Abstract
Determining factors that affect healthcare utilization by the elderly is vital for the health system to be more responsive in providing care to this vulnerable group. The main objective of this paper is to identify the effect of the predisposing, enabling, and need factors on doctor visits and in-patient care for the elderly residing in the northern region of Malaysia. A multistage cluster sampling was used in selecting the sample for the study. A total of 1414 respondents aged 60 and over were interviewed face-to-face using a structured questionnaire. A probit model was used in estimating the utilization equations. At a significance level of 0.05, except for age, all predisposing and enabling factors were not statistically significant in affecting the doctor visits. On the other hand, being a male, smoker, medical insurance holder or had not actively involved in social interaction within the reference period increases the likelihood of being in-patient. Health-related variables remain the most significant factors that determine healthcare utilization, including both doctor visits and in-patient stays, in the area of study, which suggests that government policies to improve population health may influence the level of healthcare use in the future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Malaysian healthcare is provided by both the public and private sectors. In the public health sector, the main provider is the Ministry of Health (MOH), which provides primary care, secondary care, and tertiary care through a network of health facilities nationwide. The private healthcare sector mainstay is almost entirely confined to medical and curative treatment. Although the number of private hospitals has mushroomed in the last decade and contributes to about 64% of the total number of Malaysian hospitals, public hospitals still remain the largest healthcare providers in the country with 41,483 beds, contributing to 75% of total beds. The public sector healthcare system aims to provide universal access to healthcare for all citizens through public hospitals, health clinics and mobile clinics through the MOH. Public health services are heavily subsidized by the government where the fees collected by the MOH constituted about 2% of the MOH budget in 2004 (Yu et al. 2008).
The public services are funded by general taxation allocated to the MOH. The percentage of allocation varied from 3% to 4.54% of the gross domestic product (GDP) between years 2000 and 2014 (MOH 2016). This allocation was comparatively lower than some neighboring countries like Singapore, Thailand, and the Philippines. Private sector healthcare has expanded rapidly over the last few decades, driven by rising demand for good quality healthcare services from the middle class population who can afford to pay higher user fees (Yu et al. 2008). Private facilities have been preferable to public, especially for the urban population, because of shorter waiting times and flexible opening hours. Within the private sector, private health insurance is voluntary, premiums being charged based on the individual’s health status, history of illness, coverage level, and type of health insurance. Based on the Morbidity Survey III that was conducted in 2006, 18.8% of the Malaysian population owned some type of private health insurance (Institute for Public Health 2008).
Most countries are concerned with cost control in their healthcare delivery. The increase in public health expenditure may be due to the demographic transition toward an ageing population, as the elderly have been always been associated with multiple health problems. A population is classified as ageing when older people become a proportionately larger share of the total population. Declining fertility and increasing survival rates have led to this phenomenon. Ageing is seen as a triumph of development. People live longer because of improved nutrition, sanitation, medical advances, healthcare, education, and economic well-being. It has important and far-reaching implications for all aspects of a society. In the twenty-first century, population ageing is one of the most significant trends. This trend can be seen not only in developed and industrialized nations, but also in developing countries. The growth in the numbers and proportion of elderly is rapidly progressing in developing countries, including countries that have a large population of young people. According to the United Nations Population Fund (2012), of the current 15 countries with more than ten million older persons, seven are developing countries.
It is also found that life expectancy at birth in 2012 was over 80 years in 33 countries, compared to only 19 countries having reached this level in the previous five years. At present, only Japan has an older population of more than 30%: by 2050, it is expected that 64 countries are going to join Japan. In 2010, Malaysia had about 2.3 million older persons aged 60 and over, representing 7.9% of the Malaysian population of 28 million. This number showed an increase when compared to 2000, where there were 1.45 million older persons, or 6.3% of the total population. Based upon the projection rate and current trend, the Malaysian population is expected to reach 35 million by 2020, with 3.4 million (9.71%) being senior citizens (Department of Statistics Malaysia (DOSM) 2011; Rabieyah and Hajar 2003).
The age structure of the population largely depends on changing trends in fertility, mortality, and migration, and the transition to lower fertility and mortality rates in the population in Malaysia. The older generation is not a homogenous group for which providing specific healthcare fits all. It is important not to standardize older people as a single category but to recognize that the older population is just as diverse as any other age group in terms of, for example, age, sex, ethnicity, education, income, and health. Each group of older persons—such as low income, women, men, oldest old, indigenous, illiterate, urban, or rural—has particular needs and interests that must be addressed specifically through tailored healthcare provision. Besides, Malaysia is also a unique country with its multicultural background. The main ethnic groups are Malay (50.1%), followed by Chinese (22.6%), Indian (6.7%), other (12.4%), and non-citizens (8.2%) (DOSM 2010). There are various factors—such as demographic, socioeconomic (categorized into predisposing and enabling factors), and need factors—that may affect the demand for healthcare and they are country-specific. These factors may positively or negatively influence healthcare utilization.
Therefore it is a necessary to identify how these factors affect elderly healthcare demand within the context of Malaysia’s dual healthcare system, studies on which are rather limited. This may assist policy makers in designing more responsive and equitable health policies for this vulnerable group, as its proportion in relation to the total population has been increasing over time. The main objective of this paper is to identify the determinants of healthcare utilization by the elderly in northern states of Malaysia. The determinants are divided into predisposing, enabling, and need factors.
Past Studies
Studies of healthcare utilization greatly expanded following the work of Grossman (1972). Healthcare is input for the health production of an individual. People demand healthcare so that they can have improved health, be it for consumption or investment benefits. Though health status is presumed to be the main determinant of healthcare demand, other factors may also determine it. An understanding of the influence of these factors on healthcare demand is very important for policy makers in designing an equitable health system. In healthcare demand studies, demand factors may be divided into several categories. The most common starting point in understanding health services uses the behavioral model developed by Ronald Andersen back in 1968. Since then, the model has been adapted and expanded by many healthcare access researchers (e.g., Aday and Andersen 1974, 1981; Andersen 1995; Andersen and Newman 2005; Litaker et al. 2005). The standard behavioral model has divided use factors into three main categories, namely predisposing, enabling, and need factors. While Andersen (1968) focused on families’ use, the revised versions (Aday and Andersen 1981; Andersen 1995; Andersen and Newman 2005) have proposed individual determinants of health service use, but the three main categories remain the same as those proposed by Andersen (1968). Despite numerous expansions of the model, where some proposed other categories like environmental factors, health behavior, and health outcomes, the standard model remains influential.
Predisposing factors include demographic and social-economic characteristics which exist before the onset of illness. Age and gender are considered the important predisposing factors that may influence demand. When people grow older, they become more vulnerable to ill health and chronic diseases. Health conditions of individuals deteriorate with age and the deterioration rate increases as they grow older. At an older age, they tend to demand more healthcare in order to increase their health capital. A positive relationship between age and healthcare demand has been confirmed in some studies (for example, Deb and Trivedi 1997; Laroche 2000; Pohlmeier and Ulrich 1995; Windmeijer and Santos-Silva 1997; Wolinsky et al. 1983). The effect of gender is country-and service-specific. Some studies have found that women utilize more healthcare due to child bearing and women-specific diseases (Sarma and Simpson 2006; Windmeijer and Santos-Silva 1997). Women may also demand less due to difficulties in gaining access, especially in developing countries (Puentes-Markides 1992).
Education, marital status, and employment status are the important determinants of healthcare demand and their effects have been studied by a number of researchers. Kasirye et al. (2004), in their study on Uganda, found that the higher the level of education, the higher the probability of seeking modern healthcare, which was also found in earlier studies (Deb and Trivedi 1997; Lim et al. 2005). However, Laroche (2000) suggests that people with lower educational attainment are much more likely to consult general practitioners or to be hospitalized than are those with higher education. Further studies also found the effect of education insignificant (Gertler and van der Gaag 1990).
Marital status is another common factor that is included in the healthcare demand model. Deb et al. (2006), Nandakumar et al. (2000), and Sarma and Simpson (2006) found that marital status increases the probability of doctor and GP visits, while some studies (for example, Deb and Trivedi 1997; Gerdtham and Trivedi 2001; Gurmu 1997; Windmeijer and Santos-Silva 1997) reported the unimportance of marital status in utilization of healthcare. In Wan and Odell’s (1981) study, marital status had some adverse effect on health. Those who are widowed, divorced, or separated tend to visit the physician more often than individuals who never married or are married. So, as in the case of those living alone, results show that they had more visits to the physician compared to those who lived with others.
Economic activities may influence healthcare demand due to the fact that they may determine the amount of leisure devoted to health-producing activities. Pohlmeier and Ulrich (1995) agree that work place characteristics have a significant effect on visits to a general practitioner. They found that less physical work, little stress, and high self-determination lead to fewer visits to a general practitioner. Income and social capital, among others, are categorized as factors that facilitate demand, which is known as enabling. Alderman and Gertler (1989) indicate that individuals from households with a relatively high income stand a higher probability of seeking medical care than those from poor households.
Lim et al. (2005) also revealed a link between income and healthcare utilization using data from the Canadian Community Health Survey 2000–2001. High income individuals are more likely to seek medical attention from several practitioners than those with a low income. This implies that barriers to appropriate care may exist within low income groups. They are also less likely to report suffering from long-term activity limitations than those with a lower income. Similar findings regarding the effect of income on health status within the Canadian context are also found in Laroche (2000), which reveals an insignificant role of income in determining healthcare use. Some studies also suggest that income may reduce the utilization of specific healthcare services but not others. In Italy, Atella et al. (2004) suggest that high income people are less likely to visit general practitioners (GPs) as this group prefers to visit private specialists. Studies in Germany and Canada suggest a similar effect, that high income people prefer services from specialists to those offered by a GP (Pohlmeier and Ulrich 1995; Santos-Silva and Windmeijer 2001; van Doorslaer et al. 2006). The effect of income can also be non-linear (Windmeijer and Santos-Silva 1997), implying that healthcare demand is lower in both the highest and lowest income groups, or insignificant (Deb and Trivedi 1997; Sarma and Simpson 2006). Van Doorslaer et al.’ (2006) study on income equity in Canada found that low income groups are more intensive users of the healthcare system than higher income groups in most OECD countries. Using self-reported health levels, age, and sex as proxies for standardized doctor’s visits, they measured inequity in utilization of healthcare by disposable income. For Canada, higher income people have a higher probability of seeing a doctor than lower income people with the same level of need.
Another enabling factor that has a substantial influence on the demand for healthcare is insurance coverage. Research has shown that individuals with health insurance tend to consume more healthcare services than those with no insurance. In Deb and Trivedi’s (1997) study, utilization of healthcare services (physicians and non-physicians) in an office and outpatient setting is higher for those with supplementary private insurance than for individuals without extra coverage. Sarma and Simpson (2006) found that insurance significantly determined doctor utilization for healthy users and was insignificant for the less healthy. Some studies found there to be no significant effect of insured and uninsured or of insurance type. Wan and Odell’s (1981) study on the elderly in Baltimore County, Maryland, found no relationship between insurance coverage and physician visits, as most of the respondents were covered by Medicare, Medicaid, or private insurance. In other studies, in which the datasets are based on tax-financed systems, such as Italy, the UK, Sweden, Portugal, and Spain, the role of insurance status in health demand is not prominent, and no insurance variable is included in their analysis.
Many studies have revealed that social capital is among the major determinants of health status (Norstrand and Xu 2012; Poulsen et al. 2012; Rose 2000), which may later affect healthcare utilization. Social capital can originate within the same or a nearby community or from interactions between communities. The impact of community-level social capital or social capital at the individual level may have a negative relationship with healthcare use among the elderly, as found by Laporte et al. (2008) using the 2001 Canadian Community Health Survey and Canadian census. While the net effect of social capital on healthcare access has been discussed in the literature, the findings are not conclusive. This is found from a systematic review of 21 studies by Pitkin and Varda (2009).
The most important factors in demand are the need factors, which capture the need for healthcare. Many studies found a significant positive relationship between health status and demand for healthcare (Deb and Trivedi 1997; Pohlmeier and Ulrich 1995; Santos-Silva and Windmeijer 2001). Findings by Dunlop et al. (2000) and Sarma and Simpson (2006) also indicate that self-perceived health status and number of health problems were the variables most strongly associated with visits to both GPs and specialists.
Liu et al. (2012) focused on healthcare utilization by the elderly with national health insurance in Taiwan. Using latent class analysis, they examined the effect of different health profiles on the utilization of healthcare services and associated factors. Health status indicators were measured by health conditions, limitations, and functional impairments. Four health profiles were identified and they found that different health profiles of the elderly have a significant effect on utilization and expenditure on healthcare services. The high comorbidity group tends to utilize more services in ambulatory care than the relative healthy group, while the functional impairment group had relatively high probability of needing care assistance. In terms of expenditure for in-patient care, the frail group incurred higher healthcare expenditures.
Research Methods
Data
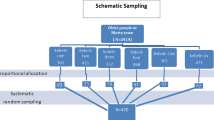
This study concentrates on healthcare utilization in the northern states in peninsular Malaysia, comprising Perlis, Kedah, Penang, and Perak. The total population of these four states in 2010 was 6.2 million. The targeted population of the present study is the elderly aged 60 and over residing in these four states. The total number of elderly within this group was 668,702. Given this, at 95% confidence level and 5 % margin of error, we required a total sample size of at least 384 respondents to represent the elderly population in the northern area. The survey involved face-to-face interviews using a structured questionnaire. The interviews were conducted from 1 September 2012 to 14 February 2013. To ensure the inclusion of working elderly, interviews were also conducted during weekends or after office hours. Participation was voluntary and every respondent was asked to sign a consent form prior to interview. These four states have different levels of economic development. Penang and Perak are considered developed states in Malaysia, whereas Kedah and Perlis are developing states. Due to the unavailability of a population frame, we used combined cluster, stratified, and snowball sampling. Cluster sampling was first applied. For each state, the targeted population was grouped into three clusters: rural, city, and big city. We randomly chose one district from each cluster to ensure the representativeness of respondents from rural and urban (city and big city) areas. We obtained a total of twelve districts (three districts for each state).
Secondly, stratified sampling was applied. Each of the three chosen districts in stage one were further stratified into two sub-areas based on the characteristics of housing estates of majority Malay and majority non-Malay. This was to ensure sufficient non-Malay representation in the sample. We randomly chose one majority Malay and one majority non-Malay housing estate from each district. Thus, a total of twenty four housing estates were chosen. Finally, we utilized snowball sampling in obtaining respondents aged 60 and over from each housing estate. The number of respondents from each housing estate was predetermined with a total of 1414 respondents being interviewed. The responses were checked and we found that the distribution of respondents by gender was comparable to that of the true population while, by race, the composition of Malay is higher by 7%.
Variables
In this study, doctor consultations or visits (DOCTOR) and in-patient stays (IN-PATIENT) were used to represent the demand for healthcare. The respondents were asked if they had visited a doctor, whether a public or private provider, in the past one month and whether they had been hospitalized in the past twelve months before the interview. Though the exploratory variables were selected based on past and current studies, which also included environmental factors, we divided them into three main categories based on Andersen and Newman’s (2005) individuals’ determinants. Predisposing factors consist of inherent factors that exist within individuals and other socioeconomic factors that we assume exist prior to illness. In this study, the predisposing factors are age, gender, ethnicity, education level, and economic activity. Ethnicity is included to pick up the effect of health belief. Engagement in exercise activities, diet, and smoking behavior are also included in this category as proxies of individual attitude toward healthcare-seeking behavior. They measure, controlling for other factors, the direct effect of individuals’ attitudes toward healthcare consumption. We presume that those who exercise and are vegetarians are those with positive attitudes toward healthcare consumption, and those who smoke are the opposite.
Other factors, including individual, family, and community resources that are able to influence healthcare use, are categorized as enabling factors in this study. We include marital status, income, living arrangements, social capital, medical insurance, district, over-the-counter (OTC) market, and alternative care as control variables in this category. We categorize marital status and living arrangements as enabling factors rather than predisposing because we want to identify the role of partners or family members as a source of alternative care to formal care, or it can be treated as a source of moral support to individuals seeking care. Social capital is measured by informal interaction within the community and the level of trust placed in the society. The district variable is included as a proxy for healthcare supply, or it can also be considered a predisposing factor if it represents the overall socioeconomic status of the people.
The over-the-counter services and alternative healthcare which represent supply of care may act as a substitute or be complementary to doctor visits. The last category is need factors. Factors that represent the need for medical care may include perceived need by individuals or evaluated needs by medical providers. Need factors used as control variables in this study comprise three self-reported health conditions—i.e., self-assessed health status, the existence of longstanding health problems, and the highest three types of health problem reported by the respondents. The definition and summary statistics of each variable used in the demand model are presented in Table 1.
Table 1 shows that 45.8% of respondents had doctor visits in the past one month before the interview, while 10.2% had been in-patients in the past 12 months prior interview. The average age was 69 years old. Slightly more than half of the respondents were men, 61.2% were Malay and 72% were married. Although the respondents were selected elderly aged 60 and over, they perceived their health status as quite good. The mean of self-perceived health is 1.5, where 1 is good and 3 is poor. Despite the good self-perceived health, 67.6% have been suffering from at least one longstanding illness. Three longstanding health problems are high blood pressure (42.4%), diabetes (23.8%), and problems concerning arms, legs, hands, feet, back, neck, joints, arthritis, and rheumatism (24.6%).
Empirical Specification
The probit model is used in estimating the utilization models. Assume that for each elderly, there is a latent variable that represents his or her unobserved utilization of doctor and in-patient services. This unobserved utilization is associated with the predisposing, enabling, and need variables of the elderly (x i ). Let y * represent this latent variable and assume that y * is a linear function of x i ; then,
where
- y * :
-
unobserved demand on healthcare
- x :
-
independent variables
- u :
-
error term
Let y be the random variable that represents the observed outcomes such that the value of y is observed as y = 1 if the elderly have utilized healthcare services and 0 otherwise. Assume that the error term in the latent Eq. (1) follows a normal distribution, and we have the probit model. The probability that the elderly have an observed outcome of utilization for healthcare (y = 1) or otherwise (y = 0) is given below:
Here Φ is the cumulative standard normal distribution function. The maximum likelihood parameter estimates (MLE) are obtained by maximizing the following log likelihood function:
with respect to β. The model is estimated with the robust variance estimator.
Findings
Doctor Visits (Doctor)
The goodness of fit test for the estimated probit model suggests that the estimated probit model for doctor visits fits the data significantly with a p-value of almost zero and pseudo R square of 0.205. There is no evidence of general specification errors, with a p-value of 0.298. Thus, the estimated probit is found to have high goodness of fit statistically. In terms of multicollinearity among independent variables, the values of variance inflation factors (VIF) are found to range from 1.06 to 2.15 with a mean value of 1.4. Since the value is below the value of 10, the estimated probit model does not suffer a serious multicollinearity problem.
Table 2 presents the estimated probit model for doctor visits and in-patient stays. Table 2 shows that predisposing and enabling factors have limited roles in determining the likelihood of a doctor visit, except for age and the use of alternative care (ALT). This implies a good level of equity in utilization as it largely depends on need factors while controlling for other variables. The negative sign of age implies that the net effect of age is negative when we control for other variables for respondents within the age group under consideration. The higher the age, the lower the net effect on doctor visit. In other words, with the same level of health status, for example, the likelihood of a visit drops as age increases. This may be due to some mobility problems among older people or the preference not to utilize formal care.
The use of alternative care has increased the likelihood of doctor visits, showing its complementary role to formal care. This shows that the elderly who seek alternative care from, for example, traditional healers and acupuncturists are still utilizing formal care. The dependency on alternative care is rather small in this study with only a 7.9% utilization rate.
Individual total income has no significant effect in the model, which suggests that there is no income-related inequity for doctor utilization. This is a good indicator for a good health system, which suggests that utilization should be based on health status rather than other factors. Health-related variables that represent the need for health services show a significant effect at the 1% level, except for ARMS. Those with longstanding illness, diabetes, or high blood pressure are more likely to visit a doctor. These findings are consistent with many other healthcare demand studies that suggest health status as the main determinant of healthcare utilization (Dunlop et al. 2000; Liu et al. 2012; Sarma and Simpson 2006).
In-Patient Stays (In-Patient)
Table 1 shows that 10% of the respondents had been in-patients in the 12 months prior to the interview. There is evidence of general specification error, with a p-value of 0.018, which may be due to high zero occurrences in the dataset. Therefore, we estimated the model using skewed probit (for a detailed specification, refer to Nagler 1994) and the result is reported in Table 2. It is found that, besides age, being a man, a smoker, or having an insurance policy increases the probability of being an in-patient. This shows that socioeconomic factors also influence the probability of being hospitalized, though we expect that factors other than health status are less important. This is because, ideally, hospital admission should be highly determined by one’s health condition, controlled by the doctors. However, admission to private hospitals may also be determined by the ability of the patients to pay, which in our study can be proxied by insurance ownership. The time constraints and opportunity costs faced by women are also higher than for men, thus deterring them from accessing health services. Women usually need their husbands’ permission to seek healthcare and they also do not have easy access to household funds.
In addition, the level of education and exercise, social interaction, and the use of over-the-counter medications have reduced the probability of being an in-patient. All these variables have the same direction but with no significant effect in the model of doctor visits. The effect of education is consistent with Grossman’s model (1972). Those with higher education will be able to improve their health efficiently, and therefore they demand less healthcare, as is also found in Laroche (2000). Older people who are actively involved with the community, such as chatting informally at the coffee shop or with neighbors, are less likely to be in-patients. This informal interaction may be the platform to exchange ideas about life, health, and medical care, which in turn becomes a source of non-formal healthcare. Another substitute to formal care is the utilization of over-the-counter medications. Utilizing over-the-counter medications may be convenient to some people, especially the elderly. Health factors which include self-assessed health, the prevalence of longstanding illness, and diabetes have significantly increased the probability of being hospitalized.
Discussion
The increase in life expectancy has caused the proportion of elderly people in the country to rise. The elderly are prone to various health problems due to the decline in their immune systems. According to Grossman (1972), age is a depreciation factor to health capital, which implies that the use of health products is required to compensate for the decline of the capital. The influence of health state on the probability of healthcare utilization shows how well our health system has been operating. An equitable healthcare utilization should be based on health status or, in some cases, demographics (Andersen and Newman 2005), but not other enabling factors. Therefore, this study aimed to understand this issue by identifying the factors that influence the utilization of healthcare. Our target was the elderly aged 60 and over in the northern region of Malaysia. We focused on two types of utilization, being doctor visits and in-patient stays.
A probit model was used to identify the determinants of these two types of utilization. From the analysis, we found that the predisposing and enabling factors played a very minimal role in the doctor visits model. Nevertheless, attention should be given to the accessibility of services, since age was significant in determining doctor visits in this study. Studies shows that the association of age and use were mixed based on the characteristics of the population under investigation. These effects should be carefully inferred, as different studies concentrate on different age groups. Many studies on working age groups have found positive effects of age, as in Deb et al. (2006), Koc (2005), and Zimmer and Trivedi (2006) within the US context, and Pohlmeier and Ulrich (1995) for data on Germany. Our study shows that the older respondents, ceteris paribus, have a lower probability of doctor visits. Within the elderly population, Deb and Trivedi (1997), using the US dataset, also found a negative effect of age among the ill group on physician office and outpatient visits but a positive effect among the same group on emergency visits and hospital stays. Schellhorn et al. (2000), on the other hand, found that age has no significant effect on primary and specialist visits in Switzerland. The negative effect may be due to some very old adults who may have mobility problems and thus cannot reach formal care. Healthcare needs are sometimes hidden and it requires health services to identify those really in need (Bień et al. 2013). In dealing with this observable fact, the mobile hospital concept may be expanded in the elderly populated areas.
We also try to establish the influence of ethnicity and education to pick up the effect of health beliefs. Different ethnicities and cultures may shape different attitudes toward healthcare utilization. For example, older Malays may substitute formal care with traditional informal care. However, we found that the utilization of Malays (62% of sample size) has no significant difference from other ethnicities, which include Chinese, Indians, and other minorities, though various studies show an association between ethnicity and use (Andersen and Newman 2005; Brown et al. 2004). Education level also does not affect doctor visits in the study. The influence of predisposing and enabling factors is more obvious in the in-patient stays model. Once again, age is significant. This shows as the person gets older, the probability of utilization decreases. This condition may be caused by various factors, such as mobility problems or a preference for the use of informal services. The effects of smoking and exercise are not consistent with the assumption at the beginning of the study. In this study, smokers and level of exercise are seen as a proxy for health-seeking behavior. They measure, controlling for other factors, the direct effect of individuals’ attitudes toward healthcare consumption. We presumed that those who exercise have positive attitudes towards healthcare consumption and hence utilize more, and those who smoke are the opposite. However, in this model, it was found that being a smoker increased the probability of hospitalization, while higher levels of exercise decreased it.
The significant positive effect of insurance found in this study has enlightened us about something important related to equity in healthcare utilization. This indicates that the ability to pay has somewhat determined the likelihood of in-patient stays, which may be induced by medical suppliers, especially those from private facilities. Within the Malaysian context, although insurance ownership has been associated with higher utilization in private rather than public hospitals (Abu-Bakar and Samsudin 2016; Samsudin et al. 2012), the supplier-induced demand phenomenon cannot be certain here as we did not differentiate the types of service. The respondents may utilize both types of service and could have more than one utilization episode. Nevertheless, our findings are consistent with the findings of Deb and Trivedi (1997), Ekman (2007), Sarma and Simpson (2006), and Zhou et al. (2014). The significant effect of insurance, controlling for health status, is an indication that those with insurance are risk averse and may be over-utilizing healthcare. From the analysis, it was also found that informal interaction with society reduces the likelihood of hospitalization. In the literature on social capital, the interaction takes two forms, these being horizontal interactions (within the community) and vertical interactions (with government agencies or other parties outside the community). Similar findings were found in Laporte et al. (2008) for Canada. However, Pitkin and Varda (2009), from a systematic review of 21 studies, found inconclusive results.
Utilization of over-the-counter medication has negatively influenced in-patient stays, which may be due to awareness and the preferences of the respondents. Elderly people take preventive measures by purchasing medications that could enhance their health status, which later reduces formal care utilization. Another reason may be their self-preference. Older generations may prefer to stay in the comfort of their own house rather than being hospitalized and buy over-the-counter medicines from pharmacies or traditional Chinese medicine outlets. From the findings, it is evident that older age elderly utilize less healthcare, which may be due to preferences and mobility problems. In this respect, establishment of an integrated health program could be useful, particularly at the location where there are many elderly. In the US, an integrated care service known as PACE (Program of All-inclusive Care for the Elderly) has been serving about three million elderly (Bodenheimer 1999). Even though there are challenges and limitations, an integrated health service is still the most important and efficient alternative compared to a single model of care. Many researchers have agreed that a fragmented system of healthcare provision and financing does not meet people’s needs (Booth et al. 1997; Weiner and Stevenson 1998). Integrated healthcare is unique in that it involves an interdisciplinary healthcare group including physicians, psychologists, social workers, occupational therapists, and physical therapists, depending on the needs of the patient. Besides, health workers from the Ministry of Health, who may be part of the program, could be trained in the diagnosis and management of, for example, high blood pressure and diabetes. By engaging trained health workers in these informal interactions, such a program would be beneficial; thus the healthcare demand of the elderly can be well managed by the authority.
As expected, most of the need factors are significant in determining the probability of in-patient stays with the expected signs which are consistent with most healthcare demand studies (Deb and Trivedi 1997; Dunlop et al. 2000; Liu et al. 2012; Pohlmeier and Ulrich 1995; Santos-Silva and Windmeijer 2001). Thus health promotion and education programs are vital to promote better population health so that the unnecessary utilization of secondary care can be controlled. This measure is important as the costs of providing secondary care are high.
Conclusion
Understanding factors that affect healthcare utilization by the elderly is vital for the health system to be more responsive in providing care to this special group. Since healthcare utilization studies at micro level are rather limited within the Malaysia context, this research attempts to reduce the gap by focusing on this special group. This study identified the determinants of healthcare demand by the elderly in the northern region of Malaysia that includes four states: Kedah, Perlis, Penang, and Perak. The determinants were divided into predisposing, enabling, and need factors. Healthcare demand in this paper was measured by visits to doctors and in-patient stays. Multistage cluster sampling was used in selecting the sample for the study. A total of 1414 respondents aged 60 to 98 were interviewed face-to-face using a structured questionnaire. A probit model was used in estimating utilization equations. Except for the need variables, most predisposing and enabling factors were not statistically significant in affecting doctor visits. Unlike doctor visits, apart from need factors, some predisposing and enabling factors were significant in determining in-patient stays. Health-related variables remain the most significant factors that determine healthcare utilization in the area of study, which suggests that government policies to improve population health may influence the level of healthcare use in the future. Due to financial constraints, we focus only on the northern region of Malaysia. The same study may be replicated to the whole of Malaysia with a larger sample of respondents.
References
Abu-Bakar, A., & Samsudin, S. (2016). Determinants of health care seeking behavior: does insurance ownership matters? International Journal of Economics and Financial Issues, 6(S7), 6–11.
Aday, L. A., & Andersen, R. M. (1974). A framework for the study of access to medical care. Health Services Research, 9(3), 208–220.
Aday, L. A., & Andersen, R. M. (1981). Equity to access to medical care: a conceptual and empirical overview. Medical Care, 19(12), 4–27.
Alderman, H. & Gertler, P. (1989). The substitutability of public and private health care for the treatment of children in Pakistan, World Bank living standard measurement study Working Paper No. 57.
Andersen, R.M. (1968). Behavioral model of families’ use of health services. Chicago (IL): University of Chicago, Center for Health Administration Studies (Report No. 25).
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior, 36, 1–10.
Andersen, R. M., & Newman, J. F. (2005). Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly. Health and Society, 51(1), 95–124.
Atella, V., Brindisi, F., Deb, P., & Rosati, F. C. (2004). Determinants access to physician services in Italy: a latent class seemingly unrelated probit approach. Health Economics, 13(7), 657–668.
Bień, B., McKee, K., Döhner, H., Triantafillou, J., Lamura, G., Doroszkiewicz, H., Krevers, B., & Kofahl, C. (2013). Disabled older people’s use of health and social care services and their unmet care needs in six European countries. European Journal of Public Health, 23(6), 1032–1038.
Bodenheimer, T. (1999). Long-term care for frail elderly people—the on Lok model. New England Journal of Medicine, 41(17), 1324–1328.
Booth, M., Fralich, J., Saucie, P., Mollica, R. & Riley, T. (1997). Integration of acute and long-term care for dually eligible beneficiaries through managed care. Technical assistance paper prepared by the Muskie School of Public Service, University of Southern Maine, and the National Academy for state health policy, under a grant from the Robert Wood Johnson Foundation Medicare/Medicaid integration program.
Brown, P., Zavestoski, S., McCormick, S., Mayer, B., Morello-Frosch, R., & Gasior, R. (2004). Embodied health movements: uncharted territory in social movement research. Sociology of Health & Illness, 26, 1–31.
Deb, P., & Trivedi, P. K. (1997). Demand for medical care by the elderly. Journal of Applied Econometrics, 12(3), 313–336.
Deb, P., Munkin, M. K., & Trivedi, P. K. (2006). Private insurance, selection and the health care use: a Bayesian analysis of a Roy-type model. Journal of Business and Economic Statistics, 24, 403–415.
Department of Statistics Malaysia. (2010). State/district bank data. Malaysia: Putrajaya.
Department of Statistics Malaysia. (2011). Population distribution and basic demographic characteristics. Malaysia: Putrajaya.
Dunlop, S., Coyte, P. C., & McIsaac, W. (2000). Socio-economic status and the utilisation of physicians’ services: results from Canadian national population health survey. Social Science and Medicine, 51(1), 123–133.
Ekman, B. (2007). The impact of health insurance on outpatient utilization and expenditure: evidence from one middle-income country using national household survey data. Health Research Policy and Systems, 5(6), 1–15.
Gerdtham, U-G. & Trivedi, P.K. (2001). Equity in Swedish health care reconsidered: new result based on the finite mixture model. SSE/EFI working paper series in Economics and finance 365: Stockholm School of Economics.
Gertler, P., & van der Gaag, J. (1990). The willingness to pay for medical care in developing countries. Baltimore: Johns Hopkins Press.
Grossman, M. (1972). On the concept of health capital and demand for health. The Journal of Political Economy, 80(2), 223–255.
Gurmu, S. (1997). Semi-parametric estimation of hurdle regression models with an application to Medicaid utilization. Journal of Applied Econometrics, 12(3), 225–243.
Institute for Public Health. (2008). National Health and morbidity survey III. Ministry of Health: Kuala Lumpur.
Kasirye, I., Ssewanyana, S., Nabyonga, J., & Lawson, D. (2004). Demand for health care services in Uganda: Implication for poverty reduction. In MPRA paper 8558. Germany: University Library of Munich.
Koc, C. (2005). Health-specific moral hazard effects. Southern Economic Journal, 72(1), 98–118.
Laporte, A., Nauenberg, E., & Shen, L. (2008). Aging, social capital, and health care utilisation in Canada. Policy and Law, 3(04), 393–411.
Laroche, M. (2000). Health status and health services utilisation of Canada's immigrant and non-immigrant populations. Canadian Public Policy, XXVI(1), 51–75.
Lim, K. L., Jacobs, P., & Klarenbach, S. (2005). A population based analysis of health care utilisation of persons with back disorders. Spine, 31(2), 212–218.
Litaker, D., Koroukian, S. M., & Love, T. E. (2005). Context and healthcare access: looking beyond the individual. Medical Care, 43(6), 531–540.
Liu, L. F., Tian, W. H., & Yao, H. P. (2012). Utilization of health care services by elderly people with national health insurance in Taiwan: the heterogeneous health profile approach. Health Policy, 108(2–3), 246–255.
Ministry of Health. (2016). Malaysia national health accounts: health expenditure report 1997–2014. Putrajaya: Malaysia National Health Accounts Unit Planning division.
Nagler, J. (1994). Scobit: an alternative estimator to logit and probit. American Journal of Political Science, 38(1), 230–255.
Nandakumar, A. K., Chawla, M., & Khan, M. (2000). Demand for outpatient health care in Egypt: perception and reality. World Development, 28(1), 187–196.
Norstrand, J. A., & Xu, Q. (2012). Social capital and health outcomes among older adults in China: the urban and rural dimension. The Gerontologist, 52(3), 325–334.
Pitkin, D. K., & Varda, D. M. (2009). Social capital and health care access: a systematic review. Medical Care Research and Review, 66(3), 272–306.
Pohlmeier, W., & Ulrich, V. (1995). An econometric model of the process two-part decision making process in the demand for health care. The Journal of Human Resources, 30(2), 339–356.
Poulsen, T., Siersma, V. D., Lund, R., Christensen, U., Vass, M., & Avlund, K. (2012). Impact of social capital on eight-year mortality among older people in 34 Danish municipalities. Journal of Aging and Health, 24(7), 1203–1222.
Puentes-Markides, C. (1992). Women and access to health care. Social Science and Medicine, 35(4), 619–626.
Rabieyah, M. & Hajar, M.T. (2003). Socio-economic characteristics of the elderly in Malaysia. Kyoto, Japan: Analysis of the 2000 Round of Censuses: 21st Population Census Conference 19–21 November 2003.
Rose, R. (2000). How much does social capital add to individual health? Social Science & Medicine, 51(9), 1421–1435.
Samsudin, S., Jamil, N., & Zulhaid, N. H. (2012). Health care utilisation in Kedah: a microeconometric analysis. OIDA International Journal of Sustainable Development, 4(5), 45–52.
Santos-Silva, J. M. C., & Windmeijer, F. (2001). Two-part multiple spell models for health care demand. Journal of Econometrics, 104(1), 67–89.
Sarma, S., & Simpson, W. (2006). A microeconometric analysis of Canadian health care utilization. Health Economics, 15(3), 219–239.
Schellhorn, M., Stuck, A. E., Minder, C. E., & Beck, J. C. (2000). Health services utilization of elderly Swiss: Evidence from panel data. Health Economics, 9(6), 533–545.
United Nations Population Fund (UNFPA). (2012). Ageing in the twenty-first century: a celebration and a challenge. New York: UNFPA.
Van Doorslaer, E., Masseria, C., & Koolman, X. (2006). Inequalities in access to medical care by income in developed countries. Canadian Medical Association Journal, 174(2), 177–183.
Wan, T. T. H., & Odell, B. G. (1981). Factors affecting the use of social and health services among the elderly. Ageing and Society, 1(1), 95–115.
Weiner, J. M., & Stevenson, D. G. (1998). State policy on long-term care for the elderly. Health Affairs, 17(3), 81–100.
Windmeijer, F. A. G., & Santos-Silva, J. M. C. (1997). Endogeneity in count data models: an application to demand for health care. Journal of Applied Econometrics, 12(3), 281–294.
Wolinsky, F. D., Coe, R. M., Miller, D. K., Prendergast, J. M., Creel, M. J., & Chavez, M. N. (1983). Health services utilization among the noninstitutionalized elderly. Journal of Health and Social Behavior, 24(4), 325–337.
Yu, C. P., Whynes, D. K., & Sach, T. H. (2008). Equity in health care financing: the case of Malaysia. International Journal for Equity in Health, 7(1), 15.
Zhou, Z., Zhou, Z., Gao, J., Yang, X., Yan, J., Xue, Q., & Chen, G. (2014). The effect of urban basic medical insurance on health service utilisation in Shaanxi province, China: a comparison of two schemes. PloS One, 9(4), 1–12.
Zimmer, D.M., & Trivedi, P.K. (2006). Using trivariate copulas to model sample selection and treatment effects: Application to family health care demand. Journal of Business & Economic Statistics, 24(1), 63–76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Universiti Utara Malaysia (PBIT: S/O Code: 123182).
Conflict of Interests
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Samsudin, S., Abdullah, N. Healthcare Utilization by Older Age Groups in Northern States of Peninsular Malaysia: The Role of Predisposing, Enabling and Need Factors. J Cross Cult Gerontol 32, 223–237 (2017). https://doi.org/10.1007/s10823-017-9318-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10823-017-9318-4