Abstract
Purpose
Contact with cardiac tissue is an important determinant of lesion efficacy during atrial fibrillation (AF) ablation. The Sensei X™ robotic navigation system (RNS) (Hansen Medical, Mountain View, CA, USA) has been validated for contact force (CF) sensing expressed in grams (g). The Thermocool® SmartTouch™ catheter enables the measurement of catheter tip CF and direction inside the heart. We aimed to investigate the catheter CF with and without RNS during pulmonary vein isolation (PVI) procedures.
Methods
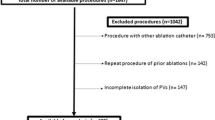
Eighty patients with symptomatic AF (56 males, age 63 ± 18) were enrolled in this study. Fifty-seven patients had paroxysmal AF and 23 early persistent AF. All procedures were performed with the Thermocool® SmartTouch™ ablation catheter. Forty patients were randomized to perform PVI with the Sensei X™ RNS (group 1), while in the other 40 patients (group 2), PVI was performed without the RNS.
Results
AF ablation was performed successfully in all patients without complications, while contact force was kept in the established 10–40 g range. A significantly higher CF was documented on the PVs in group 1 compared to group 2. The 1-year freedom from AF recurrence was higher in group 1 compared to group 2 (90 vs. 65 %, p = 0.04). Moreover, a significant reduction of fluoroscopy time was noted in the RNS group (13 ± 10 vs. 20 ± 10 min, respectively, p = 0.05).
Conclusions
The Sensei X™ RNS permits a significantly higher CF during transcatheter AF ablation with a low rate of AF recurrence at clinical follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, occurring in 1–2 % of the general population. Current international guidelines recommend catheter ablation of symptomatic AF refractory or intolerant to antiarrhythmic drugs [1, 2]. The pathogenesis of AF is complex, and several studies reported that pulmonary vein (PV) potentials play a critical role in both initiation and perpetuation of this arrhythmia; thus, pulmonary vein isolation (PVI) became the cornerstone of AF ablation [1, 2]. Transmural lesion is the hallmark of an effective and long-lasting radiofrequency (RF) lesion. Multiple studies demonstrated that one of the most important determinants in the creation of transmural lesion is the constant contact between the tip of the ablation catheter and the tissue [3–5]. A combination of qualitative measures, such as tactile feedback, fluoroscopic visualization, and electrogram amplitude assessment, are usually evaluated to estimate the quality of catheter tip-tissue contact. Insufficient contact could lead to ineffective lesions, and excess contact may increase the risk of complications such as perforation. To provide to operators with this information, new technologies have been developed to measure the contact force (CF) between the catheter tip and the target myocardium via a unique sensor located at the distal tip of an irrigated RF catheter (ThermoCool® SmartTouch™, Biosense Webster, Diamond Bar, CA, USA) [6, 7]. Furthermore, the Sensei X™ robotic navigation system (RNS) (Hansen Medical, Mountain View, CA, USA) has developed a contact sensor system called IntellisenseTM. Using force sensors and catheter ablation resistance measurement of the moving catheter, this system calculates the amount of perpendicular force in grams that the catheter is placing on the endocardium and displays it on the screen. IntellisenseTM has been validated for CF sensing expressed in grams; in particular, it has been shown that the optimal CF range, in terms of efficacy and safety, is between 10 and 40 g and a power setting of 40 W [8–15].
The aim of this study was to investigate the effect of RNS on CF using information provided by ThermoCool SmartTouch ablation catheter and to assess if CF values are increased when compared to manual approach. We sought also to determine if increased CF values could affect clinical follow-up.
2 Methods
2.1 Patient population
We prospectively enrolled 80 patients (mean age 61 ± 10 years; 56 male) from January 2013 to September 2013 for PVI procedures. All patients had symptomatic and drug-resistant AF according to the latest European Society of Cardiology guidelines [1]. Clinical data were accurately collected for each patient, such as cardiovascular risk factors, pharmacological therapy, clinical presentation, and left atrial size. After obtaining informed consent, the patients were randomized to perform PVI procedure using the ThermoCool SmartTouch ablation catheter with the RNS (group 1) or conventional manual ablation (group 2). A data manager, who was not involved in the analysis of the data and enrolment of the patients, generated the randomization sequence using a centralized web-based program. The sequence was integrated into a database created before the enrolment of the first patient. All PVI procedures were performed with the CARTO 3 electroanatomical mapping system (Biosense Webster, Diamond Bar, CA, USA). In the two study groups, we collected procedural details and CF data for all ablation sites targeted to achieve PVI.
The study was approved by the institutional review board.
2.2 ThermoCool SmartTouch and contact force technology
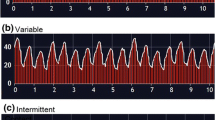
The SmartTouch catheter used in this study has the distal tip characterized by the presence of a tiny spring that connects the 3.5-mm irrigated tip dome to the proximal ring electrode. Before the mapping phase of the procedure, a calibration process was performed with the catheter in a “non-contact” position to set the baseline value. The force applied to the tissue results in the spring compression and/or stretching, and its magnitude and direction are monitored every 50 ms by the tracking of a magnetic signal between a transmitter located in the tip and three receiving sensors at the base of the spring. The real-time force is measured in grams and can be displayed as a chronological curve in the independent “real-time graph” window on the CARTO 3 screen. The direction of the force can be displayed as a color-coded arrow vector on the tip of catheter image on the main view of the CARTO 3 system.
2.3 Robotic navigation system
The RNS consists of a physician workstation located in the control room where there is a keyboard and a 3D joystick (InstinctiveMotion Controller; Hansen Medical) that allows the physician to control the robotic catheter manipulation arm attached to the EP lab table. The remote catheter manipulator controls two steerable sheaths (Artisan Extend Catheter, Hansen Medical), an outer (14F catheter) and inner one (10.5F catheter), through which any conventional ablation catheter can be inserted. The physician can navigate the catheter tip remotely, either in fluoroscopy, intracardiac echocardiography, or integrated with the 3D electroanatomic mapping systems. RNS provides through Intellisense (Hansen Medical) a continuous visual feedback on tissue-catheter contact considering an upper acceptable limit set of 40 g/cm2.
2.4 Pulmonary vein isolation
All PVI procedures were performed by experienced operators (>50 AF ablation/year, BHRS) [16] at Cardiac Arrhythmia Research Centre at Centro Cardiologico Monzino, Milan, Italy. All patients underwent pre-procedural transesophageal echocardiography to exclude left atrial thrombosis and a pre-procedure computed tomography with segmentation of the left atrium.
PVIs were carried out in conscious sedation using propofol infusion. An esophageal temperature probe was used in all patients (Esotherm Plus, FIAB) to monitor intraesophageal temperature increase. The probe was adjusted during the procedure to stay as close as possible to the ablation catheter. RF was interrupted when the endoluminal esophageal temperature increased above 39 °C, considered as cutoff limit. A decapolar catheter was placed into the coronary sinus. In all patients, intracardiac echocardiography probe was inserted in the left femoral vein through an 11F sheath in order to guide transseptal catheterization, assist placement of mapping and ablation catheters, and identify procedural complications (AcuNav Catheter, Siemens Acuson, Mountain View, CA, USA). Transseptal access to the left atrium (LA) was achieved using a standard 8.5F transseptal sheath (SL0 8.5F inner diameter, St. Jude Medical, St. Paul, MN, USA) and needle system (BRK, St. Jude Medical, St. Paul, MN, USA). Before transseptal puncture, heparin was administered intravenously as bolus (10,000 U) followed by a continuous infusion (1000 U/h) reaching ACT level >350 s. The transseptal sheath was continuously irrigated with heparinized saline (2 ml/h).
In the group 1, the ThermoCool SmartTouch catheter was introduced into the LA using the RNS. The Artisan sheath was inserted into a 14F sheath and manually advanced into the right atrium under fluoroscopic guidance and then attached to the robotic navigation arm. After manual transseptal puncture, the transseptal sheath was withdrawn back into the right atrium leaving a guide wire in the LA to mark the puncture site. The RNS was advanced across the interatrial septum following the guide wire. ICE imaging was useful to confirm the RNS position in the LA.
In the group 2, the catheter was manually introduced into the LA through a non-deflectable sheath (8.5F, SL0) positioned and kept in LA. In both groups, a circular multipolar diagnostic catheter (Lasso, Biosense Webster, Diamond Bar, CA, USA) was introduced through a second transseptal sheath into the LA and used to create the LA anatomy.
We performed circumferential PVI with RF application by dragging the catheter around the PVs and delivering energy at each point for 20–30 s until the PV potentials disappear. In both groups, RF settings was up to 25 W and 43 °C at the posterior wall of the LA and up to 35 W in other locations with the irrigation flow rate of 30 ml/min. Power was not adjusted according to CF values. In patients with early persistent AF, the ablation strategy was PVI and no additional linear ablations were created.
After ablation, effective PVI was confirmed by mapping with Lasso catheter, and the high-output PV pacing (12 V at 2.9 ms) was performed to confirm isolation. “Far field” capture and sensing were ruled out using differential pacing maneuvers. In all patients, early PV reconnection was tested during isoproterenol or adenosine infusion 30 min after PVI for each PV using the Lasso catheter. Procedures were performed either with continued oral anticoagulation using warfarin and therapeutic INR (2.0 to 2.5) or using low-molecular weight heparin bridging.
In the two study groups, CF data for all ablation sites targeted to achieve PVI were recorded and analyzed. In particular, each ipsilateral pair of PVs antra was divided into seven segments using CARTO 3 software (superior, antero-superior, postero-superior, carina, antero-inferior, postero-inferior, and inferior). Fluoroscopy time and procedural time, meant as skin-to-skin time, were collected.
2.5 Follow-up
After blanking period, patients were followed up in the outpatient clinic every 3 months. At each visit, a standard 12-lead ECG was obtained in all patients. Clinical events occurring during the follow-up and documentation of the events were carefully checked. All patients were followed up with 48-h Holter monitoring at 6 and 12 months after the PVI procedure. According to the latest HRS/EHRA/ECAS guidelines of atrial fibrillation ablation, arrhythmia recurrences were defined as episodes of AF/AFL/AT lasting >30 s documented by an ECG or Holter recording [2]. Since in the study population there were patients referred from different hospitals, they were followed up by the referring physician.
2.6 Endpoints
The primary endpoint of the study was the CF analysis during AF ablation. The secondary endpoints were comparisons of CF and the 1-year success rate, defined as freedom from AF, atrial flutter, and atrial tachycardia off antiarrhythmic drug therapy.
2.7 Statistical analysis
According to the literature, the CF during manual AF ablation is about 20 g [17, 18]. In our clinical experience, we noticed an increase on CF values using the RNS; for instance, we hypothesized an average of 30 g. Considering a standard deviation of 9 [17, 18], the sample size required to provide 0.90 statistical power and 0.01 significance level is at least 25 patients for each group. The number of enrolled patients of the present study ensures the maintenance of statistical power also in case of dropouts. All variables showing a distribution not significantly different from normal according to Kolmogorov–Smirnov were compared using the unpaired t test, whereas proportions were compared using the Fisher exact test. Variables showing a distribution significantly different from normal were compared using the Mann–Whitney U test. Data are reported as mean ± standard deviation or as median (range) or proportions. A two-tailed p value <0.05 was considered as statistically significant. SPSS 20.0 statistical software (SPSS Italia, Inc., Florence, Italy) was used for statistical analysis.
3 Results
After randomization, 40 patients were included in group 1 and 40 patients in group 2. Baseline clinical characteristics of patients are reported in Table 1. There were no significant differences between the two study groups regarding age, gender, cardiovascular risk factors, medical therapy, and form of AF. No patients had evidence of left atrial thrombosis during transesophageal echocardiography.
PVI with bidirectional block was achieved in all patients. The CF values in all PV segments were significantly higher in the RNS group; median CF values on each PV segments are reported in Fig. 1.
Acute PV reconnection was similar between the two study groups. Although a statistically significant difference was not observed, a trend has been observed in two specific PV segments: the ridge between left atrial appendage and left superior pulmonary vein (5 %, n = 2, in the robotic group vs. 17.5 %, n = 7 in the manual group, p = 0.07) and in the carina between the right PVs (2.5 %, n = 1, in the robotic group vs. 10 %, n = 5, in the manual group, p = 0.09).
A significant reduction in the fluoroscopy time was found in group 1 compared to group 2 (13 ± 10 vs. 20 ± 10 min, respectively, p = 0.05). Furthermore, in group 1, we found a significant increase in the procedure time compared to group 2 (184 ± 35 vs. 155 ± 52 min, respectively, p = 0.03). RNS setup and manipulation before the first RF delivery (i.e., setting of Artisan, hooking Artisan to the robotic arm, remote crossing of the interatrial septum) had significantly impacted the procedural time. RF time was similar in the two groups (1954 ± 654 vs. 1857 ± 912 s, p = ns). Cumulative time, from first to last ablation, although not statistically significant, was longer in the manual group (55 ± 21 vs. 65 ± 19 min, p = ns).
No patients had serious adverse events defined as phrenic nerve injury, pericardial effusion or tamponade, symptomatic cerebral ischemia, or esophageal injury. The Kaplan–Meier survival analysis confirmed a significant difference in freedom from AF between patients who underwent AF ablation using the RNS compared to manual procedures (Fig. 2). At 1-year follow-up, AF recurrence was documented in 4 patients (10 %) of group 1 and in 13 patients (32.5 %) of group 2 (p = 0.04). No further clinical adverse events were documented in other patients during clinical follow-up.
4 Discussion
The main finding of this randomized study is that the use of RNS associated with the ThermoCool SmartTouch ablation catheter increases CF values compared to manual approach. RNS allowed a significant reduction in the fluoroscopy time. Finally, patients who underwent AF ablation with the RNS showed lower AF recurrence rate at 1-year clinical follow-up.
AF is the most prevalent cardiac arrhythmia affecting 1 to 2 % of the general population. AF is known to increase the mortality risk 1.5- to 2-fold and the risk for stroke 5-fold. Current international guidelines recommend catheter ablation in patients with symptomatic AF after failure of antiarrhythmic drugs [1, 2]. Expert consensus acknowledges the importance of PV targets in the strategy of AF ablation and recommends that when PVs are targeted, complete electrical isolation should be achieved [1, 2]. PV isolation is reported to achieve durable sinus rhythm without the need for antiarrhythmic drugs in 59 to 93 % of patients with paroxysmal AF and in 20 to 61 % of patients with persistent AF [1, 2]. Arrhythmia recurrences after PV isolation are mostly due to resumption of conduction at the PV-left atrium junction [3–5]. Theoretically, the single procedure efficacy of AF ablation would be improved by creating effective transmural ablation lesions that result in more durable PVI. In addition to power and time, which are the conventional parameters adjusted during RF ablation, CF is equally important and only recently have been developed ablation catheters that have the capability to measure CF. Several studies reported that higher CF values (between 10 and 20 g) are associated with an increased ablative lesion size [6, 7, 19, 20]. Haldar et al. [6] reported a significantly lower acute PV reconnection rate (4 %) when CF information was used in real-time during PVI compared to a control group (21 %), which was blinded to the CF information. This suggests that the difference may be due to improved initial lesion formation resulting in permanent myocyte injury, particularly in regions prone to reconnection. Nakagawa et al. tested the ability of atrial potential amplitude and impedance to predict CF between three blinded operators. They found not only that these parameters are poor predictors of CF but also a wide range of CF values (1–144 g) with low median CF (8.2 g) for all operators. High CF values were transiently found, mostly during inspiration, at the rightward roof of the left atrium [21].
Regarding RNS in catheter ablation of AF, in 2012, Bai and colleagues published the worldwide experience [9]. In this study, the authors reported data of 1728 procedures performed at 12 centers with an overall complication rate of 4.7 % and a success rate of 67.1 % after 18 months of follow-up, suggesting that the RNS was effective and safe to increase catheter-tissue CF during PVI and to reduce AF recurrence rate [8–14]. In terms of fluoroscopy time, Steven et al. showed that the combination of RNS and 3D mapping significantly reduced the overall fluoroscopy time and also the operator’s fluoroscopy exposure. However, this study did not focus on the feasibility of performing PVI using the RNS, neither did it aim for long-term follow-up data [22].
In a recent large randomized trial, no significant differences were noted in 1-year single-procedure success rate of AF ablation as well as the procedural time between the manual and the robotic approach [23]. In both arms, a traditional irrigated ablation catheter without CF was used. However, the authors found a significant advantage in the fluoroscopy time and in terms of stability of the catheter evaluated in a semi-quantitative manner. This study also suggested a significant reduction in the subjectively assessed operator fatigue. This aligns with a recent publication showing that operators who ablated with real-time CF data available had lower acute PV reconnection rates than operators blinded to the CF information.
This is the first randomized study showing that position stability of the ablation catheter with RNS allows operators to reach higher values of CF compared to manual approach. Moreover, RNS with real-time CF data given by ThermoCool SmartTouch ablation catheter helps operators to stay within their selected CF range during most of the RF application. These data strongly support the notion that real-time CF sensing is important in affecting long-term ablation outcomes. In fact, the 1-year freedom from AF recurrence appears to be higher than shown in previous studies with similar patient populations and study protocols using the traditional irrigated ablation catheter without CF monitoring [23]. Recently, Ullah et al. reported a significant increase of 1-year success rate in patients undergoing persistent AF ablation with RNS and catheter with CF technology compared to manual ablation (64 vs. 36 %, p 0.01) [24]. It is conceivable that real-time visualization of CF during RF applications reduces PV reconnection by creating durable lesions, leading to fewer repeat procedures and improved success rates, without compromising the safety profile or prolonging the procedure time.
An additional finding of this study is the increase in procedure time associated with using the RNS. The increased procedure time is due to RNS setup and manipulation before the first RF delivery. Indeed, RF time is similar in the two groups. Cumulative time, from first to last ablation, although not statistically significant, is longer in the manual group. This could be explained because the operators tried to achieve the best possible CF value in the manual group avoiding RF delivery in case of unsatisfactory CF (<7 g). Despite longer procedural time, RNS is not associated to an increased complication rate. Moreover, the reduction in fluoroscopy time found in our population using the RNS plays an important role in reducing the risk of malignancy due to radiation exposure [25, 26].
4.1 Limitations
This study has several limitations. Firstly, due to the design of the study, the operators are not blinded to the ablation technique and this could have impact the study findings. In this study, the operators did not use deflectable sheaths for manual navigation, which may have affected the CF in the manual group. We also recognize that follow-up performed with ECG and Holter monitoring could underestimate asymptomatic arrhythmia episodes. Finally, we did not perform a cost-effective analysis of RNS for AF procedures, but the use of RNS can be justified by the significant reduction in fluoroscopy time and the lower AF recurrence rate.
5 Conclusions
The use of ThermoCool SmartTouch ablation catheter with the RNS is associated with increased contact between the ablation catheter and myocardial tissue and to a lower AF recurrence rate at medium clinical follow-up. Further studies with longer follow-up are needed to assess the long-term efficacy.
References
Camm, A. J., Lip, G. Y., De Caterina, R., Savelieva, I., Atar, D., Hohnloser, S. H., et al. (2012). ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. European Heart Journal, 33, 2719–2747.
Calkins, H., Kuck, K. H., Cappato, R., Brugada, J., Camm, A. J., Chen, S. A., et al. (2012). 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Heart Rhythm, 9, 632–696.
Di Biase, L., Paoletti Perini, A., Mohanty, P., Goldenberg, A. S., Grifoni, G., Santangeli, P., et al. (2014). Visual, Tactile and Contact Force Feedback: which one is more important for catheter ablation? Results from an in vitro experimental study. Heart Rhythm, 11(3), 506–513.
Kumar, S., Chan, M., Lee, J., Wong, M. C., Yudi, M., Morton, J. B., et al. (2014). Catheter-tissue contact force determines atrial electrogram characteristics before and lesion efficacy after antral pulmonary vein isolation in humans. Journal of Cardiovascular Electrophysiology, 25(2), 122–129.
Olson, M. D., Phreaner, N., Schuller, J. L., Nguyen, D. T., Katz, D. F., Aleong, R. G., et al. (2013). Effect of catheter movement and contact during application of radiofrequency energy on ablation lesion characteristics. Journal of Interventional Cardiac Electrophysiology, 38(2), 123–129.
Haldar, S., Jarman, J. W., Panikker, S., Jones, D. G., Salukhe, T., Gupta, D., et al. (2013). Contact force sensing technology identifies sites of inadequate contact and reduces acute pulmonary vein reconnection: a prospective case control study. International Journal of Cardiology, 168, 1160–1166.
Martinek, M., Lemes, C., Sigmund, E., Derndorfer, M., Aichinger, J., Winter, S., et al. (2012). Clinical impact of an open-irrigated radiofrequency catheter with direct force measurement on atrial fibrillation ablation. Pacing and Clinical Electrophysiology, 35, 1312–1318.
Okumura, Y., Johnson, S. B., Bunch, T. J., Henz, B. D., O’Brien, C. J., & Packer, D. L. (2008). A systematical analysis of in vivo contact forces on virtual catheter tip/tissue surface contact during cardiac mapping and intervention. Journal of Cardiovascular Electrophysiology, 19, 632–640.
Bai, R., DI Biase, L., Valderrabano, M., Lorgat, F., Micochova, H., Tilz, R., et al. (2012). Worldwide experience with the robotic navigation system in catheter ablation of atrial fibrillation: methodology, efficacy and safety. Journal of Cardiovascular Electrophysiology, 23, 820–826.
Duncan, E. R., Finlay, M., Page, S. P., Hunter, R., Goromonzi, F., Richmond, L., et al. (2012). Improved electrogram attenuation during ablation of paroxysmal atrial fibrillation with the Hansen robotic system. Pacing and Clinical Electrophysiology, 35(6), 730–738.
Lorgat, F., Pudney, E., van Deventer, H., & Chitsaz, S. (2012). Robotically controlled ablation for atrial fibrillation: the first real-world experience in Africa with the Hansen robotic system. Cardiovascular Journal of Africa, 23(5), 274–280.
Willems, S., Steven, D., Servatius, H., Hoffmann, B. A., Drewitz, I., Müllerleile, K., et al. (2010). Persistence of pulmonary vein isolation after robotic remote-navigated ablation for atrial fibrillation and its relation to clinical outcome. Journal of Cardiovascular Electrophysiology, 21, 1079–1084.
Di Biase, L., Wang, Y., Horton, R., Gallinghouse, G. J., Mohanty, P., Sanchez, J., et al. (2009). Ablation of atrial fibrillation utilizing robotic catheter navigation in comparison to manual navigation and ablation: single-center experience. Journal of Cardiovascular Electrophysiology, 20, 1328–1335.
Wazni, O. M., Barrett, C., Martin, D. O., Shaheen, N., Tarakji, K., Baranowski, B., et al. (2009). Experience with the hansen robotic system for atrial fibrillation ablation-lessons learned and techniques modified: Hansen in the real world. Journal of Cardiovascular Electrophysiology, 20(11), 1193–1196.
Di Biase, L., Natale, A., Barrett, C., Tan, C., Elayi, C. S., Ching, C. K., et al. (2009). Relationship between catheter forces, lesion characteristics, “popping”, and char formation: experience with Robotic Navigation System. Journal of Cardiovascular Electrophysiology, 20, 436–440.
Society, B. H. R. (2014). Standard for Interventional Electrophysiology Study and Catheter Ablation in Adults.
Kuck, K. H., Reddy, V. Y., Schmidt, B., Natale, A., Neuzil, P., Saoudi, N., et al. (2012). A novel radiofrequency ablation catheter using contact force sensing: Toccata study. Heart Rhythm, 9(1), 18–23.
Reddy, V. Y., Shah, D. C., Kautzenr, J., Schmidt, B., Saoudi, N., Herrera, C., et al. (2012). The relationship between contact force and clinical outcome during radiofrequency catheter ablation of atrial fibrillation in the TOCCATA study. Heart Rhythm, 9(11), 1789–1795.
Mizuno, H., Vergara, P., Maccabelli, G., Trevisi, N., Eng, S. C., Brombin, C., et al. (2013). Contact force monitoring for cardiac mapping in patients with ventricular tachycardia. Journal of Cardiovascular Electrophysiology, 24, 519–524.
Dello Russo, A., Fassini, G., Casella, M., Bologna, F., Al-Nono, O., Colombo, D., et al. (2014). Simultaneous assessment of contact pressure and local electrical coupling index using robotic navigation. Journal of Interventional Cardiac Electrophysiology, 40, 23–31.
Nakagawa, H., Kautzner, J., Natale, A., Peichl, P., Cihak, R., Wichterle, D., et al. (2013). Locations of high contact force during left atrial mapping in atrial fibrillation patients: electrogram amplitude and impedance are poor predictors of electrode-tissue contact force for ablation of atrial fibrillation. Circulation. Arrhythmia and Electrophysiology, 6(4), 746–753.
Steven, D., Servatius, H., Rostock, T., Hoffman, B., Drewitz, I., Mullerleile, K., et al. (2010). Reduced fluoroscopy during atrial fibrillation ablation: benefits of robotic guided navigation. Journal of Cardiovascular Electrophysiology, 21, 6–12.
Ullah, W., McLean, A., Hunter, R. J., Baker, V., Richmond, L., Cantor, E. J., et al. (2014). Randomized trial comparing robotic to manual ablation for atrial fibrillation. Heart Rhythm, 11, 1862–1869.
Ullah, W., Hunter, R. J., Haldar, S., McLean, A., Dhinoja, M., Sporton, S., et al. (2014). Comparison of robotic and manual persistent AF ablation using catheter contact force sensing: an international multicenter registry study. PACE, 37, 1427–1435.
Casella, M., Pelargonio, G., Dello Russo, A., Riva, S., Bartoletti, S., Santangeli, P., et al. (2011). "Near-zero" fluoroscopic exposure in supraventricular arrhythmia ablation using the EnSite NavX™ mapping system: personal experience and review of the literature. Journal of Interventional Cardiac Electrophysiology, 31, 109–118.
Ait-Ali, L., Andreassi, M. G., Foffa, I., Spadoni, I., Vano, E., & Picano, E. (2010). Cumulative patient effective dose and acute radiation-induced chromosomal DNA damage in children with congenital heart disease. Heart, 96, 269–274.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dello Russo, A., Fassini, G., Conti, S. et al. Analysis of catheter contact force during atrial fibrillation ablation using the robotic navigation system: results from a randomized study. J Interv Card Electrophysiol 46, 97–103 (2016). https://doi.org/10.1007/s10840-016-0102-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-016-0102-0