Abstract
Purpose
The purpose of this study was to compare baseline characteristics and ovarian stimulation outcomes between patients presenting for medically indicated vs. elective fertility preservation consultation and to determine the impact of the 2013 ASRM guidelines on oocyte cryopreservation on the patient population presenting for fertility preservation consultation.
Methods
Retrospective cohort study conducted at an academic center. Study population included 332 patients presenting for medically indicated fertility preservation consultation and 210 patients presenting for elective consultation.
Results
Patients presenting for elective fertility preservation consultation were more likely to be of advanced age, non-Caucasian, highly educated, single, nulligravid, and meet criteria for diminished ovarian reserve (DOR). Additionally, patients presenting electively were more likely to have fertility insurance benefits. A higher percentage of patients with insurance benefits for oocyte cryopreservation proceeded to stimulation. There were no differences in stimulation parameters or number of retrieved oocytes between the groups when adjusted for age. Following release of the ASRM guidelines on oocyte cryopreservation, there was no difference in the percentage of patients in the medical group who proceeded with stimulation; however, a higher percentage of patients presenting electively underwent ovarian stimulation.
Conclusion
Although the populations presenting for medical compared with elective fertility preservation differ at baseline, ovarian stimulation parameters and outcomes are similar when adjusted for age. Insurance benefits for fertility preservation are not comprehensive and impact the decision to proceed with stimulation in all patients. The publication of the ASRM guidelines on oocyte cryopreservation increased utilization of this technology among patients presenting electively; however, they remained at an advanced age and with decreased ovarian reserve parameters.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fertility preservation including embryo and oocyte cryopreservation is traditionally offered to patients requiring gonadotoxic therapy as a means of preserving reproductive potential following treatment. Increasingly, there is interest in fertility preservation for patients electing to defer childbearing for non-medical indications such as career advancement or the identification of a suitable partner [1]. Indeed, survey data suggests that the elective postponement of fertility is the most common indication for oocyte cryopreservation [2]. Social or elective oocyte cryopreservation has also gained considerable attention among the public and media as large corporations such as Google, Apple, and Facebook advertise elective egg freezing as a professional benefit. This has led to both professional and ethical debates regarding the acceptability of oocyte cryopreservation as an “insurance” policy and whether or not this provides an empowering benefit to women or a detrimental false sense of security [3,4,5,6].
In January 2013, ASRM published a practice committee guideline on mature oocyte cryopreservation in which the experimental label was removed. Of note, the guideline specifically cautioned that “there are not yet sufficient data to recommend oocyte cryopreservation for the sole purpose of circumventing reproductive aging in healthy women because there are no data to support the safety, efficacy, ethics, emotional risks, and cost-effectiveness of oocyte cryopreservation for this indication” [7]. In Europe, ESHRE endorses oocyte cryopreservation as an option for women both at risk of “premature or iatrogenic fertility loss” as well as for those who want to “protect their reproductive potential against the threat of time”; however, they specifically recommend that those pursuing social egg freezing do so before the age of 35 [8].
Previous research on fertility preservation in patients with malignancy typically compares this population to couples with infertility, with conflicting results regarding ovarian stimulation parameters and outcomes [9,10,11,12,13,14,15,16]. As for the elective fertility preservation population, most studies thus far have described the demographics of patients presenting for elective oocyte cryopreservation consultation [17,18,19]. Recently, two larger studies reported their experience with frozen oocyte thaw success and pregnancy outcomes [20, 21]. There has only been one study to date that directly compared patients with cancer to those presenting for elective fertility preservation [22].
Given the increased attention to and utilization of oocyte cryopreservation [21] as well as the distinction in practice guideline recommendations for these two groups of patients, we set out to answer two important questions: First, we assessed whether the characteristics, medical decision-making, and ovarian stimulation outcomes differed by fertility preservation indication. Second, we investigated the impact of the 2013 ASRM guidelines on the patient population presenting for fertility preservation consultation.
Materials and methods
This retrospective cohort study included all female patients who presented for fertility preservation consultation at Penn Fertility Care between January 1, 2008, and May 2, 2016. To identify all eligible subjects, physicians in the practice were first queried to obtain the diagnostic codes utilized for fertility preservation consultation. Subsequently, the Penn Medicine Data Analytics Center was utilized to identify all patients who presented with the following diagnostic V/Z codes: “Encounter for fertility preservation counseling” (V26.42, Z31.62), “Encounter for fertility preservation procedure” (V26.82, Z31.83), “Procreative management investigation and testing” (V26.2, Z31), “Procreative management and genetic counseling and testing” (V26.3, Z31.43, Z31.43), “Fertility testing” (V26.21, Z31.41), “General counseling and advice on procreative management” (V26.4, Z31.69), “Other specified procreative management” (V26.8, Z31.8, V26.89, Z31.89), “Encounter for assisted reproductive fertility procedure cycle” (V26.81, Z31.83), “Other investigation and testing” (V26.29, Z31.49), and “Unspecified procreative management” (V26.9, Z31.9). The charts of all identified patients were then reviewed to confirm presentation for fertility preservation consultation. Additionally, a list of new patient consults seen by the primary oncofertility provider in our practice were screened to ensure capture of all eligible subjects. Those patients presenting for consultation secondary to a history of malignancy, or with a medical condition necessitating gonadotoxic therapy, were defined as the medical fertility preservation group. This group was further subdivided into pre- and post-chemotherapy for subgroup analyses. Patients presenting for consultation to discuss fertility preservation without any pre-existing medical condition requiring gonadotoxic therapy were defined as the elective fertility preservation group. The study protocol was approved by the Institutional Review Board at the University of Pennsylvania (IRB #819938). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Medical records were abstracted to obtain detailed demographic and treatment-specific data. Demographic and baseline characteristics included the following: age at first consultation, race, highest level of education, partner status, gravidity, body mass index (BMI), and ovarian reserve testing (anti-Mullerian hormone level (picoAMH ELISA, Ansh Laboratories), day 3–5 follicle-stimulating hormone and estradiol, antral follicle count). Additionally, data on insurance benefits including general fertility (intrauterine insemination, +/− in vitro fertilization coverage) and oocyte cryopreservation benefits were collected. The majority of new patients seen at our practice meet with a financial counselor at the time of their initial appointment to determine current insurance benefits. For those patients who did not proceed with stimulation following their consultation, insurance benefits were inferred from financial counseling notes at this initial visit; however, definitive coverage could not be determined unless a patient underwent stimulation. In patients who ultimately proceeded with treatment, insurance coverage was verified by billing records.
For those patients who proceeded with ovarian stimulation for either oocyte or embryo banking, ovarian stimulation was performed using either luteal-phase GnRH agonist, GnRH antagonist, or microdose Lupron Flare protocols as previously described [9, 23]. The starting dose of gonadotropins was selected based on patient age, anti-Mullerian hormone (AMH), FSH, and baseline antral follicle count (AFC). Most patients with breast or endometrial cancer also received the aromatase inhibitor letrozole 5 mg (Mylan Pharmaceuticals or Teva Pharmaceuticals) throughout their stimulation cycle. Patients elected to cryopreserve either embryos or oocytes. For oocyte cryopreservation, oocytes were stripped on the day of retrieval to assess maturity prior to cryopreservation via vitrification.
Stimulation parameters including stimulation protocol, starting gonadotropin dose, highest gonadotropin dose, total duration of stimulation, number of follicles at trigger, estradiol on day of trigger (pg/mL), type of trigger (HCG vs. Lupron only vs. HCG + Lupron [24]), oocyte yield (mature and immature), development of moderate or severe OHSS (as defined by ASRM [25]), and cycle cancelation data were collected.
Statistical analysis
Association of demographic and baseline characteristics by group (medical vs. elective, pre- vs. post-ASRM guidelines, proceeding vs. not proceeding with stimulation) were compared using Pearson chi-squared, Fisher’s exact, and Wilcoxon rank-sum tests for categorical and continuous data as appropriate. Baseline ovarian reserve and ovarian stimulation parameters were compared using linear and Poisson regression models adjusting for age and starting AFC where appropriate. All hormone concentrations were transformed using natural log to reduce the influence of a left-skewed distribution of values. A two-tailed p value of <0.05 was considered statistically significant. Data analysis was performed using STATA statistical software version 12.0 (StataCorp, College Station, TX, USA).
Results
Patient characteristics
A total of 542 patients were included in this analysis; 332 presented with a medical indication for fertility preservation, while 210 presented for elective fertility preservation consultation. Baseline demographic and clinical characteristics are presented in Table 1. Compared to patients presenting with a medical indication for fertility preservation, those presenting electively were older (median age 36.8 vs. 29.3 years, p < 0.0001), more diverse (66.2 vs. 78.3% Caucasian, p = 0.002), highly educated (75.2 vs. 30.9% with master’s or graduate/professional degree, p < 0.0001), less likely to have a partner (25.7 vs. 63.0%, p < 0.0001), and more likely to be nulligravid (79.5 vs. 67.8%, p = 0.003).
Comparison of ovarian reserve markers revealed that patients presenting electively had a higher FSH (median 7.3 vs. 6.0 mIU/mL, p = 0.001), had lower baseline antral follicle count (AFC) (median 13 vs. 17, p = 0.001), and were more likely to meet criteria for diminished ovarian reserve (DOR) based on either FSH >10mIU/mL, AMH <1.0 ng/mL, or AFC <6 (38.6 vs. 23.8%, p < 0.0001). Of note, after adjusting for age, there was no difference in FSH or DOR between the two groups (p = 0.27 and p = 0.19, respectively); however, AFC remained significantly lower in the elective group (p < 0.0001).
There was no difference in overall insurance coverage status between the elective and medical groups (median 97.6 vs. 99.3%); however, a higher percentage of patients who presented for elective fertility preservation consultation had insurance benefits for fertility treatments (68.5 vs. 34.9%, p < 0.0001) and oocyte vitrification (35.6 vs. 25.9%, p = 0.03).
There were no differences in the percentage of elective or medical fertility preservation patients that proceeded to stimulation (46.9 vs. 44.7%, p = 0.62); however, those presenting electively were more likely to undergo multiple cycles (p = 0.03).
Demographic and baseline characteristics were also compared between elective and medical fertility preservation patients that presented pre-chemotherapy (n = 230) to account for expected disparities in ovarian reserve parameters and response to stimulation among those who had been exposed to gonadotoxic therapies (Supplemental Table 1). Similar to the above, the elective group had a higher maximum FSH (median 7.3 vs. 5.9mIU/mL, p = 0.0001), a lower AFC (median 13 vs. 18, p < 0.0001), and a higher percentage of patients in the elective group who met criteria for DOR based on either AMH, FSH, or AFC (38.6 vs. 21.7%, p < 0.0001). However, after adjusting for age, maximum FSH and DOR status were no longer statistically different between groups.
In order to assess for factors that may impact the decision to proceed with fertility preservation, demographic and baseline characteristics were also compared among the elective patients who did and did not proceed to ovarian stimulation (data not shown). There were overall no differences between those who did or did not proceed with stimulation; however, a higher percentage of patients who elected to proceed met criteria for diminished ovarian reserve (DOR) by either an AMH <1 ng/mL, FSH >10 mIU/mL, or AFC <6 (49.0 vs. 29.7%, p = 0.004), and this finding remained significant after adjusting for age (OR 2.30 95%CI [1.27–4.17], p = 0.006).
Ovarian stimulation cycle characteristics
One hundred seventeen pre-chemotherapy medical patients underwent a total of 130 cycles of ovarian stimulation, and 98 elective patients underwent a total of 129 cycles. Table 2 compares cycle characteristics between the elective and medical pre-chemotherapy groups. As expected based on the time-sensitive nature of stimulation in the medical group, patients presenting electively had a significantly longer time period between initial consultation and the start of their stimulation when compared with the pre-chemotherapy medical group (median 110 vs. 13 days, p < 0.0001). Stimulation protocols also significantly differed between the groups, with 11.1% of the elective patients receiving a GnRH agonist protocols, 77.8% a GnRH antagonist protocol, and 11.1% a microdose Lupron Flare protocol as compared with the medical patients in which only 3.9% received a GnRH agonist protocol, 92.9% an antagonist protocol, and 3.2% a microdose Lupron Flare protocol (p = 0.003).
Overall, there were no differences in the highest or total doses of gonadotropins, total days of stimulation, number of follicles measuring >15 mm at trigger, or type of trigger medication. Patients in the elective group received a higher starting dose of gonadotropins (median 375 vs. 300 IU, p = 0.0008); however, this difference was no longer significant after adjusting for age (p = 0.289). As expected, overall estradiol levels were higher on day of trigger in the elective vs. medical group (median 2308 vs. 1013 pg/mL, p < 0.0001); however, there were no significant differences in estradiol level when only non-letrozole cycles were included (median 2308 vs. 2116 pg/mL, p = 0.09). The total number of follicles >10 mm at trigger was lower in the elective group compared with the medical group (median 16 vs. 20, p = 0.03); however, this was no longer significant when adjusted for age (p = 0.65). There were no differences in the total number of oocytes retrieved or the percent of mature oocytes between the groups. However, the cancelation rate was significantly higher in the elective group compared with the medical group (10.9 vs. 3.9%, p = 0.03). There was no difference in the rate of moderate or severe OHSS in the medical vs. elective group (3.4 vs. 4.8%, p = 0.75); importantly, no patients required hospitalization.
Ninety-three of the elective patients cryopreserved oocytes, while one patient cryopreserved only embryos and one patient cryopreserved both embryos and oocytes. Among the cohort of pre-chemotherapy medical patients, 39 cryopreserved oocytes, 51 cryopreserved embryos only, and 11 cryopreserved both embryos and oocytes. With respect to patients who cryopreserved oocytes, four patients from the elective group and two patients from the medical group have warmed their oocytes thus far. All of these patients were at least 38 years of age at the time of cryopreservation, and none has achieved pregnancy. Of the elective patients, two elected to pursue pre-implantation genetic screening (PGS) prior to transfer and neither had normal embryos to transfer. One patient failed a single frozen embryo transfer and is planning a transfer with a remaining cryopreserved blastocyst from the cryopreserved oocytes, and the last patient did not conceive. Of the medical patients who cryopreserved oocytes, one patient did not undergo embryo transfer as her oocytes did not survive warming (four oocytes were cryopreserved prior to routine cryopreservation at our facility). The remaining patient warmed seven oocytes planning for PGS for use in a gestational carrier; however, her embryos did not develop to the blastocyst stage.
Eighteen pre-chemotherapy patients from the medical cohort have returned to utilize their embryos. Of these patients, 8/18 (44%) reported a live birth or current ongoing pregnancy. Notably, six of these patients utilized a gestational carrier. Of the ten patients who did not conceive with their cryopreserved embryos, one conceived spontaneously, one underwent a fresh IVF cycle resulting in a twin live birth with use of a gestational carrier, two patients utilized donor oocytes with subsequent live births, one is currently undergoing a repeat frozen embryo transfer with remaining embryos, and one patient is undergoing fertility treatments. Additionally, two patients have subsequently been diagnosed with recurrent metastatic malignancy and two decided against additional treatment.
Fertility insurance coverage
Data on insurance fertility benefits was available on 202/210 (96%) of the elective patients and 269/332 (81%) of the medical patients. The percentage of patients with fertility benefits in both groups of patients is shown in Table 3. Of note, among patients presenting for elective fertility preservation consultation, there was no difference in the percentage of patients with general fertility benefits who proceeded to or declined stimulation (64.5 vs. 72.6%, p = 0.23); however, a higher percentage of patients who proceeded to stimulation did specifically have oocyte vitrification benefits (45.9 vs. 26.6%, p = 0.006). In the medical fertility preservation group, a higher percentage of patients who proceeded to stimulation had both fertility and oocyte vitrification coverage as compared to patients who did not undergo stimulation (42.1 vs. 27.1%, p = 0.01 and 31.4% vs. 19.8%, p = 0.04).
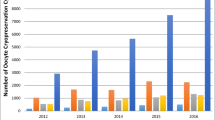
Removal of the “experimental” label from oocyte cryopreservation
We also investigated how medical decision-making may have changed as a result of the January 2013 publication of the ASRM practice guidelines removing the “experimental” label from oocyte cryopreservation. Of note, the number of consults for fertility preservation nearly doubled in our practice between 2012 and 2014 (108 consults in 2014 up from 82 in 2013 and 55 in 2012). This number continued to rise to 121 in 2015. Similarly, the number of patients proceeding to stimulation tripled in our practice in 2013 (74 individuals undergoing stimulation in 2013 up from 22 in 2012). The number of individuals undergoing stimulation then remained fairly constant with 60 individuals proceeding with stimulation in 2014 and 58 in 2015. To assess for immediate differences in the decision to proceed to stimulation after publication of the ASRM guidelines, we compared the percentage of patients who proceeded with stimulation before 2013 to those who proceeded in 2013/2014. In the medical group, there was no difference in the percentage of patients who proceeded before or after 2013 (75/165 (45.5%) pre-guidelines and 42/89 (47.2%) post-guidelines, p = 0.79). In the elective group, however, a significantly higher percentage of patients proceeded with stimulation immediately after the guidelines were published (31.8% (7/22) pre-guidelines vs. 63.4% (64/101) post-guidelines, p = 0.009). Given that a significantly higher proportion of patients in the elective group proceeded to stimulation following removal of the experimental label from oocyte cryopreservation, we also compared the demographic and baseline characteristics of these patients before and after 2013 to determine whether there were any differences in the patient populations presenting for consultation (data not shown). Overall, there were no differences in the patient’s presenting before or after release of the practice committee guidelines. While those presenting before the guidelines had a statistically lower AMH, after adjusting for age, this was no longer significant (p = 0.17).
Discussion
Increasing awareness and utilization of fertility preservation has resulted in debate among physicians, professional societies, and the public about the appropriateness of this technology for patients electively deferring childbearing as compared to those facing gonadotoxic treatment. In our study, there were clear differences between the patients who presented for elective vs. medically indicated fertility preservation consultation, with elective patients being older, single, highly educated, and more likely to have diminished ovarian reserve at presentation. This is in agreement with previous studies examining the demographics of the elective fertility preservation population [18, 19, 21, 26] and is also similar to the only other study that directly compared an elective fertility population to patients with malignancy [22]. In our study, there were no differences in baseline serum markers of ovarian reserve between medical vs. elective patients when age was taken into account. Interestingly, antral follicle count was statistically lower in the patients presenting electively, suggesting there may be other factors, not accounted for by our chart abstraction (i.e., counseling from providers outside our healthcare system, family history of difficulty conceiving, geographic or peer influences) that drive patients to seek consultation. Additional prospective studies would shed light on the factors influencing patient presentation.
Previous studies examining ovarian stimulation in patients with malignancy generally compare this population to patients with various infertility diagnoses. Furthermore, the data are conflicting with some studies demonstrating no difference in stimulation parameters or outcomes [9,10,11, 13, 15, 16], while others report that patients with malignancy have fewer oocytes retrieved [12, 14]. In our study, comparison of pre-chemotherapy medical patients to patients undergoing elective fertility preservation demonstrated no differences in total gonadotropin doses, total number of oocytes retrieved, or mature oocyte yield when age was accounted for, even though the choice of ovarian stimulation protocol differed between the groups. The cancelation rate was higher in the elective group, which is likely secondary to increased age and diminished ovarian reserve in this population. Additionally, cancer patients may have been more motivated to complete fertility preservation cycles given that patients were facing imminent gonadotoxic therapy.
We were also able to assess insurance benefits for the majority of patients who presented for consultation to infer the degree to which this factor might influence medical decision-making. Of note, among all patients who presented for fertility preservation consultation, benefits for oocyte cryopreservation were significantly higher in patients who elected to proceed to stimulation. Among the medical patients who underwent stimulation, a significantly higher percentage also had fertility benefits. Previous research in patients with malignancy has underscored the importance of financial concerns on the decision to undergo fertility preservation, with decision-making significantly impacted by the cost of treatment [27,28,29]. In a recent survey of Singaporean medical students queried about elective oocyte cryopreservation, 45.7% would undergo cryopreservation for career advancement; however, this number increased to 71.3% if a government subsidy was available [30]. Our data further supports the significance of cost on decision-making in all patients considering fertility preservation, and provides evidence that insurance coverage plays an important role in the decision to undergo fertility preservation.
In order to assess the impact of the ASRM guidelines on both patients presenting for consultation and their decision to proceed with stimulation, we also analyzed patients according to presentation before 2013 and in the immediate 2 years following the guidelines. The number of patients presenting for fertility preservation tripled in our practice in 2013 illustrating a concomitant increase in public interest following release of the guidelines. Furthermore, our temporal analysis revealed no differences in the demographics or characteristics of patients presenting for consultation; however, a significantly higher percentage of patients in the elective group proceeded to stimulation during this time. Thus, while patients presenting electively continued to be older and have decreased ovarian reserve, they were more likely to proceed with stimulation. There was no difference, however, in the percentage of patients in the medical group who decided to proceed with stimulation. This is especially interesting as the ASRM guidelines specifically cautioned against the use of this technology solely for circumvention of reproductive aging. Furthermore, other than insurance coverage, the only characteristic that differed among elective patients who proceeded to stimulation was the presence of DOR.
This finding highlights the current ethical debate regarding elective oocyte cryopreservation which argues that increased reproductive autonomy empowers women while opponents are concerned that elective oocyte cryopreservation promotes a false sense of security regarding pregnancy at an advanced age and benefits from misconceptions regarding the overall success of the technology [3,4,5, 26, 31, 32]. Indeed, misconception among the public is a major concern as studies have consistently demonstrated a significant knowledge gap regarding the natural decline in fertility and success of fertility treatments [6, 33,34,35]. Furthermore, survey data of patients who have undergone fertility preservation consistently demonstrates that the large majority of these patients wish they had undergone stimulation at an earlier age [18, 36]. In our study, only four patients in the elective group have returned to warm their oocytes; however, none have achieved pregnancy and all were greater than 38 at the time of stimulation. More recently, two larger studies reporting pregnancy rates following oocyte cryopreservation demonstrated reassuring pregnancy rates following oocyte vitrification. However, clear differences in success rates are apparent as patients age, especially after the age of 35, when significant decreases in pregnancy rates were noted, even when the same number of oocytes were thawed [20, 21]. This underscores the importance of proper patient education both by physicians as well as through public forums, especially as public awareness of this technology increases.
This is one of the first studies to directly compare patients presenting for elective vs. medically indicated fertility preservation consultation. This study is also unique in its examination of patient demographics before and after release of the 2013 ASRM guidelines and assessment of fertility insurance benefits. Limitations include the potential for selection and ascertainment bias inherent to its retrospective design. Furthermore, the data presented are from a single academic institution which limits sample size and generalizability as demographics and practice patterns may vary geographically. Indeed, a larger and national dataset would be useful in further exploring patient populations and fertility preservation outcomes. It should also be noted that concomitant with release of the ASRM guidelines was a surge in media attention as corporations such as Facebook and Apple advertised fertility preservation as a professional benefit [37]. Therefore, it is important to note that increased utilization of fertility preservation among the elective population may also have been significantly influenced by increased social media attention. Finally, the medical group consisted of a heterogeneous population including patients with a mixture of diagnoses such as malignancy, hematologic disorders, and autoimmune diseases which lends generalizability, but limits assessment of nuances between diagnostic groups.
In conclusion, while the patient populations presenting for medical or elective fertility preservation consultation may be different at baseline, there does not appear to be a difference in their response to stimulation after controlling for age. Insurance benefits for fertility preservation seem to play an important role in the decision to proceed with stimulation among all patients presenting for fertility preservation consultation. Finally, since the removal of the experimental label from oocyte cryopreservation, an increased number of patients are proceeding with elective fertility preservation; however, this population remains at an advanced age and with diminished markers of ovarian reserve. This finding underscores the importance of improved and up-to-date patient education regarding reproductive health, age-related decline in fertility, and the potential benefits of fertility preservation through oocyte cryopreservation. Most importantly, it will be critical to continue to follow these women to understand their utilization of previously cryopreserved oocytes and embryos, as well as their pregnancy, offspring, and overall health in the future.
References
Cil AP, Turkgeldi L, Seli E. Oocyte cryopreservation as a preventive measure for age-related fertility loss. Semin Reprod Med. 2015;33(6):429–35. doi:10.1055/s-0035-1567819.
Rudick B, Opper N, Paulson R, Bendikson K, Chung K. The status of oocyte cryopreservation in the United States. Fertil Steril. 2010;94(7):2642–6. doi:10.1016/j.fertnstert.2010.04.079.
Zoll M, Mertes H, Gupta J. Corporate giants provide fertility benefits: have they got it wrong? Eur J Obstet Gynecol Reprod Biol. 2015;195:A1–2. doi:10.1016/j.ejogrb.2015.10.018.
Mertes H, Pennings G. Social egg freezing: for better, not for worse. Reprod BioMed Online. 2011;23(7):824–9. doi:10.1016/j.rbmo.2011.09.010.
Goldman KN, Grifo JA. Elective oocyte cryopreservation for deferred childbearing. Curr Opin Endocrinol Diabetes Obes. 2016;23(6):458–64. doi:10.1097/MED.0000000000000291.
Daniluk JC, Koert E. Childless women’s beliefs and knowledge about oocyte freezing for social and medical reasons. Hum Reprod. 2016;31(10):2313–20. doi:10.1093/humrep/dew189.
Practice Committees of American Society for Reproductive M, Society for Assisted Reproductive T. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99(1):37–43. doi:10.1016/j.fertnstert.2012.09.028.
Ethics ETFo, Law, Dondorp W, de Wert G, Pennings G, Shenfield F, et al. Oocyte cryopreservation for age-related fertility loss. Hum Reprod. 2012;27(5):1231–7. doi:10.1093/humrep/des029.
Johnson LN, Dillon KE, Sammel MD, Efymow BL, Mainigi MA, Dokras A, et al. Response to ovarian stimulation in patients facing gonadotoxic therapy. Reprod BioMed Online. 2013;26(4):337–44. doi:10.1016/j.rbmo.2013.01.003.
Almog B, Azem F, Gordon D, Pauzner D, Amit A, Barkan G, et al. Effects of cancer on ovarian response in controlled ovarian stimulation for fertility preservation. Fertil Steril. 2012;98(4):957–60. doi:10.1016/j.fertnstert.2012.06.007.
Cardozo ER, Thomson AP, Karmon AE, Dickinson KA, Wright DL, Sabatini ME. Ovarian stimulation and in-vitro fertilization outcomes of cancer patients undergoing fertility preservation compared to age matched controls: a 17-year experience. J Assist Reprod Genet. 2015;32(4):587–96. doi:10.1007/s10815-015-0428-z.
Domingo J, Guillen V, Ayllon Y, Martinez M, Munoz E, Pellicer A, et al. Ovarian response to controlled ovarian hyperstimulation in cancer patients is diminished even before oncological treatment. Fertil Steril. 2012;97(4):930–4. doi:10.1016/j.fertnstert.2012.01.093.
Druckenmiller S, Goldman KN, Labella PA, Fino ME, Bazzocchi A, Noyes N. Successful oocyte cryopreservation in reproductive-aged cancer survivors. Obstet Gynecol. 2016;127(3):474–80. doi:10.1097/AOG.0000000000001248.
Friedler S, Koc O, Gidoni Y, Raziel A, Ron-El R. Ovarian response to stimulation for fertility preservation in women with malignant disease: a systematic review and meta-analysis. Fertil Steril. 2012;97(1):125–33. doi:10.1016/j.fertnstert.2011.10.014.
Knopman JM, Noyes N, Talebian S, Krey LC, Grifo JA, Licciardi F. Women with cancer undergoing ART for fertility preservation: a cohort study of their response to exogenous gonadotropins. Fertil Steril. 2009;91(4 Suppl):1476–8. doi:10.1016/j.fertnstert.2008.07.1727.
Quintero RB, Helmer A, Huang JQ, Westphal LM. Ovarian stimulation for fertility preservation in patients with cancer. Fertil Steril. 2010;93(3):865–8. doi:10.1016/j.fertnstert.2008.10.007.
Baldwin K, Culley L, Hudson N, Mitchell H, Lavery S. Oocyte cryopreservation for social reasons: demographic profile and disposal intentions of UK users. Reprod BioMed Online. 2015;31(2):239–45. doi:10.1016/j.rbmo.2015.04.010.
Hodes-Wertz B, Druckenmiller S, Smith M, Noyes N. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100(5):1343–9. doi:10.1016/j.fertnstert.2013.07.201.
Tsafrir A, Haimov-Kochman R, Margalioth EJ, Eldar-Geva T, Gal M, Bdolah Y, et al. Ovarian stimulation for oocyte cryopreservation for prevention of age-related fertility loss: one in five is a low responder. Gynecol Endocrinol. 2015;31(10):779–82. doi:10.3109/09513590.2015.1062859.
Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril. 2016;105(2):459–466 e2. doi:10.1016/j.fertnstert.2015.10.026.
Cobo A, Garcia-Velasco JA, Coello A, Domingo J, Pellicer A, Remohi J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril. 2016;105(3):755–764 e8. doi:10.1016/j.fertnstert.2015.11.027.
Garcia-Velasco JA, Domingo J, Cobo A, Martinez M, Carmona L, Pellicer A. Five years’ experience using oocyte vitrification to preserve fertility for medical and nonmedical indications. Fertil Steril. 2013;99(7):1994–9. doi:10.1016/j.fertnstert.2013.02.004.
Chan JL, Johnson LN, Efymow BL, Sammel MD, Gracia CR. Outcomes of ovarian stimulation after treatment with chemotherapy. J Assist Reprod Genet. 2015;32(10):1537–45. doi:10.1007/s10815-015-0575-2.
O'Neill KE, Senapati S, Maina I, Gracia C, Dokras A. GnRH agonist with low-dose hCG (dual trigger) is associated with higher risk of severe ovarian hyperstimulation syndrome compared to GnRH agonist alone. J Assist Reprod Genet. 2016;33(9):1175–84. doi:10.1007/s10815-016-0755-8.
Practice Committee of the American Society for Reproductive Medicine. Electronic address Aao, Practice Committee of the American Society for Reproductive M. Prevention and treatment of moderate and severe ovarian hyperstimulation syndrome: a guideline. Fertil Steril. 2016;106(7):1634–47. doi:10.1016/j.fertnstert.2016.08.048.
Baldwin K, Culley L, Hudson N, Mitchell H. Reproductive technology and the life course: current debates and research in social egg freezing. Hum Fertil (Camb). 2014;17(3):170–9. doi:10.3109/14647273.2014.939723.
Kim J, Deal AM, Balthazar U, Kondapalli LA, Gracia C, Mersereau JE. Fertility preservation consultation for women with cancer: are we helping patients make high-quality decisions? Reprod BioMed Online. 2013;27(1):96–103. doi:10.1016/j.rbmo.2013.03.004.
Hill KA, Nadler T, Mandel R, Burlein-Hall S, Librach C, Glass K, et al. Experience of young women diagnosed with breast cancer who undergo fertility preservation consultation. Clin Breast Cancer. 2012;12(2):127–32. doi:10.1016/j.clbc.2012.01.002.
Yee S, Abrol K, McDonald M, Tonelli M, Liu KE. Addressing oncofertility needs: views of female cancer patients in fertility preservation. J Psychosoc Oncol. 2012;30(3):331–46. doi:10.1080/07347332.2012.664257.
Tan SQ, Tan AW, Lau MS, Tan HH, Nadarajah S. Social oocyte freezing: a survey among Singaporean female medical students. J Obstet Gynaecol Res. 2014;40(5):1345–52. doi:10.1111/jog.12347.
Mertes H. Does company-sponsored egg freezing promote or confine women’s reproductive autonomy? J Assist Reprod Genet. 2015;32(8):1205–9. doi:10.1007/s10815-015-0500-8.
Linkeviciute A, Peccatori FA, Sanchini V, Boniolo G. Oocyte cryopreservation beyond cancer: tools for ethical reflection. J Assist Reprod Genet. 2015;32(8):1211–20. doi:10.1007/s10815-015-0524-0.
Bavan B, Porzig E, Baker VL. An assessment of female university students’ attitudes toward screening technologies for ovarian reserve. Fertil Steril. 2011;96(5):1195–9. doi:10.1016/j.fertnstert.2011.08.018.
Birch Petersen K, Hvidman HW, Sylvest R, Pinborg A, Larsen EC, Macklon KT, et al. Family intentions and personal considerations on postponing childbearing in childless cohabiting and single women aged 35-43 seeking fertility assessment and counselling. Hum Reprod. 2015;30(11):2563–74. doi:10.1093/humrep/dev237.
Yu L, Peterson B, Inhorn MC, Boehm JK, Patrizio P. Knowledge, attitudes, and intentions toward fertility awareness and oocyte cryopreservation among obstetrics and gynecology resident physicians. Hum Reprod. 2016;31(2):403–11. doi:10.1093/humrep/dev308.
Stoop D, Maes E, Polyzos NP, Verheyen G, Tournaye H, Nekkebroeck J. Does oocyte banking for anticipated gamete exhaustion influence future relational and reproductive choices? A follow-up of bankers and non-bankers. Hum Reprod. 2015;30(2):338–44. doi:10.1093/humrep/deu317.
Friedman D. Perk up: Facebook and apple now pay for women to freeze eggs. http://www.nbcnews.com/news/us-news/perk-facebook-apple-now-pay-women-freeze-eggs-n225011. 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the Institutional Review Board at the University of Pennsylvania (IRB #819938). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Funding sources
NIH T32 HD040135 (SBS), 5K12HD065257-07 (SBS), and 5K12HD001265-14 (SS)
Electronic supplementary material
Supplemental Table 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Schon, S.B., Shapiro, M., Gracia, C. et al. Medical and elective fertility preservation: impact of removal of the experimental label from oocyte cryopreservation. J Assist Reprod Genet 34, 1207–1215 (2017). https://doi.org/10.1007/s10815-017-0968-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-0968-5