Abstract
Purpose
To determine benefits of cleavage-stage preimplantation genetic screening (PGS) by array comparative genomic hybridization (CGH).
Methods
A retrospective case–control study was performed at a tertiary care university-affiliated medical center. Implantation rate was looked at as a primary outcome. Secondary outcomes included clinical and ongoing pregnancy rates, as well as multiple pregnancy and miscarriage rates. Thirty five patients underwent 39 fresh cycles with PGS by aCGH and 311 similar patients underwent 394 invitro fertilization cycles.
Result(s)
The implantation rate in the CGH group doubled when compared to the control group (52.63 % vs. 19.15 %, p = <0.001), clinical pregnancy rate was higher (69.23 % vs. 43.91 %, p = 0.0002), ongoing pregnancy rate almost doubled (61.54 % vs. 32.49 %, p = <0.0001), multiple pregnancy rate decreased (8.33 % vs. 34.38 %, p = 0.0082) and miscarriage rate trended lower (11.11 % vs. 26.01 %, p = 0.13).
Conclusion
Cleavage stage PGS with CGH is a feasible and safe option for aneuploidy screening that shows excellent outcomes when used in fresh cycles. This is the first report of cleavage stage PGS by CGH showing improved ongoing pregnancy rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Initial reports that aneuploidy employing FISH technology could be directly related to infertility were published in the early 1990s [5, 16, 23]. It is now accepted that the incidence of aneuploidy in embryos increases with maternal age [13]. Aneuploidy is the most common cause of miscarriage and the most common genetic abnormality in embryos [6, 24].
Fluorescence in situ hybridization (FISH) was the mainstay of preimplantation genetic screening (PGS) over the past two decades. During these years it confirmed the high rate of aneuploidy in failed cycles and miscarriages. Although initially promising, its limitations were clearly exposed. Numerous authors failed to show improvement of IVF outcomes with PGS by FISH [7, 10, 11, 20, 29, 33, 34, 36], and the European Society for Human Reproduction (ESHRE) recently recommended that this technique should be replaced by comprehensive methods of screening [12].
As opposed to FISH, CGH works by analyzing all 24 chromosomes, allowing more accurate results when detecting for aneuploidy. There are several methods of comprehensive chromosome screening (CCS), including single nucleotide polymorphism (SNP) array, CGH, and quantitative polymerase chain reaction (PCR) [9]. Studies comparing FISH with SNP array showed up to a 60 % false-positive rate with FISH. When FISH was compared to CCS, it was found that mosaicism was three times more common in FISH [35]. When compared to polar body biopsy it was found that blastomere biopsy with CCS was very accurate (94.2 %) when compared to trophoectoderm biopsy with CCS [3]. These findings support analysis of cleavage-stage biopsy with CCS techniques such as SNP or CGH, so that PGS could still be utilized with fresh-embryo transfer.
It remains unclear whether application of CCS technology for embryo selection following cleavage stage biopsy has the potential of improving implantation and pregnancy rates per cycle. We hypothesized that euploid embryos would have improved implantation despite the concern about trauma at the time of blastomere biopsy.
Materials and methods
This study was approved by the St. Luke’s-Roosevelt institutional review board. A retrospective case–control study was performed. We reviewed the Continuum Reproductive Center’s database from 2009 and 2012. During the period, a total of 35 patients underwent 39 fresh transfer cycles in which PGS was performed through CGH. All cycles starts were included in the study, regardless of their transfer status during the same time period. The indications for PGS included advanced maternal age, recurrent implantation failure (RIF) (≥2 IVF failures) and recurrent pregnancy loss (RPL) (≥2 pregnancy losses). The control group consisted of all 394 fresh, non-donor IVF cycles that resulted in at least five healthy-appearing embryos, as we do not offer PGS in general with less than five embryos produced.
The primary outcome measure was implantation rate. Clinical pregnancy, ongoing pregnancy, miscarriage and multiple pregnancy rates were the secondary outcomes assessed.
In the cycles undergoing aCGH, laser-assisted biopsy for PGS was performed at cleavage stage to remove a single blastomere. We used Genesis Genetics Institute (Detroit, USA) for our PGS, running their Genesis-24 technology. Blastomeres underwent CGH with Bacterial Artificial Chromosomes (BACs). We received the report from the lab on day five and chose which embryos to transfer.
All cycles underwent controlled ovarian hyperstimulation protocols. The dose of gonadotropins (FSH and/or human menopausal gonadotropins (hMG)) was individually adjusted based on ovarian response. Transvaginal sonography and serial E2 levels were used to monitor ovarian follicular development. Once a dominant follicle reached 19–20 mm, 10,000 IU of hCG was given. Thirty-six hours later, transvaginal ultrasound-guided oocyte retrieval was performed. Insemination was performed with intracytoplasmic sperm injection (ICSI) in all cycles. Fertilization was confirmed 20 hours later with the presence of two pronuclei (2PN).
At 48 hrs cleavage was assessed and the final decision was made to proceed the next day to embryo biopsy if a minimum of 6 cells were identified and at least 5 cleavage stage embryos were confirmed. The embryo’s were placed in a Calcium-Magnesium free buffer solution and a laser was used for zona pellucida ablation. A micropipet tool was then introduced to remove a single blastomere from the embryo. The fully intact embryo was then placed back into cell culture. The single blastomere was placed into a lysis buffered solution and tube which was sent to the genetics laboratory for testing.
Once at Genesis Genetics (Detroit, MI), single blastomeres were amplified using the BlueGnome SurePlex whole genome amplification kit (Illumina, San Diego), amplified DNA was labelled and hybridised as described previously [8] onto BlueGnome 24sure V3 BAC microrrays. Microarrays were washed, scanned and single channel images imported into BlueGnome BlueFuse software. Images were normalised in silco to further single channel male and female hybridisations, ran within the same experiment and fixed algorithms within the software automatically called whole chromosome gains and losses. Any segmental chromosomes deletions or duplications larger than 10Mbp were manually curated.
Transfer was performed on the afternoon of day five in the CGH group. One or more euploid embryos were transferred after evaluation of the embryo quality and discussion with the patient. We generally recommended transferring one embryo for patients under 35 and two embryos for patients over 35 years old. The transfer procedure was performed with a Wallace catheter with a free hand technique under trans-abdominal ultrasound guidance. In patients with no euploid embryos the embryos were either discarded or underwent a trophectoderm biopsy and cryopreserved if they were high grade blastocysts.
Luteal-phase supplementation with IM or vaginal progesterone was given to all patients. Serum β-hCG levels were tested on days 12 and 14 after embryo transfer. If positive, transvaginal sonography was performed on day 19 to confirm presence of a gestational sac or sacs. Only pregnancies that resulted in sonographically confirmed gestational sacs were considered clinical pregnancies; biochemical pregnancies were counted as IVF failure. The implantation rate was defined as the number of gestational sacs divided by the number of embryos transferred. Ongoing pregnancies were those that continued on with a normal fetal heart rate into the second trimester. Miscarriages were defined as pregnancy loss prior to 20 gestational weeks.
Implantation rate (# of sacs/# embryos transferred) and probabilities of clinical pregnancy, ongoing pregnancy, miscarriage and multiple pregnancy were estimated and compared between control and CGH embryo transfer groups. Since some patients came in for follow-up procedures and contributed more than one cycle to the analysis, the correlation among repeated measures made on the same patient had to be accounted for in all statistical modeling. A repeated measures poisson regression model was used to estimate incident rate ratios (IRR) and corresponding 95 % confidence intervals to compare the implantation rates between groups. A repeated measures log-binomial model was used to estimate relative risks (RR) and corresponding 95 % confidence intervals to compare probabilities of pregnancy outcome measures between groups. A repeated measures mixed model was used to compare means (SD) of continuous and discrete measures between groups while accounting for correlation among measures from different cycles in the same patient. All statistical analyses were performed using SAS Version 9.2 (SAS Institute, Inc., Cary, NC). All hypothesis testing was conducted at the 5 % level of significance.
Results
In the thirty-nine cycles in the group undergoing CGH, 412 embryos were produced, 327 biopsed, 83/327 (25.4 %) euploid and 207/327 aneuploid (63.3 %). 37/327 (11.3 %) embryos were reported as “no signal”, 14 underwent trophectoderm rebiopsy and 1/14 (7.1 %) was euploid. In total 57 euploid embryos were transferred in 33 cycles and 6 cycles were cancelled for no euploid embryo.
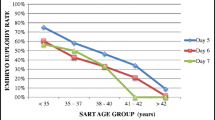
Indications for PGS can be found in Table 1. Among all age groups patients that underwent CGH were slightly older [Median 39, Range (28–42)] but there was no significant difference in their basal FSH [CGH = Median 5, Range (1–30) or AMH levels [CGH = Median 3, Range (0.4–14)] number of oocyte retrieved [CGH = Median 12, Range (5–30)] or the number of embryos fertilized [CGH = Median 9, Range (4–24)]. When comparing cases and controls, CGH cycles had significantly fewer embryos transferred. However, CGH resulted in a significant increase in implantation, clinical pregnancy and ongoing pregnancy rates, as well as a decrease in the multiple pregnancy rates and a trend towards decreased rate of miscarriages. Table 2.
Among patients less than 35 there was no difference in Age, FSH, AMH, number of oocytes or number of embryos. Despite significantly fewer number of embryos transferred, CGH resulted in significantly better implantation rate, clinical pregnancy and ongoing pregnancy rates, with a trend towards lower multiple pregnancy rate. Table 3.
Among patients 35 years or older there was no difference Age, FSH, AMH, number of oocytes retrieved or number of embryos. In the CGH cases, there were far fewer embryos transferred, with a significantly better implantation, clinical pregnancy and ongoing pregnancy rates, with a trend towards lower miscarriage rates. Table 4.
Cycles 38 years or older, that underwent CGH (n = 25) resulted in significant increase in implantation (48.6 % vs. 11.2 %, p = <0.0001), clinical pregnancy (60 % vs. 35 %, p = 0.0005) and ongoing pregnancy rates (52 % vs. 19.7 %, p = 0.0001). A non significant reduction was observed in miscarriage (13.3 % vs. 43.1 %, p = 0.08) and multiple pregnancy rates (15.4 % vs. 24.1 %, p = 0.5).
Single embryo transfer was performed in 15/33 (45.5 %) CGH cycles and 7/394 (1.8 %) controls. There was a non significant increase in implantation (66.7 % vs. 28.6 %, p = 0.17), clinical pregnancy (66.7 % vs. 28.6 %, p = 0.17) and ongoing pregnancy rates (60 % vs. 28.6 %, p = 0.2).
When we excluded cycles that had no embryos available for transfer, CGH resulted in a far higher clinical pregnancy rates (81.81 % vs. 43.91 %, p = <0.0001) and ongoing pregnancy rates (72.7 % vs 32.49 %, p = <0.0001). Among patients younger than 35 with embryos available for transfer, the clinical pregnancy rate improved to (100 % vs. 51.28 %, p = 0.01) and ongoing pregnancy rate improved to (85.7 % vs. 52.7 %, p = 0.045). Among patients 35 years or older with embryos available for transfer, the clinical pregnancy rate improved (76.9 % vs. 38.8 %, p = 0.0003) as well as the ongoing pregnancy rate (69.2 % vs. 24.9 %, p = <0.0001).
Products of conception analysis on the three miscarriages revealed two euploid and one tetraploid (96xxxx) karyotype.
Discussion
We found that our population of patients undergoing PGS and day 3 CGH were slightly older, but had far fewer embryos transferred and had a dramatic increase in implantation, clinical and ongoing pregnancy rates. Additionally blastomere biopsy and CGH markedly reduced the multiple pregnancy rates. We also found a trend towards lower miscarriage rates, which contributed to the improved ongoing pregnancy and may be significant with larger numbers.
Most studies comparing preimplanation genetic screening at the cleavage stage with CCS have reported numbers based on transferred cycles only. This study shows vastly improved outcomes even when including cycles with no euploid embryos to transfer. The reduction in miscarriages suggested in this study is consistent with other retrospective studies that have shown a decrease in miscarriage rates in patients with recurrent pregnancy loss treated with CCS [14, 22, 27].
This study does have several limitations. The main limitation is due to its retrospective design, which could lead to selection bias among patients undergoing CGH. Also, the number of CGH cases was far fewer than the number of controls. Our CGH cases were older, but were good prognosis patients as evidenced by their AMH, FSH and high embryo yield. Therefore these findings do not apply to poor responder patients. CGH is an expensive technology, primarily employed after several IVF cycles in affluent patients. The high cost of PGS presents one of the main challenges to its widespread or universal use. CGH on itself may have limited capacity in detecting polyploidy as observed in our analysis of products of conception.
Throughout the history of assisted reproduction, varied criteria has been used to select embryos with the highest probability of implantation and reproductive potential. Morphologic assessment was utilized first, followed by genetic screening with FISH. Several studies have looked at proteomics, metaboleomics and time-lapse photography to select the best embryo. Thus far these non-invasive technologies have been of limited or no value [1, 2, 4, 15, 17–19, 21, 25, 26, 30–32]. Currently CCS is being evaluated to determine how valuable it will be for embryo selection, and which patients are most likely to benefit. We also need to study which CCS technology will be most accurate and at which embryo stage it should be applied. Recent reports show that day 3 CCS is very consistent (94.2 %) with trophoectoderm CCS from the same embryo.
As to advantages of day 3 versus day 5 biopsy, our age-matched case-controlled abstract found that the blastocyst rate might be slightly reduced when biopsing on day 3, but the fully-expended and hatching blastocyst rate was the same. More than 50 % of euploid embryos would not have been able to be biopsed at day 5 (unpublished data). Most current data on day three blastomere biopsy with CCS is derived from retrospective case–control trials [14, 28, 37–39]. A large randomized controlled trial comparing cleavage-stage and blastocyst stage biopsy utilizing CGH would be helpful to determine the best timing for biopsy.
In conclusion, this is the first report to confirm increased implantation and per cycle ongoing pregnancy rates following cleavage-stage blastomere biopsy with CGH and fresh transfer. We found that CGH also led to a reduction of the number of the embryos transferred, reduced multiple pregnancy rates and resulted in a trend towards lower miscarriage rates. There is clearly a role for single embryo transfer after cleavage-stage CGH, which is further strengthened by our small but promising results. CCS utilizing CGH, whether at the cleavage or blastocyst stage, will lead to a far higher percentage of IVF patients undergoing successful single embryo transfer.
References
Assou S, Haouzi D, De Vos J, Hamamah S. Human cumulus cells as biomarkers for embryo and pregnancy outcomes. Mol Hum Reprod. 2010;16(8):531–8.
Brison DR, Houghton FD, Falconer D, Roberts SA, Hawkhead J, Humpherson PG, et al. Identification of viable embryos in IVF by non-invasive measurement of amino acid turnover. Hum Reprod. 2004;19(10):2319–24.
Capalbo A, Bono S, Spizzichino L, Biricik A, Baldi M, Colamaria S, et al. Sequential comprehensive chromosome analysis on polar bodies, blastomeres and trophoblast: insights into female meiotic errors and chromosomal segregation in the preimplantation window of embryo development. Hum Reprod. 2013;28(2):509–18.
Cruz M, Gadea B, Garrido N, Pedersen KS, Martínez M, Pérez-Cano I, et al. Embryo quality, blastocyst and ongoing pregnancy rates in oocyte donation patients whose embryos were monitored by time-lapse imaging. J Assist Reprod Genet. 2011;28(7):569–73.
Delhanty JD, Griffin DK, Handyside AH, Harper J, Atkinson GH, Pieters MH, et al. Detection of aneuploidy and chromosomal mosaicism in human embryos during preimplantation sex determination by fluorescent in situ hybridisation, (FISH). Hum Mol Genet. 1993;2(8):1183–5.
Drugan A, Koppitch 3rd FC, Williams 3rd JC, Johnson MP, Moghissi KS, Evans MI. Prenatal genetic diagnosis following recurrent early pregnancy loss. Obstet Gynecol. 1990;75(3 Pt 1):381–4.
Fauser BC. Screening of embryos for numerical chromosome abnormalities during in-vitro fertilisation is not useful for application in daily practice. Ned Tijdschr Geneeskd. 2008;152(13):734–6.
Fishel S, Gordon A, Lynch C, Dowell K, Ndukwe G, Kelada E, et al. Live birth after polar body array comparative genomic hybridization prediction of embryo ploidy-the future of IVF? Fertil Steril. 2010;93(3):1006.e1007–10.
Fragouli E, Wells D. Aneuploidy screening for embryo selection. Semin Reprod Med. 2012;30(4):289–301.
Fritz MA. Perspectives on the efficacy and indications for preimplantation genetic screening: where are we now? Hum Reprod. 2008;23(12):2617–21.
Hardarson T, Hanson C, Lundin K, Hillensjo T, Nilsson L, Stevic J, et al. Preimplantation genetic screening in women of advanced maternal age caused a decrease in clinical pregnancy rate: a randomized controlled trial. Hum Reprod. 2008;23(12):2806–12.
Harper J, Coonen E, De Rycke M, Fiorentino F, Geraedts J, Goossens V, et al. What next for preimplantation genetic screening (PGS)? A position statement from the ESHRE PGD Consortium Steering Committee. Hum Reprod. 2010;25(4):821–3.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2(4):280–91.
Hodes-Wertz B, Grifo J, Ghadir S, Kaplan B, Laskin CA, Glassner M, et al. Idiopathic recurrent miscarriage is caused mostly by aneuploid embryos. Fertil Steril. 2012;98(3):675–80.
Huang JY, Rosenwaks Z. In vitro fertilisation treatment and factors affecting success. Best Pract Res Clin Obstet Gynaecol. 2012;26(6):777–88.
Kamiguchi Y, Rosenbusch B, Sterzik K, Mikamo K. Chromosomal analysis of unfertilized human oocytes prepared by a gradual fixation-air drying method. Hum Genet. 1993;90(5):533–41.
Katz-Jaffe MG, McReynolds S, Gardner DK, Schoolcraft WB. The role of proteomics in defining the human embryonic secretome. Mol Hum Reprod. 2009;15(5):271–7.
Katz-Jaffe MG, Schoolcraft WB, Gardner DK. Analysis of protein expression (secretome) by human and mouse preimplantation embryos. Fertil Steril. 2006;86(3):678–85.
Lemmen JG, Agerholm I, Ziebe S. Kinetic markers of human embryo quality using time-lapse recordings of IVF/ICSI-fertilized oocytes. Reprod Biomed Online. 2008;17(3):385–91.
Mastenbroek S, Twisk M, van Echten-Arends J, Sikkema-Raddatz B, Korevaar JC, Verhoeve HR, et al. In vitro fertilization with preimplantation genetic screening. N Engl J Med. 2007;357(1):9–17.
Meseguer M, Rubio I, Cruz M, Basile N, Marcos J, Requena A. Embryo incubation and selection in a time-lapse monitoring system improves pregnancy outcome compared with a standard incubator: a retrospective cohort study. Fertil Steril. 2012;98(6):1481–1489.e1410.
Munne S, S ES, Grifo J, Marut E, Opsahl M and Taylor TH “Preimplantation genetic diagnosis using a-CGH significantly increases ongoing pregnancy rates per transfer.” Fertil Steril 2010; 94(S81).
Munne S, Lee A, Rosenwaks Z, Grifo J, Cohen J. Diagnosis of major chromosome aneuploidies in human preimplantation embryos. Hum Reprod. 1993;8(12):2185–91.
Palermo GD, Munne S, Colombero LT, Cohen J, Rosenwaks Z. Genetics of abnormal human fertilization. Hum Reprod. 1995;10 Suppl 1:120–7.
Pribenszky C, Losonczi E, Molnár M, Lang Z, Mátyás S, Rajczy K, et al. Prediction of in-vitro developmental competence of early cleavage-stage mouse embryos with compact time-lapse equipment. Reprod Biomed Online. 2010;20(3):371–9.
Pribenszky C, Mátyás S, Kovács P, Losonczi E, Zádori J, Vajta G. Pregnancy achieved by transfer of a single blastocyst selected by time-lapse monitoring. Reprod Biomed Online. 2010;21(4):533–6.
Rabinowitz A, Beltsos A, D Potter, Bush M, Givens C and D Smotrich. “Effects of advanced maternal age are abrogated in 122 patients undergoing transfer of embryos with euploid microarray screening results at cleavage stage.” Fertil Steril 2010;94(S80).
Rubio C, Simón C, Vidal F, Rodrigo L, Pehlivan T, Remohí J, et al. Chromosomal abnormalities and embryo development in recurrent miscarriage couples. Hum Reprod. 2003;18(1):182–8.
Schoolcraft WB, Katz-Jaffe MG, Stevens J, Rawlins M, Munne S. Preimplantation aneuploidy testing for infertile patients of advanced maternal age: a randomized prospective trial. Fertil Steril. 2009;92(1):157–62.
Scott R, Seli E, Miller K, Sakkas D, Scott K, Burns DH. Noninvasive metabolomic profiling of human embryo culture media using Raman spectroscopy predicts embryonic reproductive potential: a prospective blinded pilot study. Fertil Steril. 2008;90(1):77–83.
Seli E, Sakkas D, Scott R, Kwok SC, Rosendahl SM, Burns DH. Noninvasive metabolomic profiling of embryo culture media using Raman and near-infrared spectroscopy correlates with reproductive potential of embryos in women undergoing in vitro fertilization. Fertil Steril. 2007;88(5):1350–7.
Seli E, Vergouw CG, Morita H, Botros L, Roos P, Lambalk CB, et al. Noninvasive metabolomic profiling as an adjunct to morphology for noninvasive embryo assessment in women undergoing single embryo transfer. Fertil Steril. 2010;94(2):535–42.
Staessen C, Platteau P, Van Assche E, Michiels A, Tournaye H, Camus M, et al. Comparison of blastocyst transfer with or without preimplantation genetic diagnosis for aneuploidy screening in couples with advanced maternal age: a prospective randomized controlled trial. Hum Reprod. 2004;19(12):2849–58.
Staessen C, Verpoest W, Donoso P, Haentjens P, Van der Elst J, Liebaers I, et al. Preimplantation genetic screening does not improve delivery rate in women under the age of 36 following single-embryo transfer. Hum Reprod. 2008;23(12):2818–25.
Treff NR, Levy B, Su J, Northrop LE, Tao X, Scott Jr RT. SNP microarray-based 24 chromosome aneuploidy screening is significantly more consistent than FISH. Mol Hum Reprod. 2010;16(8):583–9.
Twisk M, Mastenbroek S, Hoek A, Heineman MJ, van der Veen F, Bossuyt PM, et al. No beneficial effect of preimplantation genetic screening in women of advanced maternal age with a high risk for embryonic aneuploidy. Hum Reprod. 2008;23(12):2813–7.
Voullaire L, Wilton L, McBain J, Callaghan T, Williamson R. Chromosome abnormalities identified by comparative genomic hybridization in embryos from women with repeated implantation failure. Mol Hum Reprod. 2002;8(11):1035–41.
Wells D, Delhanty JD. Comprehensive chromosomal analysis of human preimplantation embryos using whole genome amplification and single cell comparative genomic hybridization. Mol Hum Reprod. 2000;6(11):1055–62.
Wilton L, Voullaire L, Sargeant P, Williamson R, McBain J. Preimplantation aneuploidy screening using comparative genomic hybridization or fluorescence in situ hybridization of embryos from patients with recurrent implantation failure. Fertil Steril. 2003;80(4):860–8.
Acknowledgments
The authors thank the office and embryology staff of the Continuum Reproductive Center, and wish to acknowledge the assistance of Carolyn Waldron, MS, MA.
Disclosure
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Martin D. Keltz and Mario Vega contributed equally to this article.
Capsule Cleavage-stage PGS with CGH results in higher implantation, clinical pregnancy and ongoing pregnancy rates, while lowering multiple pregnancy and miscarriage rates.
Rights and permissions
About this article
Cite this article
Keltz, M.D., Vega, M., Sirota, I. et al. Preimplantation Genetic Screening (PGS) with Comparative Genomic Hybridization (CGH) following day 3 single cell blastomere biopsy markedly improves IVF outcomes while lowering multiple pregnancies and miscarriages. J Assist Reprod Genet 30, 1333–1339 (2013). https://doi.org/10.1007/s10815-013-0070-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-013-0070-6