Abstract
Biodegradable polymer/bioceramic composite scaffolds can overcome the limitations of conventional ceramic bone substitutes such as brittleness and difficulty in shaping. However, conventional methods for fabricating polymer/bioceramic composite scaffolds often use organic solvents (e.g., the solvent casting and particulate leaching (SC/PL) method), which might be harmful to cells or tissues. In this study, Poly (d,l-lactide)/nano-hydroxyapatite (PDLLA/NHA) composites were prepared by in-situ polymerization, and highly porous scaffolds were fabricated using a novel method, supercritical CO2/salt-leaching method (SC CO2/SL). The materials and scaffolds were investigated by scanning electronic microscopy (SEM), transmission electronic microscopy (TEM) and gel permeation chromatography (GPC). GPC showed that the molecular weight of composites decreased with increase of NHA content. However, the water absorption and compressive strength increased dramatically. The SEM micrographs showed that the scaffolds with pore size about 250 μm were obtained by controlling parameters of SC CO2/SL. The biocompatibility of PDLLA/NHA porous scaffolds were evaluated in vitro and in vivo. The evaluation on the cytotoxicity were carried out by cell relative growth rate (RGR) method and cell direct contact method. The cytotoxicity of these scaffolds was in grade I according to ISO 10993-1. There was no toxicosis and death cases observed in acute systemic toxicity test. And histological observation of the tissue response (1 and 9 weeks after the implantation) showed that there are still some slight inflammation responses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Current clinical technologies such as autografting and allografting cancellous (spongy) bone and applying vascularized grafts suffer from cost and anatomical limitations and donor site morbidity or tissue rejection [1–3]. Tissue engineering is a promising alternative for organ repairing and tissue reconstruction [4–6]. Engineering living tissue requires an appropriate cell source, optimal cell culture conditions and a biodegradable scaffold as the elements. As for the scaffold, both the material and the scaffold morphology affect the performance of the engineered tissue.
Poly (lactic acid) and its copolymer have been very attractive to tissue engineering scaffold due to their controllable biodegradability and the safety of their degraded products [7–11]. However these polymers may elicit inflammatory response in the host tissue because of the release of acidic degradation products [12, 13]. On the other hand, these synthetic resorbable polymers are more easily fabricated into complex structures yet are too weak to meet the demands of orthopedic surgery [14]. Certain bioactive ceramics such as tricalcium phosphate (TCP) and hydroxyapatite (HA), react with physiological fluids to form tenacious bonds to hard (and in some cases soft) tissue [15]. Thus porous bioactive ceramics are being considered for clinical applications, including scaffolds for tissue engineering [16]. These bioactive materials are however relatively stiff, brittle, and difficult to form into complex shapes. Composites combining these degradable polymers with inorganic bioactive phases are of particular interest as tissue engineering scaffolds [17, 18] as tailored physical, biological, and mechanical properties can be obtained.
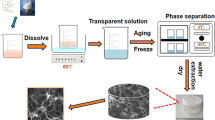
It is well known that highly open porous matrix is required for high density cell seeding and efficient nutrient and oxygen supply to the cells cultured in the three-dimensional scaffold. There have been several methods to produce highly porous biodegradable polymer scaffolds such as solvent-casting/salt leaching [19], phase separation [20], fiber extrusion and fabric forming processing [21], gas foaming [22–26] and supercritical CO2 method (SC CO2) [27–29]. The solvent-casting/salt leaching and phase separation approaches require the use of organic solvents. Residua of organic solvents in the polymer may be harmful to the transplanted cells and inactivate many biologically active factors. Fiber forming processing typically requires high temperature and is not suitable to process amorphous polymers. High temperature used in this process is also likely to denature biologically active molecules, which one might wish to incorporate into the matrix. SC CO2 has some unique properties such as liquid-like dissolving power and reduction of the glass transition temperature of polymer and a relatively low critical point (35 °C, 8 MPa). So SC CO2 is the most widely used in supercritical fluid field [30, 31]. M H Sheridan [32] had studied the effect of the choice of gas on the biomaterial scaffold structures. It was found that supercritical CO2 could produce highly porous matrix, whereas N2 and He did not lead to measurable pore formation. The unique properties of SC CO2 maybe lead to create porous polymer structures easier than other gases. SC CO2 has also many advantages in preparing porous polymer matrix, which can avoid the use of organic solvent, high temperature and decrease the saturation time compared with the usual gas foaming method. But gas foaming with pressurized carbon dioxide often results in poor interconnectivity between micro-pores, which will lower the viability of seeded cell and result in non-uniform distribution of the seeded cells throughout the matrix [25]. Here sodium chloride was used as porogen to solve the problem. SC CO2/SL had been developed to fabricate the PDLLA/NHA composite foams.
In the present work, various PDLLA/NHA composites were prepared via the in-situ polymerization of d,l-lactide monomer and nano-hydroxyapatite. Scaffolds of PDLLA/NHA composites with high porosity and pore sizes about 250 μm were fabricated through SC CO2/SL. The materials are intended as scaffolds for bone tissue engineering applications. The in vitro and in vivo responses were comprehensively assayed by in vitro cytotoxicity test, in acute systemic toxicity test and the test of local tissue responses after implantation.
Materials and methods
Materials
d,l-lactide and nano-hydroxyapatite (NHA) were prepared by our lab. Stannous octoate and other solvent used were purchased from Shanghai Chemical Reagent factory.
Synthesis of PDLLA/NHA composites
d,l-lactide (100 g), NHA (2 g) and d,l-lactide (100 g), NHA (4 g) were respectively melted at 140 °C for 30 min with stir under nitrogen atmosphere, then stannous octoate was added to the molten monomer and polymerized for 30 h at 140 °C. After polymerization, PDLLA/NHA was dissolved in chloroform, precipitated in excess methanol, and then filtered. The composites were vacuum-dried at 40 °C for 24 h and stored in a desiccator.
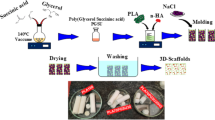
Fabrication of scaffolds with SC CO2 /SL
The porous scaffolds were fabricated using SC CO2/SL with NaCl as the porogen. 6 g PDLLA/NHA was crushed to powder (particle size in the range of 300 to 350 μm) by liquid nitrogen quenching and mixed with 2.4 g NaCl (particle size in the range of 250 to 350 μm) uniformly in Teflon mold, then put the mold into oven heating at 110 °C for 1.5 h. The mold was pressed slightly when it was removed from oven, then the mixture was naturally cooled to ambient temperature, and loaded into high pressure chamber, then CO2 gas was introduced into the chamber achieving super critical condition (35 °C, 8 MPa). Samples were allowed to equilibrate and saturate with the supercritical CO2 liquid for 30 min. At the end of the equilibration period, the gas was rapidly released (approximately a 12 s decompression), and the chamber reach ambient pressure. The samples were subsequently removed from the chamber and immersed in distilled deionized water (DW) for 48–72 h (DW was changed every 6 h) with ultrasonic vibrations to leach out the salt. After being air-dried for 48 h and vacuum-dried for 12 h, the PDLLA/NHA scaffolds were stored in a desiccator.
Morphology and structures of composites and scaffolds
The PDLLA/NHA composites and scaffolds were examinated with scanning electron microscopy (SEM) (Hitachi S-2360N). Samples were coated with gold for 5 min under a current of 18 mA before examination under an accelerating voltage of 15 kV. Nanoparticles in the composites were observed with transmission electron microscopy (TEM) (Hitachi H600).
Molecular weight of composites
Molecular weights of composites were characterized at 35 °C on gel permeation chromatography (GPC) (Waters-150C), and tetrahydrofuran was employed as the eluent at 1.0 mL/min. Narrow-distributed polystyrenes standards were employed to make a calibration curve.
Water absorption tests
Scaffolds weighed as W1 were immersed and soaked in DW, and were taken out to weigh as W2 after 1, 2, 4, 8, 12 and 24 h. Then the water absorption rate for samples at different time is calculated according to (W2−W1)/W1 × 100%.
Porosity measurements
The porosity of the scaffolds (ε) was measured by mercury pycnometry. A sample of weight Ws was placed in a pycnometer, which was completely filled with mercury and weighted to obtain W2. The density of scaffolds (ρs) was calculated according to ρs = Ws × ρHg/(Wl–W2 + Ws), where Wl is the weight of the pycnometer filled with mercury, and ρHg is the density of mercury (13.5 g/cm3). Pore volume (Vp) was calculated according to Vp = (W2−W3−Ws)/ρHg, where W3 is the weight of left pycnometer and mercury when the sample was took out carefully. The porosity of the scaffold was calculated according to ε = Vp/(Vp + Ws/ρs).
Compression tests
The compressive strength test of the samples was carried out by computer controlled DXLL-5000 tensile machine (Chemical Machinery Co., Shanghai, China). The specimens were disk-shaped with a diameter of 16 mm and 3 mm thick. The crosshead speed was 1 mm/min. Compressive strength was calculated according the following equation: \( \sigma \, = \,\frac{P} {A} \), where σ is compressive strength (MPa); P is the compression load when the specimen thickness reaches to 1 mm (N); A is cross-sectional area (mm2). Five specimens were tested for each sample and the average values were taken in this work.
Cell and culture conditions
Sprague-Dawley rat fibroblasts were cultured in Dulbecco’s modified Eagle’s medium (DMEM, Gibco) supplemented with 10% fetal bovine serum (FBS) in a humidified incubator at 37 °C and 5% CO2. Third-passage cells were used for the experiments.
Medium extract cytotoxicity
The PDLLA/NHA scaffolds were cut into small squares (length: 6 × breadth: 6 × height: 2 mm) for the in vitro cytotoxicity experiments after ethylene oxide (EO) sterilization. Each disc was extracted with DMEM (3 cm2/mL) for 24 h at 37 °C, in a 5% CO2 incubator. Several doses of extracted medium were prepared by serial dilutions with fresh medium to 1, 10, 25, 50 and 100% (original extract solution). Phenol represented the positive chemical control (0.64% v/v phenol solution; Sino-American Biotechnology Company, China). DMEM was chosen as the negative control. Third-passage SD rat fibroblasts were suspended at the concentration of 1 × 105 cells/mL, and the cells suspension were inoculated in 96-well plate (200 μL/well). The cells were cultured in a humidified incubator at 37 °C and 5% CO2, after the cells adhered on the wells, the culture medium was removed and replaced by serial diluted extracts and control solutions. The cell morphology and proliferation were observed with different cultivation time (24 h and 48 h) by inverted phase contrast microscope (Leica model: DM IRB, Shanghai).
Direct contact cytotoxicity
Different NHA content (2% and 4%) PDLLA/NHA scaffolds were cut into 6 small squares (length: 5 × breadth: 5 × height: 2 mm) respectively, and placed into DMEM prewetted for 24 h, then air-dried for use. Third-passage SD rat fibroblasts (1 × 105 cells/mL) were inoculated in 48-well plate (500 μL/well), and cultured in a humidified incubator at 37 °C and 5% CO2 till they form a monolayer. Then culture medium was aspirated and test pieces were placed carefully on the monolayer in minimum culture medium. Cultures were incubated for 24 h and 48 h, morphology of cells was assessed using inverted phase contrast microscope.
Following 24 h and 48 h incubation periods, the cell viability was measured using the MTT (3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-[2H]-tetrazolium bromide) assay. Selecting 3 wells in each group and 20 μL MTT dye (5 mg/mL) was added to each well and incubated for 4 h at 37 °C and 5% CO2. Then, 200 μL dimethyl sulfoxide solution (DMSO, Sino-American Biotechnology Company, China) was added to dissolve the formazan crystals. The absorbance values of the formazan solutions were measured using an Enzyme Linked Immunosorbent Assay microplate reader at 570 nm (ELx800, Bio-Tek Instruments, Inc.). Three absorbance values of each group were tested and the results were averaged, and the cell relative growth rate (RGR) was calculated according to following equation: \( {\text{RGR = }}\,\frac{{{\text{PG}}\,{\text{OD}}\, - {\text{BG}}\,{\text{OD}}}} {{{\text{NG}}\,{\text{OD}}\, - {\text{BG}}\,{\text{OD}}}}\, \times \,100\% \), where PG OD is positive group (PG) optical density (OD); NG OD is negative group (NG) optical density (OD); BG OD is blank group (BG) optical density (OD).
Systemic toxicity test
Institute of Cancer Research Rats (ICRRs), male or female, 6–8 weeks old, weighing 20–25 g were used for the systemic toxicity tests. The tests were conducted upon visual observations of animals that had received a large dose of extraction prepared with aforesaid method. Nine ICRRs were divided into three groups stochastically and extracts of scaffolds were administered by intraperitoneal injection to groups of three mice, which were then weighed. Control mice were injected with saline alone. For the next three days the mice were observed for adverse signs, such as convulsions or prostration, and were weighed daily.
Local implantation response evaluation
Square scaffolds (length: 5 × breadth: 5 × height: 2 mm) sterilized with EO and washed in sterile phosphate-buffered saline (PBS) (pH 7.2) at 22 °C. Nine ICRRs were divided into three groups stochastically and anaesthetized by intraperitoneal injections of 50 mg/kg body weight of a solution containing sodium pentobarbital (0.3%). After disinfection, subcutaneous pockets were made to the right and left of two midline incisions on the back. The scaffolds were implanted in the pockets at a distance of about 1 cm from the incisions (4 implants/rat). For each implantation time, one rat received two pieces of the same scaffold on one side of the midline incision and another scaffold two pieces on the other side. Implants with surrounding tissue were harvested from ICRRs and stained with hematoxylin (HE) for histological evaluation at 1 and 9 weeks after implantation.
Results and discussion
The preparation of PDLLA/NHA composites
Figure 1 shows the molecular weight of PDLLA and different NHA content PDLLA composites determined by GPC. The molecular weight of composites dramatically decreased with increasing of NHA content, and polymerization even cannot take place when NHA content exceeds 4% in polymer matrix. Lactide ring-open polymerization is very sensitive to some nucleophilic radicals and molecules. As reported in the literature, these molecules and radicals will cause chain initiation and termination at high temperatures, and this may be the primary reason for the low molecular weights [33].
The SEM and TEM micrographs of PDLLA/NHA composites (Fig. 2) show that NHA particles distribute in PDLLA matrix uniformly, however, the slight agglomeration still can be observed, which may be caused by the high surface energy of NHA. These particles have a great inclination for agglomeration, especially during melt compounding with polymers that are usually characterized by high viscosity [34]. Figure 3 shows the water adsorption ratio curves of PDLLA/NHA scaffolds with 2% and 4% NHA weight content. The water adsorption ratio of all the materials increases with soaking time, however, the increase rate decrease. The water adsorption ratio of scaffold materials enhanced obviously with NHA content increasing in polymer matrix at same soaking time in water. It indicates that a few NHA particles can improve the hydrophilic ability of scaffolds dramatically, which may be caused by high specific surface area of NHA particles.
The incorporation of NHA will lead to a composite with better bone-bonding properties. To investigate whether NHA can do some contribution to the compressive strength of composites, compressive strengths of composite foams of different NHA content (2 wt%, 4 wt%) were studied as shown in Fig. 4. Figure 4 shows that the pure PDLLA had a low compressive strength of 729 KPa. With the addition of NHA (though the molecular weight of composite foams decreased as shown in Fig. 1), the compressive strength increased. When the NHA content is 2 wt%, the compressive strength increases 17% compared to pure PDLLA. For PDLLA /NHA composite of 4 wt% NHA content, the compressive strength increased 39.2%.
The fabrication of high porosity scaffolds
As shown in Fig. 5, the porosity of the scaffolds reach 83.17 ± 2% according to the calculation method described in 2.7. Saturation pressure of supercritical CO2 has effects on both morphology and porosities of PDLLA /NHA composite scaffolds. When the pressure increases from 8 MPa to10 MPa, there is no obvious change on the porosity and pore size. But when the pressure reaches 14 MPa, most of pores are damaged and no uniform pores can be observed. In the pressure ranges of 8 to10 MPa, CO2 density as well as the amount of CO2 in the system is the key factor that affects matrix porosities. At a slightly higher pressure, CO2 density is denser; more CO2 gas will be absorbed in the composite composites, which leads to more CO2 bubbles formed in the matrix, and a little higher porosity. But keeping on increasing of pressure leads to more pores collapse and so the porosity of composites will decrease. This is probably due to the amorphous structure of PDLLA, which is easily destroyed at higher pressure for its random chain arrangement. The porosities of PDLLA/NHA composite scaffolds will increase with the increasing of saturation time. It is because that the longer the polymer is exposed to the high pressure CO2, the greater the amount of CO2 absorbed by the polymer, which increases the amount of larger bubbles to form the porous of composites. However, when CO2 reaches the saturation in the matrix, the prolonged time has minor effects on porosity. In general, the effect of temperature on the porosity of matrix is not as significant as other parameters such as salt ratio, saturation pressure, etc.
In vitro cytotoxicity evaluation
Rat fibroblast were cultivated in different scaffold extracts, and observed at 24 h and 48 h with inverted phase contrast microscope respectively. As shown in Fig. 6, these cells of experiment groups and negative groups had normal growth morphology and attached well on the bottom of the culture plate at 24 h. The fibroblast proliferated rapidly and overspread the bottom of the culture plate after changing medium 48 h.
The MTT assay revealed that the extracts of all the materials in study affected the viability of fibroblast cells. Following 48 h incubation periods, the cell viability was measured using the MTT assay, and the cell relative growth rate (RGR) reach 82.6% and 79.6% respectively in two group medium extraction (Fig. 7.). The cytotoxicity of these scaffolds was in grade I according to ISO 10993-1, that means these kind of materials have very good cytocompatibility.
The materials were placed in contact with cells during different time periods in order to identify morphological changes resulting from this contact and to see how cells were adhered and spread on the material. Some fragments of cells can be observed after loading materials 24 h, and the fibroblast cells have normal growth morphology around the materials. After 48 h, cells proliferated actively and densely assembled around the materials.
In vivo composite materials evaluation
There were no toxicosis and death cases observed after implanting operation, and the local wound dropsy alleviated after 3 days. The cut healed up after implanting operation 7 days, and the wound covered by hair. Normal activities of tested rats can be observed. Histopathological observation was done after implanting operation for 1 week and 9 weeks. As shown in Figs. 8 and 9, a great deal of neutrophils, lymphocytes and macrophages can be observed in musculature after 1 week of implanting operation, but no tissue grew into the pores of implanted materials. After 3 weeks the number of neutrophils and lymphocytes reduced, however, abundant macrophages still can be observed around implanted materials, the number of macrophages reduced obviously and a few neutrophils and lymphocytes still being after 9 weeks of implanting operation. Fiber cyst can be observed at any observation time. As observed, there was no obvious difference in tissue response between 2 wt% PDLLA/NHA and 4 wt% PDLLA/NHA.
Acute systemic toxicity was investigated by scaffold extracts intraperitone injection. There were no toxicosis and death cases observed in gross observation at 5 min and 24 h respectively.
Conclusions
In the present work, various PDLLA/NHA composites were prepared by in-situ polymerization of NHA and lactide monomer. Scaffolds with high porosity and pore sizes about 250 μm were fabricated through SC CO2/SL. The interconnected macropore structure is very suitable for cell seeding. The evaluation of PDLLA/NHA composite materials on cytotoxicity were carried out by cell relative growth rate (RGR) method and cell direct contact method. The cytotoxicity of these scaffolds was in grade I according to ISO 10993-1. PDLLA/NHA composites show better hydrophilic ability, enhanced mechanical properties and excellent biocompatibility than PDLLA materials, and the inflammatory response of tissue after implanting, which may be caused by degradation products, lightened by introducing NHA in PDLLA polymer matrix. So PDLLA/NHA nanocomposites are very attractive in tissue engineering field.
References
F. R. A. J. ROSE and R. O. C. OREFFO, Biochem. Biophys. Res. Comm. 292 (2002) 1
R. F. SERVICE, Science 289 (2000) 1498
J. R. JONES and L. L. HENCH, Mater. Sci. Technol. 17 (2001) 891
R. LANGER and J. P. VACANTI, Tissue Eng. Sci. 260 (1993) 920
Y. TABATA, Drug Discov. Today 6 (2001) 483
A. DENUZIERE, D. FERRIER, O. DAMOUR et al., Biomaterials 19 (1998) 1275
R. K. KULKARNI, K. C. PANI, C. NEUMAN et al., Arch. Surg. 93 (1966) 839
D. E. CUTRIGHT and E. E. HUNSUCK, Oral Surg. Oral Med. Oral Pathol. 31 (1971) 134
A. MAJOLA, S. VAINIONAPAA, K. VIHTONEN et al., Clin. Orthop. Relat. Res. 268 (1991) 260
S. L. SHAUG, G. M. CRANE, M. J. MILLER et al., J. Biomed. Mater. Res. 36 (1997) 17
T. B. REN, J. REN, K. F. PAN et al., J. Biomed. Mater. Res. Part A. 74 (2005) 562
L. G. GRIFFITH, Acta. Mater. 48 (2000) 263
C. M. AGRAWAL and R. B. RAY, J. Biomed. Mater. Res. 55 (2001) 141
Y. SHIKINAMI and M. OKUNO, Biomaterials 20 (1999) 859
L. L. HENCH, J. Am. Ceram. Soc. 81 (1998) 1705
P. SEPULVEDA, J. R. JONES and L. L. HENCH, J. Biomed. Mater. Res. 61 (2002) 301
A. R. BOCCACCINI, J. A. ROETHER and L. L. HENCH et al., Ceram. Eng. Sci. Proc. 23 (2002) 805
C. T. LAURENCIN, H. H. LU, In Bone Engineering, edited by J. E. Davies, (Toronto, Canada: Em Squared Incorporated 2000), p. 462
A. G. MIKOS, L. A. THORSEN, L. A. CZERWONKA, Y. BAO and R. LANGER, Polymer 35 (1994) 1068
H. LO, M. S. PONTICIELLO and K. W. LEONG, Tissue Eng. 1 (1995) 15
L. E. FREED, G. VUNJAK-NOVAKOVIC, R. J. BIRON, D. B. EAGLES, D. C. LESNOY, S. K. BARLOW and R. LANGER, Bio/Technology 12 (1994) 689
J. J. YOON and T. G. PARK, J. Biomed. Mater. Res. 55 (2001) 401
Y. S. NAM and J. J. YOON, J. Biomed. Mater. Res. 53 (2000) 1
L. SINGH and V. KUMAR, Biomaterials. 25 (2004) 2611
D. J. MOONEY, D. F. BALDWIN, N. P. SUH, J. P. VACANTI and R. LANGER, Biomaterials. 17 (1996) 1417
L. D. HARRIS, B. S. KIM and J. M. DAVID, J. Biomed. Mater. Res. 42 (1998) 396
Q. XU, X. REN, Y. CHANG, J. WANG, L. YU and D. KATHERINE, J. Appl. Polym. Sci. 94 (2004) 593
J. WANG, X. G. CHENG, M. J. YUAN and J. S. HE, Polymer 42 (2001) 8265
D. D. HILE and M. LEE, J. Control. Rel. 66 (2000) 177
J. S. CHIOU, J. W. BARLOW and D. R. PAUL, J. Appl. Polym. Sci. 30 (1985) 2633
S. K. GOEL and E. J. BECKMAN, Polymer 34 (1993) 1410
M. H. SHERIDAN, L. D. SHEA, M. C. PETERS and D. J. MOONEY, J. Control Rel. 64 (2000) 91
Y. X. LIU and C. U. J. PITTMAN, J. Polym. Sci. Part A: Polym. Chem. 35 (1997) 3655
L. F. CAI, X. B. HUANG, M. Z. RONG, W. H. RUAN and M. Q. ZHANG, Polymer 47 (2006) 7043
Acknowledgments
The project is sponsored by the key basic research foundation for development of science and technology of Shanghai, P.R. of China (Number: 05DJ14006), the research foundation for nano science and technology special project of Shanghai (Number: 0452nm088). Contract grant sponsor: Key Basic Research Foundation for Development of Science and Technology of Shanghai, P.R. of China; contract grant number: 05DJ14006. The research foundation for nano science and technology special project of Shanghai P.R. of China; contract grant number: 0452nm088.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ren, J., Zhao, P., Ren, T. et al. Poly (d,l-lactide)/nano-hydroxyapatite composite scaffolds for bone tissue engineering and biocompatibility evaluation. J Mater Sci: Mater Med 19, 1075–1082 (2008). https://doi.org/10.1007/s10856-007-3181-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-007-3181-8