Abstract
Background
Contact force-sensing technology has become a widely used addition to catheter ablation procedures. Neither the optimal contact force required to achieve adequate lesion formation in the ventricle, nor the impact of left ventricular access route on contact force has been fully clarified.
Patients and methods
Consecutive patients (n = 24) with ischemic cardiomyopathy who underwent ablation for scar-related ventricular tachycardia were included in the study. All ablations (n = 25) were performed using irrigated contact force-sensing catheters (Smart Touch, Biosense Webster). Effective lesion formation was defined as electrical unexcitability post ablation at sites which were electrically excitable prior to ablation (unipolar pacing at 10 mA, 2 ms pulse width). We explored the contact force which achieved effective lesion formation and the impact of left ventricular access route (retrograde aortic or transseptal) on the contact force achieved in various segments of the left ventricle. Scar zone was defined as bipolar signal amplitude < 0.5 mV.
Results
Among 427 ablation points, effective lesion formation was achieved at 201 points (47.1%). Contact force did not predict effective lesion formation in the overall group. However, within the scar zone, mean contact force ≥ 10 g was significantly associated with effective lesion formation [OR 3.21 (1.43, 7.19) P = 0.005]. In the 12-segment model of the left ventricle, the retrograde approach was associated with higher median contact force in the apical anterior segment (31 vs 19 g; P = 0.045) while transseptal approach had higher median force in the basal inferior segment (25 vs 15 g; P = 0.021). In the 4-segment model, the retrograde approach had higher force in the anterior wall (28 vs 16 g; P = 0.004) while the transseptal approach had higher force in the lateral wall (21 vs 18 g; P = 0.032). There was a trend towards higher force in the inferior wall with the transseptal approach, but this was not statistically significant (20 vs 15 g; P = 0.063).
Conclusions
In patients with ischemic cardiomyopathy, a mean contact force of 10 g or more within the scar zone had the best correlation with electrical unexcitability post ablation in our study. The retrograde aortic approach was associated with better contact force over the anterior wall while use of a transseptal approach had better contact force over the lateral wall.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Catheter ablation for ventricular tachycardia (VT) can reduce recurrent implantable cardioverter defibrillator (ICD) shocks and VT storm in patients with ischemic cardiomyopathy (ICM) [1,2,3]. Ablation can be limited, however, by the presence of deep substrate for the VT circuit. Despite advances in technical methods for creating deep lesions [4,5,6,7,8], most procedures are performed using standard irrigated ablation catheters. Contact force-sensing technology has become widely adopted as a tool to ensure catheter-tissue contact during radiofrequency (RF) ablation [9] and thus has the potential to lead to more reliable delivery of deeper ablation lesions [10, 11]. Currently, two contact force-sensing technologies are available; one uses microdeformation of three optical fibers connected to the catheter tip (TactiCath, Abbott medical), and the other relies on microdeflection of a spring connecting the tip of the ablation catheter with its shaft (Smart Touch, Biosense Webster). Both technologies have high resolution (< 1 g) and have been extensively validated before clinical use [12].
The role of contact force in atrial fibrillation (AF) ablation has been studied in a meta-analysis of 11 clinical trials (2 randomized and 9 cohort trials) involving 1428 adult patients, finding that the use of contact force was associated with a lower recurrence rate as well as a shorter procedure and shorter fluoroscopy times with no increase in complication rate [13]. The current guidelines recommend a minimal contact force of 5–10 g when performing AF ablation with a contact force-sensing catheter [14].
The role of contact force sensing in VT ablation has not been as clearly defined. In animal studies, it was found that 22% of the radiofrequency applications without the use of contact force do not result in identifiable lesion formation [15]. Ablation lesion size and depth in the right and left ventricles increased significantly with increasing contact force [16]. In a retrospective case series, the use of contact force was not associated with reduced recurrence in patients undergoing VT ablation [17].
The optimal contact force required to achieve adequate lesions in ventricular tachycardia ablation is unknown, as is the impact of access route to the left ventricle. We explored the optimal contact force that correlated with effective lesion formation in patients with ischemic cardiomyopathy (ICM) undergoing VT ablation.
2 Methods
2.1 Patient population
Consecutive patients undergoing ablation for ischemic scar-related sustained monomorphic ventricular tachycardia were included in the study. Patients were included if they had ischemic cardiomyopathy (ICM) and their ablation was performed with a contact force-sensing catheter. Patients were excluded if they had non-ischemic cardiomyopathy and idiopathic VT or if their ablation was performed with a non-contact force-sensing catheter. The study was approved by the research ethics board at our institution.
2.2 Ablation procedure
Ablation was performed under conscious sedation or general anesthesia using fluoroscopy and an electroanatomic mapping system (Carto3, Biosense Webster). Vascular access was obtained through the femoral veins bilaterally; femoral arterial access was obtained in all cases for pressure monitoring or retrograde aortic access to the left ventricle (LV). Access to the left ventricle was obtained either via the retrograde aortic approach or via the transseptal approach depending on operator preference. A large curve deflectable sheath (Agilis, Abbott medical) was used for transseptal cases. An irrigated contact force-sensing catheter (Smart Touch Thermocool or Thermocool SF, Biosense Webster) was used for ablation in all patients. Surround-flow catheters were used in about one third of the patients when they became available to us. Mapping of the left ventricle was performed using the ablation catheter or a 20-pole high-density multipolar catheter (Pentaray, Biosense Webster).
Left ventricular access route was recorded and a 12-segment model of the left ventricle was used (apical anterior, lateral, inferior, septal; mid-anterior, lateral, inferior, septal; basal anterior, lateral, inferior, septal). Additionally, a 4-segment model (anterior, lateral, inferior, and septal) was derived from the 12-segment model. Contact force was recorded at each ablation point, and the median force in each segment of the 12- and the 4-segment models was compared according to left ventricular access route.
Bipolar electrograms were recorded between the distal 3.5-mm tip of the ablation catheter and the ring electrode and filtered 16–500 Hz. Unipolar electrograms were recorded from the distal tip of the ablation catheter using a 1-mm ring electrode in the inferior vena cava as the indifferent electrode and were filtered 2–240 Hz. A sinus rhythm voltage map was created in all patients, and according to bipolar signal amplitude, the endocardium was defined as normal myocardium (bipolar signal amplitude > 1.5 mV), scar border zone (bipolar signal amplitude 0.5–1.5 mV), and scar zone (bipolar signal amplitude < 0.5 mV) (Fig. 1).
a Bipolar voltage map of the left ventricle in RAO view with superior angulation (0.05–1.5 mV). b Contact force map of the left ventricle in the same view (3–10 g). c Contact force > 10 g within the scar zone is associated with effective lesion formation with electrical unexcitability post ablation. d Contact force<10 g is associated with ineffective lesion formation with electrically excitable tissue present post ablation
VT was induced with a standard programmed stimulation protocol. If VT was hemodynamically tolerated, activation and entrainment mapping was performed, followed by ablation of the mapped tachycardia as well as substrate modification. If VT was not tolerated, substrate modification was performed targeting potential channels within the scar identified by presence of late potentials or sites which captured with latency (> 40-ms stimulus-QRS delay). Procedural endpoints were either VT non-inducibility or elimination of all identifiable potential channels within the scar.
At each potential ablation site, unipolar pacing was performed at an amplitude of 10 mA and pulse width of 2 ms between the distal tip of the ablation catheter and the indifferent electrode before ablation. If the site was electrically unexcitable (no myocardial capture), it was labeled as scar and no ablation was performed. If it was electrically excitable (myocardial capture), ablation was performed and immediately after ablation unipolar pacing at 10 mA@2 ms was repeated. An effective lesion was defined as electrical unexcitability post ablation in sites that were electrically excitable before ablation. For each ablation site, we collected contact force information as well as other conventional ablation parameters such as power, temperature, impedance, and unipolar and bipolar signal amplitudes. Ablation points were included in the analysis only if pacing was performed before and after the ablation. Lesions were classified as effective (electrically unexcitable post ablation) or ineffective (electrically excitable post ablation). Delta impedance was defined as maximum-minimum impedance during ablation.
2.3 Statistical analysis
Continuous variables were expressed as mean ± standard deviation and categorical variables were expressed as frequency (percentage). Ablation parameters including contact force, duration of ablation, power, temperature, baseline impedance, delta impedance, unipolar voltage, and bipolar voltage were compared between effective and ineffective ablation lesion sites in different scar zones using Student’s t test. A logistic regression model was constructed using conventional ablation parameters to examine the association between contact force and effective lesion formation. Contact force thresholds of 5, 10, 15, and 20 g were tested as predictors for electrical unexcitability post ablation in scar zone and border zone. Results were presented as odds ratios (OR) and 95% confidence intervals (CI). For the LV segment analysis, force was expressed as median (interquartile range) and tested using Wilcoxon rank sum test. Significance was defined as P < 0.05. Statistical analysis was performed using SAS version 9.4 (The SAS Institute, Cary, NC).
3 Results
Twenty-five ablation procedures were performed in 24 patients between February 2014 and April 2017. All patients were males, mean age was 67 ± 8 years, and mean ejection fraction was 34.2 ± 9.4%. Mean procedure time was 5.6 ± 1.3 h and fluoroscopy time was 17.5 ± 8.3 min. The mean number of RF applications was 60 ± 41 and the mean RF time was 38.6 ± 28.4 min (Table 1). Surround-flow ablation catheters were used in 8 procedures. A 20-pole high-density multipolar catheter was used for mapping the left ventricle in 8 procedures. Left ventricular access was obtained via retrograde aortic approach in 18 procedures and via transseptal approach in 7 procedures. The patient that had a repeat procedure had a retrograde approach for the first procedure and a transseptal approach for the second procedure. No patients had combined retrograde and transseptal approach in the same procedure.
VTs were unmappable (either non-inducible or hemodynamically not tolerated) in 14 procedures leading to a substrate modification approach. Activation and entrainment mapping was performed in the 11 procedures where one or more VTs were inducible and tolerated. Induction testing at the end of ablation was performed in 15 procedures; it was not performed in the other procedures due to the length of the procedure or the decision not to perform further ablation. Twelve out of 15 patients had no inducible VT after ablation. Two patients had ventricular flutter induced (cycle length < 240 ms), and one patient had ventricular fibrillation induced at the end of procedure.
Among 1497 ablation points, 427 fulfilled the criteria for inclusion in the study. The other points were excluded because pacing was either not performed or was performed only before or only after the ablation. An effective ablation lesion was achieved at 201 points (47.1%). In univariate analysis, lower baseline impedance within the scar zone was the only variable significantly associated with effective lesion formation (119.8 ± 12.7 vs 122.9 ± 11.7 Ω, P = 0.038). Mean contact force was not different between effective and ineffective ablation lesions both within the scar zone (20.6 ± 11.7 vs 19.5 ± 10.9 g, P = 0.45) as well as the border zone (18.9 ± 8.3 vs 19.6 ± 10.8 g, P = 0.61) respectively (Table 2).
Within the scar zone, contact force ≥ 10 g was more likely to be associated with effective lesion formation both in univariate [OR for effective lesion formation 2.76, 95% CI 1.24–5.75, P = 0.01] as well as multivariate analysis [OR for effective lesion formation 3.21, 95% CI 1.43–7.19, P = 0.005]. Other clinically relevant contact force thresholds (5, 15, and 20 g) were not significantly associated with effective lesion formation either within or outside the scar zone (Table 3).
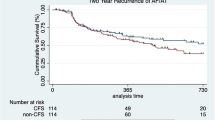
In the 12-segment model of the left ventricle, use of the retrograde approach was associated with higher median contact force in the apical anterior segment (31 vs 19 g; P = 0.045) while transseptal approach had higher median force in the basal inferior segment (25 vs 15 g; P = 0.021) (Fig. 2). In the 4-segment model, retrograde approach had higher force on the anterior wall (28 vs 16 g; P = 0.004) while transseptal approach had higher force on the lateral wall (21 vs 18 g; P = 0.032). There was a trend towards higher force in the inferior wall with the transseptal approach, but this was not statistically significant (20 vs 15 g; P = 0.063) (Table 4, Fig. 3).
Contact force (median, IQR) in the 4- and 12-segment models according to left ventricle access route. a Contact force (in grams, median (IQR)) in 12-segment LV model according to access route. (1) Apical anterior, (2) apical lateral, (3) apical inferior, (4) apical septal, (5) mid-anterior, (6) mid-lateral, (7) mid-inferior, (8) mid-septal, (9) basal anterior, (10) basal lateral, (11) basal inferior, and (12) basal septal. b Contact force (in grams, median (IQR)) in 4-segment LV model according to access route
4 Discussion
We demonstrated that a contact force of 10 g or more within the scar zone was significantly associated with electrical unexcitability post ablation, a marker of an effective ablation lesion. A number of endpoints for ablation of scar-related VT have been studied, among which non-inducibility of any VT with programmed stimulation has the most established predictive value [18]. Electrical unexcitability post ablation is an important endpoint particularly in substrate-based ablation procedures [19, 20]. Although it has not been validated in the ventricle, loss of capture post ablation in the atrium has been correlated with transmural lesion [21] and the change in pacing threshold has been correlated with lesion size in the ventricle [22].
Our results provide clinical evidence for the use of contact force-sensing technology to help guide ventricular tachycardia ablation. The lack of a demonstrable effect in the scar border zone is unsurprising; it is often more difficult to achieve sufficient lesion size to prevent capture with high output pacing in this area, presumably because of the nearby volume of healthier myocardium. It may be reasonable to extrapolate the relationship between contact force and lesion creation to the border zone.
We found no clear association between mean contact force and electrical unexcitability post ablation. This may be because incremental increases in contact with each gram of force do not have the same effect in various contact force ranges, i.e., the effect of contact force on effective lesion creation may be non-linear. Hence, we tested thresholds of 5, 10, 15, and 20 g. The 10-g threshold was the only one that was significantly associated with electrical unexcitability post ablation. It is important to note that in order to test these thresholds, we compared force range below and above a particular threshold. For example, the 10-g threshold was tested by comparing electrical excitability for all points with less than 10 g of force against points with 10 g or more. It is therefore not surprising that the higher cutoffs of 15 and 20 g were not significant as the force range below these thresholds was sufficient to create an effective lesion.
In atrial fibrillation ablation, a contact force < 20 g or a force time integral of < 400 g/s was significantly associated with reconnections post ablation [23]. The current guidelines recommend a minimum contact force of 5–10 g during atrial fibrillation ablations [14]. Similar evidence and guidelines are not available for ventricular tachycardia ablation. In terms of catheter contact in the ventricle, Jesel et al. reported that the optimal contact force threshold to obtain a signal amplitude of > 1.5 mV in the LV endocardium was 7 g [24].
We also demonstrated that the contact force achieved in various segments of the left ventricle is significantly influenced by the left ventricular access route. Previously, Tilz et al. reported that retrograde aortic approach was associated with higher contact force in the basal segments of the left ventricle while transseptal approach had higher force in the apical, mid-lateral, and mid-anteroseptal segments [25] while Jesel et al. found that transseptal approach was associated with higher force in the apical inferior and apical septal regions [24].
In our study, we studied two models of the left ventricle. In the 4-segment model, the retrograde aortic approach achieved significantly higher contact force in the anterior wall while transseptal approach achieved better contact over the lateral wall. In the 12-segment model, retrograde approach was associated with higher contact force in the apical anterior segment while transseptal approach resulted in better contact for the basal inferior segment. The difference between our results and previous studies is possibly due to the relatively small size of the studies and the use of different LV segment models. Our findings could help procedural planning by choosing the most appropriate access route based on the underlying scar and the expected VT exit sites from the 12 lead ECG.
5 Conclusions
In summary, in patients with ischemic cardiomyopathy undergoing VT ablation, a contact force threshold of 10 g or more within the scar zone had the best correlation with electrical unexcitability post ablation in our study. Retrograde aortic approach was associated with better contact force over the anterior wall while a transseptal approach achieved better contact on the lateral wall.
6 Limitations
This is a single-center study which may limit generalizability of the results. Its retrospective nature and the lack of blinded adjudication might confound the results, although this is mitigated by the use of objective measures. Although electrical unexcitability is a useful surrogate for ablation lesion effectiveness, it has not been validated in the ventricle. It is possible that pacing post ablation could result in far field capture; however, we used unipolar pacing configuration to avoid anodal capture and monitored tip positioning using three-dimensional mapping to avoid movement. Left ventricular access route was based on operator preference which could introduce operator bias. In our study, we used mean contact force, which does not consider potential variations in contact during the time of RF, due to cardiac motion or catheter movement. Further prospective studies are required to validate our results.
References
Reddy VY, Reynolds MR, Neuzil P, Richardson AW, Taborsky M, Jongnarangsin K, et al. Prophylactic catheter ablation for the prevention of defibrillator therapy. N Engl J Med. 2007;357(26):2657–65.
Kuck K-H, Schaumann A, Eckardt L, Willems S, Ventura R, Delacrétaz E, et al. Catheter ablation of stable ventricular tachycardia before defibrillator implantation in patients with coronary heart disease (VTACH): a multicentre randomised controlled trial. Lancet. 2010;375(9708):31–40.
Sapp JL, Wells GA, Parkash R, Stevenson WG, Blier L, Sarrazin J-F, et al. Ventricular tachycardia ablation versus escalation of antiarrhythmic drugs. N Engl J Med. 2016;2016(375):111–21.
AbdelWahab A, Stevenson W, Thompson K, Parkash R, Gray C, Gardner M, et al. Intramural ventricular recording and pacing in patients with refractory ventricular tachycardia: initial findings and feasibility with a retractable needle catheter. Circ Arrhythm Electrophysiol. 2015;8:1181–8. https://doi.org/10.1161/CIRCEP.115.002940.
Sapp JL, Beeckler C, Pike R, Parkash R, Gray CJ, Zeppenfeld K, et al. Initial human feasibility of infusion needle catheter ablation for refractory ventricular tachycardia clinical Perspective. Circulation. 2013;128(21):2289–95.
Abdelwahab A, Sapp JL. NaviStar® ThermoCool® catheter for ventricular tachycardia. Expert Rev Med Devices. 2007;4(3):307–14.
Gizurarson S, Spears D, Sivagangabalan G, Farid T, Ha AC, Massé S, et al. Bipolar ablation for deep intra-myocardial circuits: human ex vivo development and in vivo experience. Europace. 2014;16(11):1684–8.
Kay GN, Epstein AE, Bubien RS, Anderson PG, Dailey SM, Plumb VJ. Intracoronary ethanol ablation for the treatment of recurrent sustained ventricular tachycardia. J Am Coll Cardiol. 1992;19(1):159–68.
Matía Francés R, Hernández Madrid A, Delgado A, Carrizo L, Pindado C, Moro Serrano C, et al. Characterization of the impact of catheter–tissue contact force in lesion formation during cavo-tricuspid isthmus ablation in an experimental swine model. Europace. 2013;16(11):1679–83.
Kimura M, Sasaki S, Owada S, Horiuchi D, Sasaki K, Itoh T, et al. Comparison of lesion formation between contact force-guided and non-guided circumferential pulmonary vein isolation: a prospective, randomized study. Heart Rhythm. 2014;11(6):984–91.
Jarman JW, Panikker S, Das M, Wynn GJ, Ullah W, Kontogeorgis A, et al. Relationship between contact force sensing technology and medium-term outcome of atrial fibrillation ablation: a multicenter study of 600 patients. J Cardiovasc Electrophysiol. 2015;26(4):378–84.
Nakagawa H, Jackman WM. The role of contact force in atrial fibrillation ablation. J Atr Fibrillation. 2014;7(1)
Shurrab M, Di Biase L, Briceno DF, Kaoutskaia A, Haj-Yahia S, Newman D, et al. Impact of contact force technology on atrial fibrillation ablation: a meta-analysis. J Am Heart Assoc. 2015;4(9):e002476.
Calkins H, Hindricks G, Cappato R, Kim Y-H, Saad EB, Aguinaga L, et al. HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. J Arrhythm. 2017;14(10):e275–444.
Sacher F, Wright MJ, Derval N, Denis A, Ramoul K, Roten L, et al. Endocardial vs. epicardial ventricular radiofrequency ablation: utility of in vivo contact force assessment. Circ Arrhythm Electrophysiol. 2013;6:144–50. https://doi.org/10.1161/CIRCEP.111.974501.
Ikeda A, Nakagawa H, Lambert H, Shah DC, Fonck E, Yulzari A, et al. Relationship between catheter contact force and radiofrequency lesion size and incidence of steam pop in the beating canine heart clinical perspective. Circ Arrhythm Electrophysiol. 2014;7(6):1174–80.
Hendriks AA, Akca F, DABIRI ABKENARI L, Khan M, Bhagwandien R, YAP SC, et al. Safety and clinical outcome of catheter ablation of ventricular arrhythmias using contact force sensing: consecutive case series. J Cardiovasc Electrophysiol. 2015;26(11):1224–9.
Santangeli P, Frankel DS, Marchlinski FE. End points for ablation of scar-related ventricular tachycardia. Circ Arrhythm Electrophysiol. 2014;7(5):949–60.
Soejima K, Stevenson WG, Maisel WH, Sapp JL, Epstein LM. Electrically unexcitable scar mapping based on pacing threshold for identification of the reentry circuit isthmus: feasibility for guiding ventricular tachycardia ablation. Circulation. 2002;106(13):1678–83.
Kumar S, Romero J, Mehta NK, Fujii A, Kapur S, Baldinger SH, et al. Long-term outcomes after catheter ablation of ventricular tachycardia in patients with and without structural heart disease. Heart Rhythm. 2016;13(10):1957–63.
Kosmidou I, Houde-Walter H, Foley L, Michaud G. Loss of pace capture after radiofrequency application predicts the formation of uniform transmural lesions. Europace. 2013;15(4):601–6.
Sapp JL, Soejima K, Cooper JM, Epstein LM, Stevenson WG. Ablation lesion size correlates with pacing threshold. Pacing Clin Electrophysiol. 2004;27(7):933–7.
Neuzil P, Reddy VY, Kautzner J, Petru J, Wichterle D, Shah D, et al. Electrical reconnection after pulmonary vein isolation is contingent on contact force during initial treatment clinical perspective. Circ Arrhythm Electrophysiol. 2013;6(2):327–33.
Jesel L, Sacher F, Komatsu Y, Daly M, Zellerhoff S, Lim HS, et al. Characterization of contact force during endocardial and epicardial ventricular mapping. Circ Arrhythm Electrophysiol. 2014;7:1168–73. https://doi.org/10.1161/CIRCEP.113.001219.
Tilz RR, Makimoto H, Lin T, Rillig A, Metzner A, Mathew S, et al. In vivo left-ventricular contact force analysis: comparison of antegrade transseptal with retrograde transaortic mapping strategies and correlation of impedance and electrical amplitude with contact force. Europace. 2014;16(9):1387–95.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the research ethics board at our institution.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Elsokkari, I., Sapp, J.L., Doucette, S. et al. Role of contact force in ischemic scar-related ventricular tachycardia ablation; optimal force required and impact of left ventricular access route. J Interv Card Electrophysiol 53, 323–331 (2018). https://doi.org/10.1007/s10840-018-0396-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-018-0396-1