Abstract
Background
Pre- and postablation atrial fibrillation (AF) brain natriuretic peptide (BNP) levels were shown to predict increased recurrence of AF following ablation.
Objective
Our objective was to assess whether elevated BNP levels merely represent the presence of AF at the time of measurement or indeed the true recurrence of AF.
Methods and Results
In a prospective study of 88 patients undergoing AF ablation, BNP levels were measured immediately before, after, 24 h, and 4–6 months postablation. BNP levels were stratified by presenting rhythm and ventricular rate at the time of measurement. Median BNP level preablation was higher in patients presenting in AF compared to sinus rhythm (SR) (54(44–79) pg/ml vs. 30(18–47) pg/ml, p < 0.001). Postablation restoration of SR in patients presenting in AF reduced median BNP levels from 54(44–79) pg/ml to 40(37–51) pg/ml, (p < 0.001). However, no change was noted in patients who presented in and maintained SR throughout the procedure (30(18–47) pg/ml to 27(16–40) pg/ml, p = 0.270). At 4–6 months, BNP measured in patients in SR was not significantly different from postablation BNP (35(22–53) pg/ml vs. 38(20–52) pg/ml, p = 0.656), although 35 % of them had AF recurrence in 1-year follow-up. Median BNP level measured in five patients while in atrial arrhythmia was elevated compared to postablation BNP (464(421–464) pg/ml to 37(36–37) pg/ml, p = 0.043). BNP levels and ventricular rates are positively correlated at all times pre- and postablation.
Conclusions
BNP level rises acutely during AF and with rapid ventricular rates. BNP level seems to be a function of atrial rhythm and ventricular rate rather than short- or long-term predictor of AF ablation success.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Brain natriuretic peptide (BNP) is a neurohumoral substance produced by the ventricles in response to myocardial stretch and is a diagnostic marker of heart failure and systemic fluid overload [1]. Plasma BNP levels are known to be significantly elevated in patients with atrial fibrillation (AF) compared to those in sinus rhythm (SR) even in those without heart failure [2, 3]. These levels have been shown to drop acutely following cardioversion of AF to SR [4–6]. Pulmonary vein antral isolation (PVAI) is an effective and standard rhythm control strategy in patients with symptomatic and drug refractory AF [7, 8]. BNP levels have also been shown to decrease after successful AF ablation by pulmonary vein isolation. Few studies have suggested that reduced BNP levels 3-months postablation are predictor of successful ablation in paroxysmal, persistent, and permanent AF patients [9–12]. Few others have also suggested that preablation BNP levels correlate with increased recurrence of AF postablation [13–16].
BNP has a short biological half life of 22 min and is metabolized rapidly by an endopeptidase [17, 18]. Given its short half life, BNP levels may reflect acute changes in rhythm status and may predict meaningful hemodynamic and neurohumoral changes within 1 to 2 h of an atrial arrhythmic event. Whether BNP levels can truly predict the success of a procedure as indicated in some prior studies is questionable.
In our study, we aimed to answer this question by sequentially measuring BNP levels pre- and postablation procedure while monitoring rhythm and ventricular rate. We compared BNP levels immediately prior to, after ablation, 24 h post, and at 4 to 6-months follow-up in patients who presented for AF ablation.
2 Methods
This is a prospective observational study that enrolled patients with AF undergoing PVAI and substrate modification. The study was approved by the human subjects committee at the respective two institutions and conducted in accordance with their regulations, and an informed consent was obtained from all the participants.
Study population
Consecutive patients (n = 88) with symptomatic and drug-resistant AF undergoing ablation for the first time were enrolled after fulfilling the inclusion and exclusion criteria. Patients with renal insufficiency (serum creatinine of 1.4 or greater), left ventricular ejection fraction less than 45 %, prior myocardial infarction, congestive heart failure, rheumatic heart disease, moderate to severe valvular dysfunction, moderate to severe diastolic dysfunction, severe uncontrolled hypertension, severe left ventricular hypertrophy, and hyperthyroidism were excluded.
Pulmonary vein antral isolation
Pulmonary vein antral isolation (PVAI) was performed using intracardiac echo and 3D electroanatomic mapping (CARTO or NavX) guided, roving circular mapping catheter (Lasso®, Biosense Webster Inc., Diamond Bar, CA) technique involving isolation of all the pulmonary veins at the antral level using an open-irrigated ablation catheter (Thermocool®, Biosense Webster Inc., Diamond Bar, CA) with double transseptal puncture.
Details of the procedure are described elsewhere [19]. The ablation was done either in SR or in AF. Patients with paroxysmal AF had pulmonary vein isolation alone, and those with early persistent and prolonged persistent had additional complex fractionated electrogram ablation along the posterior wall, septum, roof, and coronary sinus. If the patients did not convert to SR at the end of the ablation, they were electively cardioverted to SR. In patients where the AF organized into an atrial flutter, it was mapped and ablated. All the patients received 40 mg of IV furosemide immediately after the procedure and 12 h post procedure. Potassium and magnesium levels were replaced appropriately.
BNP sampling
Peripheral venous samples were used for measuring BNP. A sample of 2–3 ml of blood was collected in EDTA-coated 5-ml test tubes. A total of four blood samples were obtained sequentially. The first sample was obtained immediately prior to ablation on the procedure table. The second sample was obtained immediately after the ablation within 10 min of the end of the procedure. The third sample was obtained on the first postoperative day. A final sample was collected between 4 and 6 months postablation.
BNP assay
BNP is stable in whole blood. A portable, 15-min immunoassay provided by Biosite (Triage BNP Test, Biosite Diagnostics) [20] was used to measure BNP in the whole blood samples. Blood was assayed as soon as the sample was received, and the rapid in vitro quantitative measurement of BNP was obtained within 15 min. Monthly quality controls were performed and the instrument was calibrated as per the specifications. The lowest limit of detection in this immunoassay was 5 pg/ml.
Follow-up and procedural success
A final BNP sample was obtained at 4–6 months follow-up visit. Clinical information about patient status and symptomatic AF episodes were obtained from the clinic notes. Success or failure of the AF ablation procedure and episodes of recurrent AF and atrial flutter (AFL) were ascertained from the follow-up clinic notes. The first 12 weeks postablation was considered as the blanking period. Patients free of atrial arrhythmias at 3 months follow-up off antiarrhythmic drugs (AAD) were considered to have successful ablation in the short term. Recurrence of AF beyond 3 months was considered a failed ablation procedure [21]. Patients were followed further up to 1 year to assess the long-term success.
Rhythm monitoring
All enrolled patients had a diagnosis of either paroxysmal, early persistent, or longstanding persistent AF refractory to drug therapy. Patients’ presenting rhythm prior to ablation was obtained from the EKG and telemetry monitor and review of the ablation procedure notes. Rhythm of the patient during the procedure was also reviewed, and any induction and occurrence of AF during the procedure was noted. Rhythm on the first postoperative day was noted from hospital telemetry and 12-lead EKGs. All patients were equipped with an event monitor for 3 months, and recurrence of AF episodes was assessed effectively during that period. Patients’ rhythm at follow-up visits (at 6 and 12 months or any urgent care visits) was assessed using a 12-lead EKG at the time of the visit. A repeat event monitor was given if patients complained of symptoms of AF that was not recorded on a routine EKG. BNP measurement at 4–6 months postablation was done along with the EKG. Heart rate during each BNP measurement was also noted either from the EKG, tele-monitor, or clinic visit encounter. Specifically, the heart rate was observed on the monitor in the EP lab during the BNP draw preablation and postablation, and the highest heart rate was documented. On the first postoperative day, the highest heart rate during the BNP draw was obtained from the tele-monitor. Heart rate at 4–6 month was obtained from the EKG done immediately prior to BNP draw. For patients in AF, rate controlled AF was defined arbitrarily as ventricular rate <100 bpm at rest. AF with rapid ventricular response is ventricular rate >100 bpm.
Statistical analysis
The demographic and clinical characteristics of the patient population were described by percentages, and means and standard deviations as appropriate. Statistical analysis of categorical data was done using the chi-square statistic. BNP measurements were not normally distributed. For paired comparisons of BNP measurements, the nonparametric Wilcoxon signed rank test was used, and for independent comparisons of BNP measurements, the nonparametric Mann–Whitney U test was used. Correlations between BNP levels and heart rates were made using Pearson correlation. A general linear model was used to evaluate the relative importance of atrial rhythm and ventricular rate on the elevation of BNP. A p value <0.05 was considered statistically significant. Univariate and multivariate stepwise logistic regression analysis of AF recurrence was also performed. The SPSS 16.0 statistical package was used for statistical analyses.
3 Results
3.1 Baseline characteristics
A total of 88 patients were enrolled between June 2008 and December 2009 (mean age of 60 ± 8 years, 68 % men). Please see Table 1 for baseline characteristics. A large percentage of patients had early persistent AF at 63.6 %, followed by paroxysmal AF at 33.0 %, and longstanding persistent AF at 3.4 %. Mean ejection fraction of the study population was 56.6 ± 8.3 %.
3.2 BNP levels and rhythm/rate before and immediately after AF ablation
Forty (45.4 %) patients were in AF at the beginning of the procedure and were either cardioverted (69 %) or spontaneously converted to sinus rhythm (31 %) by the end of the procedure. Thirteen (14.8 %) patients were in SR at the beginning of the procedure but developed AF during the procedure and were also either spontaneously converted or cardioverted to SR at the end of the procedure. Thirty-five (39.8 %) patients presented in and maintained SR throughout the procedure. Median BNP level preablation was higher in patients who presented in rate controlled AF compared to patients in SR (54(Q1 44–Q3 79) pg/ml vs. 30(Q1 18–Q3 47) pg/ml, p < 0.001). Following the restoration of SR with ablation (with or without cardioversion), median BNP levels dropped significantly immediately after the procedure to 40 pg/ml in the group that presented in AF (54(44–79) pg/ml to 40(37–51) pg/ml, p < 0.001). Median postablation BNP levels did not change compared to preablation BNP levels in those patients who presented in SR (30(18–47) pg/ml to 27(16–40) pg/ml, p = 0.270). Median BNP postablation in those who presented in AF was different from those in SR (40(37–51) pg/ml and 27(16–40) pg/ml, p = 0.001). Mean procedure time was 3.5 ± 0.7 h. Figure 1 shows the BNP levels at different time points in patients presenting in AF versus SR.
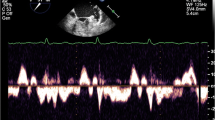
Mean ventricular rate in patients presenting with rate-controlled AF was higher than those in SR (73.4 ± 15.1 vs. 59.9 ± 12.5 bpm, p < 0.001). There was a significant positive correlation of BNP and ventricular rate preablation (Pearson correlation coefficient = 0.645, p < 0.001) (Fig. 2a). A significant positive correlation was also seen between postablation BNP levels and ventricular rate (Pearson correlation = 0.599, p < 0.001) regardless of the rhythm (see Fig. 2b).
a–d Shows the Pearson’s correlation between BNP levels and the rhythm (AF, red and SR black) at the time of measurement and ventricular rate immediately before, after, 24 h, and 4–6 months post-RF ablation. a Shows correlation of heart rate with preablation BNP levels in those presenting in SR versus AF. b Shows correlation of heart rate and BNP levels immediately after ablation. All the patients were in SR at the end of the procedure. c Shows the correlation of heart rate and BNP levels at 24-h postablation in those who were in SR versus AF at that time. d Correlation between ventricular rates and BNP levels at 4–6-months follow-up in those who were in SR versus AF
3.3 BNP levels and rhythm/rate 24-h postablation
Median BNP on the first postoperative day (24 h postablation) was 75(51–123) pg/dl and was significantly higher than the immediate postablation BNP (37(23–50) pg/dl) in all individuals (p < 0.001). This is probably either related to fluid overload from the ablation using an open-irrigated catheter or atrial tissue necrosis. Twenty-four hours postablation, 83 (94.3 %) patients were in SR. In these patients, there was no significant difference in BNP among those who presented in SR versus those who presented in AF (73 (55–115) vs. 64 (46–139), p = 0.974). The median BNP in patients in AF (n = 5) at 24 h was 207 pg/dl. Median BNP in these patients who were in AF 24-h post procedure was higher than those who were in SR (207 (194–207) vs. 71 (50–121), p = 0.001). Mean ventricular rate in these five patients in AF was significantly higher than those in SR (93.2 ± 14.6 vs. 75.3 ± 12.0, p = 0.022). There was a significant strong positive correlation between ventricular rate and BNP levels (Pearson correlation = 0.674, p < 0.001; see Fig. 2c).
3.4 BNP levels and rhythm/rate 4–6 months postablation
BNP levels were measured in 64 patients 4 to 6 months after ablation and were compared to BNP immediately postablation. All but five patients were in SR at the time of this measurement. It was found that BNP levels at 4 to 6 months in patients in SR were not significantly different from postablation BNP (35(22–53) pg/ml vs. 38(20–52) pg/ml, p = 0.656), although 21 (21/59, 35.5 %) of them had AF recurrence. Median BNP levels of the five patients who were in AF/AFL at the time of the 4- to 6-month postablation measurement were elevated compared to postablation BNP (464(421–464) pg/ml to 37(36–37) pg/ml, p = 0.043). Similarly, median BNP level of these five patients at 4–6 months was significantly higher than the BNP level at 4–6 months measured in patients who were in SR at the time of measurement (464(421–464) pg/ml to 35(22–53) pg/ml, p = 0.005). Of the 5 patients who were in AF/AFL at the time of measurement of BNP, 4 of them had rapid ventricular rates ranging from 188 to 220 and much higher BNP values ranging from 421 to 990.3. One patient who was in rate-controlled AF had a heart rate of 56 bpm and a BNP level of 26.1 pg/ml. All of these patients have stopped their AADs and titrated down on their AV nodal blockers at the time of the recurrence. There is a strong positive correlation between ventricular rate and BNP levels at 4–6 months postablation (Pearson correlation = 0.910, p < 0.001; see Fig. 2d).
3.5 BNP levels and AF recurrence 1-year follow-up
Twenty-six out of 88 patients (29.5 %) had AF recurrence at 1-year follow-up. When patients with and without AF recurrence were compared, there was no difference in BNP levels at all time points pre- and postablation. Taken otherwise, BNP levels pre- or postablation did not predict AF recurrence; see Fig. 3. Furthermore, when BNP levels were measured only when patients were in SR, BNP levels were reduced in both AF recurrence and nonrecurrence cohorts, again with no statistically significant difference in both groups at preablation, immediate postablation, and at 4–6 months (Table 2a). Similarly, when we analyzed patients with paroxysmal and persistent AF separately, there was no difference in BNP levels at any stage pre- or postablation in patients with and without a recurrence. Only at 24-h postablation did recurrent cohorts have higher BNP than nonrecurrence cohort when all patients were considered (Table 2a). At 12-months follow-up, 78 % remained arrhythmia free off antiarrhythmic drugs. None of them underwent redo ablation within 1 year. No BNP levels were measured at 12-months follow-up.
Univariate predictors for AF recurrence were found to be age (p = 0.1), preablation BNP (p = 0.14), immediate postablation BNP (p = 0.06), OSA (p = 0.09), and ACEI/ARB (p = 0.02). On multivariate analysis, OSA (p = 0.01) and presence of an ACEI/ARB inhibitor (p = 0.008) were found to be predictors of AF recurrence. BNP levels were not found to correlate with recurrence.
3.6 Elevated BNP levels as a function of atrial rhythm versus ventricular rate
BNP levels measured at any time pre- and postablation are significantly higher if patients are in AF at the time of measurement than if they are in SR (see Fig. 4). Similarly, BNP levels at all times (pre- and postablation) were positively correlated with ventricular rates (see Fig. 2–d). Since BNP levels have been shown to be elevated with atrial fibrillation as well as with an increase in heart rate in our study, we sought to determine if the elevated BNP is secondary to the atrial rhythm or the ventricular rate or both. Figure 5 shows the increase in BNP levels as the ventricular rate increases in both SR and AF. A general linear model showed that ventricular rate accounted for most of the variability (p < 0.001) in the model suggesting that it is the ventricular rate rather than the atrial rhythm that has contributed mostly to the increase in BNP level.
4 Discussion
Main study findings
Our study confirms the following: (1) BNP levels are elevated during AF and normalizes when SR is restored. (2) BNP levels are much higher in AF patients with rapid ventricular rates than those with rate-controlled AF, and BNP levels continue have a linear correlation to ventricular rates. (3) Higher ventricular rates in SR predicted higher BNP levels than lower ventricular rates. (4) BNP levels seem to correlate with the atrial rhythm and ventricular rate for a given point in time and are not predictive of either short-term or long-term success of AF ablation as was shown in earlier studies.
BNP is a 30 amino acid cardiac neurohormone peptide. Lungs, kidneys, and adrenal glands are known to produce this peptide, with the ventricles being the primary source of BNP in patients with heart failure. [22–24]. Even though ventricles are the predominant source of BNP, atria have also been shown to secrete BNP in patients with AF [25]. The exact mechanism of its production in the atria is unclear, although BNP mRNA has been detected in atrial myocytes. Increased atrial stretch has been proposed for the elevated levels in patients with AF [18, 25, 26]. BNP elevation during AF is probably related to significant atrial stretch and volume overload which becomes even more profound when AF is associated with rapid ventricular rates. Altered myocardial contractility and hemodynamics from rapid rates probably causes ventricles to secrete quantitatively much higher levels of BNP. Such correlation between rapid ventricular rates and high BNP levels was shown by Magioncalda et al. in patients presenting to the emergency rooms with supraventricular tachyarrhythmias [27].
BNP levels on postoperative day 1 have been found to be significantly higher in all individuals in our study irrespective of presenting rhythm. This observation may be related to significant fluid and pressure overload caused by open-irrigated catheter use for ablation or by the direct traumatic effects on the atrial tissue producing ablation necrosis [28]. A study by our group in the past has shown that open-irrigated catheter use for AF ablation can cause significant fluid overload (up to 4 l) and associated symptoms [29].
Prior studies have shown elevated levels of BNP in subjects with AF [30–32]. Preoperative levels of BNP have been shown to predict the occurrence of postoperative AF [33] while others have shown that preablation BNP levels predict post-AF recurrence postablation [13–16]. Some studies have shown that reduction in BNP levels 3 months after AF ablation is predictive of procedural success [9–12]. It is possible that someone who presents in AF or other atrial tachyarrhythmia 3-months postablation is likely to have an elevated BNP level. It was not clear in most of these studies what the rhythm was when BNP levels were measured or what their ventricular rates were at the time of measurement. It is possible that those who were classified as failed ablation were in AF recurrence with high BNP levels and those who had successful ablation were in sinus with low BNP levels. Thus the difference in BNP levels would simply reflect their rhythm and ventricular rate at the time the sample was obtained. The conclusions of the above-referenced studies probably do not apply to patients who are in SR at the time of BNP measurement but later had recurrent AF. Other studies have demonstrated preablation BNP and/ or N-terminal pro-BNP levels to predict postablation recurrence of AF [13–16]. This was not reproduced in our study. In our study, BNP levels at 24 h were elevated in those with AF recurrence (albeit no difference was detected when considered separately for paroxysmal and persistent AF patients likely due to a smaller power). It is possible that most of the patients who had AF recurrence were those who presented in AF with a more complex arrhythmia substrate requiring extensive ablation and infusion of more fluid thus causing an elevated BNP 24-h post procedure. Our study is important because it challenges the conclusions from other studies that pre- or postablation BNP levels cannot predict AF recurrence. We believe that elevated BNP levels are marker of the nature of the atrial substrate, presenting atrial rhythm, atrial arrhythmia burden, and ventricular rate and not a conclusive predictor of short-term or long-term procedural success.
Limitations and clinical implications
This is a small study with limited study population. We did not measure source-specific BNP to see if the elevated BNP in AF patients was mostly from atria or ventricles. However, it was obvious that there was linear correlation between ventricular rates and BNP levels both in patients with SR and AF, suggesting that quantitatively ventricles to be the bigger contributing source than the atria. When the ventricular rates are well-controlled, patients in AF had relatively higher BNP levels than those in SR. Again, the highest heart rate at the time of BNP draw was documented, and heart rate was not averaged over a period of time. Occurrence of AF postablation was monitored by event monitor reports, but if a patient had asymptomatic AF episodes not captured by the event recorder, we could have missed those AF recurrences. Our study suggests the nonutility of measuring BNP to predict AF recurrence after ablation. Clinicians should rely on clinical evidence of recurrence including symptoms and documented arrhythmia rather than a short-lived biological marker when making important decisions regarding discontinuation of antiarrhythmic drugs and anticoagulation postablation. Multiple comorbidities can affect BNP levels; rigorous effort was made to exclude the most obvious confounders. These limitations probably apply to most studies published on this subject.
5 Conclusions
BNP level rises acutely during AF and with rapid ventricular rates. BNP level seems to be a function of atrial rhythm and ventricular rate rather than short- or long-term predictor of AF ablation success.
Abbreviations
- BNP:
-
Brain natriuretic peptide
- AF:
-
Atrial fibrillation
- SR:
-
Sinus rhythm
- PVAI:
-
Pulmonary vein antral isolation
- AFL:
-
Atrial flutter
- AAD:
-
Antiarrhythmic drugs
- OSA:
-
Obstructive sleep apnea
- ACEI/ARB:
-
Angiotensin converting enzyme inhibitor/angiotensin receptor blocker
References
Levin, E. R., Gardner, D. G., & Samson, W. K. (1998). Natriuretic peptides. New England Journal of Medicine, 339, 321–328.
Silvet, H., Young-Xu, Y., Walleigh, D., & Ravid, S. (2003). Brain natriuretic peptide is elevated in outpatients with atrial fibrillation. American Journal of Cardiology, 92, 1124–1127.
Tsuchida, K., & Tanabe, K. (2004). Influence of paroxysmal atrial fibrillation attack on brain natriuretic peptide secretion. Journal of Cardiology, 44, 1–11.
Beck-da-Silva, L., de Bold, A., Fraser, M., Williams, K., & Haddad, H. (2004). Brain natriuretic peptide predicts successful cardioversion in patients with atrial fibrillation and maintenance of sinus rhythm. Canadian Journal of Cardiology, 20, 1245–1248.
Vinch, C. S., Rashkin, J., Logsetty, G., Tighe, D. A., Hill, J. C., Meyer, T. E., et al. (2004). Brain natriuretic peptide levels fall rapidly after cardioversion of atrial fibrillation to sinus rhythm. Cardiology, 102, 188–193.
Ohta, Y., Shimada, T., Yoshitomi, H., Inoue, S., Murakami, Y., Shimizu, H., et al. (2001). Drop in plasma brain natriuretic peptide levels after successful direct current cardioversion in chronic atrial fibrillation. Canadian Journal of Cardiology, 17, 415–420.
Haissaguerre, M., Jais, P., Shah, D. C., et al. (1998). Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. New England Journal of Medicine, 339, 659–666.
Jais, P., Sanders, P., Hsu, L. F., Hosini, M., & Haissaguerre, M. (2005). Catheter ablation for atrial fibrillation. Heart, 91, 7–9.
Kurosaki, K., Tada, H., Hashimoto, T., Ito, S., Miyaji, K., Naito, S., et al. (2007). Plasma natriuretic peptide concentrations as a predictor for successful catheter ablation in patients with drug-refractory atrial fibrillation. Circulation Journal, 71, 313–320.
Date, T., Yamane, T., Inada, K., Matsuo, S., Miyanaga, S., Sugimoto, K., et al. (2006). Plasma brain natriuretic peptide concentrations in patients undergoing pulmonary vein isolation. Heart, 92, 1623–1627.
Yamada, T., Murakami, Y., Okada, T., Yoshida, N., Toyama, J., Yoshida, Y., et al. (2007). Plasma brain natriuretic peptide level after radiofrequency catheter ablation of paroxysmal, persistent, and permanent atrial fibrillation. Europace, 9(9), 770–774.
Yamada, T., Murakami, Y., Okada, T., Yoshida, N., Toyama, J., Yoshida, Y., et al. (2008 Mar). Plasma brain natriuretic peptide level after hybrid therapy with pulmonary vein isolation and antiarrhythmic drugs for atrial fibrillation. International Heart Journal, 49(2), 143–151.
Hussein, A. A., Saliba, W. I., Martin, D. O., Shadman, M., Kanj, M., Bhargava, M., et al. (2011). Plasma B-type natriuretic peptide levels and recurrent arrhythmia after successful ablation of lone atrial fibrillation. Circulation, 123(19), 2077–2082.
Shin, D. I., Deneke, T., Gorr, E., Anders, H., Buenz, K., Paesler, M., et al. (2009). Predicting successful pulmonary vein isolation in patients with atrial fibrillation by brain natriuretic peptide plasma levels. Indian Pacing Electrophysiology Journal, 9, 241–246.
Hwang, H. J., Son, J. W., Nam, B. H., Joung, B., Lee, B., Kim, J. B., et al. (2009). Incremental predictive value of pre-procedural N-terminal pro-B-type natriuretic peptide for short-term recurrence in atrial fibrillation ablation. Clinical Research in Cardiology, 98, 213–218.
Mohanty, S., Mohanty, P., Di Biase, L., Rong, B., Burkhardt, D., Gallinghouse, J. G., et al. (2011). Baseline B-type natriuretic peptide: a gender-specific predictor of procedure-outcome in atrial fibrillation patients undergoing catheter ablation. Journal of Cardiovascular Electrophysiology, 22(8), 858–865.
McKie, P. M., & Burnett, J. C., Jr. (2005). B-type natriuretic peptide as a biomarker beyond heart failure: speculations and opportunities. Mayo Clinic Proceedings, 80, 1029–1036.
Redfield, M. M., Rodeheffer, R. J., Jacobsen, S. J., Mahoney, D. W., Bailey, K. R., & Burnett, J. C., Jr. (2002). Plasma brain natriuretic peptide concentration: impact of age and gender. Journal of the American College of Cardiology, 40, 976–982.
Callahan, T. D., 4th, Di Biase, L., Horton, R., Sanchez, J., Gallinghouse, J. G., & Natale, A. (2009). Catheter ablation of atrial fibrillation. Cardiology Clinics, 27, 163–178.
http://www.biosite.com/products/bnp.aspx. last accessed 4/3/10
Oral, H., Knight, B. P., Ozaydin, M., Tada, H., Chugh, A., Hassan, S., et al. (2002). Clinical significance of early recurrences of atrial fibrillation after pulmonary vein isolation. Journal of the American College of Cardiology, 40, 100–104.
Gerbes, A. L., Dagnino, L., Nguyen, T., & Nemer, M. (1994). Transcription of brain natriuretic peptide and atrial natriuretic peptide genes in human tissues. Journal of Clinical Endocrinology and Metabolism, 78, 1307–1311.
Wasywich, C. A., Webster, M. W., Richards, A. M., & Stewart, R. A. (2006). Coronary sinus and ascending aortic levels of aldosterone, angiotensin II, and B-type natriuretic peptide in patients with aortic stenosis and in patients with coronary heart disease. American Journal of Cardiology, 97, 1068–1072.
Mukoyama, M., Nakao, K., Saito, Y., Ogawa, Y., Hosoda, K., Suga, S., et al. (1990). Human brain natriuretic peptide, a novel cardiac hormone. Lancet, 335, 801–802.
Inoue, S., Murakami, Y., Sano, K., Katoh, H., & Shimada, T. (2000). Atrium as a source of brain natriuretic polypeptide in patients with atrial fibrillation. Journal of Cardiac Failure, 6, 92–96.
Qi, W. F., Kjekshus, H. F., Klinge, R. F., kjekshus, J. K., & Hall, C. (2000). Cardiac natriuretic peptides and continuously monitored atrial pressures during chronic rapid pacing in pigs. Acta Physiologica Scandinavica, 169, 95–102.
Magioncalda, A., Sartini, M., Costaguta, C., Castellaneta, M., Schenone, E., Tognoni, E., et al. (2008). The utility of assaying the N-terminal of brain natriuretic peptide precursor (NT pro-BNP) to predict the clinical outcome in patients with supraventricular tachyarrhythmias observed and treated in the emergency room. Recenti Progressi in Medicina, 99, 141–145.
Chen, L., Wei, T., Zeng, C., Chen, Q., Shi, Z., & Wang, L. (2005). Effect of radiofrequency catheter ablation on plasma B-type natriuretic peptide. Pacing and Clinical Electrophysiology, 28(3), 200–204.
Vanga, S., Pillarisetti, J., Biria, M., Rajoli, S., Pimentel, R., Lakkireddy, D. (2010). Overcoming Fluid Overload After Atrial Fibrillation Ablation with an Open Irrigated Catheter: Role of Scheduled Diuresis and Electrolyte Replacement. Heart Rhythm Supplement 7:pO-06 58. (Abs)
Li, J., & Wang, L. (2006). B-type natriuretic peptide levels in patients with paroxysmal lone atrial fibrillation. Heart and Vessels, 21, 137–140.
Kim, B. J., Hwang, S. J., Sung, K. C., et al. (2007). Assessment of factors affecting plasma BNP levels in patients with chronic atrial fibrillation and preserved left ventricular systolic function. International Journal of Cardiology, 118, 145–150.
Yamada, T., Murakami, Y., Okada, T., Kim, B. S., Kang, J. H., Lee, M. H., et al. (2006). Plasma atrial natriuretic peptide and brain natriuretic peptide levels after radiofrequency catheter ablation of atrial fibrillation. American Journal of Cardiology, 97, 1741–1744.
Wazni, O. M., Martin, D. O., Marrouche, N. F., Okamoto, M., Shimizu, T., Toyama, J., et al. (2004). Plasma B-type natriuretic peptide levels predict postoperative atrial fibrillation in patients undergoing cardiac surgery. Circulation, 110, 124–127.
Conflict of interests
No specific conflict of interests related to the study for any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pillarisetti, J., Reddy, N., Biria, M. et al. Elevated brain natriuretic peptide level in patients undergoing atrial fibrillation ablation: is it a predictor of failed ablation or a mere function of atrial rhythm and rate at a point in time?. J Interv Card Electrophysiol 40, 161–168 (2014). https://doi.org/10.1007/s10840-014-9898-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-014-9898-7