Abstract
In child clinical psychology, parent and child reports are typically used to make treatment decisions and determine the effectiveness of treatment. However, there are often moderate to large discrepancies between parent and child reports, and these discrepancies may reflect meaningful information about the parent, the child, and the parent–child relationship. Additionally, parent–child discrepancy may predict treatment outcome. This study examined parent–child discrepancy in a sample of 62 children (10.15±1.26 years old) with prominent social competence deficits and mixed diagnoses who were treated with a resilience-based, cognitive–behavioral group therapy program (the Resilience Builder Program) in a private clinical setting. Further analyses were conducted to investigate whether parent–child discrepancy related to treatment outcome. Consistent with the literature, prominent parent–child discrepancy was found across domains, with parents generally reporting more severe symptomatology. Treatment with the Resilience Builder Program resulted in significant improvement in parent report of multiple domains of functioning, including resilience, social skills, and emotion and behavior regulation. Importantly, larger parent–child discrepancy at the start of therapy was predictive of poorer overall treatment response. Given its impact on therapeutic effectiveness, these results suggest that parent–child disagreement regarding the child’s impairment at the onset of therapy is worthy of assessment prior to treatment, and may itself be a topic worthy of targeting in treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adequate assessment of child psychological conditions requires the use of multiple informants, primarily parents and children, since there is no single definitive way to measure psychopathology in children, and no viable biological marker exists for any of the mental health disorders (De Los Reyes 2011; American Psychiatric Association 2013). Discrepancies between informant reports, however, are routinely found across samples, occur across measurement methods, and are usually in the moderate to large range (De Los Reyes and Kazdin 2005). Several meta-analyses of over 50 years of published research reveal that low cross-informant correspondence is a long-known finding in clinical assessments that continues to affect assessments currently conducted in research and clinical practice (for a review, see De Los Reyes et al. 2015).
Discrepancies between parent and child reports do not simply reflect a lack of reliability or validity, because large discrepancies still exist when each informant’s report is reliable and valid across measures (e.g., Achenbach and Rescorla 2001; Baldwin and Dadds 2007; Comer and Kendall 2004). Even when measures are identical across informants, discrepancy is still high (Achenbach 2006). Thus, parent–child discrepancy should not be discarded as measurement error, but should instead be examined as a meaningful piece of data on its own (De Los Reyes and Ohannessian 2016).
De Los Reyes et al. (2013b) have advanced frameworks to explain informant discrepancies in the assessments of child and adolescent psychosocial functioning (e.g., the Operations Triad Model). The Attribution Bias Context (ABC) Model (De Los Reyes and Kazdin 2005) posits three main ways informants differ that contribute to informant discrepancies: (A) their explanations for the cause of the child’s behavior (internal or external); (B) their perspectives used to identify if and what behaviors merit treatment; and (C) the contexts in which they observe the behavior and engage in the assessment process.
Related to the second component of the ABC Model, several researchers have explored characteristics of the parent (e.g., depression), the child (e.g., attention deficit hyperactivity disorder (ADHD)), and the parent–child relationship (e.g., conflict, poor communication, low parental acceptance and engagement) that may result in differing perspectives of the child’s symptomatology and need for treatment (see De Los Reyes and Kazdin 2005, 2006; Hoza et al. 2012; Kolko and Kazdin 1993; Grills and Ollendick 2003; Treutler and Epkins 2003; Van Roy et al. 2010; Yeh and Weisz 2001; Youngstrom et al. 2000). Based on studies such as these, parent–child discrepancy may be the result of: (1) distorted perceptions due to psychopathology in one or both informants (e.g., maternal depression predicts greater parent-reported symptomatology; ADHD in the child predicts lower self-reported symptomatology (i.e., the Positive Illusory Bias (PIB), which is the tendency for youth with ADHD to report greater social competence than parents, teachers, and peers (Hoza et al. 2002)), (2) a reflection of real-world arguments between parent and child about whether a symptom is present or needs to change, (3) lack of parental acceptance of child behavior, and/or (4) poor communication about problematic symptoms. However, this prior research utilized methodologically limited methods (i.e., difference scores between parent and child report) to measure parent–child discrepancy (for a review, see De Los Reyes and Kazdin 2004; Laird and De Los Reyes 2013). The concern with relying on difference scores is that they may not provide meaningful information beyond the individual reports used to generate these difference scores. Instead, it is recommended that interaction terms be used to measure parent–child discrepancy because they provide new information beyond the main effects of the individual informants’ reports (Laird and Weems 2011) and demonstrate criterion validity by revealing the same information as direct assessments of informant discrepancy (De Los Reyes et al. 2013a).
Prior research and theoretical work has also discussed why parents are more likely than children to hold the perspective that child symptoms merit treatment, which in turn leads to parent–child discrepancy, in accordance with the ABC Model. De Los Reyes and Kazdin (2005) posit that if a child is not distressed by a behavior then he/she is unlikely to endorse its presence and/or the need for treatment. Relatedly, Phares and Danforth (1994) found adolescents are less likely to report being distressed by their behaviors than are their parents, and in turn, are less likely than their parents to want to seek treatment for these behaviors. Additionally, parents are generally the informants seeking treatment for their child (Kazdin 2000). In accordance with Tversky and Marsh’s (2000) theory that a negative perspective biases one’s memory for negative events, parents are more likely than their child to recall and endorse negative behaviors consistent with their perspective that their child needs treatment (De Los Reyes and Kazdin 2005).
While the majority of research on parent–child informant discrepancy has sought to identify factors that contribute to discrepancy, a limited number of studies have examined relationships in the opposite direction; that is, how informant discrepancy may contribute to other clinical factors, such as delinquent behaviors, police contacts, school expulsion, emotional problems, social deficits, and suicide attempts (De Los Reyes et al. 2010; Ferdinand et al. 2004; Guion et al. 2009).
Minimal research has examined if parent–child informant discrepancy contributes to the effectiveness of psychotherapeutic interventions. This is surprising given that, according to the ABC Model, one of the primary contributors to informant discrepancy is disagreement regarding whether a child’s symptoms merit treatment, and that disagreement on the need for treatment or treatment goals is a strong predictor of poor treatment outcomes (Garland et al. 2007). Disagreement about the need for treatment is likely a strong predictor of poor treatment outcomes because if either the parent or the child is unaware, or does not believe, that a particular behavior exists or needs to be treated, then he/she will be less motivated to engage in treatment, and thus treatment will be less effective (Israel et al. 2007; Brookman-Frazee et al. 2008). Two studies have examined the relationship between parent–child disagreement and a factor related to therapy outcome (i.e., attendance; parental involvement). The first found that disagreement between parents and children on treatment goals at intake predicted decreased attendance at therapy sessions (Brookman-Frazee et al. 2008). The second study found that informant discrepancy on scales measuring interpersonal problems at intake predicted decreased parental involvement in treatment (Israel et al. 2007). There are a limited number of studies that have examined the relationship between pre-treatment parent–child discrepancy and actual treatment outcome. Panichelli-Mindel et al. (2005) found that in a sample of children with anxiety disorders, when parents and children disagreed regarding the presence of an anxiety disorder (based on a structured intake interview), those youth had poorer treatment response than when both parent and child endorsed the presence of an anxiety disorder. Similarly, Humphreys et al. (2015) found that, in a sample of children receiving cognitive–behavioral therapy (CBT) for post-traumatic stress disorder, treatment responders had lower levels of parent–child symptom disagreement at baseline than treatment non-responders. Conversely, De Los Reyes et al. (2010) found that, in a sample of children with social phobia, pre-treatment parent–child discrepancies did not differ between treatment responders and non-responders. Additionally, Hoffman and Chu (2015) found that, in a sample of children receiving CBT for anxiety disorders, greater parent–child goal agreement at baseline predicted greater parental satisfaction with treatment, but did not significantly predict diagnostic remission. Only one study of which we are aware examined the relationship between pre-treatment parent–youth discrepancy and treatment outcome using currently recommended approaches to assessing discrepancy (e.g., interaction terms). In a sample of youth (ages 7–17 years) receiving CBT for anxiety disorders, youth were less likely to be diagnosis-free post-treatment if they reported fewer symptoms than their parents at the start of treatment (Becker-Haimes et al. 2017). In sum, despite a strong theoretical association, the actual nature of the relationship between parent–child discrepancy and child’s response to therapy remains unclear. If parent–child discrepancy does impede treatment success, efforts to identify discrepancies, why they occur, and ways to reduce them may contribute to increased therapy effectiveness and improved mental health for children. It is thus essential that research expand upon recent studies to examine the impact of parent–child discrepancy on treatment success using valid approaches to assess discrepancy (e.g., interaction terms).
The current study aims to address the gap in research on the impact of informant discrepancies on treatment by examining whether parent–child discrepancy affects treatment outcome in a clinical sample of children with mixed diagnoses. In doing so, we present the first study of this sort to use a sample of youth other than those with anxiety, and the first being treated in a “real-world” clinical service setting. Perhaps more importantly, this study is the second of its kind to utilize the currently recommended approach to assess discrepancy (i.e., interaction terms). Given that youth tend be less distressed by their presenting problems than their parents (Phares and Danforth 1994), and parents initiated treatment in this sample, we predicted that there would be significant discrepancies between parent and child reports, with parents reporting greater symptomatology in their children than children self-reported. Additionally, we predicted that larger parent–child discrepancies would predict worse overall treatment outcome, based on the theory that if either the parent or the child is unaware, or does not believe, that a particular behavior exists or needs to be treated, then he/she will be less motivated to engage in treatment, and thus treatment will be less effective (Israel et al. 2007; Brookman-Frazee et al. 2008).
Method
Participants
Participants included children, aged 7–12 years old, participating in the Resilience Builder Program® (RBP), manualized psychotherapy groups at Alvord, Baker, & Associates, LLC, a large private practice in Maryland. Children were primarily referred to the practice by another mental healthcare provider, pediatrician, or school counselor, although many were referred by their parents. Regardless of the referral party, parents initiated treatment. At intake a licensed clinician from the practice performed a clinical assessment to determine whether the child’s psychosocial deficits warranted inclusion in the RBP. The RBP is intended for youth with prominent psychosocial deficits, and groups include children with a range of diagnoses, including ADHD, anxiety, depression, and high-functioning autism spectrum disorders (ASD). For this particular study, with the purpose of examining parent–child discrepancy pre-therapy and its effect on post-therapy outcomes, only families who completed both a Behavioral Assessment System Checklist for Children, 2nd Edition (BASC-2; Reynolds and Kamphaus 2004) child self-report and parent report at pre- and post-therapy were included in the sample. Exclusionary criteria included a diagnosis of conduct disorder, intellectual disability, and psychosis, as these preclude enrollment in the RBP.
A total of 185 children were enrolled in the RBP and invited to enroll in the effectiveness study. Of these, 150 parents/children signed consent/assent forms, for an enrollment rate of 81%. Of the 150 children who enrolled, 62 handed in a BASC-2 self- and parent report, pre- and post-therapy, and constitute the sample of this study (see Fig. 1). We found no differences in demographic or clinical variables between the children who enrolled in the study vs. those who declined participation, or between research completers vs. dropouts (i.e., those who provided pre-therapy data but failed to provide post-therapy data) (Rich et al. 2014). All 62 children included in the subsequent analyses completed the 12-week RBP therapy. The sample reflected a total of 28 different therapy groups, conducted by eight different clinicians. Neither rates of participation in research nor therapy outcome differed based on treatment group or clinician.
Within the sample of 62 children, the average age was 10.15±1.26 years old and 62.9% were male. The majority of the sample was Caucasian (75.8%) and living with both biological parents (67.7%). All clientele were reported to have prominent social deficits as indicated by the pre-therapy scores on the Social Skills Improvement System (SSIS; Elliott et al. 2008) and the BASC-2. The average standard score on the Social Skills scale of the parent SSIS was 76.85 (indicating Below Average levels of social skills), and the average T score on the Social Skills scale of the parent BASC-2 was 40.19 (indicating At-Risk levels of social skills). Further, on these Social Skills subscales, 78.7% of the participants were in the Well Below Average or Below Average range on the SSIS, 66.1% of the participants were in the Clinically Significant or At-Risk range on the BASC-2, and 85.2% of the sample was in at least one of those clinically impaired ranges on those measure of social functioning. Additionally, to ascertain proxy information about the child’s diagnostic status, parents completed a demographic questionnaire on which they were asked “Is your child CURRENTLY diagnosed by a pediatrician or mental health professional with any of the following?” and were provided a list of common childhood psychological disorders. Of the 62 children, 72.5% had a diagnosis as reported by a parent. Of those with a diagnosis, 71.1% had ADHD, 31.2% had an anxiety disorder, 13.3% had high-functioning ASD, and 11.1% had depression. See Table 1 for a complete description of participants.
Procedure
Licensed clinicians from the practice conducted intakes to ensure that each child’s psychosocial deficits were well suited for the RBP. As part of the intake, parents were prompted to indicate on the registration form whether they were willing to be contacted about the study of RBP effectiveness. Those who marked that they were willing to be contacted were given an explanation of the study by a graduate or undergraduate research assistant. Consent and assent forms were then signed at the office, generally at the first therapy session. The effectiveness study was IRB approved.
Pre-therapy data was collected from parents and children no more than 2 weeks prior to the first therapy session. Phone calls were made to families following consent and assent to remind families to complete the measures within the required time period. Similarly, post-therapy questionnaire packets were obtained from families within 2 weeks after the final therapy session and reminder phone calls were made during this time. Once post-therapy parent and child measures were returned, children were compensated with a US$20 gift card.
The RBP is a manualized group psychotherapy intervention, based on the evidence-based principles of CBT, that is intended to increase social competence and resilience in children. The RBP was created in 1992 by Mary Alvord, Ph.D., specifically for administration in a clinical service setting (Alvord and Rich 2012; Alvord et al. 2011). This study occurred at the private psychotherapy practice of Alvord, Baker, & Associates, LLC, in the Maryland suburbs of Washington, D.C. Each Fall and Spring semester, Alvord, Baker, & Associates, LLC conducts approximately 30 youth-focused RBP psychotherapy groups. Each group has 4–6 children and is age and gender homogeneous. In the current study, nine therapists administered RBP groups, four of whom had a Ph.D. in psychology, three had a Psy.D., and two had a MSW. All of the therapists in the study had at least 2 years of experience directing RBP groups.
The RBP consists of 14 weekly 1-h sessions. Each session has a specific topic that addresses social functioning, emotional and behavioral self-regulation, and/or resilience. Each group session included four components: (1) The Interactive Didactic Component (~30 min), starts with a review of the prior week’s topic via discussion between the children about their homework. Then the therapist introduces the new topic and demonstrates the skills involved. Lastly, children discuss the behaviors needed to perform the skills, and often role-play them with therapist coaching. (2) The Behavioral Rehearsal Component (~20 min) allows children to practice the week’s skills in real-life play situations and receive peer feedback under the supervision of the therapist. (3) The Relaxation and Self-Regulation Techniques Component (~10 min) involves teaching self-regulation and calming techniques, such as progressive muscle relaxation and visualization. (4) The Parental Component includes the parents joining the group for the final 15 min once a month so that the children can demonstrate their progress and new skills. Additionally, parents receive a weekly letter explaining the week’s skills and how they can be practiced at home. Finally, a mid-therapy individual meeting is completed with each parent to review progress and address any concerns. Skill generalization is encouraged via weekly homework, the parental component, and an end-of-group field trip in the community.
Pilot effectiveness studies of the RBP suggest improved functioning in multiple domains with varied samples of youth. For example, in youth with ADHD, completion of the RBP improved social competence, self-control, and emotion regulation, while it reduced externalizing problems, hyperactivity, impulsivity, and negative emotions. These positive outcomes were observed by multiple informants (i.e., parent, child, and teacher report) across multiple contexts (i.e., at home, with peers, in school) (Rich et al. 2017). In youth with anxiety disorders, the RBP resulted in significant improvement in child, parent, and teacher report of social functioning, positive emotions, emotion regulation, and family functioning, with reduced depressive symptoms (Watson et al. 2014). Finally, in youth with ASDs, the RBP resulted in significant improvement in parents’ report of their child’s social skills and communication, and child report of improved communication skills, less negative emotion, and increased emotion control (Aduen et al. 2014).
Measures
Parents and children completed the BASC-2 and the SSIS. These measures were selected because they are commonly used measures of psychological functioning in children and provide an assessment of both broad domain functioning (i.e., internalizing and externalizing disorders), as well as a more targeted assessment of domains of interest given the prominent social impairments of our sample and the therapeutic goals of the RBP treatment (i.e., social skills, resilience, emotion regulation). Most importantly, given that this study aimed to compare functioning and outcome across informants, both the BASC-2 and SSIS can be completed by children and parents, which optimized our ability to examine informant discrepancy. Finally, these measures allowed us to address two of the three potential causes for informant discrepancy theorized in the ABC Model: the internal or external causes for the child’s difficulties, and the differing contexts (i.e., at home, in school, and with peers) in which the difficulties may be exhibited.
Behavioral Assessment System for Children, 2nd Edition (BASC-2)
The BASC-2 is a widely used comprehensive assessment of child emotional and behavioral functioning, with strong psychometric properties, including excellent internal consistency (0.90–0.97) (Reynolds and Kamphaus 2004). Parents, children, and teachers answer 139 to 160 items on a 4-point Likert scale that ranges from Never (1) to Almost Always (4). Items comprise several internalizing (e.g., Anxiety, Depression) and externalizing (e.g., Aggression, Hyperactivity) subscales. The BASC-2 was selected for evaluating the RBP because its subscales of Resiliency, Developmental Social Disorders, Emotional Self-Control, Negative Emotionality, Anger Control, and Social Skills are highly relevant to the RBP agenda.
Social skills improvement system (SSIS)
The SSIS (Elliott et al. 2008) measures several areas of child social functioning, including Social Skills (i.e., Communication, Cooperation, Assertion, Responsibility, Empathy, Engagement, and Self-Control) and Problem Behaviors (i.e., Externalizing Problems, Bullying, Hyperactivity/Inattention, Internalizing Problems, and Autism Spectrum Behaviors). Children, parents, and teachers can complete the measure. The SSIS is often viewed as a standard for social skills measurement because of its wide-ranging approach and application, ability to be used with multiple informants, and strong psychometrics, including acceptable to excellent internal consistency (0.72–0.96) (Erdlen and Rickrode 2007). It is also considered the most robust measure of change in social functioning following treatment (Sim et al. 2006). Standard scores (M = 100, SD = 15) are given for the three composite scales (Social Skills, Problem Behaviors, and Academic Competence). Categorical scores, based on 1 SD above or below the mean, are given for the subscales to indicate the child’s level of performance (i.e., average, above average, below average) in comparison to peers of the same age and sex.
Demographic Questionnaire
For the purpose of evaluating basic demographic information, a standard demographic questionnaire, including questions about the child’s age, sex, ethnicity, family composition, and socioeconomic status, was developed by the practice. Questions about current and prior psychopharmacological and/or psychotherapeutic treatment history, as well as current and past psychological diagnoses, were also included to attain basic clinical information.
Data Analyses
We assessed parent–child discrepancy based on raw pre-therapy BASC-2 scores on the only subscales common to both parent and child report forms: Attention Problems, Anxiety, Depression, Atypicality (e.g., social oddity), and Hyperactivity. To account for differing numbers of questions between parent and child scales, we calculated average raw subscale scores. Paired-sample t tests were then used to assess the degree of parent–child discrepancy.
Before examining whether pre-therapy parent–child discrepancy predicted treatment outcome, we conducted paired-sample t tests to compare pre-therapy and post-therapy BASC-2 and SSIS scores to determine which domains of greatest interest to the RBP agenda (i.e., BASC-2 Resiliency, Developmental Social Disorders, Emotional Self-Control, Negative Emotionality, Anger Control, Social Skills; SSIS Social Skills) showed significant improvement following RBP treatment. Thereafter, we regressed mean-centered parent report, mean-centered child report, and their interaction on domains with significant pre- to post-therapy change (with change scores between pre- and post-intervention as the dependent variable) (Laird and De Los Reyes 2013). This methodological approach has strong criterion validity support and is suggested to be the most accurate way to analyze the impact of discrepancy on outcome (De Los Reyes et al. 2013a). Although there is value in predicting post-therapy scores while controlling for pre-therapy functioning, change scores were used so as to provide a variable on which subsequent secondary analyses could be conducted, and because some have suggested that using change scores provides a stronger independence from sample size and is more indicative of clinically meaningful change (Eisen et al. 2007). As detailed below, there was significant change following the RBP treatment on six of the seven scales examined per parent report (i.e., BASC-2 Resiliency, Developmental Social Disorders, Emotional Self-Control, Negative Emotionality, Anger Control; SSIS Social Skills), and these served as the basis for our regression analyses. Significance was determined using a standard alpha of p < 0.05. We plotted significant interactions to examine whether parent–child dyads with little or no discrepancy (i.e., parent and child report high symptomatology; parent and child report low symptomatology) predicted significantly more treatment success than parent–child dyads with large discrepancy (i.e., parent reports low symptomatology and child reports high symptomatology; parent reports high symptomatology and child reports low symptomatology). To determine the level of symptomatology, significant interactions were plotted at ±1 SD of the moderator to determine the relationship between parent (or child) report and pre–post change scores at high (+1 SD) and low (−1 SD) levels of parent (or child) report (Whisman and McClelland 2005).
Results
Parent–Child Discrepancy
Results indicate significant parent–child discrepancy across all five BASC-2 subscales common to both parent and child: Anxiety, t(59) = 2.09, p = 0.04, Depression, t(59) = 7.10, p < 0.001, Hyperactivity, t(59) = 3.86, p < 0.001, Attention Problems, t(59) = 8.95, p < 0.001, and Atypicality, t(59) = −2.23, p = 0.03. Parents reported significantly higher scores than children on the Anxiety, Depression, Hyperactivity, and Attention Problems subscales. Conversely, children reported significantly higher scores on Atypicality (i.e., social oddities) than parents. See Fig. 2 for a graph of these results.
Treatment Outcome
Although this study focused on informant discrepancy, it is important to note that RBP therapy resulted in significant change in multiple social, emotional, and behavioral domains of parent report (see Table 2). Table 2 shows the significant improvements in parent-reported Developmental Social Disorders, t(55) = 3.64, p = 0.001, Negative Emotionality, t(55) = 4.06, p < 0.001, Emotional Self-Control t(55) = 2.78, p = 0.01, Anger Control, t(55) = 2.57, p = 0.01, and Resiliency t(55) = −2.82, p = 0.01 on the BASC-2, and significant improvement in parent-reported Social Skills t(55) = −3.34, p = 0.002 on the SSIS. It is important to note, however, that there was no significant improvement on parent-reported Social Skills on the BASC-2, and no significant change was found according to child report.
Relationship of Informant Discrepancy and Treatment Outcome
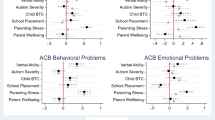
When we examined the relationship between informant discrepancy and parent-reported change following RBP therapy, results indicated that greater pre-treatment parent–child discrepancy on Depression (see Table 3), Anxiety (see Table 4), and Atypicality (see Table 5) predicted less treatment success. Conversely, greater pre-treatment parent–child discrepancy on Hyperactivity (see Table 6) predicted more treatment success.
Specifically, greater pre-treatment parent–child discrepancy on Depression significantly predicted a smaller decrease (indicating less improvement) in parent-reported Developmental Social Disorders following therapy, β = 10.80, t(58) = 2.47, p = 0.01. As can be seen in Fig. 3, and for the purposes of interpreting the other figures we present, high parent report–low child report dyads showed little improvement in Developmental Social Disorders following RBP treatment and low parent report–high child report dyads showed a slight worsening in Developmental Social Disorders following RBP treatment. Conversely, low parent report–low child report dyads and high parent report–high child report dyads showed large improvements in Developmental Social Disorders following RBP treatment, with the former more so than the latter. Greater pre-treatment parent–child discrepancy on Depression also significantly predicted less decrease (indicating less improvement) in parent-reported Anger Control, β = 13.98, t(58) = 3.03, p = 0.004, Emotional Self-Control, β = 19.05, t(58) = 2.72, p = 0.01, and Negative Emotionality, β = 11.51, t(58) = 2.27, p = 0.03 following RBP treatment. Greater pre-treatment parent–child discrepancy on Depression significantly predicted a greater decrease (indicating less improvement) in parent-reported Resiliency, β = −11.17, t(59) = −2.38, p = 0.02 following RBP treatment.
Interaction between parent-reported Depression and child-reported Depression predicts change in BASC-2 Developmental Social Disorders scores following RPB treatment. Note: BASC-2 Behavior Assessment System for Children, Second Edition, RBP Resilience Builder Program; Positive change scores reflect a decrease (improvement) in Developmental Social Disorders. Results indicate that high parent report–low child report dyads showed little improvement in Developmental Social Disorders following RBP treatment and low parent report–high child report dyads showed a slight worsening in Developmental Social Disorders following RBP treatment. Conversely, low parent report–low child report dyads and high parent report–high child report dyads showed improvements in Developmental Social Disorders following RBP treatment, with the former more so than the latter
Further, greater pre-treatment parent–child discrepancy on Anxiety significantly predicted less decrease (indicating less improvement) in parent-reported Emotional Self-Control, β = 12.33, t(59) = −2.53, p = 0.01 (see Fig. 4) following RBP treatment.
Interaction between parent-reported Anxiety and child-reported Anxiety predicts change in BASC-2 Emotional Self-Control scores following RPB treatment. Note: BASC-2 Behavior Assessment System for Children, Second Edition, RBP Resilience Builder Program; Positive change scores reflect a decrease (improvement) in Emotional Self-Control. Results indicate that high parent report–low child report dyads showed worsening Emotional Self-Control following RBP treatment and low parent report–high child report dyads showed no change in Emotional Self-Control following RBP treatment. Conversely, low parent report–low child report dyads and high parent report–high child report dyads showed large improvements in Developmental Social Disorders following RBP treatment, with the latter more so than the former
Additionally, greater pre-treatment parent–child discrepancy on Atypicality significantly predicted less decrease (indicating less improvement) in parent-reported Emotional Self-Control, β = 17.84, t(59) = 2.58, p = 0.01, and more decrease (indicating less improvement) in Resiliency, β = −11.11, t(59) = −2.44, p = 0.02 (see Fig. 5) following RBP treatment.
Interaction between parent-reported Atypicality and child-reported Atypicality predicts change in BASC-2 Resiliency scores following RPB treatment. Note: BASC-2 Behavior Assessment System for Children, Second Edition, RBP Resilience Builder Program, Negative change scores reflect an increase (improvement) in Resiliency. Results indicate that high parent report–low child report dyads showed worsening Resiliency following RBP treatment and low parent report–high child report dyads showed a slight worsening in Resiliency following RBP treatment. Conversely, low parent report–low child report dyads and high parent report–high child report dyads showed large improvements in Resiliency following RBP treatment, with the former more so than the latter
Finally, parent–child discrepancy on Hyperactivity significantly predicted a larger decrease (indicating more improvement) in parent-reported Emotional Self-Control, β = −9.77, t(59) = −2.10, p = 0.04 and Negative Emotionality, β = −10.33, t(59) = −3.11, p = 0.003 (see Fig. 6) following RBP.
Interaction between parent-reported Hyperactivity and child-reported Hyperactivity predicts change in BASC-2 Negative Emotionality scores following RPB treatment. Note: BASC-2 Behavior Assessment System for Children, Second Edition, RBP Resilience Builder Program; Positive change scores reflect a decrease (improvement) in Negative Emotionality. Results indicate that high parent report–low child report dyads and low parent report–high child report dyads showed large improvements in Negative Emotionality following RBP treatment. Low parent report–low child report dyads and high parent report–high child report dyads slight improvements in Negative Emotionality following RBP treatment
Discussion
This study was conducted in a clinical sample of children with prominent social impairments and heterogeneous diagnoses to examine parent–child informant discrepancy and whether degree of discrepancy related to treatment outcome.
Parent–Child Discrepancy
Consistent with the literature (De Los Reyes et al. 2013b; De Los Reyes and Kazdin 2005), there were significant parent–child discrepancies across all internalizing and externalizing domains examined—Anxiety, Depression, Hyperactivity, Attention Problems, and Atypicality. Parents reported significantly higher scores than children on Anxiety, Depression, Hyperactivity, and Attention Problems, whereas children reported significantly higher scores on Atypicality (i.e., social oddities). Although prior research suggests that patterns of discrepancy may vary based on the symptoms being measured (e.g., Achenbach et al. 1987, Becker et al. 2016), we note that our results found informant discrepancy across multiple domains of functioning and symptomatology (i.e., affective, behavioral, and social). The finding of higher parent scores is consistent with previous studies. It is also consistent with the ABC Model and the notion that parents typically view their child’s symptomatology as more problematic and warranting of treatment than do children (Phares and Danforth 1994). According to the ABC Model, differing perspectives on whether behaviors merit treatment is one of the primary contributors to informant discrepancy (De Los Reyes and Kazdin 2005). In this sample, parents are the informant enrolling the child in treatment, and are thus more likely to hold the perspective that treatment is warranted. Children, on the other hand, generally did not report elevated symptomatology. Potentially children in this sample underestimated their impairment, which is consistent with the PIB theory (Hoza et al. 2012). The PIB theory posits that children with ADHD overestimate their competence. A similar bias to the PIB is also seen in peer-rejected children without ADHD (Hymel et al. 1993). Given that 51% of this sample had ADHD, and the entire sample had social deficits and likely faced peer rejection, the pattern of children reporting less symptomatology than parents may reflect the composition of our sample. Thus, our data appear to support the presence of the PIB in a clinical sample of socially impaired youth with and without ADHD. The greater reports of Atypicality by youth as compared to parents is inconsistent with findings that children with a PIB are most discrepant from parent reports in their domains of most prominent impairment (Hoza et al. 2012). It is possible that since children in our sample were attending a social competence psychotherapy group, they were more aware of their social difficulties.
Treatment Outcome
According to parent report, significant treatment gains were found across multiple domains. These results provide preliminary data of the effectiveness of the RBP therapy for improving the social, emotional, and behavioral functioning of youth with prominent psychosocial impairments seen in a clinical service setting. These treatment gains were not significant according to child report.
More germane to this study, our results provide evidence of the predictive utility of informant discrepancies on treatment outcome, and uniquely so in a heterogeneous clinical sample and using interaction terms. Of the domains with significant pre- to post-therapy change, greater parent–child discrepancy on Depression, Anxiety, and Atypicality was associated with poorer therapy outcomes. Consistently, parent–child dyads in which the parent-reported high levels of symptomatology and the child-reported low levels of symptomatology pre-therapy showed the smallest changes or no decreases in symptomatology post-therapy, and sometimes even an increase in symptomatology according to parent post-therapy report. Conversely, parent–child dyads in which both the parent and child-reported low levels of symptomatology pre-therapy showed the largest decreases in symptomatology post-therapy, followed by parent–child dyads in which both the parent and child-reported high levels of symptomatology pre-therapy. These results, as predicted, suggest that parent–child agreement is associated with greater treatment success, whereas parent–child discrepancy, specifically in which the child reports less symptomatology, is associated with poorer treatment response. These results are consistent with the finding that disagreement on the need for treatment is a strong predictor of poor treatment outcomes (Garland et al. 2007). Dyads in which parents reported high levels of symptomatology and children reported low levels of symptomatology may have resulted in the poorest treatment outcomes because if a child is unaware, or does not believe, that a particular symptom exists or needs to be treated, then he/she will be less motivated to engage in treatment, and thus treatment will be less effective (Israel et al. 2007; Brookman-Frazee et al. 2008). This, however, does not explain why dyads in which both the parent- and child-reported low levels of pre-therapy symptomatology showed the largest decreases in symptomatology post-therapy. Perhaps because agreement on symptomatology may reflect a better parent–child relationship and better family functioning (Kolko and Kazdin 1993; Grills and Ollendick 2003; De Los Reyes and Kazdin 2006; Treutler and Epkins 2003; Van Roy et al. 2010), these children may have improved more because they worked successfully with their parents on the homework, skills, and goals of treatment.
Interestingly, discrepancy on the Depression subscale had the most extensive association with poor treatment outcome across multiple domains (e.g., Anger Control, Developmental Social Disorders, Emotional Self-Control, Negative Emotionality, and Resiliency). This may be due to discrepancy being greatest on the Depression subscale as compared to other subscales, indicating that a larger discrepancy has a more significant impact on outcome. Additionally, since children reported significantly less depression than their parents, it may indicate that lower child-perceived distress, operationalized in this case as lower child-reported Depression, impacts child engagement in treatment and thus treatment success. This is consistent with De Los Reyes and Kazdin’s (2005) conjecture that if a child is not distressed by his/her behaviors then he/she is unlikely to endorse the need for treatment, and, in turn, likely to show poorer treatment outcomes (Israel et al. 2007; Brookman-Frazee et al. 2008).
Surprisingly, every significant interaction term examined for the domains with significant pre- to post-therapy change revealed that greater parent–child discrepancy on Hyperactivity was associated with better therapy outcomes. Consistently, parent–child dyads in which the child-reported high levels of hyperactivity and the parent-reported low levels of hyperactivity pre-therapy showed the largest decreases in symptomatology post-therapy. It is important to note that overall parents reported significantly more Hyperactivity than their children. This particular result suggests that those few children who reported higher levels of Hyperactivity than their parents were very responsive to therapy. Perhaps these children’s self-awareness of hyperactivity was increased because they were completing the assessment in the context of starting a social competence psychotherapy group, consisting largely of children with ADHD. And perhaps this finding only appears on the Hyperactivity subscale because, of the five subscales examined, it is the most observable and the most likely for which children get frequent feedback from parents and teachers. If children see others in their group who are noticeably hyperactive and often get feedback about the impact of these behaviors on others, they may be more aware of these behaviors in themselves and more apt to endorse them. This awareness, in turn, may increase motivation to change the behavior and thus treatment success. In sum, perhaps a child reporting more Hyperactivity than their parent indicates a greater awareness and concern of one’s behaviors, thus resulting in more engagement in therapy and more therapeutic gains. Conversely, a child reporting less Depression than their parent indicates less perceived distress and in turn results in less engagement in therapy and poorer therapeutic gains.
Limitations and Future Research Directions
Our ability to describe our sample is restricted by our reliance on parent report of diagnosis. A structured diagnostic interview would be ideal but is not practical in a clinical service setting due to the time, resources, and client fees that would be required. Our dependence on parent report is consistent with other studies conducted in clinical service settings (Barrington et al. 2005; Sim et al. 2006). Furthermore, Weisz et al. (2005) state that an acceptable substitute for a clinical diagnosis is the use of a cutoff score on a standardized measure. While this study did not use a cutoff score, the average SSIS and BASC-2 scores reported earlier indicate that our sample demonstrated clinical impairment in social functioning. Finally, we note that in ascertaining diagnoses, we specifically asked parents to indicate diagnoses provided by a pediatrician or mental health professional. Another limitation of our study is that we used the same informant (parent) to assess discrepancy and outcome. This means that any informant biases in assessment of functioning may also exist in their assessment of outcome. Ideally, outcome would have been assessed using additional objective methods, such as observations or computer-based tasks. Additionally, while the matching BASC-2 subscales used to determine parent–child discrepancy assess identical constructs, we note that the items on each subscale are not identically worded. We also note that the primarily Caucasian, high-SES composition of our sample may constrict the generalizability of our results to other clinical populations and service settings. Finally, given that the ABC Model posits that informant discrepancy may in part reflect differing perspectives on what behaviors merit treatment, our study is limited by the fact that we did not directly assess if parents and children differed in their belief that therapy was warranted.
Our study provides evidence that parent–child discrepancy is indeed related to treatment outcome. In turn, the current findings further the research agenda to better understand the impact of informant discrepancies on treatment outcome, in order to ultimately inform the design of effective therapy with children. It is important to note that there is not one cause of informant discrepancy, or one informant to blame (De Los Reyes and Kazdin 2005). The differing perspectives each informant holds provide valuable assessment data (De Los Reyes 2011). Parent–child discrepancy indicates that multiple factors should be closely examined, including family functioning, awareness of problems, motivation to be involved in treatment, and conflicting perspectives. Ignoring parent–child discrepancy and not addressing what is contributing to the discrepancy, such as a lack of parent–child communication or one informant’s perspective that treatment is not needed, may result in missed opportunities to address a problem in the therapeutic environment before it potentially results in diminished treatment success and increased behavioral and emotional difficulties.
Future research should utilize clinician data and objective measures of outcome to examine whether parent–child discrepancy relates to treatment outcome. Also, since teacher report is frequently used in child clinical assessment and provides its own unique perspective and value, future studies should include teacher data (Verhulst et al. 1994). Future studies should also examine the predictors of informant discrepancy using interaction terms to assess discrepancy. The ABC Model posits that one cause of informant discrepancy is differences in perspectives about whether a symptom warrants treatment. Thus, studies should examine parents’ and children’s level of distress for assessed symptoms, their desire to reduce or change these symptoms, and their level of motivation to engage in therapy that addresses these symptoms. Furthermore, future studies should examine ways to address parent–child discrepancy so that it does not hinder treatment success. To this end, studies should examine which treatment content variables (e.g., motivational interviewing, family therapy) and process variables (e.g., child-therapist alliance, parent involvement) lead to greater parent–child agreement, and in turn, greater treatment success.
References
Achenbach, T. M. (2006). As others see us: Clinical and research implications of cross-informant correlations for psychopathology. Current Directions in Psychological Science, 15(2), 94–98.
Achenbach, T. M., McConaughy, S. H., & Howell, C. T. (1987). Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin, 101(2), 213–232.
Achenbach, T. M., & Rescorla, L. (2001). Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families.
Aduen, P., Rich, B. A., Sanchez, L., O’Brien, K., & Alvord, M. K. (2014). Resilience Builder Program therapy addresses core social deficits in youth with high-functioning autism spectrum disorder. Journal of Psychological Abnormalities in Children, 3(2), 1–10.
Alvord, M. K., & Grados, J. J. (2005). Enhancing resilience in children: A proactive approach. Professional Psychology: Research and Practice, 36(3), 238.
Alvord, M. K., & Rich, B. A. (2012). Resilience Builder groups for youth: Practice and research in a private clinical setting. Independent Practitioner, 32, 18–20.
Alvord, M. K., Zucker, B., & Grados, J. J. (2011). Resilience Builder Program for children and adolescents: Enhancing social competence and self-regulation—a cognitive–behavioral group approach.. Champaign, IL: Research Press.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Baldwin, J. S., & Dadds, M. R. (2007). Reliability and validity of parent and child versions of the multidimensional anxiety scale for children in community samples. Journal of the American Academy of Child & Adolescent Psychiatry, 46(2), 252–260.
Barrington, J., Prior, M., Richardson, M., & Allen, K. (2005). Effectiveness of CBT versus standard treatment for childhood anxiety disorders in a community clinic setting. Behaviour Change, 22(1), 29–43.
Becker, E. M., Jensen-Doss, A., Kendall, P. C., Birmaher, B., & Ginsburg, G. S. (2016). All anxiety is not created equal: Correlates of parent/youth agreement vary across subtypes of anxiety. Journal of Psychopathology and Behavioral Assessment, 38(4), 528–537.
Becker-Haimes, E. M., Jensen-Doss, A., Birmaher, B., Kendall, P. C., & Ginsburg, G. S. (2017). Parent–youth informant disagreement: Implications for youth anxiety treatment. Clinical Child Psychology and Psychiatry, doi:1359104516689586.
Boulet, J., & Boss, M. W. (1991). Reliability and validity of the brief symptom inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 3(3), 433.
Brookman-Frazee, L., Haine, R. A., Gabayan, E. N., & Garland, A. F. (2008). Predicting frequency of treatment visits in community-based youth psychotherapy. Psychological Services, 5(2), 126–138.
Comer, J. S., & Kendall, P. C. (2004). A symptom-level examination of parent–child agreement in the diagnosis of anxious youths. Journal of the American Academy of Child & Adolescent Psychiatry, 43(7), 878–886.
Crawford, A. M., & Manassis, K. (2001). Familial predictors of treatment outcome in childhood anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 40(10), 1182–1189.
De Los Reyes, A. (2011). Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child and Adolescent Psychology, 40(1), 1–9.
De Los Reyes, Alfano, C., & Beidel, D. (2010). The relations among measurements of informant discrepancies within a multisite trial of treatments for childhood social phobia. Journal of Abnormal Child Psychology, 38(3), 395–404.
De Los Reyes, A., Augenstein, T. M., Wang, M., Thomas, S. A., Drabick, D. A. G., Burgers, D. & Rabinowitz, J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141. Advance online publication.
De Los Reyes, A., Goodman, K. L., Kliewer, W., & Reid-Quinones, K. (2008). Whose depression relates to discrepancies? Testing relations between informant characteristics and informant discrepancies from both informants’ perspectives. Psychological Assessment, 20(2), 139–149.
De Los Reyes, A., & Kazdin, A. E. (2004). Measuring informant discrepancies in clinical child research. Psychological Assessment, 16, 330–334.
De Los Reyes, A., & Kazdin, A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509.
De Los Reyes, A., & Kazdin, A. E. (2006). Informant discrepancies in assessing child dysfunction relate to dysfunction within mother–child interactions. Journal of Child and Family Studies, 15(5), 643–661.
De Los Reyes, A. & Ohannessian, C. M. (2016). Introduction to the special issue: Discrepancies in adolescent–parent perceptions of the family and adolescent adjustment. Journal of Youth and Adolescence. https://doi.org/10.1007/s10964-016-0533-z.
De Los Reyes, A., Salas, S., Menzer, M. M., & Daruwala, S. E. (2013a). Criterion validity of interpreting scores from multi-informant statistical interactions as measures of informant discrepancies in psychological assessments of children and adolescents. Psychological Assessment, 25, 509–519.
De Los Reyes, A., Thomas, S. A., Goodman, K. L., & Kundey, S. M. A. (2013b). Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology, 9, 123–149.
De Los Reyes, A., Youngstrom, E. A., Pabón, S. C., Youngstroma, J. K., Feeny, N. C., & Findling, R. L. (2011). Internal consistency and associated characteristics of informant discrepancies in clinic referred youths age 11 to 17 years. Journal of Clinical Child & Adolescent Psychology, 40(1), 36–53.
Derogatis, L. R., & Melisaratos, N. (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 3, 595–605.
Eisen, S. V., Ranganathan, G., Seal, P., & Spiro, III, A. (2007). Measuring clinically meaningful change following mental health treatment. The Journal of Behavioral Health Service & Research, 34, 272–289.
Elliott, S. N., Gresham, F. M., Frank, J. L., & Beddow, P. A. (2008). Intervention validity of social behavior rating scales: Features of assessments that link results to treatment plans. Behavior Modification, 34, 15–24.
Epstein, N. B., Baldwin, L. M., & Bishop, D. S. (1983). The McMaster Family Assessment Device. Journal of Marital and Family Therapy, 9(2), 171–180.
Erdlen, R. J. J., & Rickrode, M. R. (2007). Social skills groups with youth: A cognitive behavioral perspective. In R. W. Christner, J. L. Stewart, A. Freeman, R. W. Christner, J. L. Stewart, & A. Freeman (Eds.), Handbook of cognitive-behavior group therapy with children and adolescents: Specific settings and presenting problems (pp. 485–506). New York: Routledge/Taylor & Francis.
Ferdinand, R. F., van der Ende, J., & Verhulst, F. C. (2004). Parent–adolescent disagreement regarding psychopathology in adolescents from the general population as a risk factor for adverse outcome. Journal of Abnormal Psychology, 113(2), 198–206.
Fjermestad, K. W., Lerner, M. D., McLeod, B. D., Wergeland, G. J. H., Heiervang, E. R., Silverman, W. K., Öst, L.-G., De Los Reyes, A., Havik, O. E., & Haugland, B. S. M. (2016). Therapist–youth agreement on alliance change predicts long-term outcome in CBT for anxiety disorders. Journal of Child Psychology and Psychiatry, 57, 625–632.
Garland, A. F., Haine, R. A., & Boxmeyer, C. L. (2007). Determinates of youth and parent satisfaction in usual care psychotherapy. Evaluation and Program Planning, 30(1), 45–54.
Grills, A. E., & Ollendick, T. H. (2003). Multiple informant agreement and the anxiety disorders interview schedule for parents and children. Journal of the American Academy of Child & Adolescent Psychiatry, 42(1), 30–40.
Guion, K., Mrug, S., & Windle, M. (2009). Predictive value of informant discrepancies in reports of parenting: Relations to early adolescents’ adjustment. Journal of Abnormal Child Psychology, 37, 17–30.
Hoffman, L. J., & Chu, B. C. (2015). Target problem (mis) matching: Predictors and consequences of parent-youth agreement in a sample of anxious youth. Journal of Anxiety Disorders, 31, 11–19.
Hoza, B., Pelham, Jr, W. E., Dobbs, J., Owens, J. S., & Pillow, D. R. (2002). Do boys with attention-deficit/hyperactivity disorder have positive illusory self-concepts? Journal of Abnormal Psychology, 111(2), 268.
Hoza, B., Vaughn, A., Waschbusch, D. A., Murray-Close, D., & McCabe, G. (2012). Can children with ADHD be motivated to reduce bias in self-reports of competence? Journal of Consulting & Clinical Psychology, 80, 245–254.
Humphreys, K. L., Weems, C. F., & Scheeringa, M. S. (2015). The role of anxiety control and treatment implications of informant agreement on child PTSD symptoms. Journal of Clinical Child & Adolescent Psychology, 46(6), 903–914.
Hymel, S., Bowker, A., & Woody, E. (1993). Aggressive versus withdrawn unpopular children: Variations in peer and self-perceptions in multiple domains. Child Development, 64(3), 879–896.
Israel, P., Thomsen, P. H., Langeveld, J. H., & Stormark, K. M. (2007). Parent–youth discrepancy in the assessment and treatment of youth in usual clinical care setting: Consequences to parent involvement. European Child & Adolescent Psychiatry, 16(2), 138–148.
Kabacoff, R. I., Miller, I. W., Bishop, D. S., Epstein, N. B., & Keitner, G. I. (1990). A psychometric study of the McMaster family assessment device in psychiatric, medical, and nonclinical samples. Journal of Family Psychology, 3(4), 431.
Kazdin, A. E. (2000). Psychotherapy for children and adolescents: Directions for research and practice. Oxford: Oxford University Press.
Kolko, D. J., & Kazdin, A. E. (1993). Emotional/behavioral problems in clinic and nonclinic children: Correspondence among child, parent and teacher reports. Journal of Child Psychology and Psychiatry, 34(6), 991–1006.
Laird, R. D., & Weems, C. F. (2011). The equivalence of regression models using difference scores and models using separate scores for each informant: implications for the study of informant discrepancies. Psychological Assessment, 23(2), 388.
Laird, R. D., & De Los Reyes, A. (2013). Testing informant discrepancies as predictors of early adolescent psychopathology: Why difference scores cannot tell you what you want to know and how polynomial regression may. Journal of Abnormal Child Psychology, 41(1), 1–14.
Nolen-Hoeksema, S. (2001). Gender differences in depression. Current directions in psychological science, 10(5), 173–176.
Owens, J. S., Goldfine, M. E., Evangelista, N. M., Hoza, B., & Kaiser, N. M. (2007). A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clinical Child and Family Psychology Review, 10(4), 335–351.
Panichelli-Mindel, S. M., Flannery-Schroeder, E., Kendall, P. C., & Angelosante, A. G. (2005). Disclosure of distress among anxiety-disordered youth: Differences in treatment outcome. Journal of Anxiety Disorders, 19(4), 403–422.
Phares, V., & Danforth, J. S. (1994). Adolescents’, parents’, and teachers’ distress over adolescents’ behavior. Journal of Abnormal Child Psychology, 22(6), 721–732.
Reynolds, C. R., & Kamphaus, R. W. (2004). BASC 2: Behavioral Assessment System for Children Manual (2nd ed.). Circle Pines, MN: American Guidance Service, Inc.
Richters, J. E. (1992). Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin, 112(3), 485.
Rich, B. A., Hensler, M. A., Rosen, H. R., Watson, C., Schmidt, J., Sanchez, L., O’Brien, K., & Alvord, M. K. (2014). Attrition from therapy effectiveness research among youth in a clinical service setting. Administration and Policy in Mental Health and Mental Health Services Research, 41, 343–352.
Rich, B. A., Nigro, C., Watson, C., Rosen, H. R., Sanchez, L., O’Brien, K., & Alvord, M. K. (2017). Improved functioning in children with attention deficit hyperactivity disorder following treatment with the Resilience Builder Program ® in a clinical service setting. Manuscript submitted for publication.
Schmidt, F. L., & Hunter, J. E. (1996). Measurement error in psychological research: Lessons from 26 research scenarios. Psychological Methods, 1(2), 199.
Sim, L., Whiteside, S. P., Dittner, C. A., & Mellon, M. (2006). Effectiveness of a social skills training program with school age children: Transition to the clinical setting. Journal of Child and Family Studies, 15(4), 408–417.
Treutler, C. M., & Epkins, C. C. (2003). Are discrepancies among child, mother, and father reports on children’s behavior related to parents’ psychological symptoms and aspects of parent–child relationships? Journal of Abnormal Child Psychology: An Official Publication of the International Society for Research in Child and Adolescent Psychopathology, 31(1), 13–27.
Tversky, B., & Marsh, E. J. (2000). Biased retellings of events yield biased memories. Cognitive Psychology, 40(1), 1–38.
Van Roy, B., Groholt, B., Heyerdahl, S., & Clench-Aas, J. (2010). Understanding discrepancies in parentchild reporting of emotional and behavioural problems: Effects of relational and socio-demographic factors. BMC Psychiatry, 10(1), 56.
Verhulst, F. C., Koot, H. M., & Van der Ende, J. (1994). Differential predictive value of parents’ and teachers’ reports of children’s problem behaviors: A longitudinal study. Journal of Abnormal Child Psychology, 22(5), 531–546.
Walden, T. A., Harris, V. S., & Catron, T. F. (2003). How I feel: A self-report measure of emotional arousal and regulation for children. Psychological Assessment, 15(3), 399.
Watson, C., Rich, B. A., Sanchez, L., O’Brien, K., & Alvord, M. K. (2014). Preliminary study of resilience-based group therapy for improving the functioning of anxious children. Child and Youth Care Forum, 43, 269–286.
Weisz, J. R., Doss, A. J., & Hawley, K. M. (2005). Youth psychotherapy outcome research: A review and critique of the evidence base. Annual Review of Psychology, 56, 337–363.
Whisman, M. A., & McClelland, G. H. (2005). Designing, testing, and interpreting interactions and moderator effects in family research. Journal of Family Psychology, 19(1), 111–120.
Williams, N. A., Coday, M., Somes, G., Tylavsky, F. A., Richey, P. A., & Hare, M. (2010). Risk factors for poor attendance in a family-based pediatric obesity intervention program for young children. Journal of Developmental and Behavioral Pediatrics, 31(9), 705.
Yeh, M., & Weisz, J. R. (2001). Why are we here at the clinic? Parent–child (dis)agreement on referral problems at outpatient treatment entry. Journal of Consulting and Clinical Psychology, 69(6), 1018–1025.
Youngstrom, E., Loeber, R., & Stouthamer-Loeber, M. (2000). Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. Journal of Consulting and Clinical Psychology, 68(6), 1038.
Author Contributions
J.G.: designed and executed the study, directed data analyses, and wrote the paper. B.A.R.: directed the study, assisted with data analysis, and assisted in writing the paper. B.H.: assisted with data analysis and writing the paper. S.H.: assisted with writing the paper. L.B.: assisted with study execution and writing the paper. A.D.L.R.: assisted with data analysis and writing the paper. M.K.A.: assisted with study execution and writing the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
This study complies with the Committee on Publication Ethics (COPE) guidelines. The authors have no potential conflicts of interest.
Ethical Approval
The research was approved by the Institutional Review Board at the Catholic University of America and met all standards for the protection of human participants.
Informed Consent
All participants provided consent and assent.
Rights and permissions
About this article
Cite this article
Goolsby, J., Rich, B.A., Hinnant, B. et al. Parent–Child Informant Discrepancy is Associated with Poorer Treatment Outcome. J Child Fam Stud 27, 1228–1241 (2018). https://doi.org/10.1007/s10826-017-0946-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-017-0946-7