Abstract
Composites of amorphous carbonated apatite and poly-(R)-3-hydroxybutyrate (PHB) and poly-(R)-3-hydroxybutyrate-co-(R)-3-hydroxyvalerate (PHBHV), respectively, were studied by pH monitoring upon immersion in water and by long-term osteoblast culture. For comparison, α-tricalcium phosphate (α-TCP), one glass ceramic (GB 9N), and one bioglass (Mg 5) were subjected to the same experiments. Excellent cell proliferation was found on the composite of calcium phosphate with PHB and on the reference materials (α-TCP, glass ceramic, bioglass). In contrast, cell death was observed repeatedly on the composite with PHBHV. A composite of amorphous calcium phosphate and PHB appears to be well suited as slowly biodegradable bone substitution material.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Poly-(R)-3-hydroxybutyrate (denoted as PHB in the following) and poly-(R)-3-hydroxybutyrate-co-(R)-3-hydroxyvalerate (9:1; denoted as PHBHV in the following) are well-known biodegradable polymers. Their application in biomedicine, supplementing polyglycolide, polylactide and their copolyesters has already been proposed by Doyle et al. [1]. Compared to the former, they possess a much higher chemical stability towards hydrolysis, resulting in considerably longer degradation times.
Like all biodegradable polyesters, these compounds release acidic degradation products (oligomers and monomers) during degradation in vitro and in vivo. This can be a severe problem in biomedicine, because acidosis accompanied by damage of the surrounding tissue can occur. Adopting a concept first proposed by Agrawal and Athanasiou [2] and extended by us [3], we designed composite materials that overcome this problem by using basic calcium phosphates to internally compensate the pH [4, 5]. This has the further advantage to add a well-known bioactive substance, i.e., a bone mineral-like calcium phosphate to the implant. In order to achieve a good biodegradability (high solubility), the calcium phosphate phase was prepared in an X-ray amorphous form with some content of carbonate (see the work by Doi et al. for the osteoclastic response to different calcium phosphates in vitro [6, 7]), i.e. as amorphous carbonated apatite that has similarities to the nanocrystalline calcium phosphate phase in bone [8, 9]. This extends the work reported by Chen and Wang who have prepared composites of PHBHV with hydroxyapatite and tricalcium phosphate but did not use a more soluble calcium phosphate (like ACP) but only conventional calcium phosphate ceramics from high-temperature synthesis [10]. We have shown earlier that neither pure hydroxyapatite nor β-tricalcium phosphate are able to counter the acidic degradation of polyesters [4].
For comparison, three well-known calcium phosphate phases were subjected to the same experimental studies: α-tricalcium phosphate, one glass ceramic (GB 9N) and one bioglass (Mg 5). The preparation of these materials was described earlier [11–13]. The biocompatibility was checked by monitoring the pH upon immersion in water and in cell culture medium and also by long-term osteoblast culture.
Materials and methods
Polyesters
Poly-(R)-3-hydroxybutyrate from natural origin (PHB) was obtained from Aldrich and used as purchased. Elemental analysis gave 55.5 wt% C (expected: 55.2), 7.0 wt% H (expected: 8.1), and 0.6 wt% N (expected: 0.0). The unexpected content of nitrogen is probably due to remnants from the biotechnological production process [14]. Its purity was further checked by infrared spectroscopy (IR), differential scanning calorimetry (DSC) (m.p. 167 °C), and X-ray powder diffraction, showing a partially crystalline polymer. 1H and 13C-NMR in CDCl3 showed the characteristic peaks as well as small amounts of unidentified impurities. Viscosimetry gave an average chain length (expressed as the numerical number of monomer units) of 1750 before and of 1150 after sterilization (mass per monomer: 86 g mol−1).
Poly-(R)-3-hydroxybutyrate-co-(R)-3-hydroxyvalerate) (9:1 = n:n; PHBHV) was obtained from Fluka and used as purchased. Elemental analysis gave 56.7 wt% C (expected: 56.2), 7.5 wt% H (expected: 7.1), and 0.0 wt% N (expected: 0.0). Further analysis by IR spectroscopy, DSC (m.p. 130 °C), and X-ray powder diffraction (semicrystalline polymer) confirmed the identity. However, in 1H and 13C-NMR in CDCl3 some small peaks of yet unidentified impurities were found. Viscosimetry gave an average chain length of 1270 before and of 1060 after sterilization (average mass per monomer: 87.4 g mol−1).
Calcium phosphates
Amorphous carbonated apatite (B-type) [15] was precipitated from aqueous solution by rapidly mixing a solution of NH4H2PO4 and K2CO3 with a solution of Ca(NO3)2, filtering off the precipitate after 2 min and drying at 80 °C for 12 h [9]. Its constitution was established by X-ray powder diffraction (fully X-ray amorphous), infrared spectroscopy (IR) and thermal analysis (combined thermogravimetry–differential thermal analysis–mass spectrometry; TG–DTA–MS). The sample contained 12.2 wt% water (released from 100 to 200 °C) and 2.6 wt% carbon dioxide (released from 550 to 950 °C). The sample consisted of agglomerated polycrystals of irregular shape with diameters of 5–100 μm, with most particles being in the size range of 30–70 μm. In the following, this sample is denoted as “ACP” (amorphous calcium phosphate) which is the usual term.
Porous α-tricalcium phosphate (denoted “α-TCP” in the following) was obtained from Biovision (Ilmenau, Germany). Elemental analysis according to the manufacturer gave 45.8 wt% P2O5 and 54.2 wt% CaO. Its phase purity was checked by X-ray powder diffraction.
The porous glass ceramic GB 9N from Biovision (denoted “glass ceramic” in the following) had an elemental composition of 43.2 wt% P2O5, 35.9 wt% CaO, 7.5 wt% Na2O, 10.7 wt% K2O, 1.1 wt% MgO, and 1.1 wt% SiO2. The ceramic was modified by a neutralizing surface treatment in order to avoid a decrease of the biocompatibility during degradation caused by its high solubility [12]. X-ray powder diffraction showed a good crystallinity.
The porous bioglass Mg 5 from Biovision (denoted “bioglass” in the following) had an elemental composition of 56.5 wt% P2O5, 19.6 wt% CaO, 17.4 wt% Na2O, 4.1 wt% MgO, and 2.1 wt% Al2O3. The material was completely X-ray amorphous.
Composites of polyesters and calcium phosphate
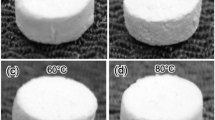
Compact pellets were prepared by thoroughly mixing (by grinding) the polymer with calcium phosphate in the w:w ratio 150 mg:30 mg. This material was compacted for 10 min at room temperature under 109 Pa uniaxial pressure to circular tablets of 13 mm diameter and about 1 mm thickness.
All pellets were immersed in pure water for 60 min before cell-seeding to remove possible degradation products from melt-pressing. They were subsequently sterilized in an autoclave at 2.1 bar and 121 °C for 20 min. Viscosity measurements showed that the average polymer chain length decreased upon sterilization (see above). No crystallization of the calcium phosphate was observed by X-ray diffraction.
The composites are denoted “PHB–ACP” and “PHBHV–ACP” in the following.
Analytical techniques
The release of acidic monomers from the polyesters, the basic reaction of the calcium phosphates, and the pH-compensation exerted by the composites were tested by immersion in pure (i.e. unbuffered, distilled) water (one pellet in 50 ml water). This system is more sensitive to release of H+ or OH− than buffered systems.
Viscosimetry was carried out with an Ubbelohde capillary viscosimeter (DIN 51562). The materials were dissolved in chloroform by stirring at room temperature. The concentrations were in the range of 0.1–1 g L−1. The insoluble residue of calcium phosphate and biologic material (for the seeded implants) was filtered off. The intrinsic viscosity at 25 °C was 129 mL g−1 for PHB and 102 mL g−1 for PHBHV.
X-ray powder diffractometry (XRD) was carried out with a Bruker AXS Advance diffractometer (nickel-filter; CuKα-radiation, λ = 154.178 pm; proportional detector) in Bragg–Brentano geometry. Differential scanning calorimetry (DSC) was carried out with a Mettler TA 4000 instrument in sealed aluminum crucibles. The heating rate was 5 K min−1 and the average sample mass was 5–8 mg. Combined thermogravimetry–differential thermal analysis–mass spectrometry (TG–DTA–MS) was carried out with a Netzsch STA 409/Balzers QMS 421 system, employing dynamic air atmosphere (50 ml min−1) and a heating rate of 5 K min−1. Open alumina crucibles served as sample holders.
Cell cultures
Primary osteoblastic cells were obtained by sequential digestion of mouse calvaria in a solution of 0.1% clostridial collagenase Ia (Sigma Chemical Co., St. Louis, MO) and 0.2% dispase (Boehringer Mannheim Biochemicals, Mannheim, Germany) from 3 day old mice and cultured in α-MEM containing 10% fetal bovine serum (FBS), and 1% penicillin–streptomycin (PS) [16, 17]. The cells were cultured in six-well plates (Falcon Labware, Oxnar, CA) on implants placed on glass coverslips at an initial density of 3 × 105 cells per well. The medium was changed after the first and the third day. Thereafter the medium was supplemented with 5 mmol β-glycerolphosphate, and 100 μg mL−1 ascorbic acid (mineralization medium) and replaced every other day. All cultures were maintained at 37 °C under 95% air/5% CO2 atmosphere.
The pH of the culture was determined each time after medium replacement (pH-meter type pH 538, WTW, Weilheim, Germany). Samples were taken after 2, 4 and 6 weeks of culture. The cultured cells on coverslips were fixed with 3.7% formaldehyde in phosphate-buffered saline solution (PBS) for 10 min at room temperature and washed in PBS. Analysis for alkaline phosphatase (enzymatic labeling) and collagen synthesis (van Gieson staining) was done according to standard protocols [16, 17]. For validation of the cell behavior all in vitro experiments were repeated four times.
For the detection of osteocalcin the antibodies used included a goat anti-mouse osteocalcin antibody (dilution 1:100) obtained from Biotrends (Cologne, Germany) and a secondary AlexaFluor 488 antibody from Molecular Probes Leiden, The Netherlands). Rhodamine conjugated phalloidine from Molecular Probes was used for specific labeling of actin. For double-immunofluorescence analysis cultured cells plated on glass coverslips and on composite pellets were used. The cells were fixed with 3.7% formaldehyde in PBS for 10 min at room temperature and washed in PBS. All subsequent incubations were performed at room temperature with PBS containing 0.05% saponin, 0.1% BSA, and 5% normal goat serum (NGS). Samples were incubated in PBS–saponin–BSA–NGS for 30 min to block non-specific binding, and then for 2 h with the primary antibody. The samples were washed in PBS–saponin–BSA and all subsequent steps were performed in the dark.
After washing the samples were incubated with the secondary antibody for 1 h. After further washing, actin was labeled by incubation with rhodamine conjugated phalloidine for 1 h. After final washing in PBS, the samples were mounted in FluorSave fluorescent mounting media (Calbiochem-Novabiochem Corp., La Jolla, CA). The samples were examined with a confocal laser scanning microscope (IX70 inverted Olympus microscope and Olympus Fluoview confocal imaging system) with a krypton/argon laser using an optical slice thickness of 2 μm.
For electron microscopy, the seeded implants were fixed with 3.5% glutaraldehyde in PBS for 10 min at room temperature and washed in PBS. The samples were subsequently dehydrated in an ascending alcohol row (ethanol–water mixtures of 40/60, 60/40, 80/20, 90/10, 100/0 = V:V). Ethanol was then replaced in four steps by amyl acetate. The pellets were subjected to critical point drying with CO2 (40 °C, 100 bar) in a Balzers Union Critical Point Dryer. Scanning electron microscopy (SEM) was carried out on gold-sputtered samples with a Philips SEM 515 instrument operating at 25 kV.
Results
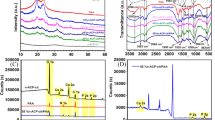
The pure polymers in water give pH values of about 6.5 (PHB) and 6 (PHBHV). The calcium phosphate phase reacts slightly basic (pH 7.5). Combined in a composite, the pH remains stable close to neutral 7 after the first 24 h. The calcium phosphates that were used for comparison gave constant pH values of 7.0 (α-TCP), 7.1 (glass ceramic), and 7.4 (bioglass) within this time interval. The results are shown in Fig. 1. Note that all pH changes are small, and that all materials react almost neutral.
Evolution of pH during immersion in pure water: (a) Poly-(R)-3-hydroxybutyrate (PHB), (b) Poly-(R)-3-hydroxybutyrate-co-(R)-3-hydroxyvalerate 9:1 (PHBHV), (c) Amorphous calcium phosphate (ACP) (d) Composite of PHB and calcium phosphate (150:30 = w:w) (PHB–ACP) (e) Composite of PHBHV and calcium phosphate (150:30 = w:w) (PHBHV–ACP). All materials show only a slight hydrolysis in this unbuffered system, as indicated by the small changes in pH (note the logarithmic scale of pH)
Osteoblast specific biocompatibility
To analyze the biocompatibility of the different materials, we incubated the samples with primary osteoblasts from mouse calvaria in α-MEM culture medium under standardized conditions.
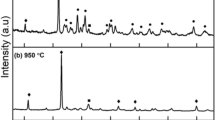
In presence of the implants, the behavior of the osteoblasts was analyzed by morphological and biochemical means. Within 4 days a confluent cell layer could be demonstrated in the presence of α-TCP, bioglass, glass ceramic, PHB–ACP, and PHBHV–ACP, respectively. The osteoblasts continued to proliferate, forming a multilayer of cells and finally produced an extracellular matrix on α-TCP, bioglass, glass ceramics and PHB–ACP. In sharp contrast, the osteoblasts did not survive in the presence of PHBHV–ACP. These results were confirmed in three independent series of experiments. In the presence of PHBHV–ACP, the cells showed numerous intracellular vacuoles with a subconfluent layer of cells after 4 days. After that, the cells progressively died. At day 9, there are only few cells left while at day 10 the culture was completely acellular (Fig. 2).
Light microscopy of osteoblast cell cultures on PHB–ACP (a and b; magnification: 100×) and PHBHV–ACP (c and d; magnification 400×). a = 7 days. b = 28 days. c = 7 days and d = 9 days. Note the rapid decline of the cells in the presence of PHBHV–ACP in comparison to the confluent and mineralized cellular layer on PHB–ACP
The pH of the medium was recorded throughout the entire culture period of 6 weeks. Because the sterility of the experiment was necessary for successful cell proliferation, the pH was recorded when the medium was changed, for the first time after 24 h and thereafter every other day. The pH remained almost constant and was within the physiological range (Fig. 3) after the first day for all materials tested except for PHBHV–ACP that gave an alkaline pH of about 7.9. The different behavior of PHBHV–ACP in cell culture and in pure water (Fig. 1) may be due to the longer observation time and the different immersion medium, possible also to a metabolic action of the osteoblasts.
Further histobiochemical analysis after 2, 4 and 6 weeks for alkaline phosphatase and collagen expression (van Gieson) demonstrated the homogeneous distribution of the osteoblasts at these times and their functional activity. Osteocalcin synthesis which is indicative for the presence of osteoblasts was detected by confocal laser microscopy after immunolabeling at the same time.
These findings confirmed that the cells maintained their osteoblastic differentiation in the presence of the different materials. For α-TCP, glass ceramic, bioglass and PHB–ACP these results were very similar and demonstrated in Fig. 4 for bioglass (alkaline phosphatase), α-TCP (collagen), and PHB–ACP (osteocalcin).
Typical osteoblastic markers can be visualized on the different bone substitutes: (a) Bioglass (10 days of differentiation, alkaline phosphatase staining (blue), light microscopy, magnification 200×). (b) α-tricalcium phosphate (10 days of differentiation, van Gieson staining; collagen (red), light microscopy, magnification 100×). (c) PHB–ACP (7 days of differentiation, double staining osteocalcin (green)/actin (red), confocal microscopy magnification 200×). Because the results for glass ceramics, bioglass, α-TCP, and PHB–ACP were practically identical, only typical stains are shown for these materials. For PHBHV–ACP, cell death was observed (not shown)
Undecalcified histology (von Kossa/van Gieson counterstaining) revealed that the entire surface of the material was covered by cells demonstrating that the surface structure was biocompatible with cell attachment on the surface of the materials. However, equal culture conditions led to different numbers of cell-layers on the single materials as shown in Fig. 5. There were thin monolayers on the surface of bioglass and large multilayers on glass ceramic, α-TCP and PHB–ACP pellets.
Undecalcified histology (van Kossa-/van Gieson-counterstaining) on α-TCP, PHB–ACP, glass ceramics (GC) and bioglass (BG) (magnification 400×). There is a small monolayer on the surface of the bioglass (d) and large multilayers on the glass ceramic (c) and β-TCP (a). Note the flared and extensive layer of osteoblasts (Ob) on the PHB–ACP-pellets (b)
Ultrastructural examination by scanning electron microscopy showed the multilayer of osteoblasts and the extracellular matrix on PHB–ACP (Fig. 6).
All materials were studied by X-ray powder diffraction after immersion in culture medium (2, 4 and 6 weeks). No conversion or recrystallization was observed in any case. This indicates that the amorphous calcium phosphate phase in the composites did not transform into crystalline hydroxyapatite upon immersion in cell culture medium as might have been expected [18, 19]. Neither did the amorphous bioglass recrystallize, as shown by X-ray diffraction. The composites were also studied by IR spectroscopy and DSC. No significant changes upon immersion were found. The average chain length of the polymers decreased from 1150 to 390 after 6 weeks for PHB–ACP and from 1060 to 670 after 2 weeks for PHBHV–ACP. This shows the slow hydrolytic degradation of the polyesters.
The calcium phosphate phase in the composites did not undergo dissolution as shown by thermogravimetric experiments after 8 weeks cell culture. After heating to 500 °C in air (combustion of the polyester), 18.9 wt% (PHB–ACP) and 23.9 wt% (PHBHV–ACP) of the calcium phosphate phase remained, respectively (initial content: 16.7 wt% ACP).
Discussion
In the literature, there are several protocols for testing the biocompatibility of bone replacement materials. Some of them are not bone-specific [20–22] and sometimes these experiments are done after in vivo testing [23]. Although the number of materials proposed as bone substitutes is continuously increasing, so far there is no gold standard for initial biocompatibility tests in vitro. This study describes an easy way of initial bone-specific tests, to determine whether or not a novel biomaterial warrants further time and cost intensive in vivo testing. This is demonstrated for commercially available materials as well as for newly designed bone substitutes. This analysis takes into account physical, biochemical and morphological criteria of bone cell cultures.
Osteoblast specific biocompatibility testing
The question of the cell source to be used is of prime importance. First, many assays rely on fibroblasts for biocompatibility and toxicity testing [24]. Fibroblasts are easy to cultivate in vitro and the results are highly reproducible, but not bone specific. Other researchers used human bone-derived cells, which are also possible, to examine the attachment of these cells on different polymers [25–29]. Only bone-derived cells can confer specificity towards bone to the test.
Second, the question remains what kind of bone-derived cells should be used. While osteoblast-like cell-lines like other authors used for biocompatibility testing [30–34] offer the advantage of easy handling, unlimited availability and high efficiency in terms of financial and human resources, one limitation is their inability to differentiate. This might be critical especially in the context of implant testing where the stimuli of the material and their consequences on cell behavior are of paramount importance. Therefore, we used authentic cells to allow a full appreciation of the biologic effects of the materials tested within the limits of the in vitro situation. However, Macnair et al. [35] compared the response of primary rat and human osteoblasts and immortalized rat osteoblast cell lines and found that even immortalized rat osteoblasts can provide a useful in vitro system for the testing of orthopaedic materials. Therefore these cell lines can also be useful with their advantage of easy repeatability and reproducibility.
Primary osteoblasts obtained from mouse calvaria combine the capacity to react within the complete physiological range of an authentic cell with the advantage of a comparatively high cell homogeneity and availability. For these two reasons, we decided to perform the experiments using authentic primary osteoblasts as the cell source.
pH-dependent cell growth on various materials
The aim of our study was to examine in vitro the osteoblast-specific biocompatibility of a new bone replacement material before in vivo testing in animals. Controlling the method we compared the results given from the new biomaterials with three industrially manufactured substances, i.e. bioglass, glass ceramics, and α-TCP which are all currently used as bone substitutes.
It is known that minor changes in the extracellular pH can affect osteoblast activity and/or differentiation [36, 37]. Note that in vivo the use of polyesters as bone substitute material is often followed by local osteolysis due to the local acidification caused by polymer degradation [38, 39]. Therefore the first requirement for a future bone substitute material is that in its presence the pH of the culture medium must remain within the narrow limits of the cell physiological range (7.2–7.6). All but one (PHBHV–ACP) of the tested substances met this first requirement and demonstrated a constant pH throughout the entire culture period beyond the first day.
Alkaline degradation of PHBHV–ACP leads to cell death of osteoblasts in vitro
In the presence of PHBHV–ACP the pH increased beyond the physiological range and the culture media remained within the alkaline range throughout the experiments. Consequently, all cells died when incubated in the presence of PHBHV–ACP which clearly excludes PHBHV–ACP from being an attractive bone substitute material. The increased pH appears to be the primary reason for cell death in the PHBHV–ACP experiment, but a general incompatibility of this substance with bone cells is also possible. Cell experiments were also performed with pure polymer PHBHV (i.e. without ACP). They led to hesitant and insufficient cell growth, suggesting that the reason for the biological incompatibility lies with the polymer and not with the calcium phosphate. After testing the physical and chemical properties, the next parameters to be determined are the cellular activity and differentiation.
Good biocompatibility of bioglass, glass ceramic, α-TCP and PHB–ACP
The excellent biocompatibility of bioglass, glass ceramics, α-TCP and PHB–ACP is demonstrated by the early confluence of the cells after 4 days. The good biocompatibility of bioglass, glass ceramics and α-TCP is in accordance with the results of other authors [13, 32, 40]. Osteoblast differentiation and function can be tested by analysis of alkaline phosphatase and collagen, i.e. major products typically expressed by osteoblasts.
Enzyme labeling for AP and van Gieson staining for collagen are easy and established methods [3, 17, 41] and additionally allow expression analysis in the direct proximity of the probes. However, the final proof that osteoblastic differentiation is maintained requires an osteoblast-specific marker. The proof of collagen and alkaline phosphatase alone is not sufficient [42, 43]. As of today, this criterion is only met by osteocalcin. Therefore the demonstration of osteocalcin expression in the cells growing on top of the pellets firmly establishes bone cell biocompatibility of the materials. Again, as for the demonstration of AP and collagen, immunolabeling for osteocalcin and visualization by confocal laser microscopy have the great advantage of allowing to localize the expression and its pattern.
The analysis is completed by histology on undecalcified sectioning of grinding dependent on the material properties of the probes, respectively. In the case of the present study, a monolayer is present on bioglass while a cell multilayer with increasing thickness was found on glass ceramic, α-TCP and the newly designed composite of PHB and calcium phosphate. The cell–implant-interface shows the direct contact of the osteoblasts with the latter materials. Morphological analysis can be completed and confirmed by ultrastructural scanning electron microscopy.
Conclusions
The biocompatibility of a new potential bone substitution material consisting of poly-3-hydroxybutyrate and bone-like calcium phosphate (PHB–ACP) was demonstrated by osteoblast-specific biocompatibility testing consisting of long-term cell culture with primary mouse osteoblasts. Evidence for the good biocompatibility was derived from light microscopy (cell morphology), histology (expression of alkaline phosphatase, collagen and osteocalcin) and scanning electron microscopy. A homologous material consisting of poly-3-hydroxybutyrate-co-3-hydroxyvalerate and bone-like calcium phosphate (PHBHV–ACP) resulted in a pH in the cell culture of about 7.9, leading to complete cell death after 10 days. The proposed standard protocol was also tested on three well-established biomaterials: glass ceramics, bioglass and α-tricalcium phosphate.
In conclusion we established a simple and reproducible method for an in vitro testing of the osteoblast-specific biocompatibility of bone replacement materials.
References
Doyle C, Tanner ET, Bonfield W (1991) Biomaterials 12:841
Agrawal CM, Athanasiou KA (1997) J Biomed Mater Res 38: 105
Linhart W, Peters F, Lehmann W, Schilling AF, Schwarz K, Amling M, Rueger JM, Epple M (2001) J Biomed Mater Res 54:162
Schiller C, Epple M (2003) Biomaterials 24:2037
Schiller C, Rasche C, Wehmöller M, Beckmann F, Eufinger H, Epple M, Weihe S (2004) Biomaterials 25:1239
Doi Y, Shibutani T, Moriwaki Y, Kajimoto T, Iwayama Y (1998) J Biomed Mater Res 39:603
Doi Y, Iwanaga H, Shibutani T, Morikawa Y, Iwayama Y (1999) J Biomed Mat Res 47:424
Weiner S, Wagner HD (1998) Annu Rev Mater Sci 28:271
Tadic D, Peters F, Epple M (2002) Biomaterials 23:2553
Chen LJ, Wang M (2002) Biomaterials 23:2631
Berger G, Gildenhaar R, Ploska U (1995) Biomaterials 16:1241
Reif D, Leuner B, Hotz G (1998) In: CL, A Ignatius (eds) Biodegradierbare Implantate und Materialien, p 270
Ignatius AA, Schmidt C, Kaspar D, Claes LE (2001) J Biomed Mater Res 55:285
Quagliano JC, Miyazaki SS (1997) Appl Microbiol Biotechnol 48:662
Elliot JC (1994) Structure and chemistry of the apatites and other calcium orthophosphates, Studies in inorganic chemistry, Elsevier, Amsterdam
Amling M, Neff L, Tanaka S, Inoue D, Kuida K, Weir E, Philbrick WM, Broadus AE, Baron R (1997) J Cell Biol 136:205
Ducy P, Starbuck M, Priemel M, Shen J, Pinero G, Geoffroy V, Amling M, Karsenty G (1999) Genes Develop 13:1025
Termine JD, Peckauskas RA, Posner AS (1970) Arch Biochem Biophys 140:318
Ofir PBY, Govrin-Lippman R, Garti N, Füredi-Milhofer H (2004) Cryst Growth Design 4:177
Brook IM, Craig GT, Hatton PV, Jonck LM (1992) Biomaterials 13:721
Lin FH, Yao CH, Sun JS, Liu HC, Huang CW (1998) Biomaterials 19:905
Marques AP, Reis RL, Hunt JA (2002) Biomaterials 23:1471
Keller JC, Collins JG, Niederauer GG, Mcgee TD (1997) Dental Mater 13:62
Ruano R, Jaeger RG, Jaeger MM (2000) J Periodontol 71:540
Oliva A, Della RF, Salerno A, Riccio V, Tartaro G, Cozzolino A, D’amato S, Pontoni G, Zappia V (1996) Biomaterials 17:1351
Oliva A, Salerno A, Locardi B, Riccio V, Della RF, Iardino P, Zappia V (1998) Biomaterials 19:1019
McFarland CD, Mayer S, Scotchford C, Dalton BA, Steele JG, Downes S (1999) J Biomed Mater Res 44:1
Disilvio L, Dalby MJ, Bonfield W (2002) Biomaterials 23:101
Dalby MJ, Bonfield W, Disilvio L (2003) J Mater Sci Mater Med 14:693
Hendrich C, Geyer M, Scheddin D, Schütze N, Eulert J, Thull R (1996) Biomed Technik 41:278
Hendrich C, Noth U, Stahl U, Merklein F, Rader CP, Schutze N, Thull R, Tuan RS, Eulert J (2002) Clin Orthop Rel Res:278
Mayr-Wohlfart U, Fiedler J, Gunther KP, Puhl W, Kessler S (2001) J Biomed Mater Res 57:132
Rea SM, Best SM, Bonfield W (2004) J Mater Sci Mater Med 15:997
Brodie JC, Goldie E, Connel G, Merry J, Grant MH (2005) J Biomed Mater Res Appl Biomater 73:409
Macnair R, Rodgers EH, Macdonald C, Wykman A, Goldie I, Grant MH (1997) J Mater Sci Mater Med 8:105
Frick KK, Jiang L, Bushinsky DA (1997) Am J. Physiol. 272:1450
Kaysinger KK, Ramp WK (1998) J Cell Biochem 68:83
Martin C, Winet H, Bao JY (1996) Biomaterials 17:2373
Winet H, Bao JY (1997) J Biomater Sci Polymer Edn 8:517
Sous M, Bareille R, Rouais F, Clement D, Amedee J, Dupuy B, Baquey C (1998) Biomaterials 19:2147
Ducy P, Schinke T, Karsenty G (2000) Science 289:1501
Ishaug SL, Yasemski MJ, Bizios R, Mikos AG (1994) J Biomed Mater Res 28:1445
Knabe G, Gildenhaar R, Berger G, Ostapowicz W, Fitzner R, Radlanski RJ, Gross U (1997) Biomaterials 18:1339
Acknowledgments
We thank C. Müldner, R. Walter, D. Keyser, and D. Tadic for experimental assistance. Financial assistance by the Deutsche Forschungsgemeinschaft (Graduiertenkolleg 476 to J.M.R. and M.E.; fellowships to A.F.S., K.S. and M.S.) is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Additional information
No benefit of any kind will be received either directly or indirectly by the authors.
W. Linhart and W. Lehmann contribute equally and therefore share first authorship
Rights and permissions
About this article
Cite this article
Linhart, W., Lehmann, W., Siedler, M. et al. Composites of amorphous calcium phosphate and poly(hydroxybutyrate) and poly(hydroxybutyrate-co-hydroxyvalerate) for bone substitution: assessment of the biocompatibility. J Mater Sci 41, 4806–4813 (2006). https://doi.org/10.1007/s10853-006-0023-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-006-0023-x