Abstract
Background Treatment of segmental bone loss remains a challenge in skeletal repair. A major therapeutic goal is the development of implantable materials that will promote bone regeneration. Objective We evaluate bone regeneration in grafts containing different concentrations autologous iliac crest bone (ACB) particles, carried in a new injectable calcium phosphate cement (CPC), in ulnar bone defects in rabbits. Methods Large upper-mid-diaphyseal defects (10 mm) were created in the left ulnae of 60 skeletally mature New Zealand white rabbits. ACB concentrations of 0, 25, 50, 75, and 100% (by volume) in CPC were used to fill operated sites. Defect bridging was monitored by serial radiography at 4, 8, and 12 weeks post-operation. Samples were then examined histologically and by manual palpation to determine the extent of new bone formation. Results At 4 weeks, we observed more elaborate structures and extensive absorption in ulnae treated with mixtures containing low concentrations of ACB (such as 0% and 25% volume of ACB/CPC), compared with those treated with mixtures containing high concentrations of ACB (such as 75% and 100% volume of ACB/CPC). At 8 weeks, histomorphometry revealed increased trabecular area and volume in the group treated with high ACB concentrations compared with those treated with low ACB concentrations. At 12 weeks, complete cortical bridging and regeneration of marrow space were detected in groups treated with high concentrations of ACB, and the amount of new bone regeneration was greater in these groups than in those treated with low ACB concentrations. Conclusions Treatment of rabbit ulnar defects with injectable CPC carrying an optimized concentration of ACB particles can lead to cortical bridging and bone marrow regeneration within 12 weeks.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The treatment of post-traumatic skeletal conditions such as delayed unions, non-unions, malunions, and other bone loss defects is challenging [1, 2]. In many cases, adjunctive measures such as bone-grafting are required to stimulate bone healing and fill bone defects. Several options currently exist for bone replacement: autologous or allogeneic cancellous or cortical bone, demineralized bone matrix, calcium phosphate-based bone-graft substitute, or autologous bone marrow [3]. Conventional bone-grafting with autologous cortical and cancellous bone harvested from the iliac crest [4] is the standard against which all other bone-graft substitutes are judged, but it has disadvantages, such as limited supply of autologous bone especially in major skeletal reconstruction, complications of pain, or infection at the donor site. Banked allogenic bone [5] has been advocated as an alternative to autografting, but allogenic bone can be associated with transmission of infection. Moreover, the efficacy of this type of graft is not clear, given evidence of non-union, fatigue fracture, and both clinical and histological evidence of graft absorption.
Owing to the disadvantages of autologous and allogenic bone-grafts, there has been an increased interest in bone substitutes [6]. From a biological point of view, calcium phosphates such as TCP-HA granules are promising synthetic alternatives to bone-grafting. In recent years, calcium phosphate cement (CPC), a mixture of several different calcium phosphates, has been developed as a novel material for bone repair [7]. This synthetic biomaterial is self-setting, relatively plastic, biocompatible, and has been tested in a clinical setting.
Mixtures of TCP granules or cement combined with autologous bone particle grafting techniques have been used for treating both bone defects and spinal fusions in clinic [8, 9]. But the morphological evaluation and volume-effect character of this graft were not reported. In early study [10], compressive strength is thought to be improved by either decreasing cement volume or increasing the ratio of bone in graft mixtures. However, it is unclear whether the ratio of bone to cement likewise affects bone regeneration. Owing these, we examine quality and quantity character of bone regeneration in rabbit ulnar defects into which we grafted varying ratios of a new injectable CPC, to mixed autologous illiac crest bone (ACB) particles.
2 Materials and methods
2.1 Preparation of CPC
CPC was generated from a mixture of solid and liquid components [11]. The solid components consisted of a mixture of beta-tricalcium phosphate (β-TCP), dicalcium phosphate dihydrate (CaHPO4H2O, DCPD), calcium carbonate (CaCO3), hydroxyapatite (HA) nano-structures (Guangzhou Jingpu New Materials Technology Co., Ltd.), and small amount of chitosan [7]. The liquid component consisted of a sodium phosphate buffer solution (NaH2PO4/Na2HPO4, pH 7.4). Before use, the powders were mixed and milled in a mortar to obtain a small particle size. The cement powder was then sterilized with 30 kGy γ irradiation, while the liquid component was filter-sterilized through a 0.2 μm filter. To deliver the cement, a 5 ml syringe was filled with a mixture of 1 g of cement powder, and 0.5 ml cement liquid. The injectability of the cement was determined 2 min after mixing and, when the syringe piston moved easily, the cement was then extruded through a needle (i.d. 1 mm, length 70 mm) and used for injection.
2.2 Preparation of ACB/CPC mixtures
Autologous cancellous bone was harvested from the right iliac crest of the rabbit at the time of grafting. A portion of the posterior iliac crest, measuring approximately 4 cm2, was resected. The internal and external tables of the excised segment of the ilium were separated and the cancellous bone was harvested with a curet. The bone was then cut into pieces about 1 mm in diameter, and was used immediately for grafting.
Increasing amounts of ACB were combined with CPC in a final volume of 2 ml each, resulting in ACB concentrations of 0%, 25%, 50%, 75%, and 100% by volume; these were mixed for about 1 min prior to use.
2.3 Segmental defect model
2.3.1 Preparation of the animal model
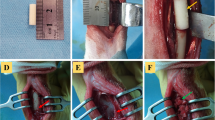
Sixty adult male New Zealand rabbits (>1-year-old and 4.0–3.0 kg) were divided into five study groups (n = 12) at random and anesthetized by an intravenous injection of pentobarbital (0.75 mg/kg). The left foreleg of all animals were depilated, cleaned, and sterilized with iodine tincture and alcohol. For each animal, an incision was made directly over the ulnae, muscles were separated and the upper–middle part of the ulnar was exposed. Bony defect of ulnar was made by excising a 1-cm-long bone segment and surrounding periosteum from the 3-cm proximal segment of the right distal radio-ulnar joint [12].
2.3.2 Implantation
Approximately 2 ml of graft material mixtures with varying concentrations of ACB were placed within ulnar defects and were held in position by suturing muscle and fascia over the graft. Once bleeding had ceased (excessive bleeding was stopped with a collagen sponge), the incision was sutured and bacitracin ointment was applied to the wound. All the procedures employed in this study were in accordance with the standards of the guidelines for the care and use of laboratory animals of the NIH.
2.3.3 Animal care before and post-operation
The operated rabbits were housed at the Experimental Animal Facility of Zhujiang Hospital and bred with standard granulose food, free moving and drinking in separate cages.
2.4 Evaluation of bone regeneration
Bone regeneration was evaluated stepwisely by plain radiograph, manual palpation, and histological analysis. Firstly, plain radiographs were taken at 4, 8, and 12 weeks after operation to monitor the healing process at the resection sites. Secondly, two rabbits from each experimental group were sacrificed at 4 and 8 weeks by overdose of pentobarbital (1 ml/kg). Other eight rabbits in every group were sacrificed at 12 weeks. The left ulnae was resected and all soft tissue was removed. And then, manual palpation was performed on each sample for bony connection examination. Thirdly, the ulnar samples were fixed in 4% paraformaldehyde. Fixed samples were decalcified with 10% nitric acid, dehydrated, cleared, and embedded in paraffin. Defect-bridging site in every sample was sectioned at 10 μm intervals, parallel to the longitudinal axis of the ulnar. About 10 sections in every sample was oven-dried, dewaxed, and subjected to routine HE staining. Finally, every section of all samples was observed under a light microscope for signs of degradation of implanted material and bone regeneration. Resorption characters, such as numbers of newly formed vessels and fibrous structures per mm2, were quantified at 4 weeks, and bone volume fractions within the defects were quantified after 8 weeks. The degree of bone regeneration was calculated as percent area of new bone in the graft, measured using Image J software [13, 14]. All measurements were performed within a region of interest, 5 mm in diameter in these 10 sections for each defect.
To observe degradation and ultrastructure of the bone–cement interface [15], two samples from each group were collected 12 weeks after grafting, and were fixed as described above. Implanted areas were split longitudinally, immersed in stepwise phosphate buffers, dehydrated through a 30–100% alcohol series at room temperature (24°C), dried at the critical point, coated with gold in vacuum, and observed by scanning electron microscope (SEM) (Hitachi X-506, Sun Yat-sen University).
2.5 Statistical analyses
Statistical analysis was performed using SPSS 11.0 software. Tukey test was used for post-hoc comparisons using a confidence level of P < 0.05 to determine the significance of differences in degree of newly formed vessels, fibrous structures and bone regeneration among the five groups. Significance of differences in manual palpation results was evaluated using a non-parametric test with Kruskal–Wallis test.
3 Results
3.1 Complications
One rabbit in 25% ACB concentrations group died during the surgical procedure due to complications from the deep anesthesia. One rabbit each from 0% to 100% ACB concentrations groups died from massive hemorrhage or other intraoperative complications. These animals were replaced in subsequent experiments. Three cases of superficial infection were noted throughout the study. These were treated by routine methods. No fractures were observed at the grafting site (not shown).
3.2 Evaluation of plain radiography
Using plain radiography, regenerated bone was clearly thinner than normal in 25%, 50% and 75% volume of ACB/CPC groups at 8 and 12 weeks. Numerous cortical irregularities were observed between defect ends (Fig. 1c, d) or located at the periphery of the defect (Fig. 1b). There was no bony connection between both ends of ulnar defect at 4, 8 weeks in every group or pure CPC group (0% volume of ACB/CPC group) and 25% volume of ACB/CPC group at 12 weeks. There were 3, 6 and 8 ulnar defects reached bony fusion in 50%, 75% and 100% volume of ACB/CPC group, respectively at 12 weeks.
Radiographs of rabbit ulnar defects (arrow showed). (a) Resorption and few bone regeneration could be detected in defects with CPC containing 25% ACB particles 8 weeks after operation. (b) Bone regeneration connecting both defect ends could be detected with CPC containing 25% ACB particles 12 weeks after operation. (c) Defects were filled with trabelulous bone with CPC containing 75% ACB particles 12 weeks after operation. (d) Defects were filled with regeneration bone with CPC containing 100% ACB particles 12 weeks after operation
3.3 Evaluation of manual palpation
Through manual palpation examination, there were no bony connection of all samples at 4 and 8 weeks in every group. At 12 weeks, bony connections between the original bone ends were observed in 0, 3, 6, 8 ulnar samples of 0%, 25%, 50%, 75%, 100% volume ACB/CPC group, respectively. No significant difference was observed between 75% and 100% volume ACB/CPC group (P > 0.05).
3.4 Histological analysis under light microscope
By histological analysis, a large area of new bone was detected within ulnae from all experimental groups. However, we observed a distinct difference in the degree of CPC degradation and formation of new bone among the five treatment groups. In all groups at 4 weeks of engraftment, we observed a region of absorption and regenerated fibrous tissue. Grafts were surrounded by fibroblasts and newly formed vessels, but inflammation cells such as leukocytes were scarce (Fig. 2a, b). In all sections, what remained of the graft appeared actively to be in the process of being resorbed by osteoclasts (Fig. 2a, b). Eight weeks after engraftment, we observed extensive recruitment of activated osteoblastic cells, woven bone structures, islands of new bone, and new blood vessels in the area of the graft in all experimental groups. Lamellar bone was observed on the graft surface, suggesting a high degree of remodeling activity (Fig. 2c, d). In the low concentrations of ACB particles groups such as 0%, 25%, or 50% volume of ACB/CPC group, many trabeculae and plastic osteoids, as well as marrow cavity-like structures were detected (Fig. 2c). Overall, the appearance of new bone tended to correlate with ACB particle concentration (Fig. 2d). By 12 weeks post-engraftment, the structures of woven bone and new blood vessels had almost disappeared, and ulnar defect was filled with newly formed bone in the high concentration of ACB particles groups such as 75% or 100% volume of ACB/CPC group. Morphologically, the new bone exhibited many characteristics of trabecular bone, such as plastic osteoid and marrow cavity-like structures. In addition, numerous activated osteoblastic cells were observed along the endosteal surface of the bone marrow cavity (Fig. 3a, b). Complete bridging of the original defect was observed by this time, and the harvesian canal was restored at the level of the bone defects (Fig. 3b). But in the groups treated with the low concentration of ACB particles such as 0%, 25%, or 50% volume of ACB/CPC group, new bone appeared among the various tissues, and was comprised mainly of woven bone, with many osteoid areas. New bone contained large marrow cavities and small cancellous bone structures (Fig. 3a). Over all, in the high concentration of ACB particle groups, more dense structures and larger amounts of new bone were observed. The cancellous bone structures were larger, while marrow cavities were smaller (Fig. 3b), than in the low concentration of ACB particles groups (Fig. 3a).
Histological evaluation of degradation and bone formation among the different treatment groups (arrow showed). (a) HE staining of a section at 4 weeks in the group treated with CPC containing 0% ACB particles (20×). (b) HE staining at 4 weeks in the group treated with a graft containing 100% ACB particles (20×). (c) HE staining at 8 weeks in the group treated with a CPC mixture containing 75% ACB particles (20×). (d) HE staining at 8 weeks in the group treated with a graft containing 100% ACB particles (20×)
Histological and scanning electron microscope (SEM) evaluation of degradation and bone formation in different treatment groups. (a) HE staining at 12 weeks in the group treated with a CPC mixture containing 50% ACB particles (20×). (b) HE staining at 12 weeks in 100% ACB particles treated group (20×). (c) SEM observation at 12 weeks in the group treated with CPC containing 0% ACB particles (10×). Arrow indicates newly formed fibrous structures in the cement. (d) SEM micrograph of bone 12 weeks after engraftment with 100% ACB particles (10×). Arrow indicates newly formed fibrous structures within the bone
Through quantity evaluation, more newly formed vessels were observed in the group treated with pure CPC (Table 1, 6.40 ± 1.26 per mm2) or ACB/CPC mixtures than in the group treated with pure ACB particles (Table 1, 4.30 ± 1.16 per mm2) at 4 weeks after operation. Fibrous structures had a higher density in the pure CPC (Table 1, 17.40 ± 2.63 per mm2) or ACB/CPC mixtures group than in the pure ACB particles group (Table 1, 13.10 ± 2.02 per mm2). In all ACB/CPC mixed groups, no difference in the number of new vessels and fibrils was detected, suggesting similar rates of absorption and regeneration in these groups (Table 1). By 8 weeks post-engraftment, the area of new bone occupied about 5.98 ± 1.44% within the region of the ulnar defect (Table 2) in the pure CPC group and 7.22 ± 2.64% in 25% volume of ACB/CPC group. In contrast, the high ACB concentration groups such as 75% and 100% volume of ACB/CPC groups, the area containing new bone was 14.88 ± 1.94% and 18.38 ± 2.28%, respectively and was larger than in the low ACB concentration groups (Table 2). The area containing new bone was almost the same in 0 and 25% ACB concentration groups, and in 50% and 75% ACB concentration groups (P > 0.05, Table 2). By 12 weeks of engraftment, in pure CPC group, new bone reached 32.42 ± 2.76% of grafted area. While in the pure or high ACB concentration group, denser structures and larger amount area of new bone were observed (Table 2, 81.98 ± 5.80% of area percent). New bone area percent reached 52.40 ± 4.46% in the 50% ACB concentration group (Table 2).
3.5 Histological analysis under SEM
By SEM, we detected many newly formed vessels and fibrous structures at the surface of the graft (Fig. 3c), as well as newly formed bone (Fig. 3d) in all groups. The new bone appeared to have grown into the graft and to have a tight connection with neighboring bone.
4 Discussion
Bone-graft substitutes have the ability of osteoconduction [16] which means a process in which the three-dimensional structure of a substance is conducive for the ongrowth and/or ingrowth of newly formed bone. They are used as autogenous bone-graft extenders, such as multi-level spinal fusion, large segmental bone defects. And now the main materials include coralline hydroxyapatite, collagen-based matrices, calcium sulfate, bioglass and calcium phosphate cement.
Coralline hydroxyapatite is produced from marine coral exoskeletons that have a very regular pore structure resembling cancellous bone. It is an effective bone-graft substitute for metaphyseal defects [17]. Animal and human studies [18, 19] have shown that vascular and fibrous tissue invade the pore structures and are subsequently converted to mature lamellar bone, similar to the process seen with autogenous bone-grafts. But it is very difficult to resorpt. Blocks of implanted coralline hydroxyapatite may remain apparent on radiographs for 10 years or longer. Collagen-based matrices [20] are xenografts consisting of sponge-like trips of purified bovine fibrillar collagen (primarily type I) that is combined with hydroxyapatite alone or with both hydroxyapatite and TCP. They are designed to be hydrated and implanted with autogenous bone marrow or bone-graft, and both have been used as bone-graft extenders to increase the volume of bone-graft into a defect when sufficient volume of autograft is not readily available. Histologic analysis in animal models has shown bone ingrowth into the matrix of the material. But it has the risk of eliciting a harmful immune reaction in vivo [21]. Calcium sulfate is one of the oldest bone-graft substitutes. Its reported use dates backed to 1892. Contemporary use of calcium sulfate occurred with the introduction of Osteoset (Wright Medical, Arlington, TN) in 1996. But the material is resorbed too rapidly to provide a long-term three-dimensional framework that could support osteoconduction [22]. Bioglass [23] is currently being developed which is composed of silica (45%), calcium oxide (24.5%), disodium oxide (24.5%), and pyrophosphate (6%). When implanted, they bind to collagen, growth factors, and fibrin to form a porous matrix to allow infiltration of osteogenic cells. Tricalcium phosphate is a random porous ceramic that undergoes partial conversion to hydroxyapatite once it is implanted into the body. While calcium phosphate cement (CPC) is an injectable paste of inorganic calcium and phosphate that hardens in situ and cures by a crystallization reaction to form dahllite. It is an osteoconductive material; it does not offer structural support, but it serves to fill areas containing bone defects or cavities. Moreover, it is quickly resorbed, and thus stimulates cell infiltration immediately following revascularisation of the site of implantation [24]. Animal’s studies [25] have shown that the material is gradually remodeled in a manner that is qualitatively similar to normal bone remodeling. Overtime, calcium phosphate undergoes osteoclastic resorption, followed by the invasion of small blood vessels that become surrounded by circumferential lamellae of new bone.
Our cement is a new bone-graft substitute composed mainly of β-TCP, DCPD and nanocrystalline-precipitated HA. In previous studies, we implanted this cement into femoral bone defects in rabbits [11]. Within 7–10 days of implantation, bone capillaries had begun to infiltrate the material. By 2 weeks of implantation, osteoid formation had begun and reached maximum bone formation within 4–8 weeks. By 8 weeks of engraftment, the cement became enclosed by newly formed lamellar bone, consistent with regeneration of the long bone defect.
Our study is the first to use CPC as a liquid scaffold for ACB particles. This mixture exhibited a consistent ability to facilitate bone regeneration, without recruitment of immune cells such as leukocytes. In addition, this cement was degraded early (within 4 weeks), leaving behind elaborate structures and new blood vessels at the site of absorption. At 8 and 12 weeks after engraftment, a large amount of new bone was detected, and correlated with the concentration of ACB particles. This trend could be explained by an increase in the production of growth-stimulating factors and increased cell proliferation induced by the engrafted bone. Because osteoblasts and endosteal cells lining the surface of the graft survive transplantation, a cancellous bone-graft acts mainly as an osteoconductive substrate, which effectively supports the ingrowth of new blood vessels and the infiltration of new osteoblasts and osteoblast precursors [26]. Osteoinductive factors released from the graft during the absorption process may also contribute to healing of the graft. When mixed with CPC, osteoblasts can absorb the cement, and form new bone directly, and osteoinductive factors may accelerate cell growth or fluid degradation of cement and thus promote new bone regeneration [27]. Moreover, cancellous bone serves as a good source of filler material and has long been used as a bone substitute in a wide variety of orthopedic operations, in combination with other biological materials such as TCP particles. Consistent with this proposal, we found that engraftment with CPC lacking ACB particles showed a lack of new bone formation, possibly owing to a deficiency in bone-promoting factors. This model can also explain why the amount of new bone increased with an increasing concentration of ACB particles. When the ACB/CPC volume ratio reached 50%, new bone regeneration consisted of 65% pure autologous bone. And when this ratio was increased to 75%, the effect of bone formation was almost the same as grafts entirely lacking CPC. Thus, the optimal ratio of bone to cement can stimulate bone healing in critical-sized defects.
The use of a combination of CPC and ACB particles provides several advantages over the use of either autogenous or allograft bone implants. First, this mixture can be used to supplement autologous cancellous bone when the supply is limited or the defect is very large. Second, this mixture does not trigger immune rejection. Moreover, this mixture is sufficiently plastic to be useful in treatment of irregular bone cavities, for example resulting from removal of bone tumors. Compared with other graft substitutes, this mixture is the only to meet criteria of biocompatability, osteoconductivity, and osteotransductivity.
Interestingly, we also observed that when the concentration of ACB particles was low, bone regeneration occurred very slowly and was limited to a small area. In addition, the observation period was only 12 weeks, which may have been an inadequate time span to observe cement absorption in this kind of graft. An interesting question for future studies is whether this type of graft could possibly be optimized by addition of other factors, such as bone morphogenetic protein (BMP).
5 Conclusions
Our results suggest that CPC can be used as a scaffold for implantation of autologous bone into proper bone defects. New bone formation is closely correlated with the concentration of ACB particles, up to a maximum concentration of 75% of the CPC.
References
A.C. Chen, E.K. Chao, Y.K. Tu, S.W. Ueng, Scaphoid nonunion treated with vascular bone grafts pedicled on the dorsal supra-retinacular artery of the distal radius. J. Trauma 61(5), 1192–1197 (2006)
D.S. Bae, P.M. Waters, M.C. Gebhardt, Results of free vascularized fibula grafting for allograft nonunion after limb salvage surgery for malignant bone tumors. J. Pediatr. Orthop. 26(6), 809–814 (2006)
G. Binyamin, B.M. Shafi, C.M. Mery, Biomaterials: a primer for surgeons. Semin. Pediatr. Surg. 15(4), 276–283 (2006)
C. Hierholzer, D. Sama, J.B. Toro, M. Peterson, D.L. Helfet, Plate fixation of ununited humeral shaft fractures: effect of type of bone graft on healing. J. Bone Joint Surg. Am. 88(7), 1442–1447 (2006)
S. Vastardis, R.A. Yukna, Evaluation of allogeneic bone graft substitute for treatment of periodontal osseous defects: 6-month clinical results. Compend. Contin. Educ. Dent. 27(1), 38–44 (2006)
R.Z. LeGeros, Properties of osteoconductive biomaterials: calcium phosphates. Clin. Orthop. Relat. Res. 395, 81–98 (2002)
H. Liu, H. Li, W. Cheng, Y. Yang, M. Zhu, C. Zhou, Novel injectable calcium phosphate/chitosan composites for bone substitute materials. Acta Biomater. 2(5), 557–565 (2006)
H.C. Pan, Y.C. Wang, C.H. Lee, D.Y. Yang, Hollow bone cement filled with impacted cancellous bone as a substitute for bone grafts in cervical spine fusion. J. Clin. Neurosci. 14(2), 143–147 (2007)
R.K. Sharma, Marriage of autogenous bone and hydroxyapatite cement for reconstruction of frontal bone defect. Plast. Reconstr. Surg. 116(5), 1568–1569 (2005)
W.H. Rijnen, J.W. Gardeniers, B.W. Schreurs, P. Buma, Impacted bone and calcium phosphate cement for repair of femoral head defects: a pilot study. Clin. Orthop. Relat. Res. 459, 216–221 (2007)
Y. Weitao, K. Kangmei, J. Anmin, An injectable cement: synthesis, physical properties and scaffold for bone repair. J. Postgrad. Med. 53(1), 34–38 (2007)
D. Keskin, C. Gundogdu, A.C. Atac, Experimental comparison of bovine-derived xenograft, xenograft-autologous bone marrow and autogenous bone graft for the treatment of bony defects in the rabbit ulna. Med. Princ. Pract. 16(4), 299–305 (2007)
J. Mueller, H. Meyer-Lueckel, S. Paris, W. Hopfenmuller, A.M. Kielbassa, Inhibition of lesion progression by the penetration of resins in vitro: influence of the application procedure. Oper. Dent. 31(3), 338–345 (2006)
H.W. Kim, S.Y. Shin, H.E. Kim, Y.M. Lee, C.P. Chung, H.H. Lee, I.C. Rhyu, Bone formation on the apatite-coated zirconia porous scaffolds within a rabbit calvarial defect. J. Biomater. Appl. 10 (2007 in press)
A.G. Dias, M.A. Lopes, J.D. Santos, A. Afonso, K. Tsuru, A. Osaka, S. Hayakawa, S. Takashima, Y. Kurabayashi, In vivo performance of biodegradable calcium phosphate glass ceramics using the rabbit model: histological and SEM observation. J. Biomater. Appl. 20(3), 253–266 (2006)
D.J. Hak, The use of osteoconductive bone graft substitutes in orthopaedic trauma. J. Am. Acad. Orthop. Surg. 15(9), 525–536 (2007)
M.J. Coughlin, J.S. Grimes, M.P. Kennedy, Coralline hydroxyapatite bone graft substitute in hindfoot surgery. Foot Ankle Int. 27(1), 19–22 (2006)
D. Stubbs, M. Deakin, P. Chapman-Sheath, W. Bruce, J. Debes, R.M. Gillies, W.R. Walsh, In vivo evaluation of resorbable bone graft substitutes in a rabbit tibial defect model. Biomaterials 25(20), 5037–5044 (2004)
C.J. Hsu, W.Y. Chou, H.P. Teng, W.N. Chang, Y.J. Chou, Coralline hydroxyapatite and laminectomy-derived bone as adjuvant graft material for lumbar posteriolateral fusion. J. Neurosurg. Spine 3(4), 271–275 (2005)
K. Hoshi, Mechanisms of bone calcification. Clin. Calcium 17(10), 1499–1507 (2007)
H. Methe, E.R. Edelman, Tissue engineering of endothelial cells and the immune response. Transplant. Proc. 38(10), 3293–3299 (2006)
K.A. Hing, L.F. Wilson, T. Buckland, Comparative performance of three ceramic bone graft substitutes. Spine J. 7(4), 475–490 (2007)
J. Moura, L.N. Teixeira, C. Ravagnani, O. Peitl, E.D. Zanotto, M.M. Beloti, H. Panzeri,A.L. Rosa, P.T. de Oliveira, In vitro osteogenesis on a highly bioactive glass-ceramic (Biosilicate). J. Biomed. Mater. Res. A. 82(3), 545–557 (2007)
A.J. Ambard, L. Mueninghoff, Calcium phosphate cement: review of mechanical and biological properties. J. Prosthodont. 15(5), 321–328 (2006)
N. Kobayashi, K. Ong, M. Villarraga, J. Schwardt, R. Wenz, D. Togawa, T. Fujishiro, A.S. Turner, H.B. Seim 3rd, T.W. Bauer, Histological and mechanical evaluation of self-setting calcium phosphate cements in a sheep vertebral bone void model. J. Biomed. Mater. Res. A 81(4), 838–846 (2007)
A. Scutt, P. Bertram, Bone marrow cells are targets for the anabolic actions of prostaglandin E2 on bone: induction of a transition from nonadherent to adherent osteoblast precursors. J. Bone Miner. Res. 10(3), 474–487 (1995)
I.A. Khlusov, A.V. Karlov, N.S. Pozhen’ko, I.V. Sukhodolo, M.Y. Khlusova. Relationship between osteogenic characteristics of bone marrow cells and calcium phosphate surface relief and solubility. Bull. Exp. Biol. Med. 141(1), 99–103 (2006)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weitao, Y., Kangmei, K., Xinjia, W. et al. Bone regeneration using an injectable calcium phosphate/autologous iliac crest bone composites for segmental ulnar defects in rabbits. J Mater Sci: Mater Med 19, 2485–2492 (2008). https://doi.org/10.1007/s10856-008-3383-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-008-3383-8