65, 374–380 (2005). doi:10.1002/ccd.20400
A. Severini et al., Polyurethane-coated, self-expandable biliary stent: an experimental study. Acad. Radiol. 2, 1078–1081 (1995). doi:10.1016/S1076-6332(05)80520-3
P. Hanefeld, U. Westedt, R. Wombacher et al., Coating of poly(p-xylylene) by PLA-PEO-PLA triblock copolymers with excellent polymer-polymer adhesion for stent applications. Biomacromolecules 7, 2086–2090 (2006). doi:10.1021/bm050642k
T. Yua, M. Shoichet, Guided cell adhesion and outgrowth in peptide-modified channels for neural tissue engineering. Biomaterials 26, 1507–1514 (2005). doi:10.1016/j.biomaterials.2004.05.012
Acknowledgements
The authors warmly wish to thank Paolo Carboni for his assistance in spray-coating technology set-up, Antonio Gloria for discussion on mechanical tests, and Cesare Luponio for helpful contribution on AFM observations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Indolfi, L., Causa, F. & Netti, P.A. Coating process and early stage adhesion evaluation of poly(2-hydroxy-ethyl-methacrylate) hydrogel coating of 316L steel surface for stent applications. J Mater Sci: Mater Med 20, 1541–1551 (2009). https://doi.org/10.1007/s10856-009-3699-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-009-3699-z