Abstract
Periprosthetic osteolysis is a major clinical problem that limits the long-term survival of total joint arthroplasties. Particles of prosthetic material stimulate immune competent cells to release cytokines, which may cause bone loss and loosening of the prosthesis. This study examined the following hypothesis. Polyethylene and titanium particles elicit a different immune response in vitro. To test these hypotheses, we used the human bone marrow cell culture model that we have established and previously used to examine particle associated cytokine release. Ultra high molecular weight polyethylene (UHMW-PE) induced a proliferation of CD14 positive cells (monocytes/macrophages) whereas cobalt chromium molybdenium (CoCrMb) particles demonstrated an increased proliferation of CD66b positive cells (granulocytes). Light and scanning microscopic evaluation revealed that the UHMW-PE particles, which have built large clusters of particles (Ø7, 5 μm), were mainly surrounded by the cells and less phagocytosed. On the other hand the smaller particles from CoCrMb have been phagocytosed by the cells. These results provide strong support for our hypothesis: that wear particles derived from prosthetic materials of different material can elicit significantly different biologic responses. In summary the results suggest that the “in vitro” response to wear particles of different biomaterials should be investigated by culture systems of various lineages of cells.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Aseptic loosening of prosthetic joint replacements is still a major problem in orthopaedic surgery. Histological investigations have shown that wear particles were present in a large number in the periarticular tissue and are a characteristic feature of loose joint prostheses [1–6]. Wear particles are mainly produced by the articulating surfaces of the artificial joint. Additionally micro movement of an endoprosthesis against the surrounding bone and/or cement may produce other particles. The predominant type of particle in periprosthetic tissues retrieved from patients with aseptic loosening is ultrahigh molecular weight polyethylene (UHMWPE) derived from wear of the bearing surface.
In vitro studies have already shown the capability of wear particles to induce the activation of monocytes and macrophages. Small particles (sub-μm) are phagocytosed by these cells inhibiting their differentiation into osteoclasts [7, 8]. Larger particles (>10 μm) that cannot be phagocytosed, however, induce the development of foreign body granulomas that lead to a chronic inflammation, causing the formation of osteolytic lesions in the periprosthetic bone.
The need to establish and investigate the differences in response to different wear particulate implant materials first was recognized several decades ago by Cohen et al. [9].
T lymphocytes have been found in periprosthetic tissue from patients with aseptic loosening [10]. However, the available in vivo an in vitro models have not determined whether lymphocytes contribute to the biological effects of wear particles. For example, macrophage recruitment and granuloma formation are similar in lymphocyte-deficient and wildtype rodents following chronic subcutaneous exposure to polymethylmethacrylate or high-density polyethylene particles [11, 12]. In contrast, injection of UHMWPE particles into the knee joint causes acute inflammation in wild-type mice but not in lymphocyte-deficient mice [13].
Numerous recent studies have attempted to compare the ability of different types of particles to induce different amounts of a range of cytokines [14–18]. It remains unclear whether the cytokine response to orthopaedic wear is an expression of cell activation or cell differentiation.
Within the present study, we test the hypothesis that the differentiation behaviour of human bone marrow cells especially the white cell lineages under the influence of cobalt–chromium–molybdenium (CoCrMb) and ultra-high-molecular weight polyethylene (UHMW-PE) wear particles are different. Because the prosthesis, in case of a total hip replacement, is implanted in the femoral shaft, in this study a heterogenous cell culture model consisting of human bone marrow cells was used [6, 19, 20]. This culture system allows the investigation of effects on either the haematopoetic or the lymphopoetic compartments during the culture period. Therefore it may serve as a suitable model to investigate the immune modulation of human bone marrow cells in response to orthopaedic wear particles in vitro.
Materials and methods
Particle production and preparation of the wells
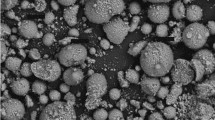
Mainly commercially available particles were used and kindly provided by Zimmer Surgery (Warsaw, IN, USA). The CoCrMb particles had an average size of ≤2.25 μm in diameter (range 1.5–3.0 μm). The size of the UHMW-PE particles range from 0.5 to 3.0 μm, however, the particles were present as clusters of particles with an average size of ≤7.5 μm.
Particle preparation and media used in this study was endotoxin-free (measured using the LAL-test Aventis Behring, Marburg, Germany), indicating that the effects seen in this study were caused by the particles. Particle sizes were confirmed using scanning electron microscopic analysis.
Before use, the UHMW-PE particles were fixed to the bottom of the wells by a collagen type 1 solution (Fa. Becton-Dickenson, Bedford, MA, USA) because of their low density [19]. To exclude an effect on the cell differentiation by collagen type 1 human bone marrow cells were cocultured with collagen type 1, without particle stimulation.
Cell isolation and culture
To investigate the differentiation behaviour of immune competent cells in vitro a culture system of human bone marrow cells was used [6, 19].
The human bone marrow was taken under sterile conditions from the metaphyseal portion of the proximal femur during total hip arthroplasty (Performed according to the guidelines for experimentation with human cells and approved by the ethical commission AZ 44/99).
The spongious bone block had an average size of 7 mm × 10 mm × 20 mm and was kept in a heparin containing phosphate buffered saline solution. Subsequently, the bone block was morsellized and sieved (pore size: 0.1 mm) to separate the cancellous bone particles. The obtained cell suspension was centrifugated (800 g, 10 °C) in a Ficoll-Histopaque density gradient (ratio: 2:1,density: 1.077 g/mL) for 20 min, the interphase was retrieved and the gradient mixture was washed twice with PBS. Afterwards the human bone marrow cells were seeded at densities of 3 × 106 cells per well (6 well bottom-9.81 cm2) and grown in an Iscove´s modified Dulbeccos Medium (IMDM, Life-Technologies, Paisley, Scotland), supplemented with 12.5% foetal calf serum (Boehringer, Mannheim, Germany), 12.5% horse serum (Boehringer, Mannheim, Germany)and 10.0 ng/mL medium growth factors (Interleukin 3 [IL-3] (Behring AG, Marburg, FRG) and granulocyte-macrophage-colony-stimulating-factor [GM-CSF] (Behring AG, Marburg, FRG). The cultures were incubated at 37 °C, 12.5% O2, 5% CO2 and 0% N2.
In the present study the time of culture was set to 6 days. The medium (IMDM) was changed every day. All donors were tested individually and the results expressed as the average of each of these values.
Cell morphology
Giemsa staining was used as a fast and easy staining method to do a differential staining of the bone marrow cells after the period of 6 days. The cultures were fixed with 70% ethanol for 30 min and stained with 10% giemsa solution for 45 min at room temperature. Afterward the stained cultures were dried and preserved with entellan and cover slips.
The acridine-orange staining was used to differentiate between vital and avital cells in vitro. The cells were incubated for 5 min at room temperature, washed twice and preserved with cover slips.
The distribution and morphology of the cultures were analyzed by SEM (scanning electron microscopy). After 6 days, surface adherent cells were fixed with a 2% ITO-Fixative (0.2 M cacodylate buffer/aqua dest/25.0% glutaraldehyde) for 1 h at room temperature. Dehydration was performed by sequential immersion in serial diluted ethanol solutions of 50,50,70,80,90 and 100% v/v and dried in a critical point chamber (Balzer Union, Lichtenstein) by exchanging the acetone against liquid carbon dioxide. Finally the specimen were sputter-coated with gold using a sputter coater (Edwards, West Sussex, UK), and observed using a ISI SX 30 scanning microscope (ISI, Great Britain).
Cell differentiation (fluorescence activating cell sorter-FACS)
To assess changes of the cell differentiation of the human bone marrow cells in the presence of particulate debris a FACS analysis was done on the day of preparation and after 6 days. The cells were removed by Accutase® (Fa. PAA Linz, Austria), visualized by light microscopic analysis and counted by the Casy® 1 TTC system (Fa. Schärfe Systems GmbH Germany). The Cell Counter + Analyser Model TTC works in combination with the electronic pulse area analysis of Schärfe System. The cell and particle concentration, all information on the diameter and the volume of the analysed sample is provided.
Thereafter the cells were incubated at 37 °C with antibodies against specific surface antigens of immune competent cell lineages for 2 h. An additional CD45 antibody marking was done to ensure that the expression of the investigated CD antibodies happened on the leukocyte population.
-
CD4 FITC; Fa. Becton Dickinson.
CD4 positive cells = T-lymphocytes;
-
CD14 FITC; Fa. Becton Dickinson.
CD14 positive cells = monocytes/macrophages
-
CD19 FITC; Fa. Becton Dickinson.
CD19 positive cells = B-lymphocytes
-
CD34 PE; Fa. Becton Dickinson.
CD34 positive cells = haematopoetic stemcells
-
CD66b FITC; Fa. Becton Dickinson.
CD66b positive cells = granulocytes
The results were represented by Dot Blot. To exclude a misinterpretation of the results, a control assay informs about unspecific bindings and allows the calibration of the system. The data interpretation was done using the software program BD CellquestTM Pro v.4.0.2.
Statistical analysis
Particulate debris was applied to the dishes in different concentrations ranging from 1 × 105 to 1 × 108 per mL medium. For each particle concentration six dishes were analysed. Human bone marrow cells were isolated from six healthy donors (3 male and 3 female patients; ranging age from 45–60 years). In summary each particle concentration was measured six-fold for each donor.
Data were represented as the mean ± SD of six measurements which have been produced for each of the 6 patients who were part of the experiments. To verify the significance of our data a two-way ANOVA-test was used. A p value of less than 0.05 was considered statistically significant.
Results
Cell morphology
Light- and scanning electron microscopy revealed two different reactions by the human bone marrow cells: (a) Smaller wear particles like particulate CoCrMb (∼1 μm) became phagocytosed and (b) clusters of particles of particulate UHMW-PE (∼7.5 μm) which were mainly present were surrounded by cells but not phagocytosed. Giemsa staining approved these findings (Figs. 1 and 2).
The acridine-organge staining demonstrated the particle concentration dependent decrease of vital cells in case of CoCrMb as well as UHMW-PE without being significant.
FACS analysis
Since previous studies have already shown constant populations of CD4, CD14, CD19, CD34 and CD66b positive cells in vitro over a period of 14 days, a new analysis was not performed [21]. The amount of vital cells was determined before analysing and interpreting the composition of the cell population (Table 1).
The results of the FACS analysis revealed a significant elevation of CD 14 positive (monocytes/macrophages) cells (p < 0.01) and a significant decrease of CD positive(B-cells) cells (p < 0.05) for cultures being stimulated by UHMW-PE. An influence on the differentiation of CD 66b (granulocytes) positive and CD 34 positive (haematopoetic stem cells) cells by UHMW-PE was not detectable (p > 0.05).
In case of particulate CoCrMb a significant increase of CD 66b positive cells could be revealed (p < 0.05). The differentiation of CD 34 positive, CD 19 positive and CD 2 positive cells remained unchanged under the influence of CoCrMb (p > 0.05). In case of CD 14 positive cells the decrease was more evident but not significant at all (p > 0.05) [Fig. 3].
Discussion
Aseptic loosening of a prosthetic material is one of the major reason for prosthetic implant failure [7, 22]. The longevity of prosthetic implants depends on numerous factors that are determined by the surgeon, by the implant and by the host reaction to the implant.
Metal-on-metal prostheses generate less volumetric wear than comparable metal-on-polyethylene prostheses do [21]. The particles produced are, however, orders of magnitude smaller and therefore as many as 100 times more particles are produced by metal-on metal as compared with metal-on-polyethylene bearings [23]. Lymphocytic infiltration also has been observed in periprosthetic tissues obtained during revision of metal-on metal joint-replacement implants. Willert and Semlitsch [24] reported infiltrates of lymphocytes and plasma cells in the absence of evidence of bacterial infection in some tissues in their series of first-generation metal-on-metal prostheses. Similar features were then found in tissues retrieved from hips with contemporary metal-on-metal prostheses that had failed at an average of thirty months after implantation [10, 25]. Other authors have reported individual cases of lymphocytic infiltration around failed modern metal-on-metal implants [26]. In contrast, infiltrates of lymphocytes or plasma cells have not been reported in studies of tissues from around metal-on polyethylene [4, 27, 28] ceramic-on-ceramic [10, 25] prostheses. Boss et al. [29] described “inflammatory infiltrates” including white blood cells around failed short-term cemented metal-on-polyethylene hip replacements, but they concluded that the predominant cell species present in periprosthetic tissues were macrophages and giant cells.
Whereas the effect of wear debris on various cell kinds has been studied extensively and the effect on the release of proinflammatory cytokines is well established, [14–18] effect on the differentiation of human bone marrow cells is less clear.
The purpose of the present study was to test the hypothesis whether UHMW-PE and CoCrMb wear may elicit a different immune response in vitro. Is the cytokine release only a phenomenon of cell activation or is it an expression of immune modulation?
This study provides strong support for the hypothesis that different cell types of the white cell lineage play a major role in particle-induced osteolysis.
The majority of the UHMW-PE particles has been shown to be submicron but mainly present in clusters of particles. Two different types of cellular responses could be observed in vitro. Small particles were phagocytosed while larger particles were surrounded by foreign body giant cells, which was reproducibly demonstrated in our culture system with particulate UHMW-PE (cluster of particles > 7.5 μm) and CoCrMb (<1 μm).
Using particulate UHMW-PE it was demonstrated that after a period of 6 days an increased proportion of macrophage/monocytes (CD 14 positive) and a decreased proportion of b-cells (CD-19 positve) was evident. The response to CoCrMb wear particles was different. It could be shown that the proportion of granulocytes/macrophages (CD66b positive) was increased. Other cell populations remained unchanged. An influence by the composition of the used medium could be excluded as previously shown [6, 19].
To assess whether the observed effects of particles on the increase or decrease of the investigated cell populations are at least partially caused by a decrease in cell number, the cell count was done before the FACS analysis. Only if highest concentrations of CoCr particles were cocultured with the human bone marrow cells a decrease was observable.
The results of Al Saffar et Revell which have shown by immunohistochemistry on tissue sections retrieved during revision of loosened total joint prosthesis an extensive number of IL-1 producing cells like macrophages and monocytes confirm the data presented herein. Moreover they found no evidence for the presence of B-lymphocytes [26].
The absence or minor role of B-lymphocytes has also been demonstrated by an investigation of Salter et al, which have analyzed pseudomembranes retrieved of late prosthetic joint failures [30].
The current results are also consistent with a recent study from Epstein et al and Davies et al. Epstein et al have demonstrated that addition of UHMW-PE particles to a retrograde inserted stainless steel Kirschner wire in femora of mice stimulated ingress of monocytes to the bone implant interface [31].
Davies et al could show that tissue samples retrieved from hips with metal-on-metal implants displayed an accumulation of plasma cells in association with macrophages that contained metallic wear-debris particles. Tissue samples obtained from hips with metal-on-polyethylene implants showed no pattern of lymphocytic infiltration, and no plasma cells. The inflammation was predominantly histiocytic [32].
Although investigations of periprosthetic tissue confirm the in vitro effects from UHMW-PE and CoCrMb as seen in the present study the influence on osteoblast-osteoclast cooperation remains unanswered. The long-term stability of arthroplasty prosthesis depends on the integration between osseous tissue and the implant material. This requires the contribution of mesenchymal stemcells and their differentiation into an osteoblastic phenotype.
The data presented herein suggest that different cellular events take place in human bone marrow if exposed to small (sub-μm) and large (>10 μm) wear particles. Small particles are phagocytosed, inhibiting the differentiation of macrophages into osteoclasts [7, 8, 33]. In addition, simultaneous inhibitory effects on the development of osteoblasts occur mediating the antiosteoclastogenic effects.
Larger particles that cannot be phagocytosed induce the development of foreign body granulomas, as shown in this study, that lead to a chronic inflammation, recruiting activated inflammatory cells and potential osteoclast progenitors to the periprosthetic site [27, 34].
In summary, this is the first in vitro study showing that wear particles shed from polyethylene and titanium can elict a different immune response in vitro. These findings suggest that the in vitro response to wear particles of different biomaterials should be investigated by culture systems of various lineages of cells. A control of the local leukopoietic environment and the prevention of large wear particles may delay or prevent the formation of osteolytic lesions.
References
S. R. GOLDRING, A. L. SCHILLER, M. ROELKE, C. M. ROURKE, D. A. O’NEIL and W. H. HARRIS, J. Bone Joint Surg. Am. 65(5) (1983) 575
K. J. KIM, J. CHIBA and H. E. RUBASH, J. Bone Joint Surg. Am. 76(2) (1994) 172–80
K. J. KIM, T. ITOH, M. TANAHASHI and M. KUMEGAWA, J. Biomed. Mater. Res. 32(1) (1996) 3–9
J. M. MIRRA, H. C. AMSTUTZ, M. MATOS and R. GOLD, Clin. Orthop. Relat. Res. (117) (1976) 221
T. P. SCHMALZRIED, M. JASTY, A. ROSENBERG and W. H. HARRIS, J. Appl. Biomater. 5(3) (1994) 185
A. WILKE, J. ORTH, M. LOMB, R. FUHRMANN, H. KIENAPFEL, P. GRISS and R. P. FRANKE, J. Biomed. Mater. Res. 40(2) (1998) 301
S. D. NEALE, D. R. HAYNES, D. W. HOWIE, D. W. MURRAY and N. A. ATHANASOU, J. Arthroplasty 15(5) (2000) 654
A. S. SHANBHAG, J. J. JACOBS, J. BLACK, J. O. GALANTE and T. T. GLANT, J. Biomed. Mater. Res. 28(1) (1994) 81
J. COHEN, J Bone Joint Surg. Am. 41-A(1) (1959) 152
H. G. WILLERT, G. H. BUCHHORN, A. FAYYAZI and C.H. LOHMANN, Vascular changes and lymphocyte aggregations in aseptic loosening of all-metal hip joint replacements Presented as a poster at the Sixth World Biomaterials Congress; (2000) May 15–20; Kamuela, HI
S. GOODMAN, J. WANG, D. REGULA and P. ASPENBERG, Acta. Orthop. Scand. 65 (1994) 15740
W. A. JIRANEK, M. MACHADO and M. JASTY et al J. Bone Joint Surg. 75A (1994) 863
J. SANDHU, J. E. WADDELL, M. HENRY and E. L. BOYNTON, J. Rheumatol. 25 (1998) 1794
B. D. BOYAN, R. BATZER, K. KIESWETTER, Y. LIU, D. L. COCHRAN, S. SZMUCKLER-MONCLER, D. D. DEAN and Z. SCHWARTZ, J. Biomed. Mater. Res. 39(1) (1998) 77
E. BOYNTON, J. P. WADDELL, J. MORTON and G. W. GARDINER, Can. J. Surg. 34(6) (1991) 599
E. L. BOYNTON, M. HENRY, J. MORTON and J. P. WADDELL, Can. J. Surg. 38(6) (1995) 507
J. CHIBA, W. J. MALONEY, K. INOUE and H. E. RUBASH, J. Arthroplasty. 16(8 Suppl 1) (2001) 101
D. W. HOWIE, D. R. HAYNES, S. D. ROGERS, M. A. MCGEE and M. J. PEARCY, Orthop. Clin. North Am. 24(4) (1993) 571
H. MALCHAU, P. HERBERTS, T. EISLER, G. GARELLICK and P. SODERMAN, J. Bone Joint Surg. Am. 84-A(Suppl 2) (2002) 2. Erratum in: J. Bone Joint Surg. Am. 86-A(2) (2004) 363
H. MALCHAU, P. HERBERTS, L. AHNFELT, Acta. Orthop. Scand. 64(5) (1993) 497
H. P. SIEBER, C. B. RIEKER and P. KOTTIG, J. Bone Joint Surg. Br. 81 (1999) 46
L. T. NILSSON, H. FRAZEN, A. S. CARLSSON and R. ONNERFALT, J. Bone Joint Surg. Br. 76(2) (1994) 235
P. J. FIRKINS, J. L. TIPPER, M. R. SAADATZADEH, E. INGHAM, M. H. STONE, R. FARRAR and J. FISHER, Biomed. Mater. Eng. 11 (2001) 143
H. G. WILLERT and M. SEMLITSCH, Clin. Orthop. 333 (1996) 4
H. WILLERT, G. BUCHHORN, A. FAYYAZI and C. LOHMANN, Osteologie 9 (2000) 2
N. Al SAFFAR and P. A. REVELL, Br. J. Rheumatol. 33(4) (1994) 309
K. HEILMANN, P. B. DIEZEL, J. A. ROSSNER and K. A. BRINKMAN, Virchows Arch. A Pathol. Anat. Histol. 366 (1975) 93
H. G. WILLERT, J. Biomed. Mater. Res. 11 (1977) 157
J. H. BOSS, I. MISSELEVICH, J. BEHAR and D. G. MENDES, J. Long Term Eff. Med. Implants 6 (1996) 73
D. M. SALTER, A. S. KRAJEWSKI and S. ROBERTSON, J. Pathol. 166(3) (1992) 271
N. J. EPSTEIN, W. E. BRAGG, T. MA, J. SPANOGLE, R. L. SMITH and S. B. GOODMAN, Acta. Orthop. 76(3) (2005) 412
A. P. DAVIES, H. G. WILLERT, P. A. CAMPBELL, I. D. LEARMONTH and C. P. CASE, JBJS Am 87 (2005) 18
A. S. SHANBHAG, J. J. JACOBS, J. BLACK, J. O. GALANTE and T. T. GLANT, J. Orthop. Res. 13(5) (1995) 792
R. PANDEY, J. QUINN, C. JOYNER, D. W. MURRAY, J. T. TRIFFITT and N. A. ATHANASOU, Ann. Rheum. Dis. 55(6) (1996) 388
Acknowledgements
The Authors wish to thank the Deutsche Arthrosehilfe e.V. Conflict of interest statement: All authors certify they not have signed any agreement with a commercial interest related to this study which would in any way limit publication of any and all data generated for the study or to delay publication for any reason. I confirm that all authors have seen and agree with the contents of the manuscript and agree that the work has not been submitted or published elsewhere in whole or in part.
Ethical Board Review statement: Performed according to the guidelines for experimentation with human cells and approved by the ethical commission AZ 44/99.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Endres, S., Bartsch, I., Stürz, S. et al. Polyethylene and cobalt–chromium molybdenium particles elicit a different immune response in vitro. J Mater Sci: Mater Med 19, 1209–1214 (2008). https://doi.org/10.1007/s10856-007-3104-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-007-3104-8