Abstract
The dramatic increase in the aging population in developed countries has led to an explosion of research on health and aging in the United States. Few studies, however, have been conducted in developing countries, even though many of these populations are experiencing a faster rate of growth in the 65+ population. Thus, although our knowledge of health and aging has increased, our knowledge of the variation in health as people age is limited. While the numbers of older adults is increasing in Africa, very little is known about the health and well-being of African elders. Recently, a growing number of researchers have focused on the plight of elders who find themselves caring for orphaned grandchildren. While several anecdotal reports have suggested that this new burden negatively impacts their health, there are few studies that systematically examine the health of African elders. As part of the Kenyan Grandparents Study, the health of 287 grandparents (age 73 ± 8) was examined using multiple methods including objective measures, clinical history, physical examination, and a modified version of the SF-36. Although all health variables were correlated with each other, different patterns were found between predictor variables and the various measures of health. Caregiving status was only associated with mental health, with caregivers having better mental health than non-caregivers. Age was associated with poorer health as measured by several SF-36 scales, physical exam, and body mass index (BMI). Women generally had a greater number of health complaints and lower quality of life as measured by the SF-36. Higher socioeconomic status was associated with better health as measured by physical exam, clinical history, SF-36, and BMI. Caring for a greater number of orphans was associated with better health on examination but no other measure of health. More social support was associated with better physical function and general health as measured by the SF-36. These data suggest that there is no strong evidence that caregiving results in poor health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the wake of the HIV/AIDS crisis, African grandparents are taking on more responsibility for their grandchildren’s care. In 2005, an estimated 24.5 million Africans were living with HIV/AIDS, accounting for approximately 64% of global HIV/AIDS cases (UNAIDS 2006). The adult population of 15- to 35-year-olds is most heavily affected, resulting in a loss of the general workforce, parents, teachers, and caregivers for the elderly. The high mortality rate of adults with HIV/AIDS has produced approximately 12 million orphans whose care has largely been left to grandparents and other relatives (UNAIDS 2006). As the working-age adults fall ill and die, HIV-affected households are reported to experience a decrease in household income, health, and food security (HelpAge International 2002; UNAIDS 2006; UNICEF 2003). Reports by the Joint United Nations Programme on HIV/AIDS (UNAIDS) and HelpAge International suggest that elderly Africans do not have the social and economic resources to care for orphaned grandchildren and are at risk of ill health, but few studies have systematically measured and compared the health status of caregivers and non-caregiving peers (HelpAge International 2002; UNAIDS 2006; UNICEF 2003).
Extended family, primarily grandparents, care for 90% of orphaned children in sub-Saharan Africa (UNICEF 2003). By 2010, approximately 6% of all African children under 15 will be orphaned due to AIDS alone. In several countries, the prevalence of AIDS orphans will be as high as 15% (UNAIDS/UNICEF 2002). The caregiving burden of grandparents is increasing. For example, in Namibia, the proportion of orphans cared for by grandparents rose from 44% in 1992 to 61% in 2000 (UNICEF 2003). Female-headed households are disproportionately affected and least likely to be able to economically sustain orphans. While grandparents in Africa are traditionally active participants in the care of grandchildren, they are taking on a new level of responsibility as they become the sole caregivers for multiple children. In many cases, as they lose their adult children, the elderly not only increase their responsibility but also lose their main source of economic support. While there is little systematic evidence, these increasing responsibilities are believed to make elders more vulnerable to nutritional deficiency and ill health (Agyarko et al. 2000; HelpAge International 2002; UNAIDS/UNICEF 2002). In fact, the AIDS pandemic has been called the “grandmother’s curse” because they are believed to be silent victims of the pandemic (Wilson and Adamchak 2000).
Several studies have documented elders’ concerns about the burden of caregiving and its consequences with respect to elder well-being. Initial reports from a World Health Organization investigation, which was conducted in Zimbabwe, Ghana, South Africa, and Tanzania, suggested that caregiving leads to considerable distress for older adults (Agyarko et al. 2000). The majority of caregivers are elderly women who have been reported to be particularly ill-equipped to care for orphans (Nalagoda et al. 1997; Nyambedha et al. 2001; Williams and Tumwekwase 2001). The primary problems for caregivers identified by Agyarko et al. (2000) were: the loss of financial support, lack of food and clothing, cost of medical fees, inability to pay school fees for orphans, and diminished livelihood opportunities. In South Africa, a death in the household and subsequent changes in living arrangements have been reported to negatively impact elders socioeconomic well-being (Ogunmefun and Schatz 2006). Elders in central and eastern Uganda reported more financial problems, distress, and health problems as a result of caring for sick children as well as anxiety over fostering orphaned grandchildren (Ssengonzi 2007). Kakooza and Kiumuna (2005) reported that among elder-headed households in the Kayunga District of Uganda, elders had on average three orphaned children who were of school-going age. This translated into a potential cost of $49–$569 per household in school related expenses, depending on the number of children and type of school that they attended. They noted that very few elder-headed households would be in the position to meet these needs, and elders in their study reported particular anxiety; however, they did not measure the actual cost to elders nor did they compare to non-caregiving elders.
In addition to financial strain, Williams and Tumwekwase (2001) report that elderly Ugandan caregivers suffer from inadequate food resources and emotional distress. Gilborn et al. (2001) report that 79% of guardians for orphans in Uganda report that they are in poor or very poor health. Unfortunately, many of these studies are descriptive, include small sample sizes, and lack an appropriate comparison group, so the impact of caregiving on elders remains inadequately understood. In an unpublished electronic report with a larger sample size, Ainsworth and Dayton (2000) report that Tanzanian elders who had a loss of a working-age adult had higher body mass indices (BMIs) than those who had no such loss. After controlling for socioeconomic status, which influences infection rates, they report that there is no difference in BMI between elders experiencing a loss and those who have not. Based on unpublished data, they suggest that funds for food are preserved at the expense of other economic needs. In a review of nutrition among elders, Charlton and Rose (2001) note, “the potential devastating socioeconomic and demographic impact of the AIDS pandemic, together with the psychosocial burden of caregiving, loneliness and bereavement associated with the outcomes of the disease, is likely to be a major determinant of health status, including nutritional status of older Africans” (p. 2427S).
Caregiving might be expected to impact health through a number of mechanisms. Luo primary caregivers in Kenya report higher parenting stress than part-time caregivers (Oburu and Palmerus 2005). Stress can contribute to ill health and is particularly known to impact the cardiovascular, immunological, gastrointestinal, and endocrine systems (McEwen 2001, 2002; McEwen and Wingfield 2003; Sapolsky 1996). Elders are particularly vulnerable to the negative consequences of stress (Frolkis 1993; Sapolsky et al. 1987; Sapolsky 1999). Socioeconomic status is commonly associated with poor health (Grundy and Sloggett 2003; Lima-Costa et al. 2003, 2005). As caregiving has been reported to be a strain on the financial resources of elders, a decrease in socioeconomic status can result in declining health status. Good nutrition is essential for good health. If, as has been reported, caregivers are not able to get adequate nutrition, then they could be expected to have declining health as a consequence. Finally, children are more susceptible to infectious disease; therefore, those elders living in close proximity to children may suffer from a greater incidence of infectious diseases.
This paper examines the impact of caregiving on the health of Kenyan Luo elders. This paper reports on a small portion of a larger study, the Kenyan Grandparents Study (KGS), which examines the impact of caregiving on physical health, stress, and nutrition of older adults in western Kenya. The specific aims of this paper are to compare health status between caregivers and non-caregivers and to examine predictors of health among Luo grandparents using a variety of subjective and objective measures of health. It was hypothesized that caregivers would have poorer health status than non-caregivers and that those with more orphans would be more likely to suffer ill health. Socioeconomic status (SES) and the number of orphans under an elder’s care were hypothesized to be negatively correlated with health status of elders. Social support and child assistance were expected be associated with better health.
Methods
Sample
Study population
According to the US Census Bureau, 4% of the Kenyan population is over the age of 60 years (Bureau 2006). By 2050, it is predicted that 13.2% will be over 60 years (Bureau 2006). Kenya is currently the 17th hardest hit country in Africa with a 6.1% HIV prevalence rate (UNAIDS 2006). Kenya has experienced a decrease in rank (from ninth) partially due to a decrease in prevalence but also due to an increase in prevalence in other African countries (UNAIDS 2006). However, Nyanza Province in Western Kenya has a prevalence rate that ranks among the highest on the continent (UNAIDS 2006). An estimated 30–39% of adults living in Nyanza Province are infected with HIV with no signs of a decrease in prevalence in the near future (Nyambedha et al. 2001; UNAIDS 2006). While exact numbers have not been published, a large portion of the 1.1 million orphans of Kenya reside in Nyanza Province (Nyambedha et al. 2003a; UNAIDS 2006; UNAIDS/UNICEF/WHO 2002).
Luo are the third largest ethnic group in Kenya and the primary inhabitants of Nyanza Province in Western Kenya (National Council for Population and Development 1999). Luo are primarily subsistence farmers and pastoralists with some additional income based on fishing, small-scale gold mining, and migrant work (Nyambedha et al. 2001; Ochieng’ 1985; Ocholla-Ayayo 1999). Luo are patriarchal and patrilocal (Ochieng’ 1985; Reynar 2000). Luo live in homesteads (dala), which consist of a father, his wives, and their children and married sons’ families (Geissler et al. 2000; Ocholla-Ayayo 1999). Polygynous marriage is common, and men typically dominate over many aspects of women’s lives (Opiyo 1996; Reynar 2000). There is a clear division of labor, with women being responsible for most household chores, farming, and caregiving (Opiyo 1996). Women have little control over family income, as they cannot own land and are less likely than men to participate in wage labor (Buzzard 1982; Opiyo 1996). Luo traditionally practice “wife inheritance” where the widow remarries someone from her husband’s family and is allowed to remain on her husband’s property. This tradition is generally seen by the Luo as a way to ensure the care of the widow and her children (Reynar 2000); however, this tradition is declining in the context of AIDS due to fear and stigma (Nyambedha et al. 2003a). As a result, many widows and orphans lose rights to their husband’s property and all of the resources that come with it (Nyambedha et al. 2003a). Therefore, the impact of caregiving is likely to be greatest on women. Many Luo older adults have limited education, and thus, there is a high level of illiteracy. Children may contribute to the household income through fishing and collecting and selling firewood, and they often assist with childcare, fetching water and firewood, and herding cattle (Geissler et al. 2000).
Nyanza province has experienced steadily increasing poverty, which has been accelerated in many communities due to HIV/AIDS (National Council for Population and Development 1999; Nyambedha et al. 2003b). Many of the regions within Nyanza province are prone to flooding, which leads to frequent crop failure. Nyambedha et al. (2003b) suggest that the elderly, due to the loss of adult children who are expected to care for them and the addition of dependent children, are disproportionately impacted by the economic downturn. Among the Luo, old age was traditionally a time to slow down and be supported. Elders have relied on their sons to provide economically and their daughters-in-law to perform household tasks. Now, many elders find themselves participating in farming activities and household chores that were traditionally relegated to the young (Nyambedha et al. 2003b). Young Luo women spend approximately 2 hours per day fetching water, 4 hours preparing food and cleaning, and 2 hours a day on agricultural work (Cook 1990). The loss of their daughters-in-law may result in a significant increase in activity for grandmothers. On the other hand, grandparents may adapt to their increasing workload by recruiting orphans to do tasks typically reserved for working-age adults. Therefore, the loss of working-age adults may affect the energy balance of elders and/or orphans by increased working load independent of nutritional intake.
Sample
Two hundred eighty-seven Luo grandparents (age 73 ± 8) participated in this study. A non-random sample of participants were recruited from 18 villages within two districts of Nyanza Province, Nyando, and Kisumu Rural with the assistance of the local chiefs. Approximately half of the grandparents were caregivers and half were non-caregivers. To be considered a caregiver, the participant was over 60, a grandparent and caregiver for at least one orphaned grandchild. Non-caregivers were over 60, grandparents, and were not the primary care provider for orphaned grandchildren. Consent to participate in the study was obtained for each of the grandparents by a native speaker of Dholuo following a protocol approved by the Kenya Medical Research Institute ethics board and the Ohio University Institutional Review Board. Selected sample characteristics are displayed in Table 1.
Data collection methods
Demographic information and risk factors
Each grandparent participated in an interview conducted in Dholuo by a trained research assistant. Data collected included demographic information, household composition, caregiving intensity and burden, and questions to assess general wealth. Household composition was determined by asking detailed questions about the age, relationship and gender of each adult and child in the homestead. The number of children in the homestead and the number of orphans under the elders care were calculated for this analysis. The participants were also asked about the number of children they have to assist them on a variety of tasks and social functions. These were summed to use in the analysis. To assess social support, participants were asked if they had someone to turn to for assistance with a number of common tasks and situations requiring emotional support. The social support scale had a Cronbach’s alpha = 0.83 and was associated with family size (p = 0.001) and SES (p = 0.002). The socioeconomic status scale was based on a scale used in Kenya by the Demographic Health Survey (National Council for Population and Development 1999). This scale has a series of questions about income and material wealth. For example, participants are asked how many livestock they have, materials with which their houses were made, and ownership of a series of material goods. This scale and similar scales have been widely used in subsistence-based economies. Data were collected via PalmPilots® using Entryware® software.
Subjective measures of health
A series of questions were used to assess elders self-perceived or subjective health. Perceived health and functional status of the Luo grandparents were measured via an adapted version of the SF-36 (Wagner et al. 1999). The SF-36 (MOS Short-Form 36) is a scale made up of 36 questions asking about perceived health and functioning on a variety of domains in the following subscales: mental health (general mental health including distress and well-being), function (limitations due to physical health problems), role physical (limitations in physical activities due to physical or emotional problems), role social (limitations in social activities due to physical or emotional problems), social functioning (limitations in role activities due to emotional problems), general health (self-rated health), vitality (energy and fatigue), and pain (general pain; Ware and Sherbourne 1992). The SF-36 is used as a measure of health-related quality of life and a basic measure of perceived health. It has been used in more than 4,000 publications and is currently being used in a large quality of life survey in more than 50 countries (Ware 2007). The version used in this project was culturally adapted and validated for use in an African context but retains all subscales of the standard SF-36 (Wagner et al. 1999; Wyss et al. 1999). The higher the score on each subscale, the greater the quality of life or better health/ function.
In addition to the SF-36, a full clinical history was obtained from each participant. The clinical history covered the following systems: cardiovascular, respiratory, gastrointestinal, genital/reproductive, urinary, musculoskeletal, endocrine, neurological, psychiatric, and integumentary (skin) and also asked questions pertaining to past medical history and illnesses. Participants were asked questions about symptoms pertinent to each system above. For example, related to the urinary system, participants were asked if they had any sensations of burning with urination, hesitancy, urgency or increase in frequency. Each symptom was recorded, and a system was considered abnormal if a participant reported one or more symptoms per system. Clinical histories were obtained by a second year osteopathic medical student with the assistance of a local research assistant. For analysis, a sum of all “abnormal” systems was calculated.
Objective measures
Various objective measures were collected to assess the health and nutritional status of Luo grandparents. These measures include anthropometric measurements, blood pressure, and hemoglobin and blood glucose levels.
Eight anthropometric measurements were taken to assess nutritional status. Height was assessed with a GPM® anthropometer (nearest mm) and weight by an Omeron® scale (nearest kg). Height and weight were used to calculate the body mass index for each participant. A Harpending® skinfold caliper (nearest 2 mm) was used to obtain skinfold measurements (triceps, subscapular, suprailiac, and calf), and a tape measure (nearest mm) was used to obtain the circumference measurements (arm, waist, hip, and calf). Standard measurement procedures were used (Lohman et al. 1989).
Blood pressure was collected with the patient sitting and was taken using a standard blood pressure cuff according to arm size on the patient’s right arm. Measurements followed the standardized protocols of the SHEP (Systolic Hypertension in the Elderly Program) Study (Labarthe et al. 1991). A series of three measurements were taken with time between each measurement for the elder to rest. The mean of the three blood pressure measurements was used in analysis.
Sterile disposable lancets were used to collect blood for hemoglobin and blood glucose assessment using standard universal precautions. These assessments occurred in the morning, and the elders were asked to fast the morning of the study. A HemoCue® system was used to assess hemoglobin levels. Blood glucose levels were assessed using a Freestyle® Glucometer.
Each grandparent participated in a physical exam. The physical exam covered the following systems: cardiovascular, respiratory, gastrointestinal, musculoskeletal, neurological, and integumentary (skin). Participant physical exams were conducted by a local clinical officer and a second year osteopathic medical student. Abnormal (pathological) findings in the physical exam were recorded. For example, rashes or fungal infections were recorded as abnormal findings in the integumentary system. Each abnormal finding was recorded, and a system was considered abnormal if at least one sign of pathology was present. The number of abnormal systems were summed for analysis.
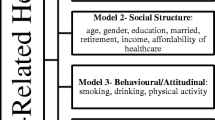
Analysis
Subjective and objective health measures were compared between caregivers and non-caregivers using a t test. The association between socioeconomic status, social support, child assistance, number of orphans, and all measures of health were examined with Pearson correlation coefficients, with a p < 0.05 indicating a significant correlation. Correlations were examined in the whole population and with men and women separately, as there may be confounding by sex. A series post hoc analyses to examine potential confounding by sex was conducted by repeating the t tests and correlation analyses separate for men and women.
Results
Caregiving status was significantly associated with mental health as measured by the SF-36 (Table 2). Caregivers reported having better mental health than non-caregivers. Height differed across caregiving groups, with non-caregivers being taller than caregivers (Table 2). No other measures of health significantly differed across caregiving groups. Compared to men, women had more health complaints during the clinical history interview and reported lower quality of life on the mental health, function, general health, role physical, and pain subscales of the SF-36, although there was no difference in the physical exam scores (Table 3). Skinfold thicknesses were greater among women than men. Calf circumference and hemoglobin were higher among men compared to women. When the analyses were repeated separately for men and women, some different patterns emerged. Few variables differed across caregiving groups among women, but, generally, female caregivers were better off than female non-caregivers (Table 4). Female caregivers had higher subscapular skinfolds and BMI and reported better vitality on the SF-36. Male caregivers, on the other hand, generally were in poorer health than male non-caregivers (Table 4). Male caregivers had lower waist and calf circumferences, smaller skinfolds at every site, and lower BMI. Male caregivers, however, did report better mental health as measured by the SF-36.
The relationship between the health variables and predictor variables was also examined. The predictor variables investigated were number of children in the household, age, number of orphans living in the household, child assistance, social support, and SES. Although many of the health variables were correlated with each other, different patterns were found between predictor variables and the various measures of health (Table 5). Increasing age was correlated with lower scores on the SF-36 measure of function and general health, indicating greater disability and poorer health. Age was negatively correlated with physical function (SF-36), general health (SF-36), diastolic blood pressure, and BMI (Table 5). The number of children in the household correlated with better health, fewer findings on physical exam, higher SF-36 general health scores, and higher hemoglobin levels (Table 5). The number of orphans in the homestead was not associated with any health variables in the entire sample. Higher SES was correlated with fewer abnormal findings upon physical exam, fewer complaints in clinical history, better mental health and pain scores on the SF-36, and higher hemoglobin and BMI (Table 5). Greater child assistance was correlated with better mental health and lower reported pain. Social support was positively correlated with high physical function and general health. Many predictor variables were correlated with one another. The number of children in the household, the number orphans, and child assistance were correlated with one another. SES was correlated with the number of children in the household. Social support was positively associated with the number of orphans and children in the household.
When the correlations were repeated among women (Table 6) and men (Table 7) separately, the direction of the associations remained the same; however, some variables were significant only among one sex or the other. With increasing age, women reported poor function and general health, more pain, and lower BMI (Table 6). Women with more orphans had few findings on physical exam. Child assistance was positively associated with mental health and hemoglobin and negatively associated with pain among women; yet, women with more social support also reported higher pain. Higher socioeconomic status was associated with fewer complaints during the clinical history, lower pain, and higher hemoglobin levels. With increasing age, men also had poorer function and general health and BMI (Table 7). Diastolic blood pressure decreased among men with age. More children in the household and more orphans was associated with better general health among men. Men with more social support had higher function and general health. Higher socioeconomic status among men was associated with fewer findings on physical exam, better mental health, and higher BMI.
Discussion
Contrary to previous studies, these results suggest that there is no strong evidence that caregivers have poorer health than non-caregivers; however, the patterns are different among men and women. Several studies have previously documented that elder caregivers generally report poor health (Agyarko et al. 2000, 2002; Nyambedha et al. 2003a, 2003b; Williams and Tumwekwase 2001). While it is likely that the impact of caregiving on African elders will vary across populations and contexts, varying methodology may also account for the difference in findings. The majority of previous studies are qualitative in nature. In these studies, elders report that the addition of orphans to the household creates great financial burden, and they perceive their health and food intake as suffering as a result. Given these findings, one would expect that at least the subjective measures of health in the current study (SF-36 and clinical history) would differ across caregiving groups. Many previous studies lack a comparison group; thus, it is impossible to know if non-caregiving elders in those regions similarly report lack of resources and poor health. It is our experience that most participants complain about their health in general terms, and these complaints often fail to correspond with objective findings. In fact, in our sample, the only subjective measure of health that was associated with the findings of the physical exam is the SF-36 pain scale. Those that report more pain have more systems with pathology.
Similar to our own findings, Ainsworth and Dayton have noted in a series of reports that elders who become caregivers of orphans do not appear to have permanent health consequences (Ainsworth and Dayton 2000; Ainsworth and Filmer 2002; Ainsworth and Semali 2000; Dayton and Ainsworth 2004). They have found that the greatest impact is during the time at which elders are caregiving for sick children and that BMI is higher among elder caregivers than non-caregivers (Dayton and Ainsworth 2004). BMI was lowest among those households that were poorest and that did not experience a death. While it may be argued that BMI is a limited indicator of health status, the current study, using a wide variety of subjective and objective measures of health, similarly found little impact of current caregiving on health. Socioeconomic status, household composition, age, and gender were more important determinants of health status among Luo elders. The impact of caregiving may vary over time, as caregivers adjust to stress and strain on resources. Dayton and Ainsworth (2004) demonstrated that the impact of an adult death changes overtime. BMI was lower among elder households with a sick family member but rebounded after the death and was highest in the households that experienced the death in their last wave of data collection. Because the current study is a cross-sectional study, we cannot determine if elders initially have a decline in health and then rebound, nor can we look at how different variables might mediate or moderate the impact of caregiving over time.
Interestingly, women who were caregivers generally had better nutritional status than women who were non-caregivers. On the other hand, male caregivers had poorer nutritional status than non-caregivers. This is opposite of what one might expect given the fact that women reportedly shoulder a greater burden of caregiving than men (Abboud et al. 1990). It may be that women, who have few resources in this society, are able use orphans as an adaptive resource to help bolster their food intake and/or decrease their energy expenditure. Men on the other hand may only become caregivers as a last resort and may not have as much social support to assist them in caregiving. Other data from the project support the first possibility rather than the second. Women who are caregivers are more likely to be widowed, have fewer adults in the homestead than non-caregivers yet they report greater assistance from children. So, there are fewer adults to feed and more children to assist in household chores. This might lead to an increase in energy intake and a decrease in energy expenditure. Among men, there is no difference in marital status between caregivers and non-caregivers, but caregivers have more living siblings than non-caregivers. There is no difference in the reported assistance from children, social support or adults in the homestead between caregiving and non-caregiving men. Male caregivers may only experience a decline in food resources and not a benefit of reduced energy expenditure as orphans join their homesteads. Despite these differences in nutritional status, other health variables were improved in both men and women with children and orphans in the homestead and the associated child assistance, although different variables were affected in men and women.
Historically, the extended family has been responsible for caring for African elders; however, modernization, urban migration, changing family structures, and the HIV/AIDS pandemic may lead to changes in the nature of these support systems (Cliggett 2005). Although family support of elders might be the ideal in African cultures, the reality of such support is likely to vary based on availability of family and specific context. Cliggett (2005) notes, “Although support for the elderly might be the moral ideal, more realistically it is a flexible cultural norm operating within a context of individual and group factors” (p. 150).
It may be that in the context of declining social support due to social factors, the loss of support due to HIV/AIDS deaths has little additional impact. If children are old enough to assist in household and farming tasks, orphans may actually provide benefit to elder caregivers rather than a drain. Supporting this idea, mental health and general health were correlated with child assistance in this sample. In addition, social support was inversely related to reported child assistance with tasks. Perhaps, the elders with lowest support rely most heavily on orphans to fill the tasks that would otherwise be filled by working-age adults who are absent for any reason. This would generally act to minimize the impact of an adult death on elders’ health and well-being.
Little is known about the overall health and well-being of elder Africans (Cohen and Menken 2006). In a recent workshop on aging in Africa in Johannesburg, it was noted that it is generally believed that due to demographic change, modernization, and the impact of HIV/AIDS, the welfare of older adults in Africa is worsening, yet very little empirical data exist to document this belief. Similar to this study, 30% of older women and 18% of older men living in Nairobi reported being sick within the past 2 weeks (Ezeh et al. 2006). There is some evidence that some African countries are beginning to experience an epidemiological transition towards an increase in chronic degenerative diseases, but East Africa is early in the transition (Kahn et al. 2006). Compared to US elders, Luo elders in this study were more likely to be undernourished, with the mean of most measures falling around the fifth to tenth percentile of American elders. The average hemoglobin level in this sample (11.8 g/dl) is categorized as mild anemia; 51% of the sample would be classified as anemic. In the USA, approximately 11% of people more than 65 years are anemic (Woodman et al. 2005). Although the average blood pressure (128/74 mmHg) would be classified as pre-hypertensive by the The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) in the USA, it is lower than what is reported among similar aged adults in the USA and Europe (Cooper et al. 2005; Wolf-Maier et al. 2003; Wolf et al. 1997). The prevalence of hypertension in the sample (blood pressure ≥140/90) was 8.9%, 24.4% had systolic and/or diastolic hypertension. This is also well below US and European rates (Wolf-Maier et al. 2003). Few data on blood pressure on population-based, non-clinical samples of older adults are available for Africa, although average blood pressure rates reported here are similar to those reported for younger samples in Tanzania (Unwin et al. 2006) and Ghana (Kerry et al. 2005). The prevalence of hypertension is lower in this sample compared to those reported in the samples above. WHO reports a mean systolic blood pressure in Kenya of 119; however, this is from a sample of 15 years old and above (WHO 2005). Because the elders in this sample generally have poor health, there may be a floor effect which limits the ability to find a difference between caregivers and non-caregivers, but the health of caregivers does not appear to be worse than non-caregivers and may actually be better for some elders.
Other studies conducted on elderly populations have shown the importance of health and variables including SES, ethnicity, and social support. The Bambuí Health and Aging Study (BHAS) is a cohort study aimed at investigating predictors of undesirable health events in the elderly (Lima-Costa et al. 2000). The study took place in Bambuí, a town in southeastern Brazil, and included 1,742 elders more than 60 years of age. Interviews and various health assessments, including blood tests, blood pressure, and anthropometric measurements, were performed (Lima-Costa et al. 2000). Several papers of interest describing aspects of BHAS include those investigating socioeconomic position, health, and self-rated health. Elders with low family income were found to have risk factors that could contribute to poor health, including low consumption of fruits and vegetables and less exercise (Lima-Costa et al. 2003). These individuals also had a lower “General Health Questionnaire score” and a lower self-rated health score (Lima-Costa et al. 2003). Furthermore, results from this study showed that a relatively small difference in income allowed for the identification of elders in poorer health (Lima-Costa et al. 2000). The study found that the self-reported health of Bambuí elders was dependent on multiple variables including SES, social support, general health, and access to care (Lima-Costa et al. 2004). Social network was found to be a major factor in the self-rated health of the poorest individuals in the BHAS (Lima-Costa et al. 2005). Socioeconomic circumstance was also found to be important in the health outcomes of elders participating in the Health Survey for England (Grundy and Sloggett 2003). The results from this study found associations between poverty and an increase in poor health (Grundy and Sloggett 2003).
The limitations of the study should be recognized. Because the sample size was relatively small and this paper presents multiple comparisons, the significance of the correlations should be interpreted with caution. The approach to the clinical history and physical exam, while consistent with a clinical approach to patient diagnosis and management, has not been tested for reliability and validity. The cross-sectional nature of the study limits our evaluation of causation. Furthermore, this sample represents only two districts within Nyanza province and consists of primarily Luo participants and cannot be generalized to all Luo or all of Kenya. Many other districts in Nyanza province, where other studies have been conducted, are believed to have higher rates of HIV. The caregivers in this sample had fewer orphans under their care than have been reported in other studies. They may also have been advantaged relative to other caregivers in Africa because primary school in Kenya is now free unlike much of Africa. It is likely that the impact of caregiving varies widely with ecological and cultural context.
Given these limitations, this study is unique in that it examines both subjective and objective measures of health. The results support the conclusions previously presented by Dayton and Ainsworth in suggesting that elder caregivers do not all have poorer health (Ainsworth and Dayton 2000; Ainsworth and Filmer 2002; Ainsworth and Semali 2000; Dayton and Ainsworth 2004). The data do demonstrate, however, that Luo elders overall do experience ill health likely stemming from a lifetime of poor nutrition, high exposure to preventable infections, and minimal access to healthcare. In addition, several socio-demographic factors may be more important determinants of the health of elders overall.
While the AIDS crisis has dramatically reduced the number of working-age adults in African populations, the number of elderly in African nations has been and is expected to continue to grow. By 2050, the population of elders living in sub-Saharan Africa is expected to increase to 130 million (8.1% of the population). While the number of elders is increasing in Africa, very little is known about their health and well-being. Social services and healthcare systems have been ill prepared to respond to the HIV/AIDS crisis and are in no way capable of responding to the needs of a growing number of elders with chronic diseases (Smith and Mensah 2003). This project and others suggest that more attention to the health and well-being of African elders is needed.
References
Abboud, L., Beyar, R., Battler, A., Rat, M., Cohen, A., & Sideman, S. (1990). Analysis and prediction of left ventricular performance under load changes during cardiac catheterization. Annals of Biomedical Engineering, 18, 445–461.
Agyarko, R. D., Kalache, A., & Kowal, P. (2000). Older people, children and the HIV/AIDS nexus. Geneva: UNAIDS.
Agyarko, R. D., Madzingira, N., Mupedziswa, R., Mujuru, N., Kanyowa, L., & Matorofa, J. (2002). Impact of AIDS on older people in Africa. Zimbabwe Case Study. Geneva: World Health Organization.
Ainsworth, M., & Dayton, J. (2000). Is the AIDS epidemic having an impact on the coping behavior and health status of the elderly? Evidence from Northwestern Tanzania.
Ainsworth, M., & Filmer, D. (2002). Poverty, AIDS and children’s schooling: A targeting dilemma. World Bank Policy Research Working Paper 2885. http://www-wds.worldbank.org/external/default/WDSConentServer/IW3P/IB/2002/10/12/000094946_02100204022275/Rendered/PDF/multi0page.pdf.
Ainsworth, M., & Semali, I. (2000). The impact of adult deaths on children’s health in northwestern Tanzania.
Bureau, U. S. C. (2006). International Data Base (IDB): Summary Demographic Data for Kenya.
Buzzard, S. (1982). Women’s status and wage employment in Kisumu, Kenya. Washington, DC: The American University.
Charlton, K. E., & Rose, D. (2001). Nutrition among older adults in Africa: The situation at the beginning of the millenium. American Society for Nutritional Sciences, 131, 2424S–2428S.
Cliggett, L. (2005). Grains from Grass. Aging, gender and famine in Rural Africa. Ithaca: Cornell University Press.
Cohen, B., & Menken, J. (2006). Aging in Sub-Saharan Africa: Recommendations for furthering research. Washingon, DC: The National Academies Press.
Cook, K. D. (1990). Determinants of female time allocation in agricultural households in southwestern Kenya. PhD thesis, Cornell University, Cornell.
Cooper, R. S., Wolf-Maier, K., Luke, A., Adebowale, A., Banegas, J. R., Forrester, T., et al. (2005). An international comparative study of blood pressure in populations of European vs. African descent. BMC Medicine, 3, 2–10.
Dayton, J., & Ainsworth, M. (2004). The elderly and AIDS: Coping with the impact of adult death in Tanzania. Social Science & Medicine, 59, 2161–2172.
Ezeh, A., Chepngeno, G., Kasiira, A., & Woubalem, Z. (2006). The situation of older people in poor urban settings: The case of Nairobi, Kenya. In B. Cohen, & J. Menken (Eds.) Aging in sub-Saharan Africa: Recommendations for furthering research pp. 189–213. Washington, DC: National Academies Press.
Frolkis, W. (1993). Stress-age syndrome. Mechanisms of aging and development, 69, 93–107.
Geissler, P. W., Nokes, K., Price, R. J., Achieng’ Odhiambo, R., Aagaard-Hansen, J., & Ouma, J. H. (2000). Children and medicines: Self-treatment of common illnesses among Luo school children in western Kenya. Social Science & Medicine, 50, 1771–1783.
Gilborn, L. Z., Nyonyintono, R., Kabumbuli, R., & Jagwe-Wadda, G. (2001). Making a difference for children affected by AIDS: Baseline findings from operations research in Uganda. New York: Population Council.
Grundy, E., & Sloggett, A. (2003). Health inequalities in the older population: The role of personal capital, social resources and socio-economic circumstances. Social Science & Medicine, 56, 935–947.
HelpAge International (2002). HIV/AIDS and older people: The African situation. Nairobi: HelpAge International.
Kahn, K., Tollman, S., Thorogood, M., Connor, M., Garenne, M., Collinson, M., et al. (2006). Older adults and the health transition in Agincourt, rural South Africa: New understanding, growing complexity. In B. Cohen, & J. Menken (Eds.) Aging in sub-Saharan Africa. Recommendation for furthering research pp. 166–188. Washington, DC: National Academies Press.
Kakooza, J., & Kiumuna, S. R. (2005). HIV/AIDS orphans’ education in Uganda: The changing role of older people. Journal of Intergenerational Relationships, 34, 63–81.
Kerry, S. M., Michah, F. B., Plange-Rhule, J., Eastwood, J. B., & Cappuccio, F. P. (2005). Blood pressure and body mass index in lean rural and semi-urban subjects in West Africa. Journal of Hypertension, 23, 1645–1651.
Labarthe, D. R., Blaufox, M. D., Smith, W. M., Lacy, C. R., Schnaper, H., LaBaw, F., et al. (1991). Systolic Hypertension in the Elderly Program (SHEP). Part 5: Baseline blood pressure and pulse rate measurements. Hypertension, 17, II62–II76.
Lima-Costa, M. F., Barreto, S. M., Firmo, J. O. A., & Uchoa, E. (2003). Socioeconomic position and health in a population of Brazilian elderly: The Bambuí Health and Aging Study (BHAS). Revista Panamericana de Salud Públuca/Pan American Journal of Public Health, 13, 387–394.
Lima-Costa, M. F., Firmo, J. O. A., & Uchoa, E. (2004). The structure of self-rated health among older adults: The Bambuí Health and Ageing Study (BHAS). Revista de Saúde Pública, 38, 827–834.
Lima-Costa, M. F., Firmo, J. O. A., & Uchoa, E. (2005). Differences in self-rated health among older adults according to socioeconomic circumstances: The Bambuí Health and Aging Study. Cadernos de Saúde Pública, 21, 830–839.
Lima-Costa, M. F., Uchoa, E., Buerra, H. L., Firmo, J. O. A., Vidigal, P. G., & Barreto, S. M. (2000). The Bambuí Health and Ageing Study (BHAS): Methodological approach and preliminary results of a population based cohort study of the elderly in Brazil. Revista de Saúde Pública, Sao Paula/Journal of Public Health, 34, 126–134.
Lohman, T. G., Roche, A. F., & Martorell, R. (1989). Athropometric standardization reference manual. Champaign: Human Kinetics Books.
McEwen, B. (2001). From molecules to mind. Stress, individual differences, and the social environment. Annals New York Academy of Sciences, 935, 42–49.
McEwen, B. (2002). The end of stress as we know it. Washington, DC: Joseph Henry Press.
McEwen, B., & Wingfield, J. (2003). The concept of allostatis in biology and biomedicine. Hormones and Behavior, 43, 2–15.
Nalagoda, F., Wawer, M., Konde-Lule, J., Menon, R., Gray, R., Serwadda, D., et al. (1997). HIV infection in rural households, Rakai District, Uganda. Health Transition Review, 7, 3–17.
National Council for Population and Development (1999). Demographic and health survey 1998. Calverton, MD: Macro International Inc.
Nyambedha, E., Wandibba, S., & Aagaard-Hansen, J. (2001). Policy implications of the inadequate support systems for orphans in Western Kenya. Health Policy, 58, 83–96.
Nyambedha, E., Wandibba, S., & Aagaard-Hansen, J. (2003a). Changing patterns of orphan care due to the HIV epidemic in western Kenya. Social Science & Medicine, 57, 301–311.
Nyambedha, E., Wandibba, S., & Aagaard-Hansen, J. (2003b). “Retirement lost”—The new role of the elderly as caretakers for orphans in western Kenya. Journal of Cross-Cultural Gerontology, 18, 33–52.
Oburu, P. O., & Palmerus, K. (2005). Stress related factors among primary and part time caregiving grandmothers of Kenyan grandchildren. International Journal of Aging and Human Development, 60, 273–282.
Ochieng’, W. (1985). People round the Lake. London: Evans Brothers Limited.
Ocholla-Ayayo, A. B. C. (1999). Traditional ideology and ethics among the Southern Luo. Uppsala, Sweden: Scandinavian Institute of African Studies.
Ogunmefun, C., & Schatz, E. (2006). Caregivers’ sacrifices: The opportunity costs of adult morbidity and mortality on female pensioners in rural South Africa. Boulder: Institute of Behavioral Science.
Opiyo, F. A. (1996). Rural Kenyan Luo women’s lived experiences: An interpretation. Greensboro: University of North Carolina at Greensboro.
Reynar, A. (2000). Fertility decision making by couples amongst the Luo of Kenya. Philadelphia: University of Pennsylvania.
Sapolsky, R. M. (1996). Why stress is bad for your brain. Science, 273, 749–750.
Sapolsky, R. M. (1999). Glucocorticoids, stress, and their adverse neurological effects: Relevance to aging. Experimental Gerontology, 34, 721–732.
Sapolsky, R., Armanini, M., Packan, D., & Tombaugh, G. (1987). Stress and glucocorticoids in aging. Endocrinology and Metabolism Clinics of North America, 16, 965–980.
Smith, S. M., & Mensah, G. A. (2003). Population aging and implications for epidemic cardiovascular disease in sub-Saharan Africa. Ethnicity and Disease, 13, S2-77–80.
Ssengonzi, R. (2007). The plight of older persons as caregivers to people infected/affected by HIV/AIDS: Evidence from Uganda. Journal of Cross Cultural Gerontology, 22, 339–353.
UNAIDS (2006). 2006 Report on the global AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS.
UNAIDS/UNICEF (2002). Children on the brink 2002. A joint report on orphan estimates and program strategies. Washington, DC: TvT Associates/The Synergy Project.
UNAIDS/UNICEF/WHO (2002). Epidemiological fact sheets on HIV/AIDS and sexually transmitted infections: Kenya. Gevenva: UNAIDS.
UNICEF (2003). Africa’s orphaned generations. New York: UNICEF.
Unwin, N., McLarty, D., Machibya, H., Aspray, T., Tamin, B., Carlin, L., et al. (2006). Changes in blood pressure and lipids associated with rural to urban migration. Journal of Human Hypertension, 20, 704–706.
Wagner, A. K., Wyss, K., Gandek, B., Kilima, P. M., Lorenz, S., & Whiting, D. (1999). A Kiswahili version of the SF-36 Health Survey for use in Tanzania: Translation and tests of scaling assumptions. Quality of Life Research, 8, 101–110.
Ware, J. E. (2007). SF-36 Health Survey Update: Rand.
Ware, J. E., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30, 473–483.
WHO. (2005). WHO Global InfoBase Online. WHO global comparable estimates: WHO.
Williams, A., & Tumwekwase, G. (2001). Multiple impacts of the HIV/AIDS epidemic on the aged in rural Uganda. Journal of Cross-Cultural Gerontology, 16, 221–236.
Wilson, A. O., & Adamchak, D. J. (2000). AIDS in Africa: The grandmothers’ disease. Comment. Journal of Age Related Disorders, 12, 5–6.
Wolf, H. K., Kuulasmaa, K., Domarkiene, S., Cepaitis, Z., Molarius, A., Sans, S., et al. (1997). Blood pressure levels in 41 populations of the WHO MONICA project. Journal of Human Hypertension, 11, 733–742.
Wolf-Maier, K., Cooper, R. S., Banegas, J. R., Giampaoli, S., Hense, H.-W., Joffres, M., et al. (2003). Hypertension prevalence and blood pressure levels in 6 European Countries, Canada and the United States. JAMA, 289, 2363–2369.
Woodman, R., Ferrucci, L., & Guralnik, J. (2005). Anemia in older adults. Current Opinion in Hematology, 12, 123–128.
Wyss, K., Wagner, A., Whiting, D., Mtasiwa, D., Tanner, M., Gandek, B., et al. (1999). Validation of the Kiswahili version of the SF-36 Health Survey in a representative sample of an urban population in Tanzania. Quality of Life Research, 8, 111–120.
Acknowledgments
This project was funded by the Ohio University Baker Fund, Ohio University College of Osteopathic Medicine Research Award, the National Science Foundation under Grant No. 0515890 and in collaboration with the Kenya Medical Research Institute. Thanks to our Kenyan Field team: Monica Audi Liech, Beryl Awour Ogot, Antoney Odhiambo Juma, Agness Atieno Aluodo, Fredrick Awili, Jack Omondi Gao, Nancy Auma Ndiege, Brenda Loice Omondi, Jared Onyango, Kennedy Otieno Nyangwara, Danish Odie Agal and Yuanita Hongo. The following medical students were integral to the data collection on this project: Chelsea Crabtree, Jennifer Drost, Sarah Schillig, and Kristina Yoder. A special thanks to the communities in Nyando and Kisumu Rural Districts. We also thank the Director of the Kenya Medical Research Institute for his permission to publish this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ice, G.H., Zidron, A. & Juma, E. Health and Health Perceptions Among Kenyan Grandparents. J Cross Cult Gerontol 23, 111–129 (2008). https://doi.org/10.1007/s10823-008-9063-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10823-008-9063-9