Abstract
Purpose
Magnetic resonance imaging (MRI) in patients with Cardiovascular Implantable Electronic Devices (CIED) has not been approved by the Food and Drug Administration. Recent data suggests MRI as a relative rather than absolute contraindication in CIED patients. Recently, the American Heart Association has recommended defibrillation threshold testing (DFTT) in implantable cardioverter defibrillator (ICD) patients undergoing MRI. We evaluated the feasibility and safety of a protocol for MRI in CIED patients, incorporating the new recommendations on DFTT.
Methods
Consecutive patients with CIED undergoing MRI were included. The protocol consisted of continuous monitoring during imaging, device interrogation pre- and post-MRI, reprogramming of the pacemaker to an asynchronous mode in pacemaker-dependent (PMD) patients and a non-tracking/sensing mode for non-PMD patients. All tachyarrhythmia therapies were disabled. Devices were interrogated for lead impedance, battery life, pacing, and sensing thresholds. All patients with ICD underwent DFTT/defibrillator safety margin testing (DSMT) post-MRI.
Results
A total of 92 MRI’s at 1.5 Tesla were performed in 38 patients. A total of 13 PMD patients, ten ICD patients, four cardiac resynchronization therapy with defibrillator (CRT-D) patients, and 11 non-PMD patients were scanned from four major manufacturers. No device circuitry damage, programming alterations, inappropriate shocks, failure to pace, or changes in sensing, pacing, or defibrillator thresholds were found on single or multiple MRI sessions.
Conclusions
Our protocol for MRI in CIED patients appears safe, feasible, and reproducible. This is irrespective of the type of CIED, pacemaker dependancy or multiple 24-h scanning sessions. Our protocol addresses early detection of potential complications and establishes a response system for potential device-related complications. Our observation suggests that routine DFTT/DSMT post-MRI may not be necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The use of magnetic resonance imaging (MRI) in patients with cardiac implantable electronic devices (CIED) such as pacemakers, implantable cardioverter-defibrillators (ICD), cardiac resynchronization therapy devices (CRT), and loop recorders has until recently, been considered an absolute contraindication. The powerful magnetic fields used in MRI are thought to be detrimental to pacemaker function and cause harm to patients undergoing MRI examinations. The potential risks of MRI on CIED include damage to hardware and inappropriate reprogramming. The effects on device hardware include device and lead movement, circuitry damage, and device-lead interface damage from heating. Inappropriate reprogramming complications include unexpected inhibition of pacing, mode changes, mode switches, inappropriate therapy, or rapid pacing leading to death [1–6].
Due to the wide spread application and powerful diagnostic capabilities of MRI, a decision to deny a patient an MRI evaluation may influence the quality of health care received. It is estimated that each year, more than one million CIED are prescribed worldwide. There have also been an increasing number of MRI systems utilized with more than 60 million magnetic imaging procedures performed yearly [7, 8]. Due to the expanding clinical indications for both CIED and MRI, there will be an increasing likelihood that patients will require both of these modalities. Expert opinion has recently suggests that the use of MRI in carefully selected patients with CIED may actually be considered a relative contraindication. This is based on a greater understanding of the inherent risks associated with MRI in this select population and the growing body of evidence demonstrating various strategies to mitigate potential complications related to cardiac device malfunction and mortality [9, 10].
Studies to determine the safety of MRI in patients with devices are limited. Despite this concern, over 500, mostly nonpacemaker dependent, patients have undergone MRI without marked complications or significant changes in CIED programming [11–13]. These cases demonstrated a favorable risk to benefit ratio using tailored MRI scanning, pre- and post-scan reprogramming and monitoring during scanning.
Despite the increasing number of successful MRI scans in patients with CIED, the cases of PMD patients remains limited, while the management of patients with ICDs is controversial. Previous studies have not evaluated defibrillation threshold testing (DFTT) or defibrillation safety margin testing (DSMT) post-MRI in patients with ICDs. Recently, the American Heart Association (AHA) has expressed concern over the lack of DFTT/DSMT in patients with ICD undergoing MRI [11]. However, there are concerns with post-MRI DFTT/DSMT, specifically dealing with cost, safety issues and lack of pre-scan DFTT/DSMT at baseline. In contrast, the European Society of Cardiology (ESC) does not support the routine use of DFTT/DSMT post-MRI believing the risk attributed to DFTT/DSMT may outweigh any potential benefit [13]. The AHA in there scientific statement regarding the safety of MRI in patients with CIED now recommends DFTT/DSMT post-MRI, despite scant data supporting the basis of this recommendation [11].
We designed a protocol incorporating the recent AHA recommendations, in order to evaluate the overall safety and efficacy of a strategy for performing MRI in patients with CIED. We evaluated 38 consecutive patients undergoing a total of 92 MRI studies. This is the first study to incorporate the new AHA recommendations regarding DFTT/DSMT in patients with CIED with one of the largest cohorts of PMD patients.
2 Methods
2.1 Patient selection
The protocol was reviewed and approved by the Providence Hospital Institutional Review Board. A total of 48 consecutive patients with CIED were evaluated for MRI and enrolled between September 2006 and December 2008. The indication for MRI was examined by a team of physicians, including an electrophysiologist and only those patients that MRI would have made a clinical impact were included. Patients were counseled on the risks and benefits of MRI and the impact it may have on their cardiac device and informed written consent was obtained. There were no exclusions based on type of cardiac device or manufacturer, device model, lead models, device dependancy, type of MRI scan, duration of study, or number of same-day studies. Of the 48 patients evaluated for MRI, ten were denied due to the fact that the MRI would not have made a significant clinical impact over an alternative imaging modality. There were no patients that refused the MRI after counseling with their physician and the protocol team of cardiovascular specialists.
2.2 MRI parameters
All MRI studies were performed at Providence Hospital and Medical Centers using an actively shielded 1.5-Tesla MRI scanner. In order to minimize the risk of radiofrequency (RF)-related potential damage caused by device or lead heating, the specific absorption rate (SAR) was limited to <2 W/kg as recommended by the ESC's position paper [13]. (I-1) MRI studies were categorized by anatomical region and designated as separate individual scanning sessions according to the Department of Radiology Protocol pertaining to safety and magnet exposure time.
2.3 Pre-MRI interrogation and patient monitoring
We have developed a protocol, which allows us to provide MRI tests to patients with a cardiac device that carry an acceptable and low risk while providing assistance with patient handling, pre-MRI interrogation, monitoring and post-MRI interrogation (Table 1). Part of our protocol consists of a study team that comprises of an electrophysiologist, cardiology fellow, pacemaker manufacturer representative and an electrophysiology nurse. These team members are present before, during, and after the MRI scan. The team is enabled to assist the electrophysiologist and to ensure patient safety. As such, rigorous safety precautions are provided for worst case scenerios, including on site availability of transcutaneous and transvenous pacing, external defibrillator and resuscitation materials as well as the capability for immediate transfer to the electrophysiology laboratory for hardware removal in the event of device failure. Non-PMD devices are switched to an OOO mode (if available) or non-tracking/sensing mode. PMD patients are reprogrammed to an asynchronous, demand pacing mode (VOO or DOO), at a rate of 80 beats per minute with maximum output settings to account for any changes in thresholds that may occur. All tachyarrhythmia therapies in ICDs were disabled.
During MRI scans, the protocol team vigilantly monitors various patient hemodynamics and cardiac parameters. Continuous monitoring of pulse oximetry as well as cycled blood pressure monitoring allows for accurate assessment of vital signs while not being subject to ECG artifacts produced by the magnetic field. Continuous verbal communication is ensured via an intercom to assess patient symptoms and is paramount for accurate real time assessment of the patients' level of consciousness.
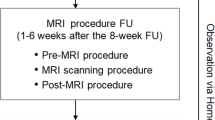
2.4 Post-MRI interrogation and follow-up
Patients were questioned by the protocol team for symptoms experienced during the MRI scan. Immediately post-MRI, devices were reprogrammed to their original settings. Devices were interrogated for lead impedance, battery life voltage, capture, and sensing thresholds immediately post-MRI and at 3 months follow-up. DSMT was performed on patients with ICDs post-MRI to evaluate for changes in defibrillator thresholds that may potentially place the patient at future risk of sudden cardiac death from lethal ventricular arrhythmias. If any changes were noted during the post-MRI interrogation, appropriate adjustments were made immediately if indicated.
2.5 Definition of defibrillation threshold testing
There are two categories for evaluating successful non-invasive defibrillation: DFTT and DSMT. The defibrillation threshold (DFT), defined as the lowest amount of energy capable of terminating an episode of induced VF, is most commonly determined through a step-down method (e.g., by successive lowering of shock strength). Because success of defibrillation is probabilistic, a true DFT cannot be established with certainty. This is why we perform DSMT, which is defined as the energy level capable of terminating at least two episodes of induced VF with at least ≥10 J of the maximum output [14, 15].
2.6 Statistical analysis
Results are reported as mean ± standard deviation (SD) or counts with percentages. Continuous variables were compared using a paired sample t test or Wilcoxon's rank-sum test when appropriate and p values <0.05 were considered significant. Statistical analysis was performed using SPSS software version 17.0 (SPSS Inc, Chicago, IL). All authors had unrestricted access to all the data and analysis.
3 Results
3.1 Patients and type of scans
As is seen in Fig. 1, a total of 92 MRI scans at 1.5-T were performed in 38 patients with CIED. Of these, 31 MRI scans were performed on 13 PMD patients and 26 MRI scans on ten ICD patients. Four patients for a total of six MRI scans were categorized as both PMD and as having a cardiac rhythm therapy device with defibrillator (CRT-D). Eleven out of the 38 patients for a total of 29 MRI scans were not PMD nor had an ICD. Four major CIED manufacturers were represented in each patient category: non-PMD, PMD, ICD, and CRT-D. Body areas scanned consisted of brain (n = 37), spine (n = 44), and others (n = 11), which was comprised of lower extremities and pelvis. Thirty out of the 38 patients (79%) had multiple same-day scans. The mean MRI scan duration was 26.1 min and did not statistically differ among dependancy status or type of device.
3.2 Safety and efficacy
All patients were able to be successfully scanned and completed their scans with the requesting physician's original intent. All MRI scans were categorized as diagnostic studies by independent readers and were free of image quality limiting artifact attributed to the CIED. No patient experienced spontaneous or device induced arrhythmias. In PMD patients, there was no evidence of pacermaker malfunction including inappropriate inhibition of pacing. There were no observed pauses noted or changes in rate settings during the MRI scanning. In addition, no patients reported pain, burning sensation or tugging during or immediately after MRI scanning. Artifacts due to electromagnetic interference (EMI) were seen in the majority of patients with ICD/CRT-Ds. In nine out of 14 (64%) patients, the EMI was interpreted by the device as fast ventricular tachycardia or ventricular fibrillation (VF; Fig. 2).
3.3 Device function post-MRI
Post-MRI device interrogation proceeded without difficulty, and there was no evidence of device circuitry damage. All pre-MRI settings remained unchanged. Compared with pre-MRI scan settings, there was no significant change in battery voltage, lead impedance or pacing and sensing thresholds (Fig. 3). There were no ICDs that delivered inappropriate therapy and no CIEDs experienced an electrical reset. These findings remained consistent without significant difference among patients irrespective of the number of same-day scans, repeat scans, or particular body part scanned. At 3 months follow-up, there were no significant changes in device parameters compared with immediate post-scan interrogation.
3.4 Multiple scans
Two patients that had experienced multiple MRI scans had additional repeat scans within 72 hours from their original scan due to changes in their clinical status. There was no significant hardware, programming, and clinical complications noted in this pre-specified subgroup of patients.
3.5 DSMT
Post-MRI DSMT was performed on 12 out of the 14 patients with ICD/CRT-Ds in accordance with our protocol. DSMT was not performed in the remaining two patients due to the discretion of the patient's individual cardiologist. DSMT was performed prior to the 3 months follow-up. During DSMT, all patients were induced into VF with shock on T wave and were successfully cardioverted. There was no difference in pre- and post-MRI DSMT (Fig. 4). Post-MRI DSMT energy delivered was determined by the device's pre-MRI DSMT settings at the time of initial implantation or subsequent generator changeout. There were no statistically significant differences in the mean energy delivered during DSMT pre- and post-MRI scanning (p = 0.26). All CIED patients that underwent DSMT had a left ventricular ejection fraction (LVEF) <35% with a mean LVEF was 27.5%. ± 6.4.
4 Discussion
There have been over 500 MRI scans successfully performed in patients with CIED [1–4]. These studies have evaluated the entire spectrum of patients with CIED including PMD and non-PMD, without significant patient or device complications. Despite the growing evidence of overall safety of MRI in CIED patients, information is still limited regarding PMD and CRT-D patients. Previous studies on PMD and CRT-D patients dealt with very small sample sizes and were limited mainly to scanning of the head [4]. In light of the new AHA statement recommending DFTT/DSMT post-MRI, no information exists on the validity of DFTT/DSMT in patients post-MRI. We report the first study to incorporate the new AHA recommendations to evaluate DFTT/DSMT, along with existing strategies in patients with CIED.
Despite the fears related to device exposure to MRI leading to hardware malfunction and damage or inappropriate reprogramming, most studies have demonstrated that under physician supervision, MRI can safely be performed on CIED patients [9–13]. In our study, using a carefully selected group of patients and utilizing a comprehensive protocol that includes a multidisciplinary team, we experienced no device and patient related complications. These include device-related symptoms, damage to hardware, inhibition of pacing, inappropriate reprogramming, spontaneous arrhythmias, or device-related arrhythmia. Moreover, PMD and CRT-D patients experienced the same efficacy and safety outcomes as non-PMD and non CRT-D patients, irrespective of the body region scanned or the number of scans.
All defibrillation safety margins post-MRI remained stable compared with pre-MRI, regardless of body region scanned. It has been reported that ICDs respond differently to MRI scans among various body regions [16–18]. This may be due to the amount of radiofrequency power that the ICD is exposed to which is dependent on the location of the scan; however this was not witnessed in our study.
4.1 Multiple scans
In our study, approximately 80% of the patients had multiple, same-day scans without changes observed in pre- and post-MRI CIED parameters or without affecting patient safety. In a recent publication, Naehle et al. reported on the cumulative effects of repeated MRI examinations on pacemakers [19]. They reported similar findings by demonstrating no change in lead impedance while demonstrating a statistically significant but clinically irrelevant trend in changes in pacing thresholds and battery life. This suggests that in CIED patients undergoing MRI, there is no cumulative effect seen with increased exposure from multiple MRI scans and therefore may exclude any potential additive risk to the patient attributed to successive scans.
4.2 Pacemaker-dependant patients
There exists a paucity of data on the reproducibility of safe and effective MRI scanning in PMD patients. The data regarding PMD patients are limited mainly to MRI of the head or shielded MRI using coils. This potentially underestimates the RF exposure to the CIED during MRI, especially when scanning in close proximity to the CIED [4, 5, 18]. Among the 17 PMD patients in our study, six patients had MRI scans (n = 13) involving the spine in close proximity to the CIED generator. The fact that no PMD patients experienced any clinical or device complication confirms the safety of MRI scanning in this highly selected group of patients when using our protocol.
4.3 Electrical reset
Electrical reset continues to be a source of concern that has been reported to occur in as high as 16% of patients undergoing MRI of the head [20]. Electrical reset is a safety feature to ensure pacing during battery end of life or with EMI interference and typically causes the device to be reverted to a default pacing mode. Despite this concern, there was no occurrence of electrical reset in all patients undergoing MRI. A possible reason for this observation as compared to previous reports, may be attributed to possible difference in programming modalities, older generation devices and the use of 3-T versus 1.5-T MRI.
4.4 Radiofrequency power
Maximum RF-induced heating occurs at the electrode-tissue boundary and may lead to deterioration of pacing thresholds [21]. Therefore, the lack of post-MRI changes in thresholds and impedance confirms no clinically relevant damage at the endocardial interface from excessive heating. Heating from RF has been shown to correlate with: higher SAR, the position of the electrode in relation to the scanner, lead configuration (looping), and likely correlates to the implantation depth and viability of the tissue [22–24]. The MRI scans in our study were performed without MRI sequence modification or alteration of MRI hardware and or software that may potentially affect the overall image quality of the scan.
4.5 Electromagnetic interference
Oversensing of EMI as VF was observed in the majority of ICD/CRT-D patients (64%). Although there exists the potential for delivering therapy for inappropriate VF sensing, it seems unlikely that ICDs can deliver an inappropriate shock within the MRI environment even when high voltage therapy is inadvertently left on [21]. The interaction between the static magnetic field and the device’s capacitor results in saturation of the transformer resulting in a short circuit with ineffective voltage transformation and the inability to charge the capacitor [21]. However, other issues may develop that are associated with EMI oversensing by ICDs and may lead to battery depletion from unintended attempts to charge the capacitor [21].
4.6 The role of defibrillator threshold testing
The management of ICD patients post-MRI remains controversial. Previous studies have concluded that post-MRI DFT/DSMT may be warranted under certain circumstances [11, 12, 25–29]. ICD malfunction has been documented in older generation devices after inadvertent MRI scans in CIED patients without using a comprehensive protocol to determine pre- and post-MRI device function.
Despite the AHA's position regarding DFTT/DSMT, dissenting opinion questions the utility of DFTT/DSMT in patients with CIED post-MRI, believing that the risk attributed to DFTT/DSMT may outweigh any potential benefit [13, 25–27]. As such, the ESC does not support the use of routine use of DFTT/DSMT post-MRI [13].
It may give reassurance to investigators that in a recent study among ICD patients without DFTT/DSMT post-MRI, five patients (21%) had successful appropriate therapy delivered for VF on long term follow-up [30]. Moreover, a number of recent studies have looked at ICD patients without undergoing DFTT and have reported no adverse events including device failure or inappropriate therapy [12, 21]. Without evidence of changes in DFT/DSM post-MRI in our cohort, the role of DFTT/DSMT, as recommended by the AHA, may not be warranted due to the potential harm and increase cost.
Routine DFTT/DSMT has been shown not to be routine after all in patients not undergoing MRI. There exists a real, albeit small increased risk of death, stroke and morbidity including prolonged resuscitation following complications associated with DFTT/DSMT [29, 31]. One must be careful not to extrapolate the data on DFTT/DSMT complications in patients not undergoing MRI to patients that are undergoing MRI, as DFTT/DSMT in this population has never been studied until now. Our study raises the question whether we should routinely perform DFTT/DSMT in ICD patients after 1.5-T MRI.
We feel that until a larger randomized study is undertaken regarding the routine use of DFTT/DSMT on post-MRI patients there may be certain conditions that warrant DFTT/DSMT post-MRI, including: patients with previously inducible VT at baseline, prior history of sustained VT, device induced ventricular arrhythmias during scanning and frequent ICD therapy utilizers. In the absence of these conditions, we feel that clinicians should refrain from routine DFTT/DSMT due to the inherent risks associated with such testing.
We believe that this is the first study to incorporate the new AHA recommendations based on DFTT/DSMT to evaluate defibrillation thresholds in patients with CIED undergoing MRI. With careful and strict supervision under an electrophysiologist-guided team, we have developed a protocol, which allows us to provide the lowest possible risk to CIED patients in need of an MRI. Our study provides a greater understanding of the overall safety and efficacy of a reproducible strategy for MRI in patients with CIED and may shed new light on the current controversy of routine DFTT/DSMT post-MRI.
References
Luechinger, R., Zeijlemaker, V. A., et al. (2005). In vivo heating of pacemaker leads during magnetic resonance imaging. European Heart Journal, 26, 376–383.
Pinski, S. L., Trohman, R. G., et al. (2002). Interference in implantable cardiac devices, part II (review). Pacing and Clinical Electrophysiology, 25(10), 1496–1509.
Gimbel, R., Bailey, S., et al. (2005). Strategies for the safe magnetic resonance imaging of pacemaker-dependant patients. Pacing and Clinical Electrophysiology, 28, 1041–1046.
Martin, E. T., Coman, J. A., et al. (2004). Magnetic resonance imaging and cardiac pacemaker safety at 1.5 Tesla. Journal of the American College of Cardiology, 43, 1315–1324.
Roguin, A., Zviman, M., et al. (2004). Modern pacemaker and implantable cardioverter/defibrillator systems can be magnetic imaging safe. in vitro and in vivo assesment of safety and function at 1.5 T. Circulation, 110, 475–482.
Derek, V. E. (2005). Is antitachycardia pacing a safe and efficacious alternative to shocks for fast ventricular tachyarrhythmia treatment? Nature Clinical Practice Cardiovascular Medicine, 2, 68–69.
Martin, E. T. (2005). Can cardiac pacemakers and magnetic resonance imaging systems co-exist? European Heart Journal, 26, 325–327.
Shellock, F., Fieno, D., et al. (2006). Cardiac pacemeaker: in vitro assesment at 1.5 T. American Heart Journal, 151, 436–443.
Gimbel, J. R. (2008). Magnetic resonance imaging of implantable cardiac rhythm Devicesat 3.0 Tesla. Pacing and Clinical Electrophysiology, 31, 795–801.
Sierra, M., & Machado, C. (2008). Magnetic resonance imaging in patients with implantable cardiac devices. Review in Cardiovascular Medicine, 9(4), 232–238.
Levine, G., Gomes, A., et al. (2007). Safety of magnetic resonance imaging in patients with cardiovascular devices. Circulation, 116, 2878–2891.
Gimbel, J. R., Kanal, E., et al. (2005). Outcomes of Magnetic Resonance Imaging (MRI) in selected patients with Implantable Cardioverter Defibrillators (ICD). Pacing and Clinical Electrophysiology, 28, 270–273.
Roguin, A., Schwitter, J., Vahlhaus, C., Lombardi, M., Priori, S., & Sommer, T. (2008). ESC position paper—magnetic resonance imaging in individuals with pacemakers or implantable cardioverter defibrillator systems. Europace, 10, 336–346.
Gold, M., Breiter, D., & Hahn, S. (2003). Safety of a single successful conversion of ventricular fibrillation before the implantation of cardioverter-defibrillators. Pacing and Clinical Electrophysiology, 26, 483–486.
Higgins, S., Mann, D., Calkins, H., et al. (2005). One conversion of ventricular fibrillation is adequate for implantable cardioverter-debibrillator. An analysis from the low energy safety study (LESS). Heart Rhythm, 2, 117–122.
Gimbel, J. R., & Kanal, E. (2004). Can patients with implantable pacemakers safely undergo magnetic resonance imaging? Journal of the American College of Cardiology, 43, 1325–1327.
Rozner, M. A., Burton, A. W., & Kumar, A. (2005). Pacemaker complication during magnetic resonance imaging. Journal of the American College of Cardiology, 45, 161–162.
Shellock, F. G., O'Neil, M., et al. (1999). Cardiac pacemeakers and implantable cardioverter defibrillators are unaffected by operation of extremity MR imaging system. American Journal of Roentgenology, 172, 165–170.
Naehle, C. P., Zeijlemaker, V., Thomas, D., Meyer, C., Strach, K., Fimmers, R., et al. (2009). Evaluation of cumulative effects of MR imaging on pacemaker systems at 1.5 Tesla. Pacing and Clinical Electrophysiology, 32(12), 1526–1535.
Naehle, C. P., Meyer, C., Thomas, D., Remerie, S., Krautmacher, C., Litt, H., et al. (2008). Safety of brain 3-T MR imaging with transmit-receive head coil in patients with cardiac pacemakers: pilot prospective study with 51 examinations. Radiology, 249(3), 991–1001.
Naehle, C. P., Strach, K., Thomas, D., Meyer, C., Linhart, M., Bitaraf, S., et al. (2009). Magnetic resonance imaging at 1.5 Tesla in patients with implantable cardioverters/defibrillators. Journal of the American College of Cardiology, 54(6), 549–555.
Hayes, D. L., Holmes, D. R., Jr., et al. (1987). Effect of 1.5 Tesla nuclear magnetic resonance imaging scanner on implanted permanent pacemakers. Journal of the American College of Cardiology, 10(4), 782–786.
Holmes, D. R., Jr., Hayes, D. L., et al. (1986). The effects of magnetic resonance imaging on implantable pulse generators. Pacing and Clinical Electrophysiology, 9(3), 360–370.
Luechinger, R., Duru, F., et al. (2001). Force and torque effects of a 1.5-Tesla MRI scanner on cardiac pacemakers and ICDs. Pacing and Clinical Electrophysiology, 24(2), 199–205.
Gimbel, J. R. (2008). The AHA scientific statement of MRI in patients with devices: neat, but incomplete. Unwise and unsupported. Pacing and Clinical Electrophysiology, 31(6), 649–651.
Coman, J. A., Martin, E. T., et al. (2004). Implantable cardiac defibrillator interactions with magnetic resonance imaging at 1.5 Tesla. Journal of the American College of Cardiology, 43, 138A.
Sandler, D. A., Coman, J. A., et al. (2006). Magnetic resonance imaging of patients with pacemakers and implantable cardioverter-defibrillators in a 1.5-Tesla magnet: A five-year experience. Heart Rhythm Society, 27th Annual Scientific Sessions, Boston, MA: May 17–20, 2006
Fiek, M., Remp, T., Reithmann, C., & Steinbeck, G. (2004). Complete loss of ICD programmability after magnetic resonance imaging. Pacing and Clinical Electrophysiology, 27, 1002–1004.
Glikson, M., Luria, D., et al. (2000). Are routine arrhythmia inductions necessary in patients with pectoral implantable cardioverter defibrillators? Journal of Cardiovascular Electrophysiology, 2, 127–135.
Nazarian, S., Roguin, A., Zviman, M. M., Lardo, A. C., Dickfeld, T. L., Calkins, H., et al. (2006). Clinical utility and safety of a protocol for noncardiac and cardiac magnetic resonance imaging of patients with permanent pacemakers and implantable-cardioverter defibrillators at 1.5 Tesla. Circulation, 114, 1277–1284.
Birnie, D., Tung, S., Simpson, C., Crystal, E., Exner, D., Ayala Paredes, F. A., et al. (2008). Complications associated with defibrillation threshold testing: the Canadian experience. Heart Rhythm, 5(3), 387–390.
Acknowledgments
We would like to specially thank the outstanding work of the Providence Hospital Heart Institute Pacemaker Clinic staff: Kim Bean, Michele Robinson and Amber Simms; Tim McElroy; the Providence Hospital Heart Institute Electrophysiology staff: Jessica Ottino, Jon Owings, Manu Seghal, Cathy Bell, Cordell Hastings, Midodrag Nedeljkovic, and Lisa Olson as well as the Providence Hospital Magnetic Resonance Imaging technicians and Department of Radiology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burke, P.T., Ghanbari, H., Alexander, P.B. et al. A protocol for patients with cardiovascular implantable devices undergoing magnetic resonance imaging (MRI): should defibrillation threshold testing be performed post-(MRI). J Interv Card Electrophysiol 28, 59–66 (2010). https://doi.org/10.1007/s10840-009-9463-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-009-9463-y