Abstract
In this study, using polylactic acid-co-glycolic acid (PLGA) with a molecular weight of 95,800 Da as drug carrier, three dose (low, moderate, high) rapamycin-eluting stents and the corresponding coating films were prepared. The pre- and post-expansion morphology of the rapamycin-eluting stent was examined by scanning electron microscopy (SEM), indicating that the coating was very smooth and uniform. The coating had the ability to withstand the compressive and tensile strains imparted without cracking from the stent during expansion process. There were many voids on stent coating surface after released for 18 days in release medium. The thermodynamics data of the stent coating film measured by differential scanning calorimetry (DSC) showed a lack of measurable solubility of rapamycin in the PLGA matrix. The release behavior of rapamycin from stent surface had a two phase release profile with a burst release period of about 2 days, followed by a sustained and slow release phase. The mass loss behavior of PLGA appeared linear throughout most of the degradation period, corresponding to an approximately constant mass loss rate. The platelet adhesion tests showed that the rapamycin-eluting films may have a good blood compatibility compared with control samples. Take into these results account, this novel rapamycin-eluting may be a good candidate to resolve in-stent restenosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In-stent restenosis is the major drawback of percutaneous transluminal coronary angioplasty (PTCA), occurring in 10–40% of the patients [1]. In-stent restenosis can be divided into two general concepts [2]: recoil and remodeling of the treated vessel and neointimal hyperplasia due to proliferative response to injury, which consists largely of smooth muscle cells proliferation and matrix formation. Recently, drug-eluting stents with synthetic polymer coatings which act as drug reservoirs and elute drugs over a period of several weeks or months opened up a new paradigm in treatment of in-stent restenosis (ISR) [3–5]. These drug-eluting stents can provide luminal scaffolding that virtually eliminates recoil and remodeling of the treated vessels. Additionally, the drug released from coatings can inhibits thrombus formation, inflammation, or cellular proliferation. After the drug releases from the polymer coatings, the remaining synthetic nonresorbable polymer coatings may lead to complications such as exaggerated inflammatory response and neointimal hyperplasia at the implant site [6, 7]. So, it is desirable to develop a drug-eluting stent with a biocompatible and biodegradable coating to prevent these unfavorable effects.
Rapamycin (Fig. 1a), which also is called sirolimus, a natural macrocyclic lactone produced by Streptomyces hygroscopicus, is a potent immunosuppressive agent approved by the Food and Drug Administration [8]. It can down-regulate cytokine dependent kinase mTOR (mammalian target of rapamycin), thus inducing cell-cycle arrest in the late G1 phase (Fig. 1b) [9, 10]. It is known that sirolimus is only effective when bound to sirolimus binding protein (FKBP), present on smooth muscle cells [11]. It inhibits the proliferation of both rat and human smooth muscle cells in vitro and reduces intimal thickening in models of vascular injury [12, 13].
Poly(lactic acid-co-glycolic acid), PLGA, a biodegradable polymer, which has many good properties such as good biocompatibility and biodegradation, is popular materials that are used extensively for controlled delivery of different drugs [14]. Using PLGA as drug carrier for stent coating may be a good candidate to overcome the side effects of nonbiodegradable polymer. In this study, a novel drug-eluting stent, spray-coated with PLGA coating which contains rapamycin, was developed. Additionally, its various in vitro characteristics and drug release profile were also investigated in this study.
Materials and methods
Materials
The material of stent used in this study was annealed 316LVM surgical grade steel tube. The bare stainless steel stents were prepared by laser cutting methods. The rapamycin was purchased from institute of microorganism, Fujian province, China, and its purity was above 98.3% (HPLC grade). The PLGA resin (the average viscosity molecular weight is 95,800) was endowed by Chengdu Zhuxin biomaterials Co., Ltd in China. All other reagents used in this study were analytical grade.
Preparation of rapamycin-eluting stents
The stents polished by electrochemical method were cleaned carefully using ultrasonic cleaning method with acetone, ethyl alcohol and distilled water in sequence. The cleaned stents were kept under vacuum to evaporate the residual water for 48 h. A 1 wt% solution of PLGA and rapamycin was sprayed onto the cleaned stent surface. The spraying system was depicted in Fig. 2. The spraying liquid from micro syringe which was atomized by ultrasonic atomization operator was sprayed onto the stent surface. The stent traversed and rotated during spraying process. Three types of stents loaded with different amounts of rapamycin were prepared: the low-dose stent (∼150 μg per stent or 125 μg/cm2), the moderate-dose stent (∼250 μg per stent or 208 μg/cm2) and the high-dose stent (∼400 μg per stent or 333 μg/cm2). The control stents with only PLGA coating were prepared by the same method. The thickness of these coatings was about 10 μm.
Fabrication of rapamycin-loaded films
The rapamycin-loaded films and control film with PLGA only were fabricated by casting method [15]. Three dose rapamycin-loaded films were prepared corresponding to the rapamycin-eluting stents: 15% (low-dose), 25% (moderate dose), 40% (high-dose) (w/w).
Thermal analysis
Thermal properties of PLGA and moderate-dose coating film were measured by DSC (DSC2920, TA Instruments, Alzenau, Germany). The casting films were dried in vacuum to evaporate water before heating. The sample was heated under dry, oxygen-free nitrogen, from 20 °C to 300 °C at a rate of 10 °C/min.
Morphology examination and balloon-expansion test
The morphology of the rapamycin-eluting stent was examined by scanning electron microscopy (SEM, Quanta200, Philipis) before balloon expansion. The stent was mounted onto angioplasty balloon (3.0 × 20 mm) then expanded. The post-expansion stents were also examined by SEM.
Release profile of rapamycin
Release profile of rapamycin was in vitro investigated by incubating the individual rapamycin-eluting stent in 1.5 mL of medium at 37 °C and pH 7.4. The medium consisted of phosphate-buffered saline containing 10% methonal (v/v) [16]. At selected time, the incubation medium was completely removed for analysis and replaced with fresh medium. An aliquot of sampled medium was measured by high performance liquid chromatography (HPLC) method (Waters 2695 separations module and Waters 2487 dual λ absorbance detector) and fixed wavelength 278 nm, the flow rate is 1 mL/min and the flow phase consisted of acetonitrile and water (65:35, v/v). Results were expressed as cumulative micrograms and weight percent of rapamycin released.
In vitro platelet adhesion test
The in vitro platelet adhesion behavior of rapamycin-loaded PLGA films and control films was examined based on the previous paper [17]. Briefly, the samples were first rinsed by PBS and contacted with platelet-rich plasma (PRP) for 2 h at 37 °C. After washing with 0.9% NaCl solution, they were fixed using glutaraldehyde solution. Washed again with 0.9% NaCl for three times, these samples were hydrated in a series of ethanol–water solutions for 5 min and dried in a dessicator. It was sputtered with gold before being imaged by scanning electron microscopy (SEM).
In vitro biodegradation experiment
The weight loss rate and water adsorption rate of PLGA were investigated according to the method described in previous paper [15]. The PLGA films with the same weight and thickness were individually incubated in 20 mL of medium at 37 °C and pH 7.4. The medium was phosphate-buffered saline and the medium was changed every week. The weight loss rate and water adsorption rate were calculated based on the following equations. Each reported value was average of data of the triplicate specimens.
where W a is the weight of swelling polymer film, W d is the weight of dried polymer film and W 0 is the initial weight of PLGA film.
Results and discussion
The morphology of rapamycin-eluting stent and balloon-dilation test
For drug-eluting stent, the surface morphology of drug-eluting stent plays an important role in clinical application. Generally speaking, a drug-eluting stent requires smooth surface and no webbings between stent struts. Smooth surface coating can significantly decrease the injury of blood vessel and make the stent go to injury site successfully. Results obtained from Scheerder [18] and Tepe [19] indicated that the smooth stent surface almost has not thrombus formation after insertion compared with rough stent surface. Figure 3a showed the SEM images of rapamycin-eluting stent. It was indicated that not only the coating was very smooth and uniform, but also the coating had not any webbings between struts.
In addition to the smooth and uniform surface, the polymeric coatings for drug delivery from stents also need to satisfy a legion of physical, biological, and regulatory criteria before they can be deemed suitable. The stent coating (drug and polymer) must withstand subsequent processing, such as sterilization, mount, and deployment without compromising the physical integrity of the coating [20]. Figure 3b showed an expanded stent sample of SEM images after being dilated by an angioplasty balloon (3.0 × 20 mm). As showed, no delamination or destruction of the coating on the stent was observed. The coating was tightly adhered to the surface of stainless steel stent, suggesting that the coating has the ability to withstand the compressive and tensile strains imparted without cracking from the stent expansion process.
In vitro biodegradation
The degradation of aliphatic polyesters proceeds through hydrolysis of the ester bonds [21]. Thus, the water contents of the specimen were first measured. Figure 4a shows the swelling rate as the function of time. The water contents before 5 days were very small. The water contents of PLGA film increased significantly from the fifth day to 20th day. This was caused by the water uptake of the polymer as a result of swelling. As the polymer chains were degraded during this period, more formed hydrophilic oligomers enhanced the water uptake. The swelling rate achieve 300% at about 3 weeks and then slightly decreased, this indicated that the water contents in the sample may win a stable saturated state.
The weight loss rate plays an important role in investigating the biodegradation process of polymer materials. Figure 4b showed the mass loss curve for a degrading PLGA polymer. The curve appeared linear throughout most of the degradation phase, corresponding to an approximately constant mass loss rate. This indicated that the sample weight decreased from the degradation start, thus, the mechanism of the PLGA was bulk degradation going with surface degradation.
The release profile of rapamycin
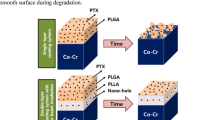
The results of in vitro elution of rapamycin from three dose rapamycin-eluting stents were showed in Fig. 5. The release behavior of rapamycin exhibited two phase release profile (Fig. 5). There was a burst release phase (before 2 days) because of immediate dissolution of rapamycin on the stent surface. The burst release amount of high-dose stent was most distinct in comparison with moderate-dose stent and low-dose stent. The drug weight percent of burst release for three stents was 4.72% for low-dose, 15.47% for moderate-dose, 20.10% for high-dose, respectively (Fig. 5b). After initial burst release followed by a longer lasting, slower sustained release period, the decreased release phase appeared to an approximate zero-order release model. The slow releasing rate was probably due to the longer diffusing route of deeper rapamycin in coating. Total available dose at 18 days for the high-dose formulation was approximately 4.5 times compared with that of moderate-dose formulation, and was 7.8 times compared with the low-dose stent. With the increase of drug-to-polymer ratio, the release rate increased. However, from the data showed in Fig. 5, it can be seen that the drug release profile of three dose stents was not proportionally linear with increasing drug loading (increasing drug-to-polymer ratio).
The stent morphology after released for 18 days was showed in Fig. 6, there were many voids on the stent coating surface. The rapamycin particles on stent surface dissolved in release medium, resulting in holes or voids on the surface. These voids or holes can form the channels through which the rapamycin diffused. It was also enhanced water uptake of polymer and thus may make the degradation become easier.
DSC analysis
DSC scans for PLGA-only and moderate-dose drug films were showed in Fig. 7. As showed, the glass transition temperature were 62.4 °C. However, the glass transition temperature of rapamycin-eluting film shifted to low temperature due to the presence of the rapamycin. There were two peaks at 180.8 °C and 193 °C at rapamycin-eluting film, it was speculated that rapamycin may have a crystallization transition, indicating that there might be indicative of weak physical interaction between rapamycin and PLGA. Overall, the thermodynamics data of the stent coating measured by differential scanning calorimetry (DSC) showed a lack of measurable solubility of rapamycin in the PLGA matrix and rapamycin may be a dispersive state in PLGA matrix.
In vitro platelet adhesion
Platelet adhesion on polymer films from human plasma is an important test for the evaluation of the blood compatibility of materials. As showed in Fig. 8, the platelets adhered on the PLGA-only film surface were significantly less than stainless steel plate, indicating that the PLGA had a better anti-platelet adhesion property. The adhered platelets on rapamycin-loaded PLGA film decreased largely compared with control samples, suggesting that rapamycin enhanced anticoagulation of PLGA samples. Unfortunately, there was no distinct difference between the low-dose film and high-dose film.
Figure 9 showed the morphology of platelets adhered on different films. In the case of PLGA-only film, the platelets adhered on film surface were generally singular with the rounded shape typical of platelets in the inactivated state and a few pseudopodia were observed compared with stainless steel plate. However, for all rapamycin-loaded films, the platelet did not aggregate and extension of pseudopodia was not observed. It was considered that the improved anticoagulation can be attributed to rapamycin released from drug-loaded films.
It is well know that platelet adhesion and activation usually occurs when the cardiovascular implant such as stent contacts with blood. The adhered platelets mainly turn on the types and conformation of adsorbed plasma protein; plasma protein adsorption strongly depends on the surface characteristic of polymer film. Rapamycin has a good antiproliferative and anti-inflammatory action, however, its anticoagulation is not clear until now. A few research results indicated that rapamycin may make platelet aggregate [22], but in our study, after loading rapamycin in PLGA films, the platelets decreased distinctly. It is speculated that the releasing rapamycin from polymer films may combine with plasma protein thus inhibit the plasma protein deposition on samples, this contributes to decrease platelet adhesion.
Conclusion
The surface of rapamycin-eluting stents using PLGA as carrier was very smooth and the coatings can withstand the compressive and tensile strains imparted without cracking from the stent during mounting and expansion process. The release profile of rapamycin from stent showed two phase profile with a burst release period for about 2 days. The mass loss behavior of PLGA film appeared linear throughout degradation process, corresponding to an approximately constant mass loss rate. The rapamycin-eluting stent may significantly inhibit the platelet adhesion from plasma and may be used to resolve the in-stent restenosis.
References
L. BAREND, M. M. NUNO, M. W. HAZEM, et al., Int. J. Cardiol. 99 (2005) 9
R. B. MARTIN, Heart 89 (2003) 218
E. REGAR, G. SIANOS and P. W. SERRUYS, Br. Med. Bull. 59 (2001) 227
M. C. MORICE, P. W. SERRUYS, J. E. SOUSA, et al., N. Engl. J. Med. 346(23) (2002) 1773
J. W. MOSES, M. B. LEON, J. J. POPMA, et al., N. Engl. J. Med. 349(14) (2003) 1315
I. K. DE SCHEERDER, K. L. WILCZEK, E. V. VERBEKEN, et al., Atherosclerosis 114 (1995) 105
E. RECHAVIA, F. LITVACK, M. C. FISHBIEN, M. NAKAMURA and N. EIGLER, Cathet. Cardiovasc. Diagn. 45 (1998) 202
C. G. GROTH, L. BACKMAN, J. M. MORALES, et al., Transplantation 67 (1999) 1036
S. O. MARX, T. JAYARAMAN, L. O. GO and A. R. MARKS, Circ. Res. 76 (1995) 412
M. POON, S. O. MARX, R. GALLO, et al., J. Clin. Invest. 98 (1996) 2277
B. BHARGAVA, G. KARTHIKEYAN, A. S. ABIZAID and R. MEHRAN, Clin. Rev. BMJ 327 (2003) 274
C. R. GREGORY, X. HUANG, R. E. PRATT, et al., Transplantation 59 (1995) 655
R. GALLO, A. PADUREAN, T. JAYARAMAN, et al., Circulation 99 (1999) 2164
W. R. GOMBOTZ and D. K. PETTIT, Bioconjug. Chem. 6 (1995) 332
A. Frank, V. Subbu, K. R. Santosh and L. H. Gan, J. Appl. Polym. Sci. 102 (2006) 3111
A. FRANK, S. V. SUBBU, K. R. SANTOSH and B. FREDDY, J. Control. Release 98 (2004) 67
J. ZHOU, J. YUAN, X. P. ZANG, et al., Colloids Surf. B Biointerfaces 41 (2005) 55
I. DE SCHEERDER and E. VERBEKEN, J. VAN HUMBEECK, Semin. Interv. Cardiol. 3 (1998) 139
G. TEPE, H. P. WENDEL, S. KHORCHIDI, et al., J. Vasc. Interv. Radiol. 13 (2002) 1029
V. R. SHRIRANG, M. M. KATHLEEN, E. R. ROBERT, et al., J. Biomed. Mater. Res. 71A (2004) 625
A. GÖPFERICH, Biomaterials 17 (1996) 103
A. BABINSKA, M. S. MARKELL, M. O. SALIFU, et al., Nephrol. Dial. Transplant, 13(12) (1998) 3153
Acknowledgements
This work is financially supported by the key basic research program No. 2005CB623904, NSFC-RGC 30318006# of Natural Science Fund of China and the innovation fund of Southwest Jiaotong University in China.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pan, C.J., Tang, J.J., Weng, Y.J. et al. Preparation and characterization of rapamycin-loaded PLGA coating stent. J Mater Sci: Mater Med 18, 2193–2198 (2007). https://doi.org/10.1007/s10856-007-3075-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-007-3075-9