Abstract
Purpose
Our objective was to determine if a change in serum P4 from day of transfer (defined as day 19) to day 28 could predict live birth outcome in patients undergoing IVF.
Methods
This study was a retrospective analysis of fresh IVF cycles from 2010 to 2013 at a single center. Primary outcomes include raw and percent change in serum P4, live birth rate, missed abortion, and biochemical pregnancies.
Results
Our results showed an association between live birth rate and percent change in P4. Patients with a 10% or greater drop in serum P4 from day 19 to day 28 had a lower live birth rate, at 26 versus 63%. Interestingly, both groups had “normal” serum P4 levels on day 19, but patients with a 10% or greater drop had lower P4 levels than their counterparts. There was no association between percent P4 change and spontaneous abortion or biochemical pregnancy.
Conclusions
This is the first study to show that percent drop in serum P4 from day of transfer to day 28 is associated with decreased rates of live birth and ongoing pregnancy in fresh IVF cycles, even despite “high or normal” P4 levels on day of transfer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rapid rise of progesterone and its sustained levels are important endocrine signals responsible for initiating the period of endometrial receptivity to implantation as well as maintaining pregnancy once implantation has occurred [1]. While the blood/serum levels of progesterone are well characterized during natural cycles with and without pregnancy, optimal levels of progesterone are not well defined for cycles of controlled ovarian hyperstimulation (COH). This is particularly true for cycles of COH in combination with oocyte retrieval and in vitro fertilization with embryo transfer. Since many programs artificially manipulate progesterone levels by administration of exogenous progesterone during these cycles of assisted reproductive technologies, it is important to know what levels of progesterone are optimal for endometrial receptivity and for supporting fetuses that have already implanted.
There has been some investigation of optimal serum progesterone levels in in vitro fertilization, yet the ideal serum level is still elusive. Many studies have evaluated serum P4 at time of trigger, with both elevated levels and low levels showing a negative impact on implantation or live birth rate [2–7]. Studies investigating serum P4 levels at time of embryo transfer (ET) also show a similar sensitive balance. For example, one study in fresh donor cycles showed that serum P4 was positively correlated with clinical pregnancy and live birth [8]. However, another study examining frozen transfer with donor oocytes showed that elevated serum P4 on day of ET was associated with lower live birth and high pregnancy loss rates [9]. While many have investigated luteal P4 levels, there has yet to be exploration of a change or trend in P4 levels.
The goal of this study was to further investigate the function of P4 levels in serum after transfer in fresh IVF cycles and their impact on pregnancy outcome. More specifically, we sought to answer the question: Is a change in serum P4 from day of embryo transfer (defined as and hereafter will be referred to as day 19) to day 28 associated with birth outcome in fresh IVF cycles?
Materials and methods
This study is a retrospective chart review, under an IRB approved by our center, of all patients who underwent fresh IVF cycles between 2010 and 2013. Exclusion criteria included patients using vaginal progesterone preparations and patients whose dose of P4 was increased, to a target serum range of 10 ng/mL. Generally, these cycles were monitored gonadotropin and antagonist cycles. Pituitary downregulation was achieved with the use of GnRH antagonist as appropriate. Patients were triggered with 500 mcg of recombinant subcutaneous HCG (ovidrel) or Lupron 40 units with 1000 units of subcutaneous HCG when the largest follicles were approximately 18–19 mm in size as per our protocol. Ultrasound-guided aspiration of ovarian follicles was performed to retrieve oocytes approximately 35 h after trigger. Fertilization was achieved via standard insemination (∼80% of the cases) or ICSI (∼20% of the cases). Embryos were then cultured, and 1, 2, or 3 were transferred as day 5/6 blastocysts per our center’s protocol.
Luteal support was provided by intramuscular injection of progesterone in oil. Progesterone administration was started on the day after retrieval and continued, if indicated, until weeks 9–10 of pregnancy and then tapered. Blood for analysis of P4 levels was drawn between 7:00 am and 8:00 am, roughly 12 h following the most recent injection. Steady-state levels are attained after 48 h with daily injections, and the peak following each injection occurs roughly 8 h after the injection [10]. Blood samples on day 19 were drawn on the sixth day of administration, several days after attainment of the steady-state level and with a standard delay of approximately 12 h between the most recent administration and the blood collection. P4 (ng/mL) values were measured in patient serum using the Immulite 2000. The mean intra-assay coefficient of variation for this assay was 5.6% and the mean inter-assay coefficient of variation for this assay was 8.0%. No changes were made to the assay during the study period to ensure consistent assessment.
Primary outcomes were the absolute change in P4 and the percent change in serum P4 (%ΔP4), live birth or ongoing pregnancy rate (LBOPR), missed abortion, and biochemical pregnancies. Statistical analyses were performed using a free online epidemiologic calculator (http://www.openepi.com/v37/Menu/OE_Menu.htm). Receiver operator characteristic curves examining whether %ΔP4 predicts the LBOPR were also created, and the area under the curve was used to estimate how well P4 predicts live birth or ongoing pregnancy. Chi-squared tests were used to compare categorical outcomes for groups, and t tests were utilized to compare continuous parameters of group demographics and cycle information.
Results
The total number of patients included in the study was 332. The total number of patients excluded was 84, with 22 using vaginal progesterone and 62 requiring an increase in progesterone dose. Of the 332 patients analyzed, the average age of patients was 38.9 years. The majority of the patients received 1 mL/day of P4 (50 mg/mL). Fifteen patients were started and maintained on doses other than 1 mL because of previous cycle data, including 12 patients at 1.5 mL and 1 patient at 0.5, 2, and 3 mL. The same dose was administered each day once started. All patients took their injections at night between the hours of 6:00–9:00 pm.
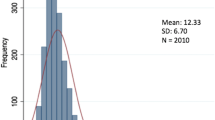
The incidence of live birth or ongoing pregnancy (LBOPR) was associated with both the actual and the percent change in P4 (%ΔP4) between day 19 and day 28. One hundred eighty-eight patients had a negative change, or drop in P4, ranging from −0.1 to −180 ng/mL and −0.5% to −95%. Five patients had no change in their P4, and 139 patients had an increase in their P4 levels ranging from +0.1 to +113 ng/mL and 0.3 to 345%. The average P4 on day 19 was 46.925 ng/mL, and the average P4 on day 28 was 34.1549 ng/mL leading to an average actual change between days 19 and 28 of −12.766 ng/mL. Given that (1) close to 60% of patients had a negative change in P4 but the LBR in this group was still 50% and (2) the range of day 19 P4 and associated negative change was so large, we chose to further investigate whether or not the %ΔP4 would be a better predictor. A receiver operator characteristic curve assessing the ability of %ΔP4 to predict LBOPR had an AUC of 0.704 (Fig. 1).
A cutoff for %ΔP4 of −10% from day 19 to day 28 was used to segregate patients into two groups (Table 1). A cutoff of 10% was deemed to be the lowest change that would likely be clinically significant with the highest sensitivity (Fig. 1). Group A (n = 153) were those patients who had a %ΔP4 that declined by 10% or more and group B (n = 179) were those that had a decline of less than 10%ΔP4 or where P4 rose. Groups A and B were not significantly different in age or number of eggs retrieved. Group B had more embryos transferred at 2.02 ± 0.84 compared to 1.81 ± 0.69 (p < 0.05), although this number is not clinically significant as group B did not have a higher multiple pregnancy live birth rate. Patients in groups A and B had similar BMI; however, not all patients had cycle BMIs recorded as records were transferred to a new electronic medical record. Group A (26%) had a significantly lower LBOPR compared to group B (63%) (p < 0.001, RR 0.42 [0.31–0.56]). These same two groups were not significantly different when pregnancy loss, spontaneous abortion, and biochemical pregnancy combined were compared (21 versus 16%; p < 0.16, RR 1.34 [0.85–2.12]). Both groups had serum P4 levels above 20 ng/mL on day 19 and day 28, but group A had significantly lower serum P4 on both days (day 19 = 30.54 ± 19.18 versus 64.66 ± 43.2, p < 0.001 and day 28 = 26.99 ± 15.19, p < 0.003). Interestingly, a decrease in P4 at 10, 20, or 30% did not result in a statistically significant difference in the spontaneous abortion/biochemical pregnancy between groups.
All patients who had a decrease in serum P4 between days 19 and 28 were then analyzed as a group. A receiver operator characteristic curve was prepared for this group to evaluate whether the change of P4 (%) was predictive of live birth or ongoing pregnancy (Fig. 2). The area under the ROC curve was 0.692, indicating a reasonable ability to predict live birth or ongoing pregnancy (Table 2). Subgroup analyses of patients with a negative change in P4 on day 28 revealed that the incidence of LBOP was significantly different comparing groups above and below the criterion (p < 0.01) at criterion levels of progesterone drop of 10, 20, 30, 40, 50, and 60%. This again highlights the likely meaningful role of maintaining serum P4 levels and the detrimental effect of a drop after transfer.
Discussion
In natural cycles, progesterone is produced by the corpus luteum, at a rate of approximately 20–50 mg a day [11]. It is generally believed that the main functions of P4 are to initiate the proliferative to secretory transition of the endometrium (leading to uterine receptivity for implantation) and to maintain pregnancy once implantation has occurred. Recognizably, then, P4 plays an important role in very early pregnancy development and likely in overall pregnancy success and live birth. After ovulation in natural cycles, typical serum P4 levels are usually between 10 and 20 ng/mL during the mid-luteal phase [12]. In in vitro fertilization, P4 can be supplemented via injectable and mucosal absorption forms in order to mimic the levels seen in natural cycles.
The main goal of this study was to examine the role of serum P4 after embryo transfer and its ability to predict pregnancy outcome. This study revealed that a lower incidence of live birth (and ongoing pregnancy, LBOPR) occurred in association with a 10% or greater drop in serum P4 between day 19 and day 28. Serum P4 during transfers associated with live birth in donor oocyte cycles average 26.7 ng/mL [8]. Interestingly, the mean serum P4 for all of our patients, regardless of degree of %ΔP4, was above this average level at both day 19 and day 28. This suggests against a deficiency of, or supplemental need for, P4 despite its historical role in luteal phase deficiency theories. In fact, the enrollment criteria for this study excluded all patients who required an increase in P4 or who had a low P4 value to start. Despite maintained P4 levels in our patients, drops of the P4 by more than 10% were associated with significantly lower implantation and live birth or ongoing pregnancies. Patients in group B (those with less than −10%ΔP4) did have slightly more embryos transferred (2.02 versus 1.81; p < 0.05). We believe that this is unlikely to have been the major contributor to the LBOPR as this 10% difference in embryos transferred is associated with a 150% increase in live birth or clinical pregnancy. As Table 2 shows, this association of a drop in P4 and lower LBOPR held true in the subgroup analyses of all patients with a negative %ΔP4, in every subgroup analysis from 10 to 60%. This reaffirms the importance of %ΔP4 after transfer in fresh IVF cycles. Furthermore, there has been evidence in spontaneous cycles that a low progesterone level in early pregnancy may be predictive of a non-viable pregnancy [13]. Therefore, our data show that a drop in progesterone likely means a poor outcome, and the predictive value of a drop in serum P4 on live birth rate could aid in the counseling and management of patients undergoing fresh IVF cycles.
The results of this study also emphasize the complex yet precise role of P4 in IVF. In one study, high serum P4 levels at embryo transfer (ET) were associated with decreased uterine contractility and also had a positive association with implantation rates [14]. In practice, if serum P4 levels are low at ET, typically less than 20 ng/mL, then P4 supplementation is usually increased. However, this “rescue” dose escalation has not consistently shown to be effective [8]. Therefore, it seems that there is something inherent to the level of P4 at or just after embryo transfer that is essential to a viable pregnancy. There have been numerous studies that have investigated the role of a change in P4 around the time of HCG trigger administration. Serum P4 level seems to be delicate, as some studies show a negative impact with high serum P4 on day of trigger and some studies have shown that both a high and low serum P4 at the time of trigger can adversely affect implantation and possibly live birth rate [2–7]. Because of this complexity, some researchers believe that neither high nor low P4 at trigger should impact clinical decision-making, such as delaying a fresh cycle to a FET cycle based on serum P4 [7]. It seems a reasonable deduction that a second factor, such as %ΔP4 after transfer, may play a large role in determining the impact of serum P4 on LBR and may also help illuminate the underlying meaning of P4 at trigger and just after. The concept of the implantation window deserves mention, and this extra metric (%ΔP4) may be used to further elucidate a patient’s implantation window.
Interestingly, parallel research has also shown that high serum P4 at trigger has a positive or direct correlation on the number of oocytes retrieved, without an obvious effect on quality [3, 6, 15–17]. A study of the cumulative effects of fresh and FET cycles has shown that elevated serum P4, previously repeatedly reported to have a negative impact on LBR, may actually depend on ovarian response [15]. In fact, another study showed that the fertilization rate increases when P4 increases the day after trigger and that this increase may have a predictive value on the total number of oocytes retrieved [17]. Taking these data into consideration, it is reasonable to infer that serum P4 may be in sensitive balance with ovarian signals, which also may impact the function, and levels, of P4 after transfer.
There are also limitations to this study. The biggest limitations of this study include (1) inclusion of only fresh cycles, (2) collection of data from a single center, and (3) the retrospective study design. Further limitations include the exclusion of patients using vaginal progesterone suppositories as the amount of absorption of P4 was too difficult to measure. It is important to note that vaginal progesterone is widely used, especially among patients who cannot tolerate injectable P4. However, the exclusion of vaginal progesterone suppositories was absolutely necessary given the differential absorption characteristics and serum dynamics with this method of supplementation. Several studies, as mentioned above, have evaluated serum P4 levels on day of trigger and their impact on cycle outcome. It is not the routine practice of this center to measure serum P4 levels on day of trigger, and therefore, this information was not included in this study. However, future investigation could include this data point to further elucidate the impact serum progesterone trend.
Lastly, this study only investigated fresh IVF with day 5/6 embryo transfers. Future investigation on donor oocyte and in cycles using other stimulation protocols is warranted for the generalizability of our results. In addition, potential research into the impacts of other factors, such as obesity and endometrial thickness, and their influence on P4 luteal requirement and P4 change would be another helpful addition to help clarify the intricate nature of the implantation window.
The results of this study could potentially impact clinical practice. For those patients who have a 10% or greater drop in progesterone on day 28, it may allow for prediction of cycle outcome after transfer and possibly used in conjunction with the pregnancy test.
References
Lessey BA. Two pathways of progesterone action in the human endometrium: implications for implantation and contraception. Steroids. 2003;68(10):809–15.
Santos-Ribeiro S, Polyzos NP, Haentjens P, Smitz J, Camus M, Tournaye H, et al. Live birth rates after IVF are reduced by both low and high progesterone levels on the day of human chorionic gonadotrophin administration. Hum Reprod. 2014;29:1698–705.
Venetis CA, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60,000 cycles. Reprod Biomed Online. 2012;97:1321–7.
Huang R, Fang C, Xu S, Yi Y, Liang X. Premature progesterone rise negatively correlated with live birth rate in IVF cycles with GnRH agonist: an analysis of 2,566 cycles. Fertil Steril. 2012;98:644–70.
Burns WN, Witz CA, Klein NA, Silverberg KM, Schenken RS. Serum progesterone concentrations on the day after human chorionic gonadotrophin administration and progesterone/oocyte ratios predict in vitro fertilization/embryo transfer outcome. J Assist Reprod Genet. 1994;11:17–23.
Huang CC, Lien YR, Chen HF, Chen MJ, Shieh CJ, et al. The duration of pre-ovulatory serum progesterone elevation before hcg administration affects the outcome of IVF/ICSI cycles. Hum Reprod. 2012;27:2036–45.
Check JH, Amui J, Choe JK, Brasile D. Relationship of serum progesterone level the day after human chorionic gonadotropin injection on outcome following in vitro fertilization embryo transfer. Clin Exp Obstet Gynecol. 2009;36:214–5.
Brady PC, Kaser DJ, Ginsburg ES, Ashby RK, Missmer SA, Correia KF, et al. Serum progesterone concentration on day of embryo transfer in donor oocyte cycles. J Assist Reprod Gen. 2014;31:569–75.
Kofinas JD, Blakemore J, McCulloh DH, Grifo J. Serum progesterone levels greater than 20 ng/mL on day of embryo transfer are associated with lower live birth and higher pregnancy loss rates. J Assist Reprod Genet. 2015;32(9):1395–9.
Paulsen RJ, Collins MG, Yankov VI. Progesterone pharmacokinetics and pharmacodynamics with 3 dosages and 2 regimens of an effervescent micronized progesterone vaginal insert. J Clin Endocrinol Metab. 2014;99(11):4241–9.
Strauss JF, Williams CJ. The ovarian life cyle. In: Strauss JF, Barbieri RL, eds. Reproductive endocrinology, 6th ed. Saunders, 2009: 155–90.
Sallam HN, Sallam A, Ezzeldin F, Agamia AF, ABou-Ali A. Reference values for the midluteal plasma progesterone concentration: evidence from human menopausal gonadotropin-stimulated pregnancy cycles. Fertil Steril. 1999;71:711–14.
Verheagen J, Gallos ID, van Mello NM, Abdel-Aziz M, Takwoingi Y, Harb H, Deeks JJ, Mol BW, Coomarasamy A. Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. Brit Med J. 2012: e6077.
Fanchin R, Righini C, Olivennes F, Taylor S, de Ziegler D, Frydman R. Uterine contractions at the time of embryo transfer alter pregnancy rates after in-vitro fertilization. Hum Reprod. 1998;13:1968–74.
Bu Z, Zhao F, Wang K, Guo Y, Su Y, Zhai J, et al. Serum progesterone elevation adversely affects cumulative live birth rate in different ovarian responders during in vitro fertilization and embryo transfer: a large retrospective study. PLOSone. 2014;9:e100011.
Cai Q, Wan F, Appleby D, Hu L. Quality of embryos transferred and progesterone levels are the most important predictors of live birth after fresh embryo transfer: a retrospective cohort study. J Assist Reprod Genet. 2014;31:185–94.
Zhu H, Liu L, Yang L, Xue Y, Tong X, Jiang L, et al. The effect of progesterone level prior to oocyte retrieval on the numbers of oocytes retrieved and embryo quality in IVF treatment cycles: an analysis of 2978 cycles. J Assist Reprod Genet. 2014;31:1183–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Blakemore, J.K., Kofinas, J.D., McCulloh, D.H. et al. Serum progesterone trend after day of transfer predicts live birth in fresh IVF cycles. J Assist Reprod Genet 34, 339–343 (2017). https://doi.org/10.1007/s10815-016-0859-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0859-1