Abstract
Behavioral parent training (BPT) is an evidence-based intervention for the treatment of attention-deficit/hyperactivity disorder and related disruptive behavior disorders in youth. Although efficacious, dropout from BPT is a notable issue, particular for high-risk families. The literature suggests that parental factors (stress, psychopathology and cognitions) may be particularly important in understanding which parents dropout from BPT. To date, however, limited attention has been given to how these factors may be related to dropout at varying points during BPT. Secondary data analyses from a completed clinical trial of a traditional BPT intervention is presented herein. Forty participants were classified into three groups based on timing of dropout from BPT (enrolled in but never attended BPT; dropped out during BPT, and completed BPT). Parent-level factors (stress, depressive symptoms, parental efficacy, and parental attributions for child behavior) were assessed at baseline and post-treatment (parental perceived barriers to treatment) to determine if these factors were differentially related to dropout group status. Results suggested that parents who never attended BPT were more likely to have lower parental efficacy and greater maladaptive attributions regarding their child compared to parents who dropped out from BPT and those who completed BPT. Moreover, parents perceptions of the relevance of BPT was lower in the never attended group and the dropped out from BPT group compared to the completed BPT group. Results of the study have implications for tailoring engagement strategies focused on parental cognitions throughout the process of BPT, particularly for high-risk families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Behavioral Parent Training (BPT) is an efficacious treatment for attention-deficit/hyperactivity disorder (ADHD; Evans et al. 2014), oppositional defiant disorder (ODD), and conduct disorder (CD; Eyberg et al. 2008), collectively referred to as disruptive behavior disorders [DBDs]). However, drop out from BPT has long been a prominent issue that often limits the potential impact of BPT for DBDs (Chacko et al. 2016; Chronis et al. 2004; Nock and Ferriter 2005). In an effort to understand and ultimately intervene to improve engagement and reduce drop out, empirical studies have focused on characterizing families (youth with DBDs and their parents) who are at risk for poor engagement/drop out from BPT (e.g., Johnston et al. 2010; Kazdin et al. 1997a; Kazdin and Mazurick 1994; Nock and Kazdin 2001; Peters et al. 2005; Webster-Stratton 1985). Moreover, although considerably less well-studied, some efforts have been made to identify characteristics of families that may be related to differential drop out from BPT over different time points (e.g., prior to the start of BPT; early vs. late drop out; Kazdin and Mazurick 1994; Schneider et al. 2013).
The development of this line of empirical investigation initially focused on measures of convenience (e.g., socioeconomic status, marital status, race/ethnicity, age of parent(s); Kazdin et al. 1997a, b). These factors, although related to engagement/drop out from BPT, are static and/or are not often malleable, and therefore, not readily useful for developing more targeted approaches to improving engagement/reducing drop out from BPT. Likewise, parameters of BPT intervention (e.g., group vs. individual formats; setting where BPT is implemented) do not clearly affect engagement/drop out (Chacko et al. 2016). Importantly, given the direct role that parents play in learning and implementing BPT content, there has been increasing interest in identifying malleable parent-level factors that may better explain drop out from BPT (Chronis et al. 2004; Morrissey et al. 1999). There are several parent-level factors that have been related to poor engagement/drop out from BPT, including parental difficulties (e.g., depressive symptoms; parental stress), parental cognitions (e.g., attributions for child behavior; parenting efficacy), and practical and perceived barriers to treatment.
Personal parental difficulties have long been noted as significantly impacting drop out from BPT (Chacko et al. 2016; Chronis et al. 2004). While there are numerous such factors (e.g., marital discord, substance use: Chronis et al. 2004), two of the more well-studied include parental depression and stress. Parents of children with ADHD, particularly mothers, are more likely to experience depressive symptoms and episodes of depression than parents of typically developing children (Chronis et al. 2003a). Importantly, higher rates of depressive symptoms is associated with a higher likelihood of drop out from BPT (Chronis et al. 2004; Webster-Stratton 1985). In addition, several studies have also demonstrated that high levels of parental stress predict drop out from BPT (Kazdin et al. 1997a, b). Parental depression and stress may decrease motivation to fully engage in treatment and make it more difficult to consistently implement changes in parenting behavior. Moreover, depressive symptoms and stress may increase the likelihood that parents perceive a treatment as very demanding, thereby increasing the chances of drop out from BPT (Nock and Ferriter 2005).
The relation between parental cognitions and engagement/drop out to BPT has also been explored. Johnston and colleagues (Johnston et al. 2010; Mah and Johnston 2008) have espoused the importance of low parenting efficacy (parents who perceive their parenting to be less effective) and maladaptive attributions of children’s behavior (i.e., attributing child behavior as internal, stable, and global) on beliefs regarding the effectiveness and acceptability of BPT, ultimately impacting engagement to BPT and outcomes following BPT. It appears that parents must believe that they have some level of effectiveness in their parenting to find interventions focused on parenting behaviors to be acceptable. Parents who perceive their parenting to be less effective may be less likely to engage in interventions that focus on parenting. Johnston et al. (2010) demonstrated that mothers’ parenting efficacy is significantly and positively correlated with acceptability of BPT. Additionally, attributions of children’s behavior have implications for parents’ expectations of the usefulness of treatment and ultimately may also predict engagement in treatment (Peters et al. 2005; Miller and Prinz 2003; Morrissey-Kane and Prinz 1999). For instance, research has shown that some parents of children with ADHD are more likely to attribute causes of their child’s behavior to enduring symptoms of the disorder and to factors that are out of the child’s control (Johnston and Freeman 1997). As such, for these parents, it is not surprising that there is lower acceptability of interventions such as BPT that emphasize improving behavior through altering contingencies in the environment. Accordingly, Johnston et al. (2010) found that when attributions of a child’s ADHD symptoms are pervasive and enduring, but are within the child’s control, BPT has been rated as more acceptable. While parental attributions and efficacy have been shown to be related to acceptability and outcomes following BPT, there are no studies to date, to our knowledge, that have specifically assessed the relation between parenting attributions and efficacy and drop out from BPT—an important understudied area of investigation (Mah and Johnston 2008).
Based on the seminal work of Kazdin et al. (1997a, b), practical barriers to treatment and parental perceptions of treatment have been found to be related to treatment engagement. Practical barriers include stressors and obstacles that compete with treatment (e.g., conflict with significant other), as well as treatment demands. Perceived barriers include parental perceptions of the relevance of treatment (meeting expectations for content and focus of treatment). Practical and perceived barriers to treatment have also been shown to be related to drop out from BPT. For instance, a negative relation has been demonstrated between perceptions of treatment (i.e., perceived relevance, effectiveness) and drop out in BPT (Kazdin et al. 1997a, b; Nock and Kazdin 2001); however, others have not found this relation (Johnston et al. 2010). Moreover, the greater the number of perceived barriers to treatment, the more likely a family will terminate BPT early or miss multiple sessions. Indeed, drop out rates are highest in families who perceive multiple barriers and stressors associated with BPT (Kazdin et al. 1997a, b).
A less well-studied issue in understanding drop out in BPT has been the extent to which specific family variables are related to drop out at various points during BPT. Kazdin and Mazurick (1994) investigated whether certain factors (i.e., socioeconomic status, parental stress, psychopathology, antisocial behavior, adverse child-rearing practices, intellectual functioning, child relationships with other antisocial youth) distinguished between families who drop out early (completed 6 or fewer sessions) vs. later (completed between 7 and 14 sessions). Characteristics of families who drop out of BPT early included single-parent status, minority status, low income, poor living accommodations, and adverse family child-rearing practices, parenting stress, mother’s history of antisocial behavior, and contact with antisocial peers. Characteristics of families who drop out of BPT later included poor adaptive functioning at school and living in a home with a non-biological parent. This study did not assess parent-level process factors such as attributions and sense of efficacy.
Although there has been considerable progress in the literature on characterizing families who drop out from BPT, there remains a need to differentiate characteristics of families who drop out from BPT at varying time points. To our knowledge, there has been one investigation into factors that differentiate parents who never attend BPT from those who prematurely drop out and from those who complete BPT (Schneider et al. 2013). Schneider et al. evaluated the extent to which child (i.e., ethnicity, severity of ADHD problems, severity of other externalizing behaviors) and parent/family factors (i.e., stress, psychopathology, socioeconomic status, single parenthood status) were predictive of never attending BPT or dropping out after initiating BPT in a sample of families of school-age children with ADHD. Results of this study suggest that single-parent status was the only factor to be related to either never attending or dropping out from BPT.
There are several implications and limitations of the literature in this area. First, it is surprising that there is a dearth of empirical investigation into factors related to drop out from BPT at varying time points, particularly regarding families who initiate treatment but never attend. This is a notable issue given that some studies have shown that between 25–50 % of families who are scheduled to begin BPT never attend a single session (Chacko et al. 2016, 2012; Peters et al. 2005). Second, the aforementioned Schneider et al. (2013) study suggests that a focus on understanding factors related to drop out may be particularly important in groups that are at higher-risk (e.g., single-parents) for never attending and dropping out from BPT (Chronis et al. 2004). Lastly, as discussed earlier, moving beyond distal factors (e.g., child ethnicity, socioeconomic status, single-parent status, etc.) toward more proximal, malleable factors may prove most useful in order to develop targeted approaches to addressing drop out from BPT across varying time points. To our knowledge, the only two studies that have focused on identifying factors related to drop out at varying points during BPT are limited in that they primarily focused on a variety of distal, static factors (Kazdin and Mazurick 1994; Schneider et al. 2013).
Understanding which factors characterize families who differentially drop out from BPT has several important clinical implications. Ongoing assessment of parent-level factors are increasingly utilized to tailor BPT (Chacko et al. 2015; Rajwan et al. 2014). Determining which factors are most important at various stages of drop out in BPT can allow for BPT practitioners to systematically track, identify, and address challenges before drop out occurs. Similarly, there is a growing interest in identifying methods to improve engagement to BPT (Chacko et al. 2016, 2012; Becker et al. 2015; Lindsey et al. 2014) with attention being given to various aspects of engagement (attendance vs. homework completion). Understanding which factors characterize families who drop out from BPT at various key points can foster efforts to target engagement during critical junctures in treatment. Given that specific engagement methods appear to be differentially effective for specific engagement outcomes (Becker et al. 2015; Lindsey et al. 2014), identifying discrete factors related to specific points of drop out in BPT may allow for further development of the armamentarium of engagement strategies now being actively developed for BPT.
Additionally, while drop out from BPT is a universal issue (Chacko et al. 2016), as others have stated (Kazdin and Whitley 2003), it is particularly important to understand drop out in certain high-risk populations. For example, there is substantial data that single-parent (often mothers) status is significantly related to drop out during BPT (e.g., Chacko et al. 2008, 2009; Kazdin and Mazurick 1994; Kazdin et al. 1993; Schneider et al. 2013). Single mothers experience multiple adverse factors that impact their involvement in BPT, including higher rates of depression and stress as well as less social support (Cairney et al. 2003). These parents are also more likely to have greater practical barriers to treatment participation (Kazdin et al. 1997b; Kazdin and Wassell 2000) as well as maladaptive cognitions regarding treatment and their children (Nock and Kazdin 2001), which consequently result in additional difficulties for these families during BPT. Thus, it is not surprising that single-mother families are less likely to enroll in BPT (Cunningham et al. 2000), complete BPT (Kazdin and Mazurick 1994; Kazdin et al. 1993), improve following BPT (Dumas and Wahler 1983; Webster-Stratton and Hammond 1990), and maintain treatment gains over time (Bagner and Eyberg 2003; Chacko et al. 2009; Webster-Stratton 1985). As such, focusing efforts on identifying characteristics of single-mother families who drop out at various points during BPT may be particularly important.
The aim of the present investigation was to identify factors that differentially characterize high-risk parents (i.e., single-mothers) of school-age youth with ADHD who either do not attend BPT, drop out from BPT, or complete BPT, focusing on key parent-level factors (i.e., depressive symptoms, parental stress, parenting efficacy, attributions for their child’s behavior, and common perceived/practical barriers to treatment participation). Based on the literature, we hypothesized the following associations between these parent-level factors and drop out. First, we hypothesized that there would be differences in parental cognitions regarding parenting (parenting efficacy) and their child (attributions for behavior) between families who never attend BPT compared to those who drop out or those who complete BPT. As indicated in the literature (Mah and Johnston 2008), parents likely come into intervention with a set of attributions regarding their child and sense of efficacy regarding their parenting based on a history of parenting their child. When faced with BPT, an intervention that focuses on changes to parenting behavior, those parents with maladaptive (i.e., internal, stable and global) attributions regarding their child’s behavior and low levels of parenting efficacy may view BPT as an intervention that is not acceptable/effective for addressing their child’s problematic behavior. As such, these families may not participate in BPT from the outset of treatment. We also hypothesized that that there would be differences in perceived and practical barriers to treatment between families who drop out from BPT compared to families that complete BPT, which aligns with previous work in this area (Kazdin et al. 1997a; Kazdin and Holland et al. 1997; Kazdin and Mazurick 1994). More specifically, we hypothesized that the dropout group would report higher levels of perceived and practical barriers compared to those who complete BPT. Lastly, we hypothesized that there would be differences in parenting stress and depressive symptoms between families who never attend BPT, those who drop out from BPT, and those who complete BPT. More specifically, given the consistent relations between stress and depressive symptoms and BPT engagement (Chronis et al. 2004), we hypothesized that the never attend group will report higher rates of parenting stress and depressive symptoms, followed by the dropout group, followed lastly by the treatment completer group.
Method
Participants
Between September 2002 and March 2005, single-mother families were recruited for participation in a randomized controlled trial of two versions of group-based BPT and a wait-list control group through radio advertisements, mailings, and school referrals (Chacko et al. 2009). Recruitment information was minimal and only conveyed that a research study was being conducted comparing different forms of a parenting intervention to improve ADHD and related behavioral concerns for single-mother-headed families of school-age children. Families were enrolled through direct phone contact with the research staff. Once contacted, families were provided information on the intervention and were scheduled to participate in an intake session to determine eligibility and to discuss the study interventions.
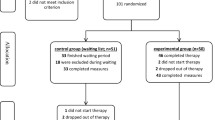
Inclusion into the study required that children be between five and twelve years old at the start of treatment and meet diagnostic criteria for ADHD (any type), through a formal structured assessment prior to enrolling in the study (see Chacko et al. (2009) for details of assessment and diagnostic process). Families were excluded if the child had an IQ of less than 80, was diagnosed with a pervasive developmental disorder, or if there was evidence of psychosis. These exclusion criteria have been typically used to obtain a relatively homogenous sample of youth with ADHD that will most benefit from BPT. Youth with lower IQ, pervasive developmental disorders and/or psychosis often require different and more intensive services (Chacko et al. 2015). Mothers’ consent and child assent was obtained before the initial intake. The study procedures were approved by the University’s Social and Behavioral Sciences Institutional Review Board. The final sample consisted of 120 children with ADHD and their single mothers. Herein we utilize data on participants assigned to the traditional BPT group (n = 40; see Table 1 for demographic description of study participants).
Procedures
Traditional BPT
The traditional BPT program is a manualized, nine-week BPT program held for two and one-half hours each week that was developed for this study based on empirically supported BPT interventions (e.g., Cunningham et al. 1998). Single mothers engaged in a collaborative, large-group format to discuss and learn about core effective BPT strategies (e.g., positive attending, planned ignoring, incentive systems). Furthermore, sessions included videotapes of parenting errors whereby single mothers identified these errors and then formulated alternative parenting strategies. Furthermore, therapists facilitated group discussions by asking questions to encourage single mothers to make adaptive attributions about the effects of their parenting on their children’s behavior. Therapists modeled the parenting techniques and single mothers role-played the use of the BPT technique(s) in session. Single mothers were assigned weekly homework assignments based on the content of the session. See Table 2 for the content of BPT sessions. For this study, three group-based BPT groups were conducted over the course of the period of the study. BPT groups were conducted at the University ADHD Center. In addition, a meal was provided during each BPT group. No other incentives or support (e.g., transportation; incentives for attendance) was provided to families.
During the program, children (and their siblings who were within the 5–12 age range) participated in a concurrent traditional, group-based social skills program (Cunningham et al. 1998). Children were divided into two groups based on the developmental level of the child. Typically, children between the ages of 5 to 8 formed one group while children between the ages of 9 to 12 formed another group. Children were supported in the acquisition of key social skills used in peer contexts (e.g., cooperation, validation) through didactic training, modeling, role-playing and ongoing support of the skills through age-appropriate small-group games. The child group was focused on providing childcare for families rather than therapeutic benefit as traditional social skills interventions for youth with ADHD have not been shown to be effective (Evans et al. 2014).
Treatment integrity and fidelity
All BPT groups were conducted by the same two doctoral-level clinical psychology students. The two facilitators underwent extensive training on ADHD and behavioral interventions, including BPT, over a 4 year period. Training included intensive coursework and practicum experiences as well as completion of two external training programs led by renowned leaders in the BPT field. Supervision of facilitators was provided by a licensed clinical child psychologist with extensive expertise in ADHD and behavioral interventions. Treatment integrity to the content and process of BPT treatment sessions was measured by two independent coders who reviewed 100 % of the treatment session videotapes and completed checklists of the required components for each session. Data indicated that 100 % of the BPT sessions were completed as manualized. Additionally, raters (study participants and independent raters) assessed therapist skill/behavior. High levels of treatment fidelity and therapist competence were observed (see Chacko et al. (2012) for greater details).
Group classification
Families enrolled in the traditional BPT program were classified into three groups: (1) Never Attenders (N = 11): Families who presented at study intake but subsequently did not attend a BPT session, (2) Treatment Dropouts (N = 15): Families who attended at least one BPT session but dropped out from the treatment, and; (3) Treatment Completers (N = 14): Families that did not meet definition for drop out. Drop out from BPT was defined as a parent explicitly stating that she did not want to continue treatment or a parent failing to appear for three consecutive sessions despite repeated efforts by investigators to contact and engage the parent. Identical procedures to define drop out have been used in other studies of BPT (e.g., Miller and Prinz 2003; Nock and Kazdin 2005).
Measures
Parental psychosocial adjustment
Depressive symptoms
The Beck Depression Inventory (BDI; Beck and Steer 1987) is a 21-item self-report measure used to assess depressive symptoms over the preceding two week period. Each item (e.g., I am so sad or unhappy that I can’t stand it; I feel that the future is hopeless and things cannot improve; I feel I am a complete failure as a person) is rated on a scale from one to four, with higher total scores on the BDI indicating a greater degree of depression. The BDI is highly correlated with clinical ratings of depression (r = .72), and has been shown to have high internal consistency in both clinical and nonclinical samples, with mean coefficient alphas of .86 and .81, respectively (Beck et al. 1988). A total score on the BDI, which is a sum of the 21-item measure, was used in the study. Chronbach alpha for this sample was .83.
Parenting stress
The Parenting Stress Index-Short Form (PSI-SF; Abidin 1995) is a 36-item self-report measure used to assess parenting stress in three domains: Parental Distress (e.g., I feel trapped by my responsibilities as a parent), Parent-Child Dysfunctional Interaction (e.g., I expected to have closer and warmer feelings for my child that I do and this bother me), and Difficult Child (e.g., My child gets upset easily over the smallest things). The PSI-SF is measured along a 5-point scale from 1 (Strongly Disagree) to 5 (Strongly Agree), with higher total scores indicating greater levels of parenting stress. High levels of internal consistency (alpha = .83) and 1 year stability (r = .75) have been reported (Haskett et al. 2006). The PSI-SF correlates with parental perceptions of child adjustment and observed parent and child behavior adjustment (Haskett et al. 2006). For this study, the Total Stress score, which is the sum of the three PSI-SF domains, was used. Chronbach alpha for the total score for this sample was .81.
Parental cognitions of parenting and children’s behavior
Attributions of child behavior
The Children’s Attribution Style Questionnaire-Parent Version (CASQ-P; Kaslow et al. 1978) is a 24-item forced-choice measure of parents’ attributions about positive (e.g., Your child received a good grade on a test) and negative events (e.g., Your child broke a glass) related to their child. For positive and negative child outcomes, three attribution dimensions are assessed: internal/external, global/specific, and stable/unstable. A total score for positive outcomes and a total score for negative outcomes are computed. For the positive event composite, high scores indicate a more adaptive (i.e., more external, situational, specific) attribution style. For the negative event composite, high scores indicate a more depressive (i.e., more internal, stable, global) attribution style. A total score, which is the score for positive event composite minus the score for negative even composite, was used in this study. Higher total scores indicate more adaptive attributions for child behavior. Chronbach alpha for this sample was .80.
Parenting efficacy
Parenting efficacy was measured using the Parenting Sense of Competence Scale–Efficacy Subscale (PSOC-Efficacy; Johnston and Mash 1989). The measure has seven items (e.g., I honestly believe I have all the skills necessary to be a good mother to my child) rated on a 6-point scale from strongly agree to strongly disagree. Scores are averaged across items and higher scores indicate greater feelings of parenting efficacy. The measure has demonstrated internal consistency and correlates as expected with measures of parenting (e.g., McLaughlin and Harrison 2006) and child problems (e.g., Johnston and Mash 1989). Scores on the measure predict treatment response among families of children with ADHD (Hoza et al. 2000). Chronbach alpha for this sample was .83.
Parental perceived barriers to treatment
Barriers to treatment
The Barriers to Treatment Scale (BTS; Kazdin et al. 1997b) is a 44-item self-report measure that is rated along a five-point scale from 1 (Never a problem) to 5 (Always a problem). The BTS assesses barriers to treatment participation involving stressors and obstacles that compete with treatment (e.g., Treatment was in conflict with other activities), treatment demands and issues (e.g., I felt this treatment was more work than expected), and perceived relevance of treatment (I felt that treatment did not focus on my life and problems). Several items were removed from the original BTS that were not applicable to this study (e.g., My medical insurance did not cover this treatment), with a total score calculated from 36 items. Four subscales are obtained on the BTS (Stressors—Obstacles; Treatment Demands; Relevance of Treatment; Relationship with Therapist). Subscales focused on (1) stressors/obstacles, (2) treatment demands, and (3) relevance of treatment was utilized in this study. The relationship with therapist subscale was not used in the study as families categorized as never attending treatment would not have interacted with the therapist during treatment. Barriers to treatment were assessed at the end of treatment. Chronbach alpha’s were .81, .84 and .79 for the stressors-obstacles, treatment demands, and relevance of treatment subscales, respectively.
Results
A series of one-way between-groups analysis of variance were conducted to characterize group status (Never Attended, Dropout, Completed) on the seven dependent variables (see Table 3 for means, standard deviations, and group comparisons). Data were available for all participants at pre- and post-treatment. Analysis of patterns of dropout suggest that dropout occurred at session five for the Dropout group—representing a midway point of BPT—with a range of attendance from four to five sessions. For the Completed group, there was an average of eight session attended with a range of attendance from eight to nine sessions. As such, the Dropout group and Completed group significantly differ in terms of average sessions attended. There was a statistically significant difference (p < .05) in CASQ scores for the three groups: F (2, 37) = 9.81, p < .0001, ηp2 = .35, as well as in Parenting Efficacy Scores: F (2, 37) = 22.10, p < .0001, ηp2 = .54, and Barriers to Treatment Scale—Relevance of Treatment Scores: F (2, 37) = 5.27, p = .01, ηp2 = .21. Effect sizes suggest that the difference in mean scores across these three variables between groups was large. Post-hoc comparisons using the Tukey HSD test indicated that the mean CASQ score for the Never Attend group was significantly lower than the mean CASQ scores for both the Dropout and Completed groups. There was no difference in mean CASQ scores between the Dropout and Completed groups. Similarly, post-hoc comparisons using the Tukey HSD test indicated that the mean Parenting Efficacy score for the Never Attend group was significantly lower than the mean Parenting Efficacy scores for both the Dropout and Completed groups, with no difference in mean Parenting Efficacy scores between the Dropout and Completed groups. Lastly, post-hoc comparisons using the Tukey HSD test indicated that the mean Barriers to Treatment Scale, Relevance of Treatment subscale score for Never Attend group was significantly greater than that of the Completed groups. Additionally, the mean Relevance of Treatment subscale score (from the Barriers to Treatment Scale) for the Dropout group was significantly greater than that of the Completed group. There were no statistically significant differences on the Relevance of Treatment subscale scores between the Never Attend and Dropout groups.
Discussion
The aim of the present investigation was to identify factors that differentially characterize high-risk parents (i.e., single mothers) of school-age youth with ADHD who do not attend group-BPT, from those who drop out from group-BPT, and those who complete group-BPT, focusing on key parent-level factors (i.e., depressive symptoms, parental stress, parenting efficacy, attributions for their child’s behavior, and common perceived/practical barriers to treatment participation). Our hypotheses were partially confirmed. First, it was found that parental cognitions (parenting efficacy and attributions for child behavior) were significantly lower/less adaptive in single mothers who never attended BPT relative to single mothers who drop out from and completed BPT. In addition, barriers to treatment (i.e., treatment relevance) were greater for those families who never attended and those who drop out from BPT compared to families that completed BPT. Contrary to our hypothesis, there were no statistically significant differences between the three groups on parenting stress and depressive symptoms. To our knowledge, this is one of only two other investigations (i.e., Kazdin and Mazurick 1994; Schneider et al. 2013) of factors related to drop out at varying points in BPT. Moreover, aside from Schneider et al. (2013), this is the only investigation focused on families who initiate but never attend BPT. Importantly, unlike Schneider, the current investigation focused on parent-level, malleable risk factors in a sample of parents at high-risk for drop out (i.e., single mothers). These findings, clinical implications, and future research directions are discussed below.
Parents who never attended BPT had lower ratings of parenting efficacy and had greater maladaptive attributions (i.e., internal, global, and stable) for their child’s behavior than parents who drop out from and those who completed BPT. These findings extend upon the literature regarding BPT for ADHD (Johnston et al. 2010; Mah and Johnston 2008), which has demonstrated that these factors are related to acceptability; the current study suggests that these factors are also related to drop out from BPT. In particular, these factors are most prominent in those families who never attend BPT. These findings suggest that it is critical to assess parental self-perceptions as well as parental views of their child when they are enrolling in BPT. It may be that these factors relate reciprocally—having low parenting efficacy may be due to attributions that a child’s behavior is not controllable and vice versa. Given this potential relation, it is not surprising that these parents also perceived BPT to be less relevant in meeting their needs (despite never having participated in a BPT session) compared to those families who completed BPT. Identifying families who have these cognitions may lead to recommendations for alternative evidence-based strategies that do not require high levels of investment in parenting and take a biologically-driven etiological perspective on child behavior (i.e., stimulant medication). Alternatively, as some have suggested (Chacko et al. 2009, 2012; Chronis et al. 2004; Mah and Johnston 2008; Peters et al. 2005), addressing these factors directly prior to enrolling in BPT will be necessary. More specifically we (Chacko et al. 2015) have recommended that BPT should include a preparation stage that allows parents to learn about BPT, address concerns regarding the process of BPT, and clarify expectations regarding BPT. In light of the findings of this study, it appears that explicit discussions regarding self-perceptions of parenting efficacy and attributions regarding their child’s behavior should be included as part of an intake prior to enrollment of BPT. It may be that frank discussions can help to clarify whether BPT is an acceptable intervention for a family with low parenting efficacy and maladaptive attributions, thereby helping parents make more informed decisions about treatments for their child. Importantly, this is not to say that low parenting efficacy or higher levels of maladaptive cognitions should preclude a family from participating in BPT. Moreover, as group-BPT interventions often require sufficient numbers of enrolled families, determining whether a family will actively participate in group-BPT has practical importance to facilitators and the process and functioning of a group. As such, ensuring that parents are in fact fully planning to attend group-BPT can be enhanced by attention to these parent-level factors before the start of the intervention.
The only factor that was significantly different between families who drop out from BPT relative to those that completed BPT was parents’ perspectives regarding the relevance of BPT. This finding provides further evidence for perceived barriers representing a critical aspect of engagement in general, but more specifically to drop out from BPT (Kazdin et al. 1997a, b; Kazdin and Mazurick 1994). Importantly, unlike studies which have found that practical barriers are related to engagement in general, it appears that the perceived relevance of treatment is particularly important for families who at least participate in BPT. This nuance is important, as perceptions of barriers may be more malleable than the practical barriers that parents experience. For parents who drop out from BPT, it appears that monitoring of their perception of the relevance of BPT in a simple and ongoing manner is necessary. Determining when relevance of BPT becomes problematic is needed to target efforts at adapting content and focus to address issues with relevance. This is likely a more pertinent issue in group-based (compared to individually-based) BPT, given the inherent challenges of consistently gauging the individual responses/perspectives of all members in a group. It may be necessary to gauge relevance using the Barriers to Treatment Scale- Relevance of Treatment subscale and having separate discussions (by phone or in person) with parents who note challenges with the relevance of BPT. It may be that addressing relevance can ultimately be achieved through changes to the treatment format (moving from group-based to individually-formatted BPT) or augmenting services (adding medication, addressing parental mental health concerns, etc.). If improving outcomes is the goal of treatment, then understanding when and how to tailor treatment is important. Assessing relevance of ongoing treatment appears to be a straightforward and meaningful way to engage parents in the treatment process and to ensure that families are receiving services they find acceptable and effective to address their concerns. Unfortunately, ongoing systematic attention to parents’ perceptions of relevance of BPT does not appear to be a common occurrence (Chacko et al. 2015).
To our surprise, ratings of depressive symptoms, parental stress, and practical stressors/obstacles and treatment demands were not significantly different between groups. There may be several reasons for these results. For example, overall group sample sizes were small, and as such, there was low power to detect differences for these specific measures. Between-group effect sizes for depressive symptoms were in the mild-to-moderate range, and therefore, the associations between depression and drop out were likely too small to be detected. It is likely that further study with a larger sample is necessary before a strong conclusion can be made about the relative importance of parenting stress and depressive symptoms and their relation to various points of drop out from BPT.
There are notable limitations and future directions in this line of empirical research. First, the findings of this study are constrained by the study sample and intervention. Single mothers of school-age children with ADHD and related DBDs represent a specific population where attributions of child behavior, parenting efficacy, and perceived relevance of treatment may be unique relative to other populations (e.g., intact families; children with only oppositional and defiant behaviors; young children). Single mothers represent a high-risk population for drop out to BPT (Schneider et al. 2013), and their parenting efficacy may be in part affected by being the primary (if not sole) caregiver for their children. While BPT is an evidence-based treatment for ADHD (Evans et al. 2014), BPT was not developed as a treatment specifically for ADHD (Chacko et al. 2015), and others have noted the potential insufficiency of BPT to address what many consider a biologically-driven disorder (Antshel and Barkley 2008; Chacko et al. 2014). Given the nature and presentation of ADHD, the increasing proliferation of the biological model of ADHD, and the ubiquitous use of medication as a treatment, it would not be surprising that some parents of youth with ADHD may perceive BPT as not being relevant to their needs. This perception of relevance may be less of an issue for treatment of purely oppositional, aggressive and conduct problems, where BPT has its roots (Eyberg et al. 2008). Moreover, parents of school-aged youth, compared to younger children, have a longer history of parenting their child. As such, these parents have more opportunities to observe the effects of their parenting and make attributions for their child’s behavior. It is likely that parents of older youth may have more negative experiences, resulting in lower parenting efficacy and are therefore more likely to attribute their child’s behavior to uncontrollable factors. Parents of younger children may not have had consistent or sufficiently negative experiences with their child to develop a more stable sense of low parenting efficacy and internal, stable and global child attributions.
Additionally, aspects of the BPT intervention used in this investigation, such as frequency (one session per week), duration (nine weeks), format (group), a concurrent child group, and potential incentives (e.g., meals provided at group) may address obstacles and therefore pose less demands compared to other versions of BPT. As a comparison, in Kazdin’s seminal work on perceived and practical barriers to treatment participation (Kazdin et al. 1997a, b; Kazdin and Mazurick 1994), a more demanding (individual format) and longer (16-session) BPT intervention was studied, which likely presented more practical barriers. On the other hand, group-based BPT is a fixed intervention that does not allow for a great deal of tailoring for an individual family (schedule, content, pace, etc.), and likely poses different obstacles for families. While concurrent child groups and meals are often a feature of research studies (Chacko et al. 2008, 2009, 2015; Fabiano et al. 2009) these may not be feasible within routine practice—thereby differentially impacting dropout in these settings. Collectively, practical and perceived demands are likely directly related to type of BPT treatment used and setting of implementation.
The findings of this study, as well as other studies assessing engagement broadly and drop out more specifically, are also constrained by how these constructs are defined. In this study, we utilized a definition for drop out during BPT based on definitions utilized in other studies (Miller and Prinz 2003; Nock and Kazdin 2005). This definition is useful as it appears to meaningfully characterize subgroups of families based on theoretically derived factors of drop out. However, as some have noted (Chacko et al. 2016), studies of drop out from BPT often differ in the ways that they define rates and patterns of dropout, making it difficult to compare findings across studies. Furthermore, in their review of the literature, Chacko et al. (2016) highlighted that studies often used different informants (parent, clinician and observer) when assessing drop out, which further contributes to challenges in interpretation across studies. The literature on drop out would benefit from utilizing multiple definitions of drop out from multiple informant perspectives but done so in a consistent manner that can be compared across studies.
An understudied aspect of drop out is the time-course relation between potential parent-level factors (e.g., parenting efficacy), child-levels factors (e.g., child behavior; functional impairment; ADHD symptoms) and drop out. The current study assessed parent-level factors at the beginning and end of treatment; this approach does not dynamically capture the relation between changes in these factors over the course of treatment and potential drop out. As has been seen in BPT studies for ADHD (see Chacko et al. 2015 for a review) some of the parent-level factors related to drop out (parenting efficacy) are often improved following BPT. There is a great deal of literature suggesting that child-level outcomes also improve following BPT for children with ADHD (Chacko et al. 2015). As such, these factors are not fixed, but are instead dynamic and time-dependent. As we described earlier, while clinically it may prove useful to obtain systematic, ongoing assessment of key factors related to drop out, it is imperative that future studies of drop out to BPT capture the dynamic interplay between parent- and child-level factors and drop out from BPT. In fact, as Kazdin (2000) noted, there is a significant number of families who are considered “dropouts” from BPT but likely do so because they have experienced some benefit and may no longer see the need to continue with treatment. As such, these are not “dropouts” but are likely best considered “responders” to an abbreviated form of BPT. Understanding these nuances requires research using ongoing systematic assessment of key factors and outcomes at multiple levels and perspectives.
In summary, this investigation is novel in some respects, extends the literature in the field of drop out from BPT in general and specifically for group-BPT for single-mother families of youth with ADHD, and offers clear clinical recommendations. Nevertheless, further research is warranted. Specifically, future research should utilize larger samples of more diverse families and evaluate multiple malleable parent-level factors (e.g., motivation; readiness for change) and child-level factors (e.g., child behaviors, symptoms) in the context of varying types of BPTs (e.g., parent-child interaction therapy) over the course of BPT. A body of research documenting the importance of key variables in differentiating groups who drop out at various points during BPT will further lead to targeted approaches to engage and retain families in one of the few efficacious psychosocial treatments for ADHD and DBDs.
References
Abidin, R. R. (1995). Parenting Stress Index. 3rd edn. Odessa, FL: Psychological Assessment Resources.
Antshel, K. M., & Barkley, R. (2008). Psychosocial interventions in attention deficit hyperactivity disorder. Child and Adolescent Psychiatric Clinics of North America, 17(2), 421–437.
Bagner, D. M., & Eyberg, S. E. (2003). Father involvement in parent training: When does it matter? Journal of Clinical Child and Adolescent Psychology, 32, 599–605.
Beck, A. T., & Steer, R. A. (1987). Beck Depression Inventory Manual. NY: The Psychological Corporation, Harcourt Brace Jovanovich, Inc.
Beck, A. T., Steer, R. A., & Garbin, M. G. (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8(1), 77–100.
Becker, K. D., Lee, B. R., Daleiden, E. L., Lindsey, M., Brandt, N. E., & Chorpita, B. F. (2015). The common elements of engagement in children’s mental health services: Which elements for which outcomes? Journal of Clinical Child & Adolescent Psychology, 44(1), 30–43.
Cairney, J., Boyle, M., Offord., D., & Racine, Y. (2003). Stress, social support, and depression in single and married mothers. Social Psychiatry and Psychiatric Epidemiology, 38, 442–449.
Chacko, A., Alan, C., Uderman, J., Cornwell, M., Anderson, L., & Chimiklis, A. (2015). Training parents of children with ADHD. In R. Barkley (Ed), Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 4th edn. (pp. 513–536). New York, NY: Guilford Press.
Chacko, A., Gopalan, G., Franco, L., Dean-Assael, K., Jackson, J., Marcus, S., Hoagwood, K., & McKay, M. (2015). Multiple-Family Group service delivery model for the children with disruptive behavior disorders. Journal of Emotional and Behavioral Disorders, 23, 67–77.
Chacko, A., Jensen, S., Lowry, L. S., Cornwell, M., Chimiklis, A., Chan, E., Lee, D., & Pulgarin, B. (2016). Engagement in behavioral parent training: Review of the literature and implications for practice. Clinical Child and Family Psychology Review, 19, 204–215.
Chacko, A., Kofler, M., & Jarrett, M. (2014). Improving outcomes for youth with ADHD: Conceptual framework for combined neurocognitive and skill-based treatment approaches. Clinical Child and Family Psychology Review, 17, 368–384.
Chacko, A., Wymbs, B. T., Arnold, F. W., Pelham, W. E., Swanger-Gagne, M., Girio, E. L., Pirvics, L., Herbst, L., Guzzo, J. L., Phillips, C., & O’Connor, B. (2009). Enhancing traditional behavioral parent training for single-mothers of children with ADHD. Journal of Clinical Child and Adolescent Psychology, 38, 206–218.
Chacko, A., Wymbs, B. T., Chimiklis, A., Wymbs, F. A., & Pelham, W. E. (2012). Evaluating a comprehensive strategy to improve engagement to group-based behavioral parent training for high-risk families of children with ADHD. Journal of Abnormal Child Psychology, 40, 1351–1362.
Chacko, A., Wymbs, B. T., Flammer-Rivera, L., Pelham, W. E., Walker, K. S., Arnold, F., Visweswaraiah, H., Swanger-Gagne, M., Girio, E., Pirvics, l, & Herbst, L. (2008). A pilot study of the feasibility and efficacy of the Strategies to Enhance Positive Parenting program for single mothers of children with ADHD. Journal of Attention Disorders, 12(3), 270–280.
Chronis, A. M., Chacko, A., Fabiano, G. A., Wymbs, B. T., & Pelham, W. E. (2004). Enhancements to the behavioral parent training paradigm for families of children with ADHD: Review and future directions. Clinical Child and Family Psychology Review, 7, 1–27.
Chronis, A. M., Lahey, B. B., Pelham, W. E., Kipp, H., Baumann, B., & Lee, S. S. (2003a). Psychopathology and substance abuse in parents of young children with attention deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1425–1432.
Cunningham, C. E., Boyle, M., Offord, D., Racine, Y., Hundert, J., Secord, M., & McDonald, J. (2000). Tri-ministry study: Correlates of school-based parent course utilization. Journal of Consulting and Clinical Psychology, 68, 928–933.
Cunningham, C. E., Bremner, R., & Secord, M. (1998). COPE: The Community Parent Education Program: A School-Based Family Systems Oriented Workshop for Parents of Children with Disruptive Behavior Disorders. Hamilton, ON: COPE Works.
Dumas, J. E., & Wahler, R. G. (1983). Predictors of treatment outcome in parent training: Mother insularity and socioeconomic disadvantage. Behavioral Assessment, 5, 301–313.
Evans, S. W., Owens, J. S., & Bunford, N. (2014). Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology, 43(4), 527–551.
Eyberg, S. M., Nelson, M. M., & Boggs, S. R. (2008). Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child & Adolescent Psychology, 37(1), 215–237.
Fabiano, G. A., Chacko, A., Pelham, W. E., Robb, J., Walker, K. S., Arnold, F., Sastry, A., Flammer, L., Keenan, J. K., Visweswaraiah, H., Shulman, S., Herbst, L., & Pirvics, L. (2009). A Comparison of behavioral parent training programs for fathers of children with attention-deficit/hyperactivity disorder. Behavior Therapy, 40, 190–204.
Haskett, M. E., Ahern, L. S., Ward, C. S., & Allaire, J. C. (2006). Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child & Adolescent Psychology, 35(2), 302–312.
Hoza, B., Owens, J. S., Pelham, W. E., Swanson, J. M., Conners, K., Hinshaw, S. P., Arnold, L. E., & Kraemer, H. C. (2000). Parent cognitions as predictors of child treatment response in attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology, 28, 569–583.
Johnston, C., Mah, J. W. T., & Regambal, M. (2010). Parenting cognitions and treatment beliefs as predictors of experience using behavioral parenting strategies in families of children with attention-deficit/hyperactivity disorder. Behavior Therapy, 41, 491–504.
Johnston, C., & Mash, E. J. (1989). A measure of parenting satisfaction and efficacy. Journal of Clinical Child Psychology, 18, 167–175.
Johnston, C., & Freeman, W. (1997). Attributions for child behavior in parents of children without behavior disorders and children with attention deficit-hyperactivity disorder. Journal of Consulting and Clinical Psychology, 65(4), 636–645.
Kaslow, N. J., Tanenbaum, R. L., & Seligman, M. E. P. (1978). The KASTAN: A children’s attributional styles questionnaire. Philadelphia, PA: Unpublished manuscript, University of Pennsylvania.
Kazdin, A. E. (2000). Psychotherapy for children and adolescents: Directions for research and practice. Oxford University Press, New York, NY.
Kazdin, A. E., Holland, L., & Crowley, M. (1997a). Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology, 65, 453–463.
Kazdin, A. E., Holland, L., Crowley, M., & Brenton, S. (1997b). Barriers to treatment participation scale: Evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry, 38, 1051–1062.
Kazdin, A. E., & Mazurick, J. L. (1994). Dropping out of child psychotherapy: Distinguishing early and late dropouts over the course of treatment. Journal of Consulting and Clinical Psychology, 62, 1069–1074.
Kazdin, A. E., Mazurick, J. L., & Bass, D. (1993). Risk for attrition in treatment of antisocial children and families. Journal of Clinical Child Psychology, 22, 2–16.
Kazdin, A. E., & Wassell, G. (2000). Predictors of barriers to treatment and therapeutic change in outpatient therapy for antisocial children and their families. Mental Health Services Research, 2, 27–40.
Kazdin, A. E., & Whitley, M. K. (2003). Treatment of parental stress to enhance therapeutic change among children referred for aggressive and antisocial behavior. Journal of Consulting and Clinical Psychology, 71, 504–515.
Lindsey, M. A., Brandt, N. E., Becker, K. D., Lee, B. R., Barth, R. P., Daleiden, E. L., & Chorpita, B. F. (2014). Identifying the common elements of treatment engagement interventions in children’s mental health services. Clinical Child and Family Psychology Review, 17(3), 283–298.
Mah, J. W., & Johnston, C. (2008). Parental social cognitions: Considerations in the acceptability of and engagement in behavioral parent training. Clinical Child and Family Psychology Review, 11(4), 218–236.
McLaughlin, D. P., & Harrison, C. A. (2006). Parenting practices of mothers of children with ADHD: The role of maternal and child factors. Child and Adolescent Mental Health, 11(2), 82–88.
Miller, G. E., & Prinz, R. J. (2003). Engagement of families in treatment for childhood conduct problems. Behavior Therapy, 34(4), 517–534.
Morrissey-Kane, E., & Prinz, R. J. (1999). Engagement in child and adolescent treatment: The role of parental cognitions and attributions. Clinical Child and Family Psychology Review, 2(3), 183–198.
Nock, M. K., & Ferriter, C. (2005). Parent management of attendance and adherence in child and adolescent therapy: A conceptual and empirical review. Clinical Child and Family Psychology Review, 8, 149–166.
Nock, M. K., & Kazdin, A. E. (2001). Parent expectancies for child therapy: Assessment and relation to participation in treatment. Journal of Child and Family Studies, 10, 155–180.
Nock, M. K., & Kazdin, A. E. (2005). Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology, 73, 872–879.
Peters, S., Calam, R., & Harrington, R. (2005). Maternal attributions and expressed emotion as predictors of attendance at parent management training. Journal of Child Psychology and Psychiatry, 46(4), 436–448.
Rajwan, E., Chacko, A., Wymbs, B. T., & Wymbs, F. A. (2014). Evaluating clinically significant change in parent and child functioning: Comparison of traditional and enhanced behavioral parent training. Journal of Abnormal Child Psychology, 42, 1407–1412. doi:10.1007/s10802-014-9877-6.
Schneider, B., Gerdes, A., Haack, L., & Lawton, K. (2013). Predicting treatment dropout in parent training interventions for families of school-aged children with ADHD. Child & Family Behavior Therapy, 35(2), 144–169.
Webster-Stratton, C. (1985). Predictors of treatment outcome in parent training for conduct disordered children. Behavior Therapy, 16, 223–243.
Webster-Stratton, C. H. (1985). The effects of father involvement in parent training for conduct problem children. Journal of Child Psychology and Psychiatry, 26, 801–810.
Webster-Stratton, C., & Hammond, M. (1990). Predictors of treatment outcome in parent training for families with conduct problem children. Behavior Therapy, 21, 319–337.
Funding
This study was funded by the National Institute of Mental Health (F32HD054067)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Chacko, A., Wymbs, B.T., Rajwan, E. et al. Characteristics of Parents of Children with ADHD Who Never Attend, Drop Out, and Complete Behavioral Parent Training. J Child Fam Stud 26, 950–960 (2017). https://doi.org/10.1007/s10826-016-0618-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-016-0618-z