Abstract
Percutaneous devices are extensively used in modern medicine therapies, even in long term applications. Complications from their use, related to bacterial colonization and/or to materials thrombogenicity, may result in a significant morbidity and mortality incidence. In this study, a novel polycarbonate-urethane (PCU), incorporating a tailor-made diamino-diamide-diol (PIME) showing the ability to bind heparin at physiological pH, was compared to commercial medical-grade PCUs (Carbothane® and Bionate®). Mechanical and thermal properties were evaluated by tensile tests, dynamic mechanical analysis and differential scanning calorimetry. The presence of a low amount of PIME chain extender in Bionate® polyurethanes (Bionate-PIME) slightly affects the mechanical properties, remaining however comparable with the medical grade PCUs used for the fabrication of cardiovascular devices. To verify thereof heparin surface adsorbed in disfavouring bacterial colonization, heparinized Bionate-PIME was tested for bacterial adhesion, using Bionate® and Carbothane® as reference. In vitro bacterial interaction tests were performed with the strains mainly involved in the pathogenesis of device-related infections (S. epidermidis and S. aureus). MTT tests and SEM observations showed a decrease in colonization of the different strains on the heparinized Bionate-PIME surfaces, confirming that preadsorbed heparin plays a role in mediating the biomaterial surface/bacterial cells interactions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intravascular devices have become usual in medical practice and are essential components of modern medicine. Among them, percutaneous devices, and particularly central venous catheters (CVCs), are extensively used for a number of clinical purposes, such as drug administration, parenteral nutrition, monitoring and sampling of biological signals and tissues [1–2], even in long term applications. Although these devices contribute to the shortening of the hospitalization period and to a general improvement in the quality of clinical treatments, their use has led to the development of new families of diseases related to the use of biomaterials and medical devices [3]. The impact of infections acquired in hospitals is considerable [4]: i.e. infections related to intravascular catheters are one of the major causes of morbidity and mortality in the United States [5].
When a synthetic material surface comes in contact with blood, two major adverse reactions may take place: thrombus formation and microbial colonization. These two blood-material interaction consequences lead to a number of clinical complications, ranging from local site infections and septic trombophlebitis to catheter related bloodstream infections, endocarditis and other metastatic infections as well as thrombosis [6, 7]. Even though the incidence of bacterial infection may be reduced by strict hygienic rules, strategies aimed to modify intravascular catheters surface or to propose innovative materials become decisive.
Materials used to fabricate these devices play a key role. Segmented and thermoplastic polyurethanes are the most widely used materials for intravascular catheters [8] and have been receiving increasing interest for the development of different blood-contacting medical devices. Among them, polycarbonate-urethanes (PCUs) are extensively used due to their biostability and appropriate mechanical properties [9] for long term applications.
To prevent bacterial adhesion and to locally control the coagulation and inflammation induced by polymer surfaces, the material surface can be modified [10]. Different surface treatments are currently under evaluation, ranging from non fouling surfaces [11] to biocidal polymeric surface modifiers [12]. Although most of these strategies seem to show good responses in decreasing bacterial colonization, and therefore the incidence of infective episodes, none of them shows the ability to combine antithrombogenicity and antibacterial activity.
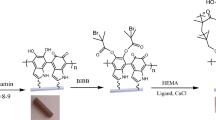
In the past years, a tailor-made diamino-diamide-diol, PIME (Fig. 1) was developed and used as chain extender in the synthesis of polyurethanes. Via its –OH end groups, PIME can be inserted in the backbone of a polymer during the polymerization process. Due to the presence of tertiary amino groups in alternation with amido groups, PIME-containing materials showed the ability to bind heparin at physiological pH, prevalently via ionic interactions, with the contribution of other electrostatic and hydrophobic interactions [13, 14].
Heparin is a natural polysaccharide acting as anticoagulant, often administered during surgical procedures to control blood clotting. Anticoagulants are used for the prevention of ischemic events resulting from thrombosis, and their immobilization on the cardiovascular devices are actively investigated to prevent local clot formation [10]. When bound onto a surface, besides the anticoagulant effects, heparin seems also to play a role in decreasing fibronectin deposition and bacterial adherence in vivo [15].
The aim of this work was to verify the ability of a heparinized surface to prevent bacterial adhesion and diminish their colonization. For this purpose, an innovative PCU, Bionate-PIME (synthesized by The Polymer Technology Group, Berkley, CA), containing low bulk amounts of PIME in the main backbone, was selected. Thermo-mechanical properties were compared to those of materials used to produce intravascular catheters: a poly(carbonate urethane), Carbothane®, and a silicone MED-4750 Nusil. The ability to decrease bacterial adhesion, due to the presence of bound heparin, was checked by S. aureus strains and S. Epidermidis strains.
Materials and methods
Materials preparation
Catheters
Polycarbonate-urethane (Carbothane®, \( \phi \) out = 5 Fr) and silicone (MED-4750 NuSil Technology, \( \phi \) out = 6.5 Fr) commercial catheters were kindly provided by P1H (Amaro, Ud, IT).
Bionate® and Bionate-PIME films
Pellets of aromatic Bionate® (lot number 092696) and aliphatic Bionate-PIME (lot number XCL112999.1) were kindly provided by The Polymer Technology Group (PTG, Berkeley, CA, USA). Chemical composition of PCUs used in this study is summarized in Table 1. To synthesize Bionate-PIME, some of the butandiol (0.1–0.5% mole fraction) was substituted with the diamine-diamide-diol PIME [14]. Material pellets were preconditioned for 48 h at 80 °C and extruded into strips (0.5 mm thick, 25 mm width) by using a four heat zones micro-extruder (GiMac, Castronno, IT).
Carbothane® films
Carbothane® films were obtained by solvent casting from the catheters. A 10% w/v solution was prepared by dissolving the PCU catheter in dymethylacetamide (DMAC), at 50 °C. The solution was cast in a glass Petri dish (\( \phi \) = 10 cm), allowing the solvent to evaporate at reduced pressure at 55 °C, until complete evaporation. Films 0.3 mm thick were obtained.
Heparinization
Disk specimens (\( \phi \) = 5 mm) were punched out from Bionate® and Bionate-PIME films. All the specimens were previously disinfected in ethanol (70 vol.%) for 30 min and then washed in a NaCl (0.9% w/v) sterile solution for 10 min. Specimens were then washed in a Phosphate Buffered Saline (PBS) solution for 24 h and then immersed overnight in a solution 0.5% w/v of Ca–heparin from porcine intestinal mucosa (166 USP units/mg Sigma Aldrich, H-9399) in PBS at 37 °C. Specimens were then rinsed in a sterile PBS solution.
Materials characterization
Scanning electron microscopy
Scanning electron microscopy (SEM) was used to evaluate the surface morphology of the materials and the bacterial adhesion onto untreated and heparinized PCUs. The samples were sputter-coated with gold and observed with Cambridge Stereoscan 440 microscope with 10 kV accelerating voltage.
Differential scanning calorimetry
Thermal properties were investigated using differential scanning calorimetry (DSC, Mettler TA3000) in the temperature range −100 to +250 °C, at a heating rate of 20 °C/min under nitrogen atmosphere.
Tensile tests
Uniaxial tensile tests were performed with a MTS 1/MH electromechanical system equipped with a 5 kN load cell, at a crosshead speed of 200 mm/min. Dumbbell specimens (n = 5) were cut with a die from the extruded strips according to the ASTM D638; catheter were mounted in the grips as previously described [9]. High capacity pneumatic grips, allowing a correct specimen alignment and removing the bending effects, were used. Tensile test results were recorded and elaborated with Testworks® software.
Dynamic mechanical analysis
Dynamic mechanical analysis (DMA) were carried out using a DMA 2980 analyzer (TA Instruments), in tensile mode, using specimens of 8 × 3 × 0.5 mm3. Storage modulus (E′), loss modulus (E′′) and tanδ (tanδ = E′′/E′) were recorded in the temperature range 0–250 °C at the heating rate of 1 °C/min; an oscillation amplitude of 25 μm at 1 Hz was applied. Tests were performed in duplicate.
In vitro bacterial interaction tests
Bacterial strains and growth condition
The bacterial strains selected for this study, Staphylococcus aureus Cowan 1, Staphylococcus aureus 8325-4, Staphylococcus epidermidis RP62A (a slime producer), Staphylococcus epidermidis HB (a non slime producer), were purchased by ATCC. All strains were cultured in Brain Heart Infusion (BHI, Difco, CA) supplemented with 10% (v/v) horse serum (Oxoid, Italy) to improve their growth. These cultures, used as source for the experiments, were statically incubated at 37 °C under aerobic conditions and reduced at a final density of 1 × 1010 cells/mL as determined by comparing the OD600 of the sample with a standard curve relating OD600 to cell number.
In vitro bacterial adhesion
Heparin-treated and untreated samples were disinfected in ethanol 70% (v/v) and extensively washed with sterile distilled water. Samples were then statically incubated with 100 μL (1 × 104 cells/mL) of each bacterial suspension for 24 h at 37 °C. After extensive washing with PBS (Phosphate Buffer Saline), bacteria viability was evaluated by MTT (3-(4,5) dimethylthiazol-2-yl-2,5 diphenyl tetrazolium bromide) (Sigma, USA) test by monitoring the absorbance at 595 nm in a Micro-plate Reader (Bio-Rad Richmond, CA, USA) as previously described [16]. The number of bacterial cells adherent to heparin-treated and untreated samples was drawn from a calibration curve. Tests were performed in triplicate and submitted to statistical analysis (t-student tests).
Scanning electron microscopy (SEM)
Heparin-treated and untreated samples were incubated with 100 μL (1×104 cells/mL) of each bacterial strains for 24 h at 37 °C. After washing in PBS to remove the aspecifically bound bacteria, samples were fixed with a 2.5% v/v glutaraldehyde solution in 0.1 M cacodylate buffer (pH 7.2) for 1 h at 4 °C. Samples were then briefly washed with cacodylate buffer and then dehydrated through a graded series of ethanol (up to 100%). The specimens, mounted on aluminium stubs, were sputter-coated with gold, and observed with a Cambridge Stereoscan 440 microscope at 10 kV acceleration voltage. Samples with adherent bacteria were observed at 2,000× magnification [17].
Results and discussion
Material characterization
At SEM, surfaces of extruded Bionate® and Bionate® PIME appear regular, smooth and with good homogeneity (data not shown). The possibility of obtaining an optimal set up was achieved via micro-extrusion, that allows to process small quantities of a thermoplastic polymers.
A comparative study of the mechanical properties of the two commercial catheters was performed to evaluate the possible use of Bionate-PIME as a candidate material for the design and fabrication of cardiovascular devices. In Table 2 mechanical parameters for Carbothane® and MED-4750 NuSil catheters are reported (tubes specimens). Carbothane® catheter is stiffer and shows better mechanical properties than silicone catheter, as expected.
By SEM observation, for both catheters radio-opaque barium sulphate dispersed in the polymer matrix was found (data not shown). The presence of this additive, although useful for clinical application, results in a lowering of the polymer mechanical properties [18].
In Table 2 mechanical parameters obtained by tensile stress-strain curves of extruded Bionate® and Bionate-PIME films are reported (Dumbbell specimens). Bionate® films show better mechanical properties if compared to Bionate® PIME: both materials show a typical elastomeric σ/ε behaviour, with the final part of the curve characterized by an increasing of the stress value. Moreover, the materials show low values of the elastic modulus in comparison to Carbothane® and MED-4750 ones. Nevertheless, they are in the same range of Carbothane® catheters evaluated in this study.
Storage modulus and tanδ for Bionate® and Bionate-PIME obtained from the dynamic mechanical analysis performed on films are shown in Fig. 2. These materials exhibit a similar behaviour, with a first small decrease in the storage modulus at 55 °C (T onset = 55 °C for Bionate-PIME and 54 °C for Bionate®). This decrease is probably due to the melting of the crystallites in soft segments domains, although tanδ peak associated to this transition is not distinguishable probably as a result of overlapping with the below zero glass transition. The ultimate storage modulus decrease starts at a different temperature for the two materials: 125 and 158 °C for Bionate-PIME and Bionate®, respectively, as calculated from E′ onset. This difference in melting temperature, can be further appreciated evaluating the correspondent tanδ curves: Bionate- PIME shows an increase in tanδ starting at 93 versus 150 °C for Bionate® (values from the onset).
Stiffness of Bionate® is higher than Bionate-PIME, confirming the static tensile tests results. The presence of PIME in the polymer backbone seems to slightly modify the mechanical properties of Bionate®: in spite of the lowering of the elastic modulus, the mechanical properties remain comparable to the other PCUs used for flexible cardiovascular devices. Previous studies showed feasibility by replacing all of the normal diol chain extenders with the heparin-binding diol PIME, but the synthesis product showed reduced mechanical properties [14]. The PIME chain extender, incorporated during the synthesis of the polyurethane at very low bulk concentration does not seem to significantly affect the mechanical properties of Bionate® PCU.
Results of DSC tests on Bionate® and Bionate-PIME are summarized in Table 3. Both materials show the typical behaviour of a block segmented thermoplastic polyurethane, with a glass transition related to the amorphous phase and a melting temperature due to the hard segment domains. The presence of PIME in the Bionate® backbone seems to affect the thermal properties, both in terms of Tg (−38 vs. −16 °C for Bionate® and Bionate-PIME, respectively) and Tm. In particular, Bionate-PIME exhibits a melting transition of both soft (Tmsoft) and hard segments (Tmhard), whereas Bionate® shows only a melting transition, characterized by the presence of a double peak. The thermal properties derived from the DMA tests well fit with the DSC data.
Bacterial adhesion
Viability assay
MTT test performed on Bionate®, Bionate-PIME and Carbothane® films after 24 h of bacterial cells incubation are reported in Fig. 3. The results show significant differences between the viability of S. aureus (Fig. 3A, B) and S. epidermidis (Fig. 3C, D) strains onto the different polymeric surfaces.
The number of S. aureus Cowan 1 and S. aureus 8325-4 adherent onto untreated PCU surfaces are increased of 3–4 order of magnitude after incubation, compared to seeded bacteria number; in particular, this behaviour is more relevant for Carbothane® (Fig. 3A, B). Conversely, the presence of adsorbed heparin on Bionate-PIME surface leads to the presence of bacterial cells number lower than 104 cells. A significant difference was detected in MTT absorbance values comparing Bionate-PIME heparinized to the other materials either heparinized or untreated.
The behaviour of S. epidermidis RP62A and HB strains is slightly different for all the three considered PCUs. The Bionate® films show no significant differences between heparinized and untreated samples, whereas the presence of heparin leads to a lower colonization onto the surface of Bionate-PIME (Fig. 3C). There are not significant differences between the Bionate® and Bionate-PIME heparinized surfaces. For S. epidermidis HB, the number of adherent cells is slightly lower for the Bionate-PIME, both for untreated and heparinized surfaces (Fig. 3D). Bionate® and Carbothane® (untreated and heparinized) show a higher colonization for this strain, compared to Bionate-PIME (p < 0.5).
SEM observations
Scanning electron microscopy images of S. epidermidis RP62A and S. aureus 8325-4 strains onto Bionate®, Bionate-PIME (either heparinized or untreated) and Carbothane® films are reported in Figs. 4 and 5, respectively. No significant differences in bacterial distribution of S. epidermidis RP62A onto the untreated and heparinized Bionate® surfaces are observed (Fig. 4A–C). Conversely, bacterial colonization onto heparinized Bionate-PIME surface is randomly distributed: small cell clusters were detected, confirming the lower value detected for the viability assay (Fig. 4D). A similar behaviour is observed for S. aureus 8325-4 strain: untreated surfaces show a uniform compact and dense layer of bacterial cells (Fig. 5A–C), whereas the heparin-treated materials show small clusters of cells which are randomly distributed (Fig. 5D).
The results reported in this study clearly indicate that the absorption of heparin onto the Bionate-PIME surface plays a key-role in reducing the bacterial cells colonization of material surfaces; in fact, this effect was not observed onto either heparinized Bionate®, or untreated Bionate® and untreated Bionate-PIME.
Taken together, these data indicate that the use of Bionate-PIME and the treatment of its surface with heparin could diminish the incidence of pre- and post-operative bacterial infection of catheters. Furthermore, the usage of heparin could avoid many of the drawbacks of traditional antibiotic prophylaxis and may have the potential to be a safe and effective addition to the prevention of bacterial infection.
Conclusions
In this work, the ability to prevent bacterial adhesion by surfaces with bound heparin was investigated. A poly(carbonate urethane), Bionate-PIME, containing low bulk amounts of the diamino-diamide-diol PIME was compared with two commercial medical-grade polymers used for fabrication of long term catheters in blood-contacting applications. Mechanical properties of Bionate-PIME resulted comparable with those of medical-grade PCU used for catheter fabrication, and suitable for improving the performances of cardiovascular devices.
The ability to bind heparin at physiological pH of PIME-containing polyurethanes leads to a twofold advantage. Beside the local control of the coagulation process, the adsorption of heparin onto Bionate-PIME surface was shown to play a role in mediating bacterial cells interaction. Heparinized PCU surfaces proved to decrease the colonization ability of the bacterial strains (S. epidermidis and S. aureus) mainly involved in the pathogenesis related to medical device infections.
To better understand the role of heparin in mediating the process of material/cells interaction and to assess the obtained results over a longer time period (>24 h) further studies are necessary. Particularly, the stability of bound heparin to Bionate-PIME has to be evaluated under dynamic conditions.
References
P. N. DANESE, Chem. Biol. 9 (2002) 873
Y. H. AN and R. J. FRIEDMAN, J. Biomed. Mater. Res. (Appl. Biomater.) 43 (1998) 338
L. RIMONDINI, M. FINI and R. GIARDINO, J. Appl. Biomater. Biomech. 3 (2005) 1
D. W. SPELMAN, MJA 176 (2002) 286
P. EGGIMANN, H. SAX and D. PITTET, Microbes Infect. 6 (2004) 1033
M. K. SCHINABECK and M. A. GHANNOUM, Clin. Microbiol. Newsl. 25 (2003) 113
J. N. BAUMGARTNER and S. L. COOPER, J. Biomed. Mater. Res. 40 (1998) 660
P. FRANCOIS, P. VAUDAUX, N. NURDIN, H. J. MATHIEU, P. DESCOUTS and D. P. LEW, Biomaterials 17 (1996) 667
M. C. TANZI, S. FARÈ and P. PETRINI, J. Biomater. Appl. 14 (2000) 325
M. C. TANZI, Export Rev. Med. Devices 2 (2005) 473
B. D. Ratner and A. S. Hoffman, Biomaterials science: An introduction to materials in medicine (Elsevier Academic Press: San Diego, 2004) p. 197
U. MAKAL, L. WOOD, D. E. OHMAN and K. J. WYNNE, Biomaterials 27 (2006) 1316
P. PETRINI, M. C. TANZI, L. VISAI, F. CASOLINI and P. SPEZIALE, J. Biomater. Sci. Polym. Ed. 11 (2000) 353
R. S. WARD, K. R. MCCREA, Y. TIAN and M. C. TANZI, in Proceedings of the 7th world biomaterials congress, Sidney, May 2004 (Australian Society for Biomaterials Inc.: Victoria, 2004) p. 433
P. APPELGREN, U. RANSJÖ, L. BINDSLEV and O. LARM, Lancet 345 (1995) 130
L. RIMONDINI, S. FARÈ, E. BRAMBILLA, A. FELLONI, C. CONSONNI, F. BROSSA and A. CARASSI, J. Periodontol. 68 (1997) 556
L. VISAI, S. RINDI, P. SPEZIALE, P. PETRINI, S. FARÈ and M. C. TANZI, J. Biomater. Appl. 16 (2002) 191
G. LEWIS, C. S. J. van HOOY-CORSTJENS, A. BHATTARAM and L. H. KOOLE, J. Biomed. Mater. Res. (Appl. Biomater.) 73 (2005) 77
Acknowledgements
The Authors thanks Plan1Health (Amaro, Ud, I) for the financial support, PTG (Berkeley, CA, USA) for providing the materials, and GiMac (Castronno, Va, I) for the extrusion process.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Nardo, L., Farè, S., Di Matteo, V. et al. New heparinizable modified poly(carbonate urethane) surfaces diminishing bacterial colonization. J Mater Sci: Mater Med 18, 2109–2115 (2007). https://doi.org/10.1007/s10856-007-3083-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-007-3083-9