Abstract
This systematic review evaluates the efficacy of parenting interventions on parent, infant and parent-infant relationship outcome measures for parents of infants under 12 months old. Parent outcomes examined included competence, and confidence; baby outcomes included infant behaviours of crying, settling, and sleeping problems and parent-infant relationship outcomes included parental responsiveness. Systematic searches of five databases were carried out. In total, 36 randomised controlled trials over the past 35 years were included in the meta-analyses, with a total of 4880 participants. Interventions were carried out either during pregnancy or within the first 12 months after birth and involved teaching specific strategies and provision of information on infant development and behaviour. Mean effect sizes were obtained using a structural equation modelling (SEM) approach to meta-analysis. Heterogeneity was found on parent responsiveness and infant sleep. Potential moderator variables were assessed for these two outcomes using the SEM approach. Results showed that early parenting interventions are effective in improving parental responsiveness (d = 0.77), and improving or preventing infant sleep problems (d = 0.24), but not crying problems (d = 0.27) possibly due to low power. No conclusions could be drawn in regards to parental competence or confidence. Moderator analysis showed that for interventions aimed at improving responsiveness, briefer interventions were more effective than longer ones; and studies published more recently reported smaller effects than older studies. No other moderators influenced the assessed intervention outcomes. The findings of this study provide further evidence for the positive effects of early parenting interventions for infants under 12 months of age, however future research is needed to assess intervention effects on parental competence and confidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The early months of a baby’s life and family formation are vitally important for infant mental health and development. The parent-child relationship has a pervasive influence on the psychological, physical, social and emotional wellbeing of children from birth onwards (Murray et al. 1996). Critical to the infant’s wellbeing is the environment into which they are born, and in particular parenting has been identified as impacting on every aspect of development (Schulz et al. 2006).
The transition to parenthood is associated with many positive experiences, yet also poses numerous challenges and demands. Parents often experience sleep deprivation, difficulties developing confidence and effective parenting skills, a decline in the couple relationship and increased conflict, and increases in psychological distress such as postnatal depression (Feeney et al. 2001). Although many of the challenges form part of a normal transition to parenthood and may decline over time without intervention, continuing and elevated levels of parental distress have been associated with long-term negative effects on parent mental health and child development (Kingston et al. 2012).
Infant behaviours such as excessive crying, fussing and sleeping problems are found in approximately 20% of all children and are the most common complaints for which parents seek professional help (Hemmi et al. 2001; Wolke et al. 2002). Infants referred for persistent crying problems and associated sleeping or feeding problems are at increased risk for developing more severe problems later in childhood including ADHD, conduct problems, negative emotionality and academic difficulties (Hemmi et al. 2001; Wolke et al. 2002). While crying and sleep behaviour problems are developmentally normative, if parents do not have effective strategies for settling their baby, establishing good sleep routines and gradually teaching their baby to self-soothe, it can lead to ongoing adjustment problems for the baby.
Factors that have been shown to contribute to positive infant outcomes include parental responsiveness, parental confidence and competence (Smith et al. 2006). Parental responsiveness, also often called sensitivity, refers to parents’ ability to recognise infants’ cues and appropriately respond or act on those cues (Karl 1995). It is an important factor in the development and promotion of secure mother-infant attachment (De Wolff and van IJzendoorn 1997; Raval et al. 2001). By sensitively responding to the infant’s signals, the parent develops a secure relationship with the baby (De Wolff and van IJzendoorn) and high levels of responsiveness have been linked to fewer crying problems (Bell and Ainsworth 1972). In contrast, low maternal responsiveness has been found to be a risk factor for sleep disorders in infants (Priddis 2009), thus demonstrating the importance of responsiveness in infant sleep as well as crying problems.
Parental confidence or self-efficacy, terms that are often used interchangeably, refer to one’s belief of being able to perform parenting tasks competently and effectively (Teti and Gelfand 1991). Parental self-efficacy has been associated with responsive and stimulating caretaking, and the ability to understand and respond to infant signals (Coleman and Karraker 1997). Increased sense of efficacy may also be linked to better infant sleep (Wolfson et al. 1992) and maternal responsiveness (Bohlin and Hagekull 1987). Therefore, it is an important factor in new parent’s adjustment to parenthood (Jones and Prinz 2005). Parental competence refers to the parent’s ability or skills to adapt their behaviour in ways that meets their infant’s needs (Hamilton-Dodd et al. 1989). Higher parental competence has been associated with lower parenting stress during newborn care, lower levels of baby blues and depressive symptoms (Denis et al. 2012; Liu et al. 2011) and higher infant soothability at five months of age (Leerkes and Crockenberg 2002). Therefore, responsiveness, confidence and competence play a major role in influencing both sleep and crying in babies, the two most commonly reported baby behaviour concerns.
Four previous reviews have summarised the effects of parenting interventions on a variety of parent and infant outcomes relevant to this study. Pinquart and Teubert’s (2010) meta-analysis integrated the effects of 142 randomised controlled trials (RCTs) of interventions promoting positive and effective parenting at the transition to parenthood that started either during pregnancy or the first six months post birth. Parenting interventions were defined as educating new parents in parenting skills, coping with stressors, promoting positive interactions between partners and stimulating child development. Interventions had very small to small positive effects on parenting quality, parental stress, reduced child abuse, health promoting behaviours of parents, and cognitive, social and motor development, infant and parent mental health, and couple adjustment. However, parenting quality or ability is a very broad construct and the authors did not specify which particular aspect of parenting quality was improved through parenting interventions. In addition, because of the broad definition of parenting intervention, there was considerable variety in the characteristics of the included interventions. All were educational but without an explicit skills training component, and each aimed to improve a different outcome. This could explain the small or very small effects they found.
Another meta-analysis investigated the effects of 77 preventative interventions aimed at enhancing parental sensitivity and infant attachment security that started before the child turned four and a half years (Bakermans-Kranenburg et al. 2003). Results showed that interventions were effective in improving parental responsiveness and infant attachment security. This review included families at risk of developing problems or already experiencing difficulties in parenting and included families varying in risk status. The review also included interventions with children aged up to four and a half years of age, thus it is unclear whether parenting interventions specifically for parents of babies (below 12 months of age) would improve parental sensitivity. Finally, their results showed that effects in RCTs were significantly smaller than those in non-randomised trials.
A systematic review by Douglas and Hill (2013) analysed the effects of 43 behavioural interventions for infant sleep and crying when conducted in the first six months of life and found no improvements, claiming that studies that do find an effect are methodologically flawed. However, the review itself has limitations in that it did not conduct any statistical analyses (e.g., meta-analysis), included non-RCTs, and two RCTs which did not even assess a parenting intervention. Contrary to this, another review by Bryanton and Beck (2010) assessed the effectiveness of 25 educational interventions for parents of infants in the first eight weeks post birth and only included RCTs. Results showed that educational interventions that were aimed at sleep enhancement increased the amount of infant sleep, and education about infant behaviour increased maternal knowledge of infant behaviour. Due to heterogeneity issues, outcomes on infant growth and development, crying, infant preventative care, maternal/ paternal infant care competency and confidence, parent-infant interactions could not be meta-analytically analysed. Further, the number of identified trials for each outcome was small and the review limited the included interventions to a very narrow window of only eight weeks post birth. Given the mixed findings, considerable heterogeneity in the included studies and limitations of the previous reviews, the effects of parenting interventions on parenting (responsiveness, confidence and competence) and baby outcomes (sleep and crying) remain unclear and we do not know the extent to which these outcomes may be modified by parenting programs in babies under 12 months of age.
A new approach is required which can disentangle the effectiveness of parenting interventions for parents of infants for each specific outcome for parents and their babies. We also need to learn what aspects of the interventions itself makes an intervention effective and how the study designs can impact on this effectiveness. Given the volume of work conducted in this area, and the clear limitations in the effectiveness of interventions to date, it becomes critical to have clear evidence relating to specific parenting and infant behaviours in order to develop more effective approaches. The previous reviews have provided a starting point suggesting that interventions for parents of infants can be effective, but this current review takes it the next step further by selecting the specific parenting outcomes of confidence and competence rather than just parenting quality, as well as responsiveness; specifying the age group of infants to younger than 12 months as infant development and behaviour is quite different from before and after one year of age (James-Roberts and Plewis 1996); and finally extending the review of parenting interventions on infant crying and sleeping by choosing RCTs only (for higher study quality) and including studies that go beyond eight weeks post birth.
Previous reviews of parenting interventions for parents of infants have shown positive effects on a range of parent and child outcomes. However, the size of these effects can vary depending on several study, intervention and participant characteristics (Pinquart and Teubert 2010). It is important to investigate what makes interventions more or less effective in order to make evidence based program recommendations. We chose to focus on the following moderators based on those that have been assessed in previous reviews (Bakermans-Kranenburg et al. 2003; Pinquart and Teubert 2010). This study used all of the following moderators except for staff qualification (reason outlined at the end of the Method section).
One moderator is the onset of an intervention. Interventions aimed at preventing parenting and child problems should ideally start before any significant problems occur (Heinicke et al. 1988). Pinquart and Teubert (2010) did not find significant variation in effect sizes between prenatal and postnatal interventions other than for infant cognitive development, for which postnatal interventions were more effective. Contrarily, Bakermans-Kranenburg et al. (2003) found that interventions starting later were more effective than prenatal or early postnatal interventions in improving parental responsiveness.
The length of the intervention and number of sessions can also impact results. It is often assumed that more intensive interventions result in larger effects (Pinquart and Teubert 2010); however, it appears that beyond a certain threshold, longer interventions may not contribute to any further effects. Pinquart and Teubert found that interventions lasting between three and six months tended to have the largest effects on parenting, followed by shorter interventions and then longer interventions. Similarly, Bakermans-Kranenburg et al. (2003) found that shorter interventions showed larger effects on parental sensitivity than longer interventions.
Another moderator is the place of intervention delivery. Interventions conducted in parents’ homes might be more effective than those conducted in the community, in particular postnatal interventions, as parents with a new baby might experience fewer barriers to participation. This can decrease participant attrition and ensure delivery of adequate intervention dose. However, Bakermans-Kranenburg et al. (2003) found no difference between interventions conducted at home to interventions conducted elsewhere in regards to responsiveness.
The format of the intervention delivery is a further factor. A variety of delivery modalities are available (e.g., individual, group, self-directed) and given the demands on parents of babies it is important to consider the most efficient and effective ways of program delivery. Pinquart and Teubert (2010) found weaker effects on child social development for interventions held in group format, but they found opposite results on parental health promoting behaviours.
Staff qualification can affect intervention results as well. Pinquart and Teubert (2010) found stronger effects for interventions led by child mental health professionals than interventions led by lay persons, possibly because professionals (e.g., psychologists, nurses) may have better skills in interacting with families and delivering an intervention compared to lay persons.
The risk status of the participants is also important. Families experiencing a number of risk factors may be more likely to benefit from parenting interventions than those with fewer risk factors (Pinquart and Teubert 2010). Bakermans-Kranenburg et al. (2003) found no association between a variety of risk factors and intervention outcomes, except for interventions that were conducted with clinically referred samples, which were more effective than those with non-clinical samples. Pinquart and Teubert (2010) did not find any significant results of risk factors influencing intervention effects.
Another moderator is the year of study publication. Pinquart and Teubert (2010) found that more recent studies had weaker effects compared to older studies on some outcomes. This may be due to the increasing amount of parenting information that is now freely available.
Finally, the study quality affects outcomes. Bakermans-Kranenburg et al. (2003) found that RCTs had smaller effects compared to non-RCTs, indicating that the study design can influence outcomes, possibly because of better control of extraneous variables that can impact the results.
While there appears to be support for the effectiveness of parenting interventions on a variety of parent and infant outcomes, previous meta-analyses used very broad definitions of parenting interventions, or been very restrictive in outcomes assessed or intervention delivery. Thus, previous reviews have not assessed the effects of parenting interventions on parental responsiveness specifically for infants under 12 months of age, despite the clear importance of responsiveness in this age group. Nor have they investigated outcomes on parent confidence and competence, which are crucial to infant development. While Pinquart and Teubert (2010) conducted a review on parenting interventions, the parenting outcomes examined are very broad and were not clearly defined (i.e. parenting quality), we don’t yet know what aspects of parenting this referred to. There is also conflicting and lacking knowledge on the effects of interventions in improving infant sleep and crying problems due to significant limitations in the design of previous reviews. Therefore, substantial gaps remain in our understanding of parenting interventions for parents of infants, including knowledge about key factors identified in the theoretical and empirical literature as being critical to infant development (Coleman and Karraker 1997; Leerkes and Crockenberg 2002; Raval et al. 2001) as well as infant behaviours commonly seen as problematic by parents (Hemmi et al. 2001).
A new review on the specific parenting outcomes is needed to clarify which interventions are effective for new parents, and what factors make them more or less effective. This is required so that future parenting interventions can be developed in the most effective way. Therefore, we investigated the effects of interventions on parenting competence and confidence in addition to parent responsiveness and infant behaviours. Specifically, this review aimed to estimate the effects of interventions intended to help parents through the transition to parenthood on these outcomes by including RCTs only and overcoming methodological limitations of previous reviews. Non-random studies are more susceptible to inflated effects whereas RCTs provide a better control of the effects of extraneous variables. This aids in pinpointing whether effects are actually due to the intervention. Our first goal was to separately assess intervention outcomes on parental responsiveness, confidence, and competence due to their inherent importance in influencing baby development and behaviour, and infant crying and sleeping as the most commonly identified baby outcomes (Hemmi et al. 2001; Wolke et al. 2002). Second, we aimed to identify moderators of intervention outcomes to find out which interventions are most beneficial to families. We performed a series of meta-analyses to provide a more comprehensive understanding of the effects of parenting interventions in improving parenting outcomes and thus preventing or treating infant behaviour problems.
Method
Search Strategy
This review focused on interventions aimed at enhancing positive parenting skills in order to improve parent and child outcomes. Outcome variables were parental responsiveness, infant sleep and crying behaviours, and parental confidence and competence. Studies were systematically identified in electronic databases (PsycInfo, Medline, Cinahl, Scopus and Cochrane Library). An extensive and broad range of search terms was used to obtain a large sample of studies encompassing a wide variety of interventions and outcomes. Search terms included: (Baby OR parent* OR “expect* parent*” OR infant* OR pregnan* OR “first baby” OR maternal OR antenatal OR postnatal OR prenatal OR postpartum OR newborn) AND (training OR program* OR intervention OR *education* OR “parent effectiveness training”) AND (“baby behavio*” OR “infant behavio*” OR settl* OR cry* OR sleep* OR feed* OR responsiveness OR bond* OR sensitiv* OR competence OR confidence OR self-efficacy OR expectation OR attitudes). An asterisk indicates that the search contained but was not limited to that word or word fragment and quotation marks limited the searches to the word phrases. Cross-referencing and forward searching was completed on identified full-text articles with an additional four eligible articles identified. No earliest time limit was specified and studies up until February 2016 were identified. Searches limited studies to those in the English language.
Included studies needed to meet the following criteria: (a) evaluation of a parenting intervention that teaches parenting skills and includes an educational component, (b) randomized controlled trial, (c) the onset of the intervention was either during pregnancy or the first 12 months post birth, and (d) assessed parental responsiveness, confidence, or competence; or baby sleep and crying behaviours. Studies were excluded if: (a) programs did not target the improvement of parenting skills (e.g., programs primarily focusing on the couple relationship or parent mental health), (b) programs focusing exclusively on treatment or prevention of psychological disorders (including Shaken Baby Syndrome) or exclusively assessing outcomes on child cognitive, motor and social development and health, (c) onset of intervention was more than 12 months after childbirth or if the mean age of all infants at onset was above 12 months, (d) parents or infants with a physical or mental disability, (e) assessed interventions on preterm infants, low birth weight infants or infants in the neonatal intensive care unit, (f) interventions focused on improving breastfeeding, (g) interventions exclusively evaluating single strategies or techniques (e.g., kangaroo care, massage, controlled crying, Brazelton Neonatal Behavioural Assessment Scale).
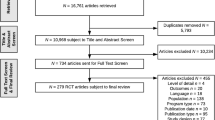
Figure 1 shows the flow diagram of the search strategy. The search identified 62 relevant papers of which 28 were excluded from the meta-analyses because they did not meet the inclusion criteria. Reasons for excluding these studies were: (a) studies were not available in English (N = 3), (b) the intervention started (for the majority of participants) when infants were older than 12 months (N = 7), (c) the study was not an RCT (N = 8), (d) intervention focused on assessing single strategies or techniques (N = 2), (e) intervention targeted couple relationship or parental mental health (N = 2), (f) intervention was not for parents but for health care providers (N = 2), (g) did not assess relevant outcome measures or did not report relevant results (N = 2) and (h) the publication duplicated results published in another paper already included in this study (N = 2). Overall, 34 eligible studies were included assessing the outcomes of parental responsiveness (N = 16), infant crying (N = 8) and sleeping behaviours (N = 13) and confidence and competence (N = 4) of parents. An updated search was conducted prior to finalisation of the manuscript for publication (February 2016) and two new eligible studies (assessing parental responsiveness) were found and added to the meta-analysis. The full search yield was reviewed for inclusion by the first author on the basis of title, abstract and full text. The second author reviewed full text articles to ensure adherence to the inclusion criteria. Discrepancies were resolved through discussion.
Prisma flow chart describing identification and selection of studies for inclusion in the meta-analysis, adapted from Moher et al. (2009)
Data Extraction
The following variables were extracted: year of publication, country in which the intervention was carried out, total number of participants and those allocated to intervention and control groups, sample characteristics (i.e. participating parent, age of parent and baby), outcome variable measurement, risk status (universal vs. risk), length of intervention in weeks, number of sessions, place of intervention delivery (home vs hospital vs community), onset of intervention (prenatal vs postnatal), format of intervention (individual, group or self-directed) and qualification of staff who delivered the intervention (professional vs non-professional).
Study Quality
All studies were assessed for quality using the PEDro scale (“PEDro scale 2016”), which is an 11 item scale designed for rating methodological quality of RCTs. Criteria 2 to 9 refer to the internal validity and criteria 10 and 11 rate the sufficiency of provided statistical information to make results interpretable. The range of possible scores is 0 to 11, with higher numbers indicating better quality. None of the studies used blinding of subjects (item 5) or blinding of therapists who administered the therapy (item 6), both of which are rarely possible to achieve in psychological interventions for practical and ethical reasons. The highest possible rating was therefore 9. Trials in this study scored between 4 and 9 points on the PEDro scale as shown in Table 1. Overall, included studies scored on average 6.5 points.
Effect Size Calculation
Results of each study were extracted from a variety of statistical outcomes, which in most cases were means and standard deviations. When those were not available even after approaching the authors of the papers, we used the F statistic, t statistic, chi-squared statistic and probability values to calculate the standardized mean difference, d, for post intervention scores. In some cases, papers only reported that the results were significant or non-significant. Non-significant results (N = 3) were coded as having an effect size of .01. For significant results (N = 1), we used probability of .05 in order to calculate the effect size (as suggested by Card 2012). We have conducted sensitivity analyses by using the effect size of 0.1 and 0.2 for the non-significant results and .01 for the significant result, but the overall results were consistent, thus the results are robust to the imputations of the missing effect sizes. Effect sizes can be interpreted using Cohen’s (1992) guidelines (small = .2; moderate = .5; large = .8).
Effect sizes were calculated for each outcome variable. Baseline results were not included as these were not available for several studies where interventions started during pregnancy. Where papers reported results from multiple measures of the same outcome variable, for example if sleep outcomes in infants were assessed in total minutes of sleep and number of awakenings at nights, we averaged the effect sizes (according to Card 2012). This way each paper contributed one effect size per outcome variable where relevant. When results of the outcomes were assessed at multiple time points (e.g., post and follow-up), we only used post assessment results, because in some cases follow-up results were only a few weeks after the post results and there were not enough studies available to investigate follow-up results separately. Calculation of d included a correction for biases when sample sizes were small (less than 30; N = 9) by using the following formula: d = (1- (3/ 4N-9)*d (Wilson 2011).
Computation and Testing of Effect Sizes
We applied an SEM approach to meta-analysis by Cheung (2008) in Mplus v.7.1 (Muthén and Muthén 1998–2011) to compute and test the effect sizes. Calculations were performed by employing a mixed-effects model to obtain mean effect sizes and to evaluate moderating effects. Three separate SEM meta-analyses were conducted for parent responsiveness, infant crying and infant sleeping. We did not conduct a meta-analysis for parent confidence (N = 4) or competence (N = 1) due to small n. Computation of the overall effect size per outcome was based on a weighted average of the effect sizes using a random-effects model. A random effects model is recommended when the effect sizes vary between studies and not all sources of heterogeneity can be identified (Card 2012).
To examine if there was significant variation between studies, the Q-test for heterogeneity was computed (Hedges and Olkin 1985). A significant Q statistic indicates that there is significant variability amongst effect sizes in the sample of studies. It follows the chi square distribution with degrees of freedom calculated as the number of studies minus 1. Therefore, the significance of the Q statistic depends on its value relative to degrees of freedom (Hedges and Olkin 1985). Further, the I 2 index was computed to provide a measure of the degree of heterogeneity. This index is interpreted as the percentage of variability among effect sizes that exists between studies relative to the total variability among effect sizes. The I 2 index can be interpreted as follows: 0% indicates no variability, i.e. homogeneity; 25% indicates small heterogeneity; 50% indicates medium heterogeneity and 75% is considered as large heterogeneity (Higgins et al. 2003).
Moderators used for analyses included: year (continuous), risk status (categorical: universal or risk), number of sessions (1 missing data point; continuous), length of intervention in weeks (continuous; 2 missing data points); onset of the intervention (categorical: prenatal or postnatal), place where the intervention was conducted (2 missing data points; categorical: home, or hospital/ community setting), quality of the study (continuous using the PEDro scale) and intervention format. Format was categorical with three categories (delivered individually, in group, or self-directed), thus it was dummy coded in order to be correctly used as a moderating variable for the baby sleep outcome. The moderating effect of staff qualification was not assessed due to lack of variability (only professionals delivered the program, except for one study, which used a lay person).
Results
Study Characteristics
The 36 papers included in the three meta-analyses documented the results of 35 different parenting interventions for parents of infants (See Table 2 for characteristics). All trials were published in peer-reviewed journals between 1982 and 2014. A total of 4880 families participated in the interventions (2471 in the intervention and 2408 in the control group). In the majority of trials, only the mother participated (N = 26), in six trials the father participated as well, and in two trials only fathers participated. The parents were on average 28 years old (SD = 4.14).
Fifteen trials included families without any risk factors and 21 trials selected participants based on a range of risk factors including low education or income, psychosocial or depressive risk, infants with colic, infants with or at risk of developing a sleeping problem, and parents with an insensitive parenting style. Most interventions were conducted postnatally (N = 26), seven commenced during pregnancy but continued postnatally and one intervention was conducted exclusively during pregnancy.
Eighteen studies aimed to improve parental responsiveness. Of those, an average of 10 sessions (range = 1–43) were conducted over an average length of 16 weeks (range = 1–56). Interventions were delivered in participants’ home (N = 11) or in hospital (N = 6), with one study not reporting place of delivery. The format was either individual consultations (N = 14) or group sessions (N = 4). Eight trials aimed to reduce infant crying with an average of 2.25 sessions (range = 1–5), mostly conducted weekly. Interventions were delivered in participants’ home (N = 5) or in hospital (N = 3). The format was either individual consultations (N = 4) or self-directed (N = 4). Fourteen studies reported on thirteen trials aimed to improve infant sleep with an average of 2.5 sessions (range = 1–6) conducted over an average of 11.4 weeks (range = 3–26; Sleep et al. 2002, and St James-Roberts et al. 2001, reported results of the same trial). Interventions were delivered in participants’ home (N = 5) or in hospital (N = 6). The format was either individual consultation (N = 9), group (N = 1) or self-directed (N = 3). Confidence was assessed in four studies and competence was assessed in one study.
Measures
Responsiveness was assessed using observational measures for all studies, in which the mother-infant interactions were observed in the home environment. Parents were asked to behave as they normally do with their infant in daily interactions, and data were coded for responsiveness and sensitivity to infant distress and social signals, and anticipation of infant’s needs. Infant crying and sleep was predominantly assessed using behaviour diaries that parents completed generally for a 24 or 48 h period. Other measurements included asking participants whether the infant sleep was considered a problem over the past 2 weeks, standardized interview schedules assessing settling difficulties and night waking, and actigraphy on the infant’s ankle. Confidence and competence was assessed using self-report questionnaires. Table 2 shows the type of measures for each study.
Types of Interventions
Interventions were grouped based on the outcome of interest (see Table 2). Interventions aimed at improving parental responsiveness employed a range of techniques and strategies, though all of them based their interventions on some form of attachment-based and/or cognitive-behavioural models. Interventions commonly discussed the importance of responsiveness and encouraged contingent responding to the infant as well as used facilitator modelling and video feedback. Interventions focused on improving infant sleep and crying behaviours generally utilised a behavioural model by providing specific management plans, specific strategies and techniques such as swaddling or controlled crying, in addition to providing information on physiological changes in the infant, normal sleep patterns, infant development, advice and reassurance.
Treatment Effects
Intervention effects were analysed separately for each outcome and forest plots for these are provided in Figs 2–4. We ran the analyses with and without the outliers and found no significant differences between them so analyses with outliers were reported as we felt that would be more representative of the studies. Participants in intervention groups demonstrated significantly more responsiveness towards their baby compared to control participants, k = 18, d = 0.77, 95%CI (0.50–1.03), Z = 4.72, p < .001. This effect is moderate to large. The heterogeneity between effect sizes was large (I 2 = 0.82, T 2 = 0.21), but not significant, Q(17) = 95.36, p = .129. However, low power can explain non-significant Q statistics with small sample sizes (Higgins et al. 2003). Given the large I 2, moderator analysis was conducted to explore possible variation.
In regards to infant sleep, participants in intervention groups showed significantly better infant sleep behaviours, k = 13, d = 0.24, 95%CI (0.14–0.35), Z = 3.93, p < .001 compared to control conditions. This is a small effect. There was significant variation in effect sizes for these studies, Q(12) = 16.52, p = .002, I 2 = 0.33, T 2 = 0.01, and thus moderators were explored to explain this heterogeneity.
Interventions assessing crying did not show significant intervention effects, k = 8, d = 0.27, 95%CI (0.034–0.498), Z = 1.89, p = .059. There was no significant heterogeneity in effect sizes for these studies, Q(7) = 12.60, p = .194, I 2 = 52.4, T 2 = 0.03.
Confidence and competence were not assessed via meta-analyses due to the small number of studies assessing these outcomes; however we examined the effect sizes for each of the four studies individually. Hamilton-Dodd et al. (1989) found that mothers who completed a maternal preparation program were not more confident or competent compared to the control group. Wolfson et al. (1992) found a large significant effect on parental confidence, d = 0.93, p < .01, and Barlow et al. (2013) found a small significant effect of self-efficacy (i.e. confidence) at 12 months (d = 0.23). Finally, Magill-Evans et al. (2007) did not find a significant effect on father confidence between intervention and control group.
Moderator Effects
Table 3 shows the results of the combined and single moderator analyses for parent responsiveness and infant sleep. For parent responsiveness, the predictor year of publication was significant, so that older studies had higher effect sizes than newer studies. No other predictor was significant in the combined analysis. Individual analysis (assessing effects of each moderator separately) also found a significant impact of year of publication. In addition, interventions with fewer sessions were more effective than ones with a larger number of sessions. None of the moderators explained heterogeneity of effect sizes for infant sleep in either the combined or single moderator analysis.
Discussion
This review analysed the results of 36 papers that assessed 35 different interventions conducted over three decades. These studies comprised families from a range of countries and different risk backgrounds. This study has overcome the limitations of previous reviews (Bakermans-Kranenburg et al. 2003; Bryanton and Beck 2010; Pinquart and Teubert 2010) by restricting inclusion of studies to those of sound methodology (i.e. RCTs), specifying and clearly defining outcome variables crucial to infant development and specifying a time period that focuses on the transition to parenthood (i.e. during pregnancy up until 12 months post birth) rather than a very small window of eight weeks post birth (Bryanton and Beck 2010) or beyond infancy into early childhood (Bakermans-Kranenburg et al. 2003). Overall, this review adds to the literature by providing a more focused and in-depth picture of the effects of parenting interventions at the transition to parenthood. We found clear support for the efficacy of early parenting interventions in improving parental responsiveness specifically for babies under 12 months, identified a lack of empirical studies evaluating parental confidence and competence with those included having inconclusive results, and found support for interventions reducing infant sleep problems, but not infant crying. However, the result on infant crying is likely underpowered. The effect size for infant crying was comparable to infant sleep (d = .27 vs. d = .24), but there were fewer studies for infant crying (8 vs. 13).
Bakermans-Kranenburg et al. (2003) only found a small effect on maternal sensitivity whereas our results found a moderate to large effect. This difference might be because they assessed children up to age four and a half years and the definition and assessment of responsiveness in children older than 12 months might be different. Our effect size for parental responsiveness is very promising, because high levels of responsiveness are crucial to the parent-infant relationship, secure attachment and infant development (Raval et al. 2001; Smith et al. 2006), and is an important skill in responding to baby’s signals effectively.
The effect on parental responsiveness is also larger compared to the effects on infant sleep and crying, which could be due to the different types of interventions that are used to increase parental responsiveness and those aimed at improving infant crying and sleep problems. Responsiveness interventions employed an attachment-based approach and offered participants practice through facilitator modelling, video feedback and active encouragement of responsiveness towards the baby. Sleep and crying interventions on the other hand, used a behavioural approach and were mainly informational in that they provided advice on strategies, but did not offer much facilitator support and practice within the intervention sessions. The more active practice component within responsiveness interventions may be the active ingredient required to produce higher levels of change (Kaminski et al. 2008). Moreover, it is unclear whether the approach these interventions used played a role in influencing outcomes. Perhaps a combination of both attachment and behavioural-based interventions could lead to more effective outcomes for parents and infants as a more positive parent-child relationship coupled with effective behavioural strategies may provide parents with a more comprehensive skill set. Untangling the approach and content of these interventions is an important future research direction in order to design the most effective parenting interventions for parents of babies.
Moreover, just as plausible is the consideration that interventions on responsiveness measure an outcome that is more direct compared to measuring infant crying and sleep. Both types of parenting interventions, whether aimed at parent responsiveness or infant behaviours, intervene at the parent level. Therefore, greater effects are to be expected when the direct outcome of measurement is a change in parent behaviours. Infant behaviours are only indirectly affected and depend on how well the parent puts their learned skills into practice. Smaller effects on these outcomes are reasonable. An interesting research focus would be to conduct a longitudinal study in which parenting skills are assessed as a mediator in affecting baby behaviours at a later time point.
Interventions focused on parental responsiveness showed large heterogeneity, which was partially explained by the number of sessions and the year of publication. Older studies were more effective compared to newer studies. Pinquart and Teubert’s (2010) reasoned that knowledge of effective parenting strategies has become more widespread and more easily available so that parents start out with higher levels of skills and knowledge, and parents in control groups can obtain information from alternative sources. Consistent with previous reviews (Bakermans-Kranenburg et al. 2003; Pinquart and Teubert 2010), longer interventions were less effective compared to those with fewer sessions. However, this latter effect was only found in the single moderator analysis, and not in the combined analysis, which takes other moderators into consideration. Thus the moderator findings on the number of sessions should be interpreted with caution. Given the finding by Bakermans-Kranenburg et al. (2003) that responsiveness interventions were more effective when delivered later in development (cf. prenatal or early postnatal interventions), comparing these three time points (i.e. prenatal, early postnatal and late postnatal) might have explained some of the heterogeneity. However, our analyses did not detect a difference between prenatal and postnatal interventions. Analysing the early and late postnatal period separately was not feasible due to low power (N = 4 and 9, respectively). After inspecting the effect sizes for these groups individually, we could not determine a trend to support Bakermans-Kranenburg et al.’s finding.
Our results on infant sleep problems showed a significant, although small effect, demonstrating that parenting interventions can improve infants’ sleep, which supports and adds further evidence to Bryanton and Beck’s (2010) study. None of the inspected moderators explained the variance between studies, possibly due to the small number of studies, and hence low power (Cohen et al. 2002). This systematic review investigated the effects of early parenting interventions on infant crying. Our review included additional studies on infant crying that have been conducted since Bryanton and Beck’s review in 2010, which shows that interest in this research area has increased.
There are several possible explanations for the small and non-significant result on infant sleep and crying, respectively. First, the small number of studies included in the meta-analyses limits the power to detect an effect (Cohen et al. 2002). Second, the studies included babies of varying ages; some infants were newborns whereas in other studies they were up to 12 months of age. In the first year of life, there are significant developmental changes in infants’ sleep and crying behaviours (James-Roberts and Plewis 1996), which can make it difficult to assess intervention effects. For example, it may be more difficult to change these behaviours in newborns as they have limited self-regulatory ability and, cry and wake more often at night because of a need to feed compared to older babies. Douglas and Hill (2013) found no improvement in infant sleep following interventions conducted before the age of six months, citing the impact of feeding as a variable that explains any effects on sleep or crying. We were not able to verify the difference between interventions done in the early or late postnatal period for infant crying or sleep outcomes, because all interventions for crying were done in the early postnatal period, and most sleep interventions in the late postnatal period. Another reason could be the lack of a practice component in these interventions as outlined earlier, which may have impacted on parents’ ability to implement strategies effectively. Potential barriers for parents to using the strategies, such as emotional anxiety in implementing controlled crying, might explain this. Assessing parent’s implementation of the strategies provided in the interventions would be informative.
Competence was only assessed in one study and confidence in four studies, with inconsistent results. This was very surprising given the well-acknowledged importance of these outcomes as key parenting skills that can ultimately lead to other positive outcomes in parents and infants (Denis et al. 2012; Jones and Prinz 2005; Leerkes and Crockenberg 2002; Wolfson et al. 1992). Thus, no clear conclusions can be drawn and further research is critical to investigate the effects of interventions for parents with babies as well as to examine the influence of competence and confidence in improving other outcomes.
One of the key strengths of these meta-analyses compared to previous reviews is the fact that we limited the included studies to RCTs. This allowed us to more specifically assess whether the interventions are effective under strict criteria. This is a necessary precursor to determine before non-RCTs are evaluated because these are more prone to be affected by extraneous variables. This is particularly important given the somewhat inconsistent and at best small effects shown in previous reviews, which have included a diversity of methodological formats. Our review has demonstrated the effectiveness of interventions for responsiveness and infant sleep, however, there is a clear need for more high quality studies relating to infant crying interventions to be carried out before determining their use in real-world applications.
Limitations and Future Research Directions
The number of included studies in these meta-analyses per outcome variable was small. The moderator analysis was able to explain some of the variance in responsiveness, but outstanding variance in effect sizes remained unexplained for parent responsiveness and for infant sleep. Moderators chosen to investigate in these meta-analyses were based on findings in previous reviews, thus it is interesting that while some of them explained variance in Pinquart and Teuberts’ (2010) review, they did not explain any variance in infant sleep and parent responsiveness except for year of publication and number of sessions. This study extends the existing knowledge in this field by demonstrating the efficacy of parenting interventions on improving responsiveness and infant sleep. However, given the small number of studies that have been conducted in this important field, it is questionable whether sufficient high quality studies have been done on parenting interventions for infants in order to conclusively state what makes an intervention effective. Future RCTs should investigate the effects of interventions on infant crying, and particularly on parent competence and confidence in order to shed light on some of the inconsistencies found in this review.
To aid future review ability to conduct accurate and reliable analyses, it would also be important for RCT studies, as well as non-RCTs, to provide more information in their reporting. In this review, it was not always possible to obtain statistical information even as simple as means and standard deviations for control and intervention groups, which makes calculating effect sizes difficult. A clearer definition of the interventions would also be helpful, such as more detail on the intervention content.
The way the key outcomes of this review were measured should also be considered when conducting future trials of parenting interventions for parents of infants. There was measurement variability with some studies choosing self-report measures by parents (for confidence, competence, infant sleep and crying), or observational measures such as actigraphy (for infant sleep) or home observation (for responsiveness) of the parent-infant interaction. Our results showed that studies assessing responsiveness, measured using observational tools, showed stronger effects, compared to studies on infant sleep and crying, which were predominantly assessed using self-report (e.g. baby diary). This measurement variability may partly explain the inconsistent results between outcomes, as self-reporting on how much infants sleep or cry may be less reliable, given that such reports may be influenced by sleep deprivation or poor memory recollection of the exact length of time their baby slept or cried. It would be helpful if future studies could utilise more direct measures for these outcomes and also provide data on comparisons between these two different measurement approaches to measuring infant behaviour.
There was also insufficient follow-up data available to analyse the effect of early parenting interventions in the long term. It would be important for future studies to investigate long-term effects of these interventions and how improvements in responsiveness, infant sleep and crying, as well as parental confidence and competence may lead to changes in later child development. Furthermore, this review limited the assessment of interventions on only a few key parent and infant outcomes at the expense of excluding other important outcomes at the transition to parenthood. For example, exposure to trauma or violence in the family home can have a large influence on child development and future studies should examine these in more detail. Finally, the majority of the included studies mainly involved mothers in the intervention. Fathers often feel unsupported at the transition to parenthood (Deave and Johnson 2008; Halle et al. 2008) so future trials should aim to involve more fathers in the intervention and assess whether inclusion of fathers leads to increased positive outcomes for infants and parents.
References
References marked with an asterisk indicate studies included in the meta-analyses
*Akai, C. E., Guttentag, C. L., Baggett, K. M., & Willard Noria, C. C. (2008). Enhancing parenting practices of at-risk mothers. Journal of Primary Prevention, 29, 223–242.
*Ammanti, M., Speranza, A. M., Tambelli, R., Muscetta, S., Lucarelli, L., & Vismara, L., et al. (2006). A prevention and promotion intervention program in the field of mother-infant relationship. Infant Mental Health Journal, 27(1), 70–90.
Bakermans-Kranenburg, M. J., van Ijzendoorn, M. H., & Juffer, F. (2003). Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin, 129(2), 195–215.
*Barlow, et al. (2013). Effect of a paraprofessional home-visiting intervention on American Indian teen mothers’ and infants’ behavioral risks: A randomized controlled trial. American Journal of Psychiatry, 170(1), 83–93.
Bell, S. M., & Ainsworth, S. M. D. (1972). Infant crying and maternal responsiveness. Child Development, 43(4), 1171–1190.
Bohlin, G., & Hagekull, B. (1987). “Good Mothering”: Maternal attitudes and mother-infant interaction. Infant Mental Health Journal, 8(4), 352–363.
Bryanton, J., & Beck, C. T. (2010). Postnatal parental education for optimizing infant general health and parent-infant relationships (Review). The Cochrane Library, 12, 1–90.
Card, N. A. (2012). Applied meta-analysis for social science research. New York, NY: Guildford Press.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159.
Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2002). Applied multiple regression/ correlation analysis for the behavioural sciences. 3rd ed. London: Lawrence Erlbaum.
Cooper, P. J., De Pascalis, L., Woolgar, M., Romaniuk, H., & Murray, L. (2015). Attempting to prevent postnatal depression by targeting the mother–infant relationship: A randomized controlled trial. Primary Health Care Research & Development, 16(383–397). 10.1017/S1463423614000401.
*Cooper, P. J., Tomlinson, M., Swartz, L., Landman, M., Molteno, C., & McPherson, K., et al. (2009). Improving quality of mother-infant relationship and infant attachment in socioeconomically deprived community in South Africa: Randomized controlled trial. BMJ, 338:b974, 1–8.
Coleman, P. K., & Karraker, K. H. (1997). Self-Efficacy and parenting quality: Findings and future applications. Developmental Review, 18, 47–85.
Cheung, M. W. L. (2008). A model for integrating fixed-, random-, and mixed-effects meta- analyses into structural equation modeling. Psychological Methods, 13(3), 182–202.
Deave, T., & Johnson, D. (2008). The transition to parenthood: what does it mean for fathers? Journal of Advanced Nursing, 63(6), 626–633.
Denis, A., Ponsin, M., & Callahan, S. (2012). The relationship between maternal self-esteem, maternal competence, infant temperament and post-partum blues. Journal of Reproductive and Infant Psychology, 30(4), 388–397.
De Wolff, M. S., & van IJzendoorn, M. H. (1997). Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development, 68(4), 571–591.
*Dickie, J. R., & Gerber, S. C. (1980). Training in social competence: The effect on mothers, fathers, and infants. Child Development, 51, 1248–1251.
*Dihigo, S. K. (1998). New strategies for the treatment of colic: Modifying the parent/infant interaction. Journal of Pediatric Health Care, 12, 256–262.
Douglas, P. S., & Hill, P. S. (2013). Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: A systematic review. Journal of Development & Behavioural Pediatrics, 34, 497–507.
Feeney, J. A., Hohaus, L., Noller, P., & Alexander, R. P. (2001). Becoming parents: Exploring the bonds between mothers, fathers, and their infants. New York, NY: Cambridge University Press.
Guttentag, C. L., Landry, S. H., Williams, J. M., Baggett, K. M., Noria, C. W., & Borkowski, J. G., et al. (2014). “My Baby & Me”: Effects of an early, comprehensive parenting intervention on at-risk mothers and their children. Development Psychology, 50(5), 1482–1496.
Halle, C., et al. (2008). Supporting fathers in the transition to parenthood. Contemporary Nurse, 31, 57–70.
*Hamilton-Dodd, C., Kawamoto, T., Clark, F., Burke, J. P., & Fanchiang, S. P. (1989). The effects of a maternal preparation program on mother-infant pairs: A pilot study. The American Journal of Occupational Therapy, 43(8), 513–521.
Hemmi, M. H., Wolke, D., & Schneider, S. (2001). Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: A meta-analysis. Archives of Disease in Childhood, 96, 622–629.
Hedges, L. V., & Olkin, I. (1985). Statistical methods for meta-analysis. San Diego, CA: Academic Press.
Heinicke, C. M., Beckwith, L., & Thompson, A. (1988). Early intervention in the family system: A framework and review. Infant Mental Health Journal, 9, 111–141.
Higgins, J. P. T., Thompson, S. G., Decks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327, 557–560.
*Hiscock, H., Bayer, J., Gold, L., Hampton, A., Ukoumunne, O. C., & Wake, M. (2007). Improving infant sleep and maternal mental health: A cluster randomised trial. Archives of Disease in Childhood, 92, 952–958.
*Hiscock, H., Cook, F., Bayer, J., Le, H., Mensah., F., Cann, W., Symon, B., & St James-Roberts, I. (2014). Preventing early infant sleep and crying problems and postnatal depression: A randomized trial. Pediatrics, 133, e346–e354.
*Hiscock, H., & Wake, M. (2002). Randomised controlled trial of behavioural infant sleep intervention to improve infant sleep and maternal mood. BMJ, 324, 1–6.
James-Roberts, I., & Plewis, I. (1996). Individual differences, daily fluctuations, and developmental changes in amounts of infant waking, fussing, crying, feeding, and sleeping. Child Development, 67, 2527–2540.
Jones, T. L., & Prinz, R. J. (2005). Potential roles of parental self-efficacy in parent and child adjustment: A review. Clinical Psychology Review, 25, 341–363.
*Kalinauskiene, L., Cekuoliene, D., Van IJzendoorn, M. H., Bakermans-Kranenburg, M. J., Juffer, F., & Kusakovskaja, I. (2009). Supporting insensitive mothers: The Vilnius randomized control trial of video-feedback intervention to promote maternal sensitivity and infant attachment security. Child: Care, Health, and Development, 35(5), 613–623.
Kaminski, J. W., Valle, L. A., Filene, J. H., & Boyle, C. L. (2008). A meta-analytic review of components associated with parent training effectiveness. Journal of Abnormal Child Psychology, 36(4), 567–589.
Karl, D. (1995). Maternal responsiveness of socially high-risk mothers to the elicitation cues of their 7-month-old infants. Journal of Pediatric Nursing: Nursing Care of Children and Families, 10, 254–263.
*Keefe, M. R., Lobo, M. L., Froese-Fretz, A., Kotzer, A. M., Barbosa, G. A., & Dudley, W. N. (2006). Effectiveness of an intervention for colic. Clinical Pediatrics, 45, 123–133.
*Kerr, S. M., Jowett, S. A., & Smith, L. N. (1995). Preventing sleep problems in infants: A randomized controlled trial. Journal of Advanced Nursing, 24, 938–942.
Kingston, D., Tough, S., & Whitfield, H. (2012). Prenatal and postpartum maternal psychological distress and infant development: A systematic review. Child Psychiatry Human Development, 43, 683–714.
*Landry, S. H., Smith, K. E., & Swank, P. R. (2006). Responsive parenting: Establishing early foundations for social, communication, and independent problem-solving skills. Developmental Psychology, 42(4), 627–642.
Leerkes, E. M., & Crockenberg, S. C. (2002). The development of maternal self-efficacy and its impact on maternal behavior. Infancy, 3, 227–247.
Liu, C. C., Chen, Y. C., Yeh, Y. P., & Hsieh, Y. S. (2011). Effects of maternal confidence and competence on maternal parenting stress in newborn care. Journal of Advanced Nursing, 68(4), 908–918.
*Magill-Evans, J., Harrison, M. J., Benzies, K., Gierl, M., & Kimak, C. (2007). Effects of parenting education on first-time fathers’ skills in interactions with their infants. Fathering, 5(1), 41–56.
*McRury, J. M., & Zolotor, A. J. (2010). A randomized, controlled trial of a behavioral intervention to reduce crying among infants. Journal of the American Board of Family Medicine, 23(3), 315–322.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. (2009). Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. Plos Medicine, 6(7), 1–6.
Murray, L., Fiori-Cowley, A., Hooper, R., & Cooper, P. J. (1996). The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Development, 67, 2512–2516.
Muthén, L. K., & Muthén, B. O. (1998–2011). Mplus user’s guide. Sixth Edition Los Angeles, CA: Muthén & Muthén.
*Niccols, A. (2008). ‘Right from the start’: Randomized trial comparing an attachment group intervention to supportive home visiting. Journal of Child Psychology and Psychiatry, 49(7), 754–764.
*Nikolopoulou, M., & St James-Roberts, I. (2003). Preventing sleeping problems in infants who are at risk of developing them. Archives of Diseases in Childhood, 88, 108–111.
*Parkin, P., Schwartz, C. J., & Manuel, B. A. (1993). Randomized controlled trial of three interventions in the management of persistent crying of infancy. Pediatrics, 92(2), 197–202.
PEDro Scale. (2016, October 4). http://www.pedro.org.au/english/downloads/pedro-scale/.
*Pfannenstiel, A. E., & Honig, A. S. (1991). Prenatal intervention and support for low-income fathers. Infant Mental Health Journal, 12(2), 103–115.
Pinquart, M., & Teubert, D. (2010). Effects of parenting education with expectant and new parents: A meta-analysis. Journal of Family Psychology, 24(3), 316–327.
Priddis, L. E. (2009). Tuned in parenting and infant sleep patterns. Early Child Development and Care, 179(3), 259–269.
*Puckering, C., McIntosh, E., Hickey, A., & Longford, J. (2010). Mellow babies: A group intervention for infants and mothers experiencing postnatal depression. Counselling Psychology Review, 25(1), 28–40.
Raval, V., Goldberg, S., Atkinson, L., Benoit, D., Myhal, N., & Poulton, L., et al. (2001). Maternal attachment, maternal responsiveness and infant attachment. Infant Behavior & Development, 24(3), 281–304.
*Salisbury, A. L., High, P., Twomey, J. E., Dickstein, S., Chapman, H., Liu, J., & Lester, B. (2012). A randomized control trial of integrated care for families managing infant colic. Infant Mental Health Journal, 33(2), 110–122.
Schulz, M. S., Cowan, C. P., & Cowan, P. A. (2006). Promoting healthy beginnings: A randomized controlled trial of a preventive intervention to preserve marital quality during the transition to parenthood. Journal of Consulting and Clinical Psychology, 74(1), 20–31.
*Scott, G., & Richards, M. P. M. (1990). Night waking in infants: Effects of providing advice and support for parents. Journal of Child Psychology Psychiatry, 31(4), 551–567.
*Sleep, J., Gillham, P., St James-Roberts, I., & Morris, S. (2002). A randomized controlled trial to compare alternative strategies for preventing infant crying and sleep problems in the first 12 weeks: The COSI study. Primary Health Care Research and Development, 3, 176–183.
Smith, K., Landry, S., & Swank, P. (2006). The role of early maternal responsiveness in supporting school-aged cognitive development for children who vary in birth status. Pediatrics, 117, 1608–1617.
*St James-Roberts, I., Sleep, J., Morris, S., Owen, C., & Gillham, P. (2001). Use of a behavioural programme in the first 3 months to prevent infant crying and sleeping problems. Journal of Paediatrics and Child Health, 37, 289–297.
*Stremler, R., Hodnett, E., Kenton, L., Lee, K., Weiss, S., Weston, J., & Willan, A. (2013). Effect of behavioural-educational intervention on sleep for primiparous women and their infants in early postpartum: multisite randomised controlled trial. BMJ, 346, 1–14.
*Stremler, R., Hodnett, E., Lee, K., MacMillan, S., Mill, C., & Ongcangco, L. (2006). A behavioral-educational intervention to promote maternal and infant sleep: A pilot randomized, controlled trial. Sleep, 29(12), 1609–1615.
*Symon, B. G., Marley, J. E., Martin, A. J., & Norman, E. R. (2005). Effect of a consultation teaching behaviour modification on sleep performance in infants: A randomised controlled trial. Medical Journal of Australia, 182, 215–218.
Teti, D. M., & Gelfand, D. M. (1991). Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development, 62, 918–929.
*van den Boom, D. C. (1994). The influence of temperament and mothering on attachment and exploration: An experimental manipulation of sensitive responsiveness among lower-class mothers with irritable infants. Child Development, 65(5), 1457–1477.
*van Doesum, K. T. M., Riksen-Walraven, J. M., Hosman, C. M. H., & Hoefnagels, C. (2008). A randomized controlled trial of a home-visiting intervention aimed at preventing relationship problems in depressed mothers and their infants. Child Development, 79(3), 547–561.
*Velderman, M. K., Bakermans-Kranenburg, M. J., Juffer, F., & van IJzendoorn, M. H. (2006). Effects of attachment-based interventions on maternal sensitivity and infant attachment: Differential susceptibility of highly reactive infants. Journal of Family Psychology, 20(2), 266–274.
*Wendland-Carro, J., Piccinini, C. A., & Miller, W. S. (1999). The role of an early intervention on enhancing the quality of mother-infant interaction. Child Development, 70(3), 713–721.
*Whitt, J. K., & Casey, P. H. (1982). The mother-infant relationship and infant development: The effect of pediatric intervention. Child Development, 53(4), 948–956.
Wilson, D.B. (2011). Effect size calculations and elementary meta-analysis. http://gemini.gmu.edu/cebcp/SymposiumPresentations/Wilson.pdf. Accessed 19 September 2013.
*Wolfson, A., Lacks, P., & Futterman, A. (1992). Effects of parent training on infant sleeping patterns, parents’ stress, and perceived parental competence. Journal of Consulting and Clinical Psychology, 60(1), 41–48.
Wolke, D., Rizzo, P., & Woods, S. (2002). Persistent infant crying and hyperactivity problems in middle childhood. Pediatrics, 109, 1054–1060.
Acknowledgment
This study was unfunded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The Parenting and Family Support Centre is partly funded by royalties stemming from published resources of the Triple P—Positive Parenting Program, which is developed and owned by The University of Queensland (UQ). Royalties are also distributed to the Faculty of Health and Behavioural Sciences at UQ and contributory authors of published Triple P resources. Triple P International (TPI) Pty Ltd is a private company licensed by Uniquest Pty Ltd on behalf of UQ, to publish and disseminate Triple P worldwide. The authors of this report have no share or ownership of TPI. Dr Alina Morawska receives royalties from TPI. TPI had no involvement in the study design, collection, analysis or interpretation of data, or writing of this report. Dr Mandy Mihelic is an employee at UQ and was a student at UQ at the time this study was developed and carried out. Ania Filus has no conflict to declare.
Informed Consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Mihelic, M., Morawska, A. & Filus, A. Effects of Early Parenting Interventions on Parents and Infants: A Meta-Analytic Review. J Child Fam Stud 26, 1507–1526 (2017). https://doi.org/10.1007/s10826-017-0675-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-017-0675-y