Abstract
Purpose
This publication will evaluate the available evidence in the literature comparing fresh embryo transfer (ET) and elective frozen-thawed embryo transfer (FET) regarding the possible interference of controlled ovarian stimulation (COS) in implantation and endometrial receptivity, IVF safety, and obstetric and perinatal outcomes.
Methods
We performed a review in the literature of the available evidence comparing fresh to elective FET (freeze-all policy).
Results
The improvements made in cryopreservation techniques have led to few or no detrimental effects to the embryo and have resulted in no consequences to the offspring when compared to fresh embryos; this has allowed reproductive practitioners to create the freeze-all policy (when all viable embryos are electively cryopreserved in the fresh cycle and transferred in a posterior cycle). There are increasing concerns about the adverse effects associated with COS over the endometrial and uterine environments, as well as with the safety of COS in pregnancies that have originated from fresh ET during in vitro fertilization (IVF) treatments. COS may contribute to modifications in the endometrium, which might be related to poorer outcomes when fresh ET is performed. It has been suggested that obstetric and perinatal outcomes in pregnancies resulting from fresh ET are poorer when compared with those that occur after FET. In cycles with fresh ET, there is still a risk of ovarian hyperstimulation syndrome (OHSS).
Conclusion
There is growing evidence in the literature suggesting better IVF outcomes, and decreased obstetric and perinatal morbidity when adopting the freeze-all policy instead of fresh ET.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In vitro fertilization (IVF) has been performed for more than 30 years, and it is estimated that in developed countries, more than 1 % of all births are generated from assisted reproductive therapies (ART) [1]. Controlled ovarian stimulation (COS) is considered an essential step during IVF treatments, as its main objective is to induce the development of multiple follicles and maximize the chances of a positive outcome [2].
Nowadays, fresh embryo transfer (ET) is the norm in ART procedures. However, there are increasing concerns about the adverse effects of COS over the endometrial and uterine environment, as well as regarding the safety of COS in pregnancies that have originated from ART. There is growing evidence that COS may contribute to modifications in the endometrium, which might be related to poorer outcomes when fresh ET is performed [3]. It has been suggested that obstetric and perinatal outcomes in pregnancies following ART are poorer when compared with those that occur after spontaneous conception [4, 5]; however, this can differ among fresh ET and frozen–thawed embryo transfer (FET) [6]. In cycles with fresh ET, there is still a risk for the development of severe ovarian hyperstimulation syndrome (OHSS), which is an iatrogenic, serious, and potentially life-threatening complication of ovarian stimulation; it occurs in around 1–14 % of IVF cycles [7, 8], and the use of antagonist protocols with a gonadotropin-releasing hormone agonist (GnRHa) trigger and subsequent elective cryopreservation of all embryos would almost eliminate the risk of OHSS [9].
With the advances made in cryopreservation techniques, the quality of the frozen embryos and their potential for implantation are similar to those observed with fresh embryos [10, 11]. Thus, it would be plausible to discuss the freeze-all policy, which is performed with the elective cryopreservation of all viable embryos in a fresh IVF or IVF/ICSI cycle and the future transfer of frozen–thawed embryos. The objective of this policy is to place the embryos in a more favorable intrauterine environment, without facing the possible adverse effects of supraphysiologic hormonal levels over the endometrial receptivity [12].
Implantation is one of the most important steps for achieving ART success, and its effectiveness relies upon embryo quality, a reciprocal blastocyst–endometrium interaction (which is dependent on factors such as embryo and endometrium quality), and endometrial receptivity [3, 13]. In the past few years, most of the improvements in IVF techniques have been based on embryo quality. Most of the studies on this issue have focused on embryo improvements, but they have not been concerned with the intrauterine microenvironment and its consequences on embryo implantation [14]. This publication will evaluate the available evidence in the literature comparing fresh ET and elective FET regarding the possible interference of COS in implantation and endometrial receptivity, IVF safety, and obstetric and perinatal outcomes.
COS and endometrial receptivity
The implantation window is a self-limited period marked by structural and functional maturation of the endometrium, which is necessary for blastocyst attachment. During this period, the endometrium undergoes transformations mediated by a large number of genes and gene products, which are differentially expressed during the receptive phase of the menstrual cycle [15]. Many genes related to endometrial receptivity are regulated by hormones [16], and the COS may alter the gene expression of more than 200 genes related to implantation when compared to natural cycles without hormone stimulation [17–19]. These modifications may occur both under GnRHa and GnRH antagonist protocols for ovarian stimulation [20].
There is evidence that the supraphysiologic levels of estradiol and progesterone during COS could lead to morphologic and biochemical modifications, and consequently impair endometrial receptivity. Such changes may lead to embryo–endometrium asynchrony, thereby reducing the implantation rates during IVF/ICSI treatments [21–23]. Higher levels of estradiol may lead to alterations in endometrial maturation and implantation [24]. In the final follicular phase, the subtle increases in progesterone levels are associated with advancements in the endometrium’s ultrastructural morphology and echogenicity [25, 26], and these levels seem to have a negative impact on embryo implantation [27, 28]. Some authors have demonstrated that when this endometrial advancement exceeds 3 days, pregnancy is not achieved if fresh ET is performed [19, 23]. These alterations may result in embryo–endometrium asynchrony, and they may decrease the implantation rates during ART treatments [3]. However, to date, there is no consensus regarding at what threshold a cycle becomes supraphysiologic and may lead to changes in endometrial receptivity [29].
All of these hormonal changes discussed above do not seem to impact embryo quality [21]. Studies on oocyte donation programs have demonstrated that increases in progesterone levels in donors have no adverse effects on oocyte quality and in the implantation rates in recipients, corroborating the fact that progesterone levels do not impact embryo quality, but they probably influence the endometrium [30, 31].
Endometrial development and priming are controlled more precisely during frozen–thawed cycles when compared to COS with gonadotropins, and this could be related to better endometrial receptivity [32], favoring those patients adopting the freeze-all policy.
COS and uterine contractility
It is known that uterine contractions (UC) at the time of embryo transfer adversely affect IVF outcomes [33], and that supraphysiologic hormonal levels may increase these UC [34]. Some studies found that uterine contractility is much higher in stimulated cycles than in natural cycles [35]; however, there are no studies comparing COS cycles and cycles with endometrial priming for FET. We can hypothesize that during FET, due the lower hormonal levels, the UC would be lower than in the fresh ET, because high concentrations of circulating E2 in IVF patients may increase these UC [36]. These effects of UC seems to be more important for cleavage-stage embryo transfer because the contractility decreases progressively and reaches a nearly quiescent status at the time of blastocyst transfer [37].
IVF and OHSS – the OHSS-free clinic concept
OHSS is an iatrogenic, potentially lethal, and still one of the major complications encountered during COS in IVF [38]. It occurs in approximately 1–14 % of ART cycles and is related to increased vascular permeability (VP) [7, 8]. Human chorionic gonadotropin (hCG), either exogenous or endogenous, is the most probable triggering factor of this syndrome [39]. Following the administration of hCG, the expression of vascular endothelial growth factor (VEGF) and VEGF receptor 2 (VEGFR-2) mRNA increases significantly, rising to a maximum level that coincides with peaked VP. These findings suggest that the syndrome can be prevented by inducing ovulation with a GnRHa instead of hCG, preventing VEGF overexpression [40]. This strategy would prevent the early, but not the late, onset of OHSS.
The prevention of OHSS is the most important aspect of its management [41]. In the past few years, several preventive measures have been developed to prevent its onset, but until now, the most effective method is to substitute the use of hCG by administering a GnRHa for final oocyte maturation and by introducing the freeze-all strategy [42]. Devroey and colleagues introduced the concept of an OHSS-free clinic, in which the trigger of final oocyte maturation in patients with an antagonist protocol should be performed with the use of a GnRHa and via the cryopreservation of all embryos – not by performing the fresh ET [42]. This strategy virtually eliminates the onset of early and late OHSS [43], although two recent publications reported three cases of OHSS in patients triggered with GnRHa in antagonist GnRH cycles and following the adoption of a freeze-all strategy [44, 45].
Cryopreservation
With the advent and improvement of the vitrification technique, oocyte cryopreservation has become an alternative and good option for patients performing an IVF cycle, mainly in those with an increased risk for OHSS. The oocyte survival rates after vitrification are excellent [46, 47], and the pregnancy rates and safety levels using vitrified oocytes may be comparable to those associated with fresh oocytes [48].
Following the first description of a pregnancy resulting from FET [49], the embryo cryopreservation technique has evolved and become an established, safe, and effective procedure during IVF treatments [50]. Embryo cryopreservation was previously successfully performed with slow-freezing methods, and in the past few years, the vitrification method has become increasingly more utilized, showing excellent results with up to a 95 % survival rate of vitrified blastocysts [10]. There is still no consensus regarding which of the techniques (slow freezing versus vitrification) is best for embryo cryopreservation, although some recent studies have shown better results with vitrification [51, 52]. There is no evidence regarding the consequences to the offspring originated from cryopreserved embryos [53]. The transfer of frozen–thawed embryos does not seem to have an adverse effect on neonatal outcomes [54]. Thus, the improvements in the cryopreservation techniques leading to the absence of detrimental effects to the embryo, and no consequences to the offspring when compared to fresh embryos, allowed reproductive practitioners to create the freeze-all policy.
IVF/ICSI outcomes of fresh versus frozen–thawed ET
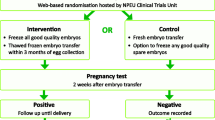
Considering all the possible side effects of COS on endometrial receptivity, as discussed above, recent studies have shown better IVF outcomes when performing elective FET. Furthermore, using the freeze-all strategy, there is an advantage in that the entire cohort of embryos is cryopreserved – not just the “second best”, which is what occurs when the morphologically best embryos are transferred in a fresh cycle [55]. A recent meta-analysis showed an increase of 32 % in the ongoing pregnancy rate when elective FET was performed when compared to FET [3]. There are only three randomized clinical trials (RCTs) [56–58] in the literature that have compared the IVF outcomes of fresh ET and elective FET. All of them showed better results in the elective FET cycles. However, all of these studies only evaluated patients with a good prognosis. There is a recent cohort study that has evaluated the freeze-all strategy in patients with a previous failed blastocyst transfer. The researchers found encouraging results, showing an odds ratio for live births of 3.8 when using the freeze-all policy instead of fresh ET [59]. There is still a lack of higher-quality RCTs regarding the freeze-all policy and its relationship to IVF outcomes, the best developmental stage for embryo cryopreservation when applying this strategy, and the best endometrial priming to perform the FET.
Obstetric and perinatal outcomes from fresh ET compared to frozen–thawed ET
In a recent review and meta-analysis, Pandey et al. concluded that the risks of obstetric and perinatal complications are higher in singleton pregnancies after IVF/ICSI when compared with natural conception [4]. However, some observational studies have suggested that pregnancies that occurred after FET seem to have better obstetric and perinatal outcomes when compared to fresh ET [6], suggesting an advantage in performing FET than fresh ET.
It seems that ectopic pregnancy is more frequent in pregnancies that result from IVF treatments when compared to natural pregnancies. This higher risk would be related to increased UC and supraphysiologic hormonal levels during COS [60]. The COS and the supraphysiologic hormonal levels may be related to altered placentation, leading to an increased risk of pre-eclampsia, low birth weight, prematurity, small size for gestational age, antepartum hemorrhage, and perinatal death [6, 53, 61]. When comparing the risk of major congenital anomalies between children conceived after fresh ET and FET, no difference between the techniques was shown [62]. In other hand, there is an increased risk of macrosomia in singletons born after FET when comparing to fresh embryo transfer [63].
Pre-implantation genetic screening (PGS)
Nowadays, there is a trend toward performing the PGS in the blastocyst stage with 24-chromosome screening. There are growing evidence showing higher implantation and delivery rates following the 24-chromosome screening when compared to fluorescent in-situ hybridization (FISH) PGS [64]. The use of comprehensive chromosome screening (CCS) in blastocyst stage with elective single embryo transfer (eSET) is as effective as double-embryo transfer of unscreened embryos and dramatically reduce the risk of twins [65]. However, it is unclear if the screened embryo transfer results in better outcomes when performed in fresh or FET cycles [66]. Sometimes, it is not possible to obtain the screening result within the implantation window. The embryos that the biopsy needs to be performed on day 6 are not eligible for fresh embryo transfer due to an asynchrony between the embryo and endometrium. In these cases, it is necessary to perform the cryopreservation of all embryos and a posterior frozen-thawed embryo transfer [67].
Costs
Regardless of the growing evidence favoring the freeze-all strategy, there are, unfortunately, no studies concerning the cost-effectiveness of elective FET when compared to fresh ET. It is necessary to conduct these studies to determine whether a change in policy (performing elective FET instead of fresh ET) is cost effective when considering the cryopreservation costs, the costs associated with endometrial priming, and even the emotional distress that arises for patients that did not undergo fresh ET.
Conclusion
There is growing evidence in the literature suggesting better IVF outcomes when adopting the freeze-all policy instead of fresh ET. Most of these differences stem from the consequences associated with COS on endometrial receptivity. More important than the pregnancy and implantation rates is the safety of the ART procedures. It seems that the freeze-all policy may decrease the risks of OHSS development, as well as obstetric and perinatal morbidity and mortality. More research and RCTs are necessary to establish a change in the routine policy regarding embryo transfer.
References
Sutcliffe AG, Ludwig M. Outcome of assisted reproduction. Lancet. 2007;370(9584):351–9.
Siristatidis C, Sergentanis TN, Kanavidis P, Trivella M, Mavromatis I, Psaltopoulou T, et al. Controlled ovarian hyperstimulation for IVF: impact on ovarian, endometrial and cervical câncer – a systematic review and meta-analysis. Hum Reprod Update. 2013;19:105–23.
Roque M, Lattes K, Serra S, Solà I, Geber S, Carreras R, et al. Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril. 2013;99:156–62.
Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update. 2012;18:485–503.
Pinborg A, Wennerholm UB, Romundstad LB, Loft A, Aittomaki K, Söderström-Anttila V, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcomes? Systematic review and meta-analysis. Hum Reprod Update. 2013;19:87–104.
Maheshwari A, Pandey S, Shetty A, Hamilton M, Bhattacharya S. Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of frozen thawed versus fresh embryos generated through in vitro fertilization treatment: a systematic review and meta-analysis. Fertil Steril. 2012;98:368–77.
Nastri CO, Ferriani RA, Rocha IA, Martins WP. Ovarian hyperstimulation syndrome: pathophysiology and prevention. J Assist Reprod Genet. 2010;27:121–8.
Youssef MA, van Wely M, Hassan MA, Al-Inany HG, Mochtar M, Khattab S, et al. Can dopamine agonists reduce the incidence and severity of OHSS in IVF/ICSI treatment cycles? A systematic review and meta-analysis. Hum Reprod Update. 2010;16:459–66.
Griesinger G, Schultz L, Bauer T, Broessner A, Frambach T, Kissler S. Ovarian hyperstimulation syndrome prevention by gonadotropin-releasing hormone agonist triggering of final oocyte maturation in a gonadotropin-releasing hormone antagonist protocol in combination with a ‘freeze-all’ strategy: a prospective multicentric study. Fertil Steril. 2011;95:2029–33.
Cobo A, de los Santos MJ, Castellò D, Gámiz P, Campos P, Remohí J. Outcomes of vitrified early cleavage-stage and blastocyst-stage embryos in a cryopreservation program: evaluation of 3,150 warming cycles. Fertil Steril. 2012;98:1138–46.
Herrero L, Matínez M, Garcia-Velasco JA. Current status of human oocyte and embryo cryopreservation. Curr Opin Obstet Gynecol. 2011;23:245–50.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. High ongoing pregnancy rates after deferred transfer through bipronuclear oocyte cryopreservation and post-thaw extended culture. Fertil Steril. 2009;92:1594–9.
Diedrich K, Fauser BC, Devroey P, Griesinger G, Evian Annual Reproduction (EVAR) Workshop Group. The role of the endometrium and embryo in human implantation. Hum Reprod Update. 2007;13:365–77.
Evans J, Hannan NJ, Edgell TA, Vollenhoven BJ, Lutjen PJ, Osianlis T et al. Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Hum Reprod. 2014.
Bhagwat SR, Chandrashekar DS, Kakar R, Davuluri S, Bajpai AK, Nayak S, et al. Endometrial receptivity: a revisit to functional genomics studies on human endometrium and creation of HGEx-ERdb. PLoS One. 2013;8:e58419.
Schubert C. World of reproductive biology. Biol Reprod. 2014;91:1. doi:10.1095/biolreprod.114.121335.
Horcajadas JA, Riesewijk A, Polman J, van Os R, Pellicer A, Mosselman S, et al. Effect of controlled ovarian hyperstimulation in IVF on endometrial gene expression profiles. Mol Hum Reprod. 2005;11:195–205.
Labarta E, Martínez-Conejero JA, Alamá P, Horcajadas JA, Pellicer A, Simón C, et al. Endometrial receptivity is affected in women with high circulatin progesterone levels at the end of the follicular phase: a functional genomics analysis. Hum Reprod. 2011;26:1813–25.
Van Vaerenbergh I, Fatemi HM, Blockeel C, Van Lommel L, In’t Veid P, Schuit F, et al. Progesterone rise on HCG day in GnRH antagonist/rFSH stimulated cycles affects endometrial gene expression. Reprod Biomed Online. 2011;22:263–71.
Haouzi D, Assou S, Dechanet C, Anahory T, Dechaud H, De Vos J, et al. Controlled ovarian hyperstimulation for in vitro fertilization alters endometrial receptivity in humans: protocol effects. Biol Reprod. 2010;82:679–86.
Bourgain C, Devroey P. The endometrium in stimulated cycles for IVF. Hum Reprod Update. 2003;9:515–22.
Devroey P, Bourgain C, Macklon NS, Fauser BC. Reproductive biology and IVF: ovarian stimulation and endometrial receptivity. Trends Endocrinol Metab. 2004;15:84–90.
Kolibianakis E, Bourgain C, Albano C, Osmanagaoglu K, Smitz J, Van Steirteghem A, et al. Effect of ovarian stimulation with recombinant follicle-stimulating hormone, gonadotropin releasing hormone antagonists, and human chorionic gonadotropin on endometrial maturation on the day of oocyte pick-up. Fertil Steril. 2002;78:1025–9.
Groothuis PG, Dassen HHNM, Romano A, Punyadeera C. Estrogen and the endometrium: lessons learned from gene expression profiling in rodents and human. Hum Reprod Update. 2007;13:405–17.
Nikas G, Develioglu OH, Toner JP, Jones Jr HW. Endometrial pinopodes indicate a shift in the window of receptivity in IVF cycles. Hum Reprod. 1999;14:787–92.
Venetis CA, Kolibianakis EM, Papanikolaou E, Bontis J, Devroey P, Tarlatzis BC. Is progesterone elevation on the day of human chorionic gonadotrophin administration associated with the probability of pregnancy in in vitro fertilization? A systematic review and meta-analysis. Hum Reprod Update. 2007;13:343–55.
Kiliçdag EB, Haydardedeoglu B, Cok T, Hacivelioglu SO, Bagis T. Premature progesterone elevation impairs implantation and live birth rates in GnRH-agonist IVF/ICSI cycles. Arch Gynecol Obstet. 2010;281:747–52.
Huang R, Fang C, Xu S, Yi Y, Liang X. Premature progesterone rise negatively correlated with birth rate in IVF cycles with GnRH agonist: an analysis of 2,566 cycles. Fertil Steril. 2012;98:664–70.
Barnhart KT. Introduction: are we ready to eliminate the transfer of fresh embryos in in vitro fertilization? Fertil Steril. 2014;102:1–2.
Melo MA, Meseguer M, Garrido N, Bosch E, Pellicer A, Remohi J. The significance of premature luteinization in an oocyte-donation programme. Hum Reprod. 2006;21:1503–7.
Check JH, Wilson C, Choe JK, Amui J, Brasile D. Evidence that high serum progesterone (P) levels on day of human chorionic gonadotropin (hCG) injection have no adverse effect on the embryo itself as determined by pregnancy outcome following embryo transfer using donated eggs. Clin Exp Obstet Gynecol. 2010;37:179–80.
Richter KS, Shipley SK, McVearry I, Tucker MJ, Widra EA. Cryopreserved embryo transfers suggest that endometrial receptivity may contribute to reduced success rates of later developing embryos. Fertil Steril. 2006;86:862–6.
Fanchin R, Righini C, Olivennes F, Taylor S, de Ziegler D, Frydman R. Uterine contractions at the time of embryo transfer alter pregnancy rates after in-vitro fertilization. Hum Reprod. 1998;13:1968–74.
Fanchin R, Ayoubi JM, Olivennes F, Righini C, de Ziegler D, Frydman R. Hormonal influence on the uterine contractility during ovarian stimulation. Hum Reprod. 2000;15 Suppl 1:90–100.
Zhu L, Li Y, Xu A. Influence of controlled ovarian hyperstimulation on uterine peristalsis in infertile women. Hum Reprod. 2012;27:2684–9.
Moraloglu O, Tonguc E, Var T, Zeyrek T, Batioglu S. Treatment with oxytocin antagonists before embryo transfer may increase implantation rates after IVF. Reprod Biomed Online. 2010;21:338–43.
Fanchin R, Ayoubi JM, Righini C, Olivennes F, Schönauer LM, Frydman R. Uterine contractility decreases at the time of blastocyst transfers. Hum Reprod. 2001;16:1115–9.
de Mouzon J, Goossens V, Bhattacharya S, Castilla JA, Ferraretti AP, Korsak V, et al. Assisted reproductive technology in Europe, 2007: results generated from European registers by ESHRE. Hum Reprod. 2012;27:954–66.
Humaidan P, Quartarolo J, Papanikolaou EG. Preventing ovarian hyperstimulation syndrome: guidance for the clinician. Fertil Steril. 2010;94:389–400.
Gómez R, Soares SR, Busso C, Garcia-Velasco JA, Simón C, Pellicer A. Physiology and pathology of ovarian hyperstimulation syndrome. Semin Reprod Med. 2010;28:448–57.
Aboulghar M. Symposium: update on prediction and management of OHSS. Prevention of OHSS. Reprod Biomed Online. 2009;19:33–42.
Devroey P, Polyzos NP, Blockeel C. An OHSS-Free Clinic by segmentation of IVF treatment. Hum Reprod. 2011;26:2593–7.
Kol S, Humaidan P. GnRH agonist triggering: recent developments. Reprod Biomed Online. 2013;26:226–30.
Fatemi HM, Popovic-Todorovic B, Humaidan P, Kol S, Banker M, Devroey P, et al. Severe ovarian hyperstimulation syndrome after gonadotropin-releasing hormone (GnRH) agonist trigger and “freeze-all” approach in GnRH antagonist protocol. Fertil Steril. 2014;101:1008–11.
Ling LP, Phoon JW, Lau MS, Chan JK, Viardot-Foucault V, Tan TY, et al. GnRH agonist trigger and ovarian hyperstimulation syndrome: rellok at ‘freeze-all strategy’. Reprod Biomed Online. 2014. doi:10.1016/j.rbmo.2014.05.012.
Kuwayama M, Vatja G, Kato O, Leibo SP. Highly efficient vitrification methid for cryopreservation of human oocytes. Reprod Biomed Online. 2005;11:300–8.
Nagy ZP, Chang CC, Shapiro DB, Bernal DP, Kort HI, Vatja G. The efficacy and safety of human oocyte vitrification. Semin Reprod Med. 2009;27:450–5.
Cobo A, Meseguer M, Remohí J, Pellicer A. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Hum Reprod. 2010;25:2239–46.
Trounson A, Mohr L. Human pregnancy following cryopreservation, thawing and transfer of an eight-cell embryo. Nature. 1983;305:707–9.
Bedoschi G, Oktay K. Current approach to fertility preservation by embryo cryopreservation. Fertil Steril. 2013;99:1496–502.
Loutradi KE, Kolibianakis EM, Venetis CA, Papanikolaou EG, Pados G, Bontis I, et al. Cryopreservation of human embryos by vitrification or slow freezing: a systematic review and meta-analysis. Fertil Steril. 2008;90:186–93.
AbdelHafez FF, Desai N, Abou-Setta AM, Falcone T, Goldfarb J. Slow freezing, vitrification and ultra-rapid freezing of human embryos: a systematic review and meta-analysis. Reprod Biomed Online. 2010;20:209–22.
Ishihara O, Araki R, Kuwahara A, Itakura A, Saito H, Adamson GD. Impact of frozen-thawed single-blastocyst transfer on maternal and neonatal outcome: an analysis of 277,042 single-embryo transfer cycles from 2008 to 2010 in Japan. Fertil Steril. 2014;101:128–33.
Liu SY, Teng B, Fu J, Li X, Zheng Y, Sun XX. Obstetric and neonatal outcomes after transfer of vitrified early cleavage embryos. Hum Reprod. 2013;28:2093–100.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C. Clinical rationale for cryopreservation of entire embryo cohorts in lieu of fresh transfer. Fertil Steril. 2014;102:3–9.
Aflatoonian A, Oskouian H, Ahmadi S, Oskouian L. Can fresh embryo transfers be replaced by cryopreserved-thawed embryo transfers in assisted reproductive cycles? A randomized controlled trial. J Assist Reprod Genet. 2010;27:357–63.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril. 2011;96:344–8.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfers in high responders. Fertil Steril. 2011;96:516–8.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C. Freeze-all can be a superior therapy to another fresh cycle in patients with prior fresh blastocyst implantation failure. Reprod Biomed Online. 2014;29:286–90. doi:10.1016/j.rbmo.2014.04.009.
Shapiro BS, Daneshmand ST, De Leon L, Garner FC, Aguirre M, Hudson C. Frozen-thawed embryo transfer is associated with significantly reduced incidence of ectopic pregnancy. Fertil Steril. 2012;98:1490–4.
Wennerholm UB, Henningsen AK, Romundstad LB, Bergh C, Pinborg A, Skjaerven R, et al. Perinatal outcomes of children born after frozen-thawed embryo transfer: a Nordic cohort study from the CoNARTaS group. Hum Reprod. 2013;28:2545–53.
Pelkonen S, Hartikainen AL, Ritvanen A, Koivunen R, Martikainen H, Gissler M, et al. Major congenital anomalies in children born after frozen thawed embryo transfer: a cohort study 1995–2006. Hum Reprod. 2014;29.
Pinborg A, Henningsen AA, Loft A, Malchau SS, Forman J, Andersen AN. Large baby syndrome in singletons born after frozen embryo transfer (FET): is it due to maternal factors or the cryotechnique? Hum Reprod. 2014;29:618–27.
Scott Jr RT, Franasiak JM, Forman EJ. Comprehensive chromosome screening with synchronous blastocyst transfer: time for a paradigm shift. Fertil Steril. 2014;102:660–1.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100:100–7.
Hill D, Surrey M, Danzer H, Ghadir S, Chang W, Barritt J. Significant improvement in pregnancy rates following frozen embryo transfers when combined with microarray-comparative genomic hybridization (aCGH). Fertil Steril. 2013;3:S108–9.
Rubio C, Rodrigo L, Mir P, Mateu E, Peinado V, Milán M, et al. Use of array comparative genomic hybridization (array-CGH) for embryo assessment: clinical results. Fertil Steril. 2013;99:1044–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Freeze-all policy is a viable strategy for IVF cycles and it is related to better IVF outcomes and decreased obstetric and perinatal morbidity.
Rights and permissions
About this article
Cite this article
Roque, M. Freeze-all policy: is it time for that?. J Assist Reprod Genet 32, 171–176 (2015). https://doi.org/10.1007/s10815-014-0391-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-014-0391-0